Diagnostic Techniques to Increase the Safety of Phakic Intraocular Lenses
Abstract
1. Introduction
2. Types of Phakic Intraocular Lenses
2.1. Iris-Supported Anterior Chamber Phakic Intraocular Lenses
2.2. Angle-Supported Anterior Chamber Phakic Intraocular Lenses
2.3. Posterior Chamber Phakic Intraocular Lenses
3. Addressing the Risk of Endothelial Cell Loss
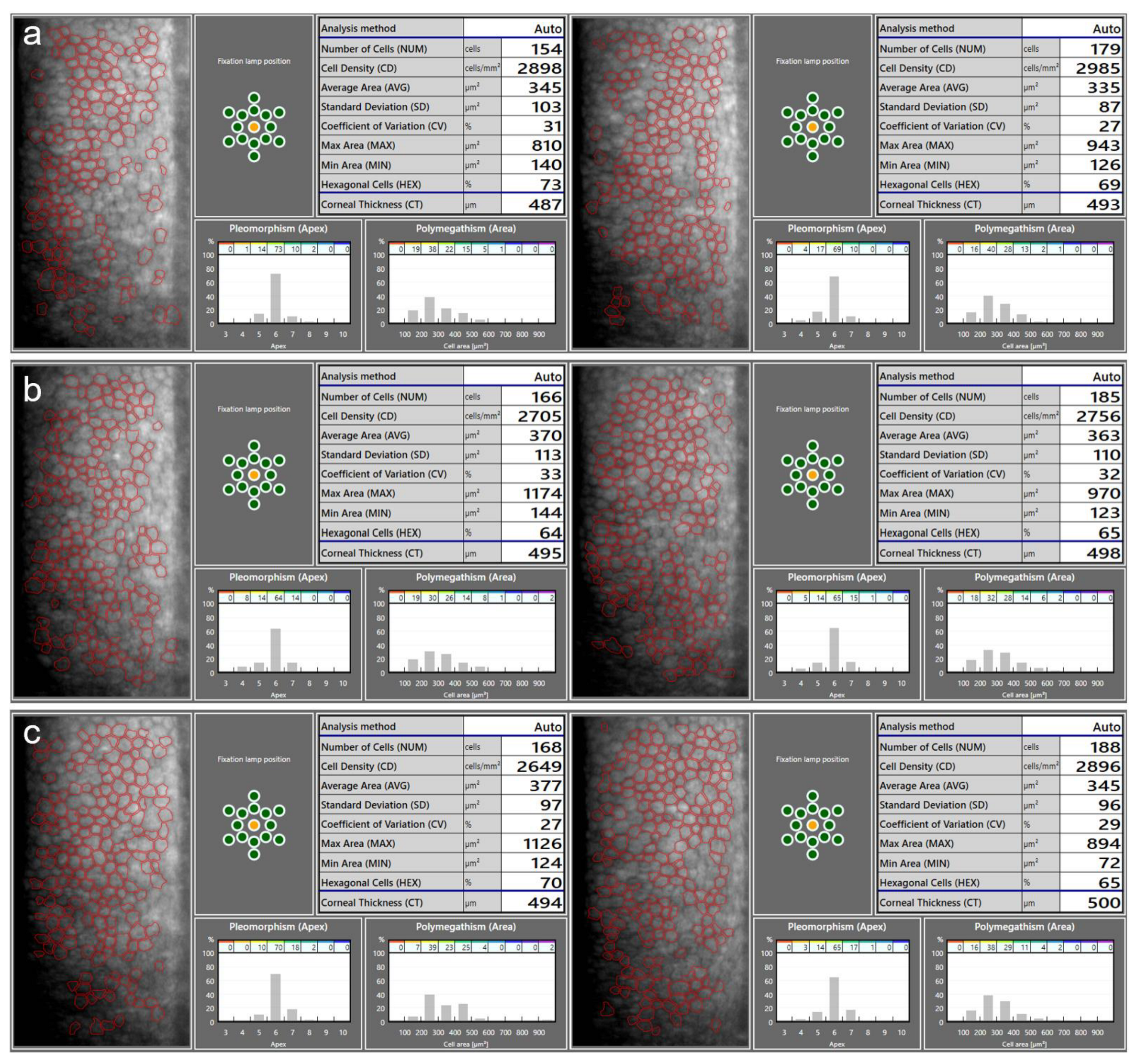
3.1. Endothelial Cell Density Measurement
3.2. Assessing Endothelial Cell Loss
3.3. Endothelial Cell Loss and the Phakic Intraocular Lens Type
3.4. Anterior Chamber Morphometrics
3.4.1. Distance from the Phakic Intraocular Lens to the Endothelium
3.4.2. Anterior Chamber Depth
4. Addressing the Risk of Cataract
The Influence of the Vault on Cataract Development
5. Addressing the Risk of Ocular Hypertension and Glaucoma
6. Measurement of the Vault
7. ICL Vault Prediction
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Auffarth, G.U.; Apple, D.J. History of the development of intraocular lenses. Ophthalmologe 2001, 98, 1017–1028. [Google Scholar] [CrossRef] [PubMed]
- Güell, J.L.; Morral, M.; Kook, D.; Kohnen, T. Phakic intraocular lenses part 1: Historical overview, current models, selection criteria, and surgical techniques. J. Cataract. Refract. Surg. 2010, 36, 1976–1993. [Google Scholar] [CrossRef] [PubMed]
- Alió, J.L.; Toffaha, B.T.; Peña-Garcia, P.; Sádaba, L.M.; Barraquer, R.I. Phakic intraocular lens explantation: Causes in 240 cases. J. Refract. Surg. 2015, 31, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Schallhorn, S.C.; Sugar, A.; Farjo, A.A.; Majmudar, P.A.; Trattler, W.B.; Tanzer, D.J. Phakic intraocular lens implantation for the correction of myopia: A report by the American Academy of Ophthalmology. Ophthalmology 2009, 116, 2244–2258. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, T.; Kook, D.; Morral, M.; Güell, J.L. Phakic intraocular lenses: Part 2: Results and complications. J. Cataract. Refract. Surg. 2010, 36, 2168–2194. [Google Scholar] [CrossRef]
- Espandar, L.; Meyer, J.J.; Moshirfar, M. Phakic intraocular lenses. Curr. Opin. Ophthalmol. 2008, 19, 349–356. [Google Scholar] [CrossRef]
- Martínez-Plaza, E.; López-Miguel, A.; Holgueras, A.; Barraquer, R.I.; Alió, J.L.; Maldonado, M.J. Phakic intraocular lenses: Recent advances and innovations. Arch. Soc. Esp. Oftalmol. 2020, 95, 178–187. [Google Scholar] [CrossRef]
- Ophtec, B.V. Sicherheitsmitteilung (Field Safety Notice, FSN). Phake Intraokularlinsen Artisan und Artiflex. Available online: https://www.bfarm.de/SharedDocs/Kundeninfos/DE/11/2021/20671-21_kundeninfo_de.pdf?__blob=publicationFile (accessed on 30 June 2023).
- Kommission Refraktive Chirurgie (KRC). Bewertung und Qualitätssicherung refraktiv-chirurgischer Eingriffe durch die DOG und den BVA—KRC-Empfehlungen. Available online: http://bva.dog/krc/qualit.pdf (accessed on 30 June 2023).
- Naujokaitis, T.; Auffarth, G.U.; Łabuz, G.; Khoramnia, R. Endothelial Cell Loss in Patients with Phakic Intraocular Lenses. Klin. Monbl. Augenheilkd. 2023; Submitted. [Google Scholar]
- Qasem, Q.; Kirwan, C.; O’Keefe, M. 5-year prospective follow-up of Artisan phakic intraocular lenses for the correction of myopia, hyperopia and astigmatism. Ophthalmologica 2010, 224, 283–290. [Google Scholar] [CrossRef]
- Kwitko, S.; Zambon, G.M.; Marafon, S.B. Artisan and artiflex phakic intraocular lenses for high ametropia: Long-term results. Arch. Clin. Exp. 2021, 3, 39–46. [Google Scholar]
- Budo, C.; Hessloehl, J.C.; Izak, M.; Luyten, G.P.; Menezo, J.L.; Sener, B.A.; Tassignon, M.J.; Termote, H.; Worst, J.G. Multicenter study of the Artisan phakic intraocular lens. J. Cataract. Refract. Surg. 2000, 26, 1163–1171. [Google Scholar] [CrossRef]
- Castro de Luna, G.; Ramos-López, D.; Castaño Fernández, A.B.; Cuevas Santamaría, D. Artiflex foldable lens for myopia correction results of 10 years of follow-up. Eye 2019, 33, 1564–1569. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, J.F.; Fernández-Vega-Cueto, L.; Alfonso-Bartolozzi, B.; Montés-Micó, R.; Fernández-Vega, L. Five-Year Follow-up of Correction of Myopia: Posterior Chamber Phakic Intraocular Lens with a Central Port Design. J. Refract. Surg. 2019, 35, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, S.; Casamenti, V.; Benedetti, M. Long-term endothelial changes in phakic eyes after Artisan intraocular lens implantation to correct myopia: Five-year study. J. Cataract. Refract. Surg. 2007, 33, 784–790. [Google Scholar] [CrossRef]
- Eldanasoury, A.M.; Roozbahani, M.; Tolees, S.; Arana, C. Long-Term Effect of Anterior Chamber Depth on Endothelial Cell Density in Patients with Iris-Fixated Phakic Intraocular Lenses. J. Refract. Surg. 2019, 35, 493–500. [Google Scholar] [CrossRef]
- Güell, J.L.; Morral, M.; Gris, O.; Gaytan, J.; Sisquella, M.; Manero, F. Five-year follow-up of 399 phakic Artisan-Verisyse implantation for myopia, hyperopia, and/or astigmatism. Ophthalmology 2008, 115, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Jonker, S.M.R.; Berendschot, T.; Ronden, A.E.; Saelens, I.E.Y.; Bauer, N.J.C.; Nuijts, R. Long-Term Endothelial Cell Loss in Patients with Artisan Myopia and Artisan Toric Phakic Intraocular Lenses: 5- and 10-Year Results. Ophthalmology 2018, 125, 486–494. [Google Scholar] [CrossRef]
- Jonker, S.M.R.; Berendschot, T.; Ronden, A.E.; Saelens, I.E.Y.; Bauer, N.J.C.; Nuijts, R. Five-Year Endothelial Cell Loss After Implantation with Artiflex Myopia and Artiflex Toric Phakic Intraocular Lenses. Am. J. Ophthalmol. 2018, 194, 110–119. [Google Scholar] [CrossRef]
- Kim, T.Y.; Moon, I.H.; Park, S.E.; Ji, Y.W.; Lee, H.K. Long-Term Follow-Up of Corneal Endothelial Cell Changes After Iris-Fixated Phakic Intraocular Lens Explantation. Cornea 2023, 42, 150–155. [Google Scholar] [CrossRef]
- Monteiro, T.; Correia, F.F.; Franqueira, N.; Mendes, J.C.; Pinto, C.; Vaz, F. Long-term efficacy and safety results after iris-fixated foldable phakic intraocular lens for myopia and astigmatism: 6-year follow-up. J. Cataract. Refract. Surg. 2021, 47, 211–220. [Google Scholar] [CrossRef]
- Monteiro, T.; Pinto, C.; Franqueira, N.; Faria-Correia, F.; Mendes, J.; Sánchez, J.A.; Vaz, F. Efficacy and Safety After Toric Posterior Chamber Implantable Collamer Lens and Toric Iris-Fixated Foldable Phakic Intraocular Lens for Myopic Astigmatism. J. Refract. Surg. 2022, 38, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Nemcova, I.; Pasta, J.; Hladikova, K.; Komarc, M.; Pospisilova, D.; Nemec, P.; Tesar, J.; Kratky, V.; Sin, M. Myopic Correction with Iris-Fixated Phakic Intraocular Lenses: Twelve-Year Results. J. Ophthalmol. 2021, 2021, 7027793. [Google Scholar] [CrossRef] [PubMed]
- Javaloy, J.; Alió, J.L.; Iradier, M.T.; Abdelrahman, A.M.; Javaloy, T.; Borrás, F. Outcomes of ZB5M angle-supported anterior chamber phakic intraocular lenses at 12 years. J. Refract. Surg. 2007, 23, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Plainer, S.; Wenzl, E.; Saalabian, A.A.; Wohlfart, C.; Vidic, B.; El-Shabrawi, Y.; Ardjomand, N. Long-term follow-up with I-CARE phakic IOLs. Br. J. Ophthalmol. 2011, 95, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, T.; LaFontaine, L.; Andrew, R. Long-term safety follow-up of an anterior chamber angle-supported phakic intraocular lens. J. Cataract. Refract. Surg. 2017, 43, 1163–1170. [Google Scholar] [CrossRef]
- Papa-Vettorazzi, M.R.; Moura-Coelho, N.; Manero, F.; Cruz-Rodriguez, J.B.; Elies, D.; Güell, J.L. Long-term efficacy and safety profiles of iris-fixated foldable anterior chamber phakic intraocular lens implantation in eyes with more than 10 years of follow-up. J. Cataract. Refract. Surg. 2022, 48, 987–992. [Google Scholar] [CrossRef]
- Sanders, D.R.; Vukich, J.A.; Doney, K.; Gaston, M.U.S. Food and Drug Administration clinical trial of the Implantable Contact Lens for moderate to high myopia. Ophthalmology 2003, 110, 255–266. [Google Scholar]
- Rayner, S.A.; Bhikoo, R.; Gray, T. Spherical implantable collamer lenses for myopia and hyperopia: 126 eyes with 1-year follow up. Clin. Exp. Ophthalmol. 2010, 38, 21–26. [Google Scholar] [CrossRef]
- Packer, M. Meta-analysis and review: Effectiveness, safety, and central port design of the intraocular collamer lens. Clin. Ophthalmol. 2016, 10, 1059–1077. [Google Scholar] [CrossRef]
- Gonvers, M.; Bornet, C.; Othenin-Girard, P. Implantable contact lens for moderate to high myopia: Relationship of vaulting to cataract formation. J. Cataract. Refract. Surg. 2003, 29, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kang, D.S.; Ha, B.J.; Choi, M.; Kim, E.K.; Seo, K.Y.; Kim, T. Effect of Accommodation on Vaulting and Movement of Posterior Chamber Phakic Lenses in Eyes with Implantable Collamer Lenses. Am. J. Ophthalmol. 2015, 160, 710–716.e1. [Google Scholar] [CrossRef] [PubMed]
- Vasavada, V.; Srivastava, S.; Vasavada, S.A.; Sudhalkar, A.; Vasavada, A.R.; Vasavada, V.A. Safety and Efficacy of a New Phakic Posterior Chamber IOL for Correction of Myopia: 3 Years of Follow-up. J. Refract. Surg. 2018, 34, 817–823. [Google Scholar] [CrossRef]
- Brar, S.; Gautam, M.; Sute, S.S.; Pereira, S.; Ganesh, S. Visual and Refractive Outcomes with the Eyecryl Phakic Toric IOL Versus the Visian Toric Implantable Collamer Lens: Results of a 2-Year Prospective Comparative Study. J. Refract. Surg. 2021, 37, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Taneri, S.; Dick, H.B. Initial clinical outcomes of two different phakic posterior chamber IOLs for the correction of myopia and myopic astigmatism. Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 1763–1772. [Google Scholar] [CrossRef] [PubMed]
- Stodulka, P.; Slovak, M.; Sramka, M.; Polisensky, J.; Liska, K. Posterior chamber phakic intraocular lens for the correction of presbyopia in highly myopic patients. J. Cataract. Refract. Surg. 2020, 46, 40–44. [Google Scholar] [CrossRef]
- Kohnen, T.; Maxwell, A.; Holland, S.; Lane, S.; Von Tress, M.; Salem, C.; Fontaine, L.; Laura, M.P.H. Ten-year safety follow-up and post-explant analysis of an anterior chamber phakic IOL. J. Cataract. Refract. Surg. 2020, 46, 1457–1465. [Google Scholar] [CrossRef]
- Menezo, J.L.; Cisneros, A.L.; Rodriguez-Salvador, V. Endothelial study of iris-claw phakic lens: Four year follow-up. J. Cataract. Refract. Surg. 1998, 24, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- MacRae, S.; Holladay, J.T.; Hilmantel, G.; Calogero, D.; Masket, S.; Stark, W. Special Report: American Academy of Ophthalmology Task Force Recommendations for Specular Microscopy for Phakic Intraocular Lenses. Ophthalmology 2017, 124, 141–142. [Google Scholar] [CrossRef]
- Benetz, B.A.; Lass, J.H. Specular Microscopy. Cornea 2018, 37 (Suppl. S1), S7–S8. [Google Scholar] [CrossRef]
- Waring, G.O., 3rd; Bourne, W.M.; Edelhauser, H.F.; Kenyon, K.R. The corneal endothelium. Normal and pathologic structure and function. Ophthalmology 1982, 89, 531–590. [Google Scholar] [CrossRef] [PubMed]
- Laing, R.A.; Sanstrom, M.M.; Berrospi, A.R.; Leibowitz, H.M. Changes in the corneal endothelium as a function of age. Exp. Eye Res. 1976, 22, 587–594. [Google Scholar] [CrossRef]
- Edelhauser, H.F. The balance between corneal transparency and edema: The Proctor Lecture. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1754–1767. [Google Scholar] [CrossRef]
- McCarey, B.E.; Edelhauser, H.F.; Lynn, M.J. Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices, and new intraocular drugs and solutions. Cornea 2008, 27, 1–16. [Google Scholar] [CrossRef]
- Rio-Cristobal, A.; Martin, R. Corneal assessment technologies: Current status. Surv. Ophthalmol. 2014, 59, 599–614. [Google Scholar] [CrossRef]
- Huang, J.; Maram, J.; Tepelus, T.C.; Modak, C.; Marion, K.; Sadda, S.R.; Chopra, V.; Lee, O.L. Comparison of manual & automated analysis methods for corneal endothelial cell density measurements by specular microscopy. J. Optom. 2018, 11, 182–191. [Google Scholar]
- Pop, M.; Payette, Y. Initial results of endothelial cell counts after Artisan lens for phakic eyes: An evaluation of the United States Food and Drug Administration Ophtec Study. Ophthalmology 2004, 111, 309–317. [Google Scholar] [CrossRef]
- Luft, N.; Hirnschall, N.; Schuschitz, S.; Draschl, P.; Findl, O. Comparison of 4 specular microscopes in healthy eyes and eyes with cornea guttata or corneal grafts. Cornea 2015, 34, 381–386. [Google Scholar] [CrossRef]
- Goldich, Y.; Marcovich, A.L.; Barkana, Y.; Hartstein, M.; Morad, Y.; Avni, I.; Zadok, D. Comparison of corneal endothelial cell density estimated with 2 noncontact specular microscopes. Eur. J. Ophthalmol. 2010, 20, 825–830. [Google Scholar] [CrossRef]
- Garza-Leon, M. Corneal endothelial cell analysis using two non-contact specular microscopes in healthy subjects. Int. Ophthalmol. 2016, 36, 453–461. [Google Scholar] [CrossRef]
- Salvetat, M.L.; Zeppieri, M.; Miani, F.; Parisi, L.; Felletti, M.; Brusini, P. Comparison between laser scanning in vivo confocal microscopy and noncontact specular microscopy in assessing corneal endothelial cell density and central corneal thickness. Cornea 2011, 30, 754–759. [Google Scholar] [CrossRef]
- Fliotsos, M.J.; Deljookorani, S.; Dzhaber, D.; Chandan, S.; Ighani, M.; Eghrari, A.O. Qualitative and quantitative analysis of the corneal endothelium with smartphone specular microscopy. Cornea 2020, 39, 924. [Google Scholar] [CrossRef]
- Ono, T.; Mori, Y.; Nejima, R.; Iwasaki, T.; Miyai, T.; Miyata, K. Corneal endothelial cell density and morphology in ophthalmologically healthy young individuals in Japan: An observational study of 16842 eyes. Sci. Rep. 2021, 11, 18224. [Google Scholar] [CrossRef]
- Bourne, W.M.; Nelson, L.R.; Hodge, D.O. Central corneal endothelial cell changes over a ten-year period. Investig. Ophthalmol. Vis. Sci. 1997, 38, 779–782. [Google Scholar]
- Doors, M.; Cals, D.W.; Berendschot, T.T.; de Brabander, J.; Hendrikse, F.; Webers, C.A.; Nuijts, M.M.A. Influence of anterior chamber morphometrics on endothelial cell changes after phakic intraocular lens implantation. J. Cataract. Refract. Surg. 2008, 34, 2110–2118. [Google Scholar] [CrossRef]
- Mishima, S. Clinical investigations on the corneal endothelium-XXXVIII Edward Jackson Memorial Lecture. Am. J. Ophthalmol. 1982, 93, 1–29. [Google Scholar] [CrossRef]
- Alfonso, J.F.; Baamonde, B.; Fernández-Vega, L.; Fernandes, P.; González-Méijome, J.M.; Montés-Micó, R. Posterior chamber collagen copolymer phakic intraocular lenses to correct myopia: Five-year follow-up. J. Cataract. Refract. Surg. 2011, 37, 873–880. [Google Scholar] [CrossRef]
- Bouheraoua, N.; Bonnet, C.; Labbé, A.; Sandali, O.; Lecuen, N.; Ameline, B.; Borderie, V.; Laroche, L. Iris-fixated phakic intraocular lens implantation to correct myopia and a predictive model of endothelial cell loss. J. Cataract. Refract. Surg. 2015, 41, 2450–2457. [Google Scholar] [CrossRef]
- Chebli, S.; Rabilloud, M.; Burillon, C.; Kocaba, V. Corneal Endothelial Tolerance After Iris-Fixated Phakic Intraocular Lens Implantation: A Model to Predict Endothelial Cell Survival. Cornea 2018, 37, 591–595. [Google Scholar] [CrossRef]
- Moya, T.; Javaloy, J.; Montés-Micó, R.; Beltrán, J.; Muñoz, G.; Montalbán, R. Implantable Collamer Lens for Myopia: Assessment 12 Years After Implantation. J. Refract. Surg. 2015, 31, 548–556. [Google Scholar] [CrossRef]
- Papa-Vettorazzi, M.R.; Güell, J.L.; Cruz-Rodriguez, J.B.; Moura-Coelho, N.; Elies, D. Long-term efficacy and safety profiles after posterior chamber phakic intraocular lens implantation in eyes with more than 10 years of follow-up. J. Cataract. Refract. Surg. 2022, 48, 813–818. [Google Scholar] [CrossRef]
- Royo, M.; Jiménez, Á.; Martínez-Alberquilla, I.; Alfonso, J.F. Eight-year follow-up of Artiflex and Artiflex Toric phakic intraocular lens. Eur. J. Ophthalmol. 2022, 32, 2051–2058. [Google Scholar] [CrossRef]
- Saxena, R.; Boekhoorn, S.S.; Mulder, P.G.; Noordzij, B.; van Rij, G.; Luyten, G.P. Long-term follow-up of endothelial cell change after Artisan phakic intraocular lens implantation. Ophthalmology 2008, 115, 608–613.e1. [Google Scholar] [CrossRef]
- Gaurisankar, Z.S.; van Rijn, G.A.; Cheng, Y.Y.Y.; Luyten, G.P.M.; Beenakker, J.M. Two-year results after combined phacoemulsification and iris-fixated phakic intraocular lens removal. Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 1367–1375. [Google Scholar] [CrossRef]
- de Vries, N.E.; Tahzib, N.G.; Budo, C.J.; Webers, C.A.; de Boer, R.; Hendrikse, F.; Nuijts, R.M. Results of cataract surgery after implantation of an iris-fixated phakic intraocular lens. J. Cataract. Refract. Surg. 2009, 35, 121–126. [Google Scholar] [CrossRef]
- Vargas, V.; Marinho, A.; El Sayyad, F.; Alio Del Barrio, J.L.; Alio, J.L. Safety and visual outcomes following Iris-claw phakic intraocular lens bilensectomy. Eur. J. Ophthalmol. 2021, 31, 1795–1801. [Google Scholar] [CrossRef]
- Vargas, V.; Alió, J.L.; Barraquer, R.I.; Antin, J.C.D.; García, C.; Duch, F.; Balgos, J.; del Barrio, J.L.A. Safety and visual outcomes following posterior chamber phakic intraocular lens bilensectomy. Eye Vis. 2020, 7, 34. [Google Scholar] [CrossRef]
- Doors, M.; Berendschot, T.T.; Webers, C.A.; Nuijts, R.M. Model to predict endothelial cell loss after iris-fixated phakic intraocular lens implantation. Investig. Ophthalmol. Vis. Sci. 2010, 51, 811–815. [Google Scholar] [CrossRef]
- Choi, J.H.; Lim, D.H.; Nam, S.W.; Yang, C.M.; Chung, E.S.; Chung, T.Y. Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J. Cataract. Refract. Surg. 2019, 45, 1555–1561. [Google Scholar] [CrossRef]
- Fernández-Vega-Cueto, L.; Alfonso-Bartolozzi, B.; Lisa, C.; Madrid-Costa, D.; Alfonso, J.F. Seven-year follow-up of posterior chamber phakic intraocular lens with central port design. Eye Vis. 2021, 8, 23. [Google Scholar] [CrossRef]
- Guber, I.; Mouvet, V.; Bergin, C.; Perritaz, S.; Othenin-Girard, P.; Majo, F. Clinical Outcomes and Cataract Formation Rates in Eyes 10 Years After Posterior Phakic Lens Implantation for Myopia. JAMA Ophthalmol. 2016, 134, 487–494. [Google Scholar] [CrossRef]
- Igarashi, A.; Shimizu, K.; Kamiya, K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am. J. Ophthalmol. 2014, 157, 532–539.e1. [Google Scholar] [CrossRef]
- Lee, J.; Kim, Y.; Park, S.; Bae, J.; Lee, S.; Park, Y.; Lee, J.; Lee, J.-E. Long-term clinical results of posterior chamber phakic intraocular lens implantation to correct myopia. Clin. Exp. Ophthalmol. 2016, 44, 481–487. [Google Scholar] [CrossRef]
- Nakamura, T.; Isogai, N.; Kojima, T.; Yoshida, Y.; Sugiyama, Y. Posterior Chamber Phakic Intraocular Lens Implantation for the Correction of Myopia and Myopic Astigmatism: A Retrospective 10-Year Follow-up Study. Am. J. Ophthalmol. 2019, 206, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Packer, K.T.; Vlasov, A.D.; Greenburg, D.L.; Coggin, A.; Weightman, J.W.; Beltran, T.M.; Berry-Cabán, C.S.; Carroll, R.B. U.S. military implantable collamer lens surgical outcomes: 11-year retrospective review. J. Cataract. Refract. Surg. 2022, 48, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Pesando, P.M.; Ghiringhello, M.P.; Di Meglio, G.; Fanton, G. Posterior chamber phakic intraocular lens (ICL) for hyperopia: Ten-year follow-up. J. Cataract. Refract. Surg. 2007, 33, 1579–1584. [Google Scholar] [CrossRef] [PubMed]
- Edelhauser, H.F.; Sanders, D.R.; Azar, R.; Lamielle, H. Corneal endothelial assessment after ICL implantation. J. Cataract. Refract. Surg. 2004, 30, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Morral, M.; Güell, J.L.; El Husseiny, M.A.; Elies, D.; Gris, O.; Manero, F. Paired-eye comparison of corneal endothelial cell counts after unilateral iris-claw phakic intraocular lens implantation. J. Cataract. Refract. Surg. 2016, 42, 117–126. [Google Scholar] [CrossRef]
- Tahzib, N.G.; Nuijts, R.M.; Wu, W.Y.; Budo, C.J. Long-term study of Artisan phakic intraocular lens implantation for the correction of moderate to high myopia: Ten-year follow-up results. Ophthalmology 2007, 114, 1133–1142. [Google Scholar] [CrossRef]
- Yaşa, D.; Ağca, A. Verisyse versus Veriflex Phakic Intraocular Lenses: Refractive Outcomes and Endothelial Cell Density 5 Years after Surgery. J. Ophthalmol. 2018, 2018, 4210460. [Google Scholar] [CrossRef]
- Marta, A.; Leite, J.; Abreu, A.C.; Monteiro, S.; Pinto, C. Long-term results in patients with iris-fixated foldable phakic intraocular lenses for myopia and astigmatism. J. Cataract. Refract. Surg. 2022, 48, 993–998. [Google Scholar] [CrossRef]
- Yildirim, Y.; Çakmak, S.; Sucu, M.E.; Kepez Yildiz, B.; Kirgiz, A.; Akbas, Y.B.; Yasa, D.; Demirok, A. Comparative study of small-incision lenticule extraction and phakic intraocular lens implantation for the correction of high myopia: 6-year results. J. Cataract. Refract. Surg. 2021, 47, 221–226. [Google Scholar] [CrossRef]
- Yildirim, T.M.; Khoramnia, R.; Son, H.-S.; Mayer, C.S.; Łabuz, G.; Munro, D.J.; Auffarth, G.U. Reasons for explantation of phakic intraocular lenses and associated perioperative complications: Cross-sectional explant registry analysis. BMC Ophthalmol. 2021, 21, 80. [Google Scholar] [CrossRef]
- de Souza, R.F.; Allemann, N.; Forseto, A.; Barros, P.S.; Chamon, W.; Nosé, W. Ultrasound biomicroscopy and Scheimpflug photography of angle-supported phakic intraocular lens for high myopia. J. Cataract. Refract. Surg. 2003, 29, 1159–1166. [Google Scholar] [CrossRef]
- Pavlin, C.J.; Foster, F.S. Ultrasound biomicroscopy. High-frequency ultrasound imaging of the eye at microscopic resolution. Radiol. Clin. N. Am. 1998, 36, 1047–1058. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Drechsler, J.; Lin, A.; Widlus, M.; Qureshi, A.; Stoleru, G.; Saeedi, O.; Levin, M.R.; Kaleem, M.; Jaafar, M. Repeatability and Reliability of Quantified Ultrasound Biomicroscopy Image Analysis of the Ciliary Body at the Pars Plicata. Ultrasound Med. Biol. 2021, 47, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, M.; Bühren, J.; Kohnen, T. Position of angle-supported, iris-fixated, and ciliary sulcus-implanted myopic phakic intraocular lenses evaluated by Scheimpflug photography. Am. J. Ophthalmol. 2004, 138, 723–731. [Google Scholar] [CrossRef]
- Rabsilber, T.M.; Khoramnia, R.; Auffarth, G.U. Anterior chamber measurements using Pentacam rotating Scheimpflug camera. J. Cataract. Refract. Surg. 2006, 32, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Baïkoff, G. Anterior segment OCT and phakic intraocular lenses: A perspective. J. Cataract. Refract. Surg. 2006, 32, 1827–1835. [Google Scholar] [CrossRef]
- Meduri, E.; Gillmann, K.M.; Bravetti, G.E.; Niegowski, L.J.; Mermoud, A.; Weinreb, R.N.; Mansouri, K.M. Iridocorneal Angle Assessment After Laser Iridotomy with Swept-source Optical Coherence Tomography. J. Glaucoma. 2020, 29, 1030–1035. [Google Scholar] [CrossRef]
- Gonzalez-Lopez, F.; Mompean, B.; Bilbao-Calabuig, R.; Vila-Arteaga, J.; Beltran, J.; Baviera, J. Dynamic Assessment of Light-Induced Vaulting Changes of Implantable Collamer Lens with Central Port by Swept-Source OCT: Pilot Study. Transl. Vis. Sci. Technol. 2018, 7, 4. [Google Scholar] [CrossRef]
- Gaurisankar, Z.S.; van Rijn, G.A.; Luyten, G.P.M.; Beenakker, J.M. Differences between Scheimpflug and optical coherence tomography in determining safety distances in eyes with an iris-fixating phakic intraocular lens. Graefes. Arch. Clin. Exp. Ophthalmol. 2021, 259, 231–238. [Google Scholar] [CrossRef]
- Lomoriello, D.S.; Lombardo, M.; Gualdi, L.; Iacobelli, L.; Tranchina, L.; Ducoli, P.; Serrao, S. Stability of cachet phakic intraocular lens position during 6-months follow-up. Open Ophthalmol. J. 2013, 7, 20–23. [Google Scholar] [CrossRef][Green Version]
- Güell, J.L.; Morral, M.; Gris, O.; Gaytan, J.; Sisquella, M.; Manero, F. Evaluation of Verisyse and Artiflex phakic intraocular lenses during accommodation using Visante optical coherence tomography. J. Cataract. Refract. Surg. 2007, 33, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Vicent, A.; Pérez-Vives, C.; Ferrer-Blasco, T.; García-Lázaro, S.; Montés-Micó, R. Device interchangeability on anterior chamber depth and white-to-white measurements: A thorough literature review. Int. J. Ophthalmol. 2016, 9, 1057–1065. [Google Scholar]
- Khoramnia, R.; Rabsilber, T.M.; Auffarth, G.U. Central and peripheral pachymetry measurements according to age using the Pentacam rotating Scheimpflug camera. J. Cataract. Refract. Surg. 2007, 33, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xia, Z.; Han, X.; Liu, Z.; Lin, H.; Qiu, X.; Zhang, M.; Ruan, X.; Chen, X.; Jin, G.; et al. Accuracy of Intraocular Lens Calculation Formulas in Patients Undergoing Combined Phakic Intraocular Lens Removal and Cataract Surgery. Am. J. Ophthalmol. 2022, 234, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Shajari, M.; Scheffel, M.; Koss, M.J.; Kohnen, T. Dependency of endothelial cell loss on anterior chamber depth within first 4 years after implantation of iris-supported phakic intraocular lenses to treat high myopia. J. Cataract. Refract. Surg. 2016, 42, 1562–1569. [Google Scholar] [CrossRef] [PubMed]
- Ophtec, B.V. Urgent Field Safety Notice for ARTIFLEX phakic IOL, ARTIFLEX Toric Phakic IOL by Ophtec BV. Available online: https://www.bfarm.de/SharedDocs/Kundeninfos/EN/11/2021/20671-21_kundeninfo_en.html (accessed on 30 June 2023).
- Gilani, F.; Cortese, M.; Ambrósio, R.R.; Lopes, B.; Ramos, I.; Harvey, E.M.; Belin, M.W. Comprehensive anterior segment normal values generated by rotating Scheimpflug tomography. J. Cataract. Refract. Surg. 2013, 39, 1707–1712. [Google Scholar] [CrossRef]
- Niu, L.; Miao, H.; Han, T.; Ding, L.; Wang, X.; Zhou, X. Visual outcomes of Visian ICL implantation for high myopia in patients with shallow anterior chamber depth. BMC Ophthalmol. 2019, 19, 121. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Zhao, J.; Sun, L.; Zhao, J.; Niu, L.; Wang, X.; Zhou, X. Four-year observation of the changes in corneal endothelium cell density and correlated factors after Implantable Collamer Lens V4c implantation. Br. J. Ophthalmol. 2021, 105, 625–630. [Google Scholar] [CrossRef]
- Qian, T.; Du, J.; Ren, R.; Zhou, H.; Li, H.; Zhang, Z.; Xu, X. Vault-correlated efficacy and safety of Implantable Collamer Lens V4c implantation for myopia in patients with shallow anterior chamber depth. Ophthalmic. Res. 2023, 66, 445. [Google Scholar] [CrossRef] [PubMed]
- Richdale, K.; Bullimore, M.A.; Zadnik, K. Lens thickness with age and accommodation by optical coherence tomography. Ophthalmic. Physiol. Opt. 2008, 28, 441–447. [Google Scholar] [CrossRef]
- Gimbel, H.V.; LeClair, B.M.; Jabo, B.; Marzouk, H. Incidence of implantable Collamer lens-induced cataract. Can J. Ophthalmol. 2018, 53, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, A.; Kamiya, K.; Ichikawa, K.; Kitazawa, Y.; Kojima, T.; Nakamura, T.; Shimizu, K. Multicenter clinical outcomes of hole implantable collamer lens implantation in middle-aged patients. Sci. Rep. 2022, 12, 4236. [Google Scholar] [CrossRef]
- Lackner, B.; Pieh, S.; Schmidinger, G.; Simader, C.; Franz, C.; Dejaco-Ruhswurm, I.; Skorpik, C. Long-term results of implantation of phakic posterior chamber intraocular lenses. J. Cataract. Refract. Surg. 2004, 30, 2269–2276. [Google Scholar] [CrossRef]
- Sanders, D.R. Anterior subcapsular opacities and cataracts 5 years after surgery in the visian implantable collamer lens FDA trial. J. Refract. Surg. 2008, 24, 566–570. [Google Scholar]
- Sanders, D.R.; Vukich, J.A. Incidence of lens opacities and clinically significant cataracts with the implantable contact lens: Comparison of two lens designs. J. Refract. Surg. 2002, 18, 673–682. [Google Scholar] [CrossRef]
- Yang, W.; Zhao, J.; Zhao, J.; Shen, Y.; Niu, L.A.; Ruma, A.; Wang, X.; Zhou, X. Changes in anterior lens density after Implantable Collamer Lens V4c implantation: A 4-year prospective observational study. Acta Ophthalmol. 2021, 99, 326–333. [Google Scholar] [CrossRef]
- Ye, Y.; Zhao, J.; Niu, L.; Shi, W.; Wang, X.; Zhou, X. Long-term evaluation of anterior lens density after implantable collamer lens V4c implantation in patients with myopia over 40 years old. Br. J. Ophthalmol. 2022, 106, 1508–1513. [Google Scholar] [CrossRef] [PubMed]
- Utine, C.A.; Bayraktar, S.; Kaya, V.; Eren, H.; Perente, I.; Kucuksumer, Y.; Kevser, M.A.; Yilmaz, O.F. ZB5M Anterior Chamber and Fyodorov’s Posterior Chamber Phakic Intraocular Lenses: Long-Term Follow-Up; Slack Incorporated Thorofare: West Deptford, NJ, USA, 2006; pp. 906–910. [Google Scholar]
- Baikoff, G.; Lutun, E.; Wei, J.; Ferraz, C. Contact between 3 phakic intraocular lens models and the crystalline lens: An anterior chamber optical coherence tomography study. J. Cataract. Refract. Surg. 2004, 30, 2007–2012. [Google Scholar] [CrossRef] [PubMed]
- Abulafia, A.; Barrett, G.D.; Rotenberg, M.; Kleinmann, G.; Levy, A.; Reitblat, O.; Koch, D.D.; Wang, L.; Assia, E.I. Intraocular lens power calculation for eyes with an axial length greater than 26.0 mm: Comparison of formulas and methods. J. Cataract. Refract. Surg. 2015, 41, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Jiang, W.; Lin, T.; Wu, X.; Lin, H.; Chen, W. Meta-analysis of accuracy of intraocular lens power calculation formulas in short eyes. Clin. Exp. Ophthalmol. 2018, 46, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Khoramnia, R.; Auffarth, G.; Łabuz, G.; Pettit, G.; Suryakumar, R. Refractive outcomes after cataract surgery. Diagnostics 2022, 12, 243. [Google Scholar] [CrossRef] [PubMed]
- Ichhpujani, P.; Bhartiya, S.; Sharma, A. Premium IOLs in Glaucoma. J. Curr. Glaucoma. Pract. 2013, 7, 54–57. [Google Scholar] [PubMed]
- Sheu, S.-J.; Ger, L.-P.; Ho, W.-L. Late increased risk of retinal detachment after cataract extraction. Am. J. Ophthalmol. 2010, 149, 113–119.e1. [Google Scholar] [CrossRef] [PubMed]
- Daien, V.; Le Pape, A.; Heve, D.; Carriere, I.; Villain, M. Incidence, risk factors, and impact of age on retinal detachment after cataract surgery in France: A national population study. Ophthalmology 2015, 122, 2179–2185. [Google Scholar] [CrossRef]
- Colin, J.; Robinet, A.; Cochener, B. Retinal detachment after clear lens extraction for high myopia: Seven-year follow-up. Ophthalmology 1999, 106, 2281–2284; discussion 5. [Google Scholar] [CrossRef]
- Poulsen, C.D.; Green, A.; Grauslund, J.; Peto, T. Long-term outcome of patients operated with pars plana vitrectomy for primary rhegmatogenous retinal detachment. Ophthalmic Res. 2020, 63, 25–33. [Google Scholar] [CrossRef]
- Lackner, B.; Pieh, S.; Schmidinger, G.; Hanselmayer, G.; Dejaco-Ruhswurm, I.; Funovics, M.A.; Skorpik, C. Outcome after treatment of ametropia with implantable contact lenses. Ophthalmology 2003, 110, 2153–2161. [Google Scholar] [CrossRef]
- Arne, J.L.; Lesueur, L.C. Phakic posterior chamber lenses for high myopia: Functional and anatomical outcomes. J. Cataract. Refract. Surg. 2000, 26, 369–374. [Google Scholar] [CrossRef]
- Kamiya, K.; Shimizu, K.; Igarashi, A.; Hikita, F.; Komatsu, M. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch. Ophthalmol. 2009, 127, 845–850. [Google Scholar]
- Schmidinger, G.; Lackner, B.; Pieh, S.; Skorpik, C. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology 2010, 117, 1506–1511. [Google Scholar] [CrossRef]
- McLeod, S.D. Long-term Clinical Outcomes and Cataract Formation Rates After Posterior Phakic Lens Implantation for Myopia. JAMA Ophthalmol. 2016, 134, 494–495. [Google Scholar] [CrossRef] [PubMed]
- Wannapanich, T.; Kasetsuwan, N.; Reinprayoon, U. Intraocular Implantable Collamer Lens with a Central Hole Implantation: Safety, Efficacy, and Patient Outcomes. Clin. Ophthalmol. 2023, 17, 969–980. [Google Scholar] [CrossRef]
- Jiménez-Alfaro, I.; Benítez del Castillo, J.M.; García-Feijoó, J.; Gil de Bernabé, J.G.; Serrano de La Iglesia, J.M. Safety of posterior chamber phakic intraocular lenses for the correction of high myopia: Anterior segment changes after posterior chamber phakic intraocular lens implantation. Ophthalmology 2001, 108, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, J.F.; Fernández-Vega, L.; Lisa, C.; Fernandes, P.; Jorge, J.; Micó, R.M. Central vault after phakic intraocular lens implantation: Correlation with anterior chamber depth, white-to-white distance, spherical equivalent, and patient age. J. Cataract. Refract. Surg. 2012, 38, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Chen, X.; Cheng, M.; Lei, Y.; Jiang, Y.; Xu, Y.; Wang, X.; Zhou, X. Long-Term Vault Changes in Different Levels and Factors Affecting Vault Change After Implantation of Implantable Collamer Lens with a Central Hole. Ophthalmol. Ther. 2023, 12, 251–261. [Google Scholar] [CrossRef]
- McCaughey, M.V.; Mifflin, T.; Fenzl, C.R.; Goldsmith, J.; Moshirfar, M. Pseudophacomorphic Glaucoma along with Pupillary Block after Visian™ Implantable Collamer Lens Implantation for High Myopia. Open J. Ophthalmol. 2014, 4, 107–111. [Google Scholar] [CrossRef][Green Version]
- Vetter, J.M.; Tehrani, M.; Dick, H.B. Surgical management of acute angle-closure glaucoma after toric implantable contact lens implantation. J. Cataract. Refract. Surg. 2006, 32, 1065–1067. [Google Scholar] [CrossRef]
- Senthil, S.; Choudhari, N.S.; Vaddavalli, P.K.; Murthy, S.; Reddy, J.C.; Garudadri, C.S. Etiology and Management of Raised Intraocular Pressure following Posterior Chamber Phakic Intraocular Lens Implantation in Myopic Eyes. PLoS ONE 2016, 11, e0165469. [Google Scholar] [CrossRef]
- Ye, C.; Patel, C.K.; Momont, A.C.; Liu, Y. Advanced pigment dispersion glaucoma secondary to phakic intraocular collamer lens implant. Am. J. Ophthalmol. Case Rep. 2018, 10, 65–67. [Google Scholar] [CrossRef]
- Hu, Z.; Chen, C.; Sun, M.; Yuan, R.; Ye, J. The Relationship between Anterior Chamber Angle and Intraocular Pressure Early after V4c Implantable Collamer Lens Implantation. J. Ophthalmol. 2020, 2020, 4014512. [Google Scholar] [CrossRef]
- Montés-Micó, R.; Ruiz-Mesa, R.; Rodríguez-Prats, J.L.; Tañá-Rivero, P. Posterior-chamber phakic implantable collamer lenses with a central port: A review. Acta Ophthalmol. 2021, 99, e288–e301. [Google Scholar] [CrossRef]
- Aguilar-Valenzuela, L.; Lleó-Pérez, A.; Alonso-Muñoz, L.; Casanova-Izquierdo, J.; Pérez-Moltó, F.J.; Rahhal, M.S. Intraocular pressure in myopic patients after Worst-Fechner anterior chamber phakic intraocular lens implantation. J. Refract. Surg. 2003, 19, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Alió, J.L.; de la Hoz, F.; Pérez-Santonja, J.J.; Ruiz-Moreno, J.M.; Quesada, J.A. Phakic anterior chamber lenses for the correction of myopia: A 7-year cumulative analysis of complications in 263 cases. Ophthalmology 1999, 106, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Bowd, C.; Zangwill, L.M.; Berry, C.C.; Blumenthal, E.Z.; Vasile, C.; Sanchez-Galeana, C.; Bosworth, C.F.; Sample, P.; Weinreb, R.N. Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1993–2003. [Google Scholar]
- Wan, T.; Yin, H.; Yang, Y.; Wu, F.; Wu, Z.; Yang, Y. Comparative study of anterior segment measurements using 3 different instruments in myopic patients after ICL implantation. BMC Ophthalmol. 2019, 19, 182. [Google Scholar] [CrossRef]
- Scharf, D.; Yildirim, T.M.; Auffarth, G.U.; Mayer, C.S.; Choi, C.Y.; Khoramnia, R. Implantation einer phaken Hinterkammerlinse bei Keratokonus [Implantation of a Phakic Posterior Chamber Lens in Eyes with Keratoconus]. Klin. Monbl. Augenheilkd. 2020, 237, 1102–1106. (In German) [Google Scholar]
- Almorín-Fernández-Vigo, I.; Sánchez-Guillén, I.; Fernández-Vigo, J.I.; De-Pablo-Gómez-de-Liaño, L.; Kudsieh, B.; Fernández-Vigo, J.; Merino, A. Agreement between optical coherence and Scheimpflug tomography: Vault measurements and reproducibility after implantable collamer lens implantation. J. Fr. Ophtalmol. 2021, 44, 1370–1380. [Google Scholar] [CrossRef]
- Alfonso, J.F.; Lisa, C.; Palacios, A.; Fernandes, P.; González-Méijome, J.M.; Montés-Micó, R. Objective vs. subjective vault measurement after myopic implantable collamer lens implantation. Am. J. Ophthalmol. 2009, 147, 978–983.e1. [Google Scholar] [CrossRef]
- Du, C.; Wang, J.; Wang, X.; Dong, Y.; Gu, Y.; Shen, Y. Ultrasound biomicroscopy of anterior segment accommodative changes with posterior chamber phakic intraocular lens in high myopia. Ophthalmology 2012, 119, 99–105. [Google Scholar] [CrossRef]
- Lee, H.; Kang, S.Y.; Seo, K.Y.; Chung, B.; Choi, J.Y.; Kim, K.S.; Kim, T.-I. Dynamic vaulting changes in V4c versus V4 posterior chamber phakic lenses under differing lighting conditions. Am. J. Ophthalmol. 2014, 158, 1199–1204.e1. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Shimizu, K.; Igarashi, A. Vault Changes Caused by Light-Induced Pupil Constriction and Accommodation in Eyes with an Implantable Collamer Lens. Cornea 2019, 38, 217–220. [Google Scholar] [CrossRef]
- Zaldívar, R.; Adamek, P.; Zaldívar, R.; Domínguez, M.S.; Cerviño, A. Intraoperative Versus Postoperative Vault Measurement After Implantable Collamer Lens Implantation in a Large Cohort of Patients. J. Refract. Surg. 2021, 37, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Matarazzo, F.; Day, A.C.; Fernandez-Vega Cueto, L.; Maurino, V. Vertical implantable collamer lens (ICL) rotation for the management of high vault due to lens oversizing. Int. Ophthalmol. 2018, 38, 2689–2692. [Google Scholar] [CrossRef] [PubMed]
- Zaldivar, R.; Zaldivar, R.; Adamek, P.; Cerviño, A. Intraoperative adjustment of implantable collamer lens vault by lens rotation aided by intraoperative OCT. J. Cataract. Refract. Surg. 2022, 48, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, K.; Shimizu, K.; Takahashi, M.; Ando, W.; Hayakawa, H.; Shoji, N. Eight-Year Outcomes of Implantation of Posterior Chamber Phakic Intraocular Lens with a Central Port for Moderate to High Ametropia. Front. Med. 2021, 8, 799078. [Google Scholar] [CrossRef]
- Kamiya, K.; Ryu, I.H.; Yoo, T.K.; Kim, J.S.; Lee, I.S.; Kim, J.K.; Ando, W.; Shoji, N.; Yamauchi, T.; Tabuchi, H. Prediction of Phakic Intraocular Lens Vault Using Machine Learning of Anterior Segment Optical Coherence Tomography Metrics. Am. J. Ophthalmol. 2021, 226, 90–99. [Google Scholar] [CrossRef]
- Trancón, A.S.; Manito, S.C.; Sierra, O.T.; Baptista, A.M.; Serra, P.M. Determining vault size in implantable collamer lenses: Preoperative anatomy and lens parameters. J. Cataract. Refract. Surg. 2020, 46, 728–736. [Google Scholar] [CrossRef]
- Cerpa Manito, S.; Sánchez Trancón, A.; Torrado Sierra, O.; Baptista, A.M.; Serra, P.M. Biometric and ICL-related risk factors associated to sub-optimal vaults in eyes implanted with implantable collamer lenses. Eye Vis. 2021, 8, 26. [Google Scholar] [CrossRef]
- Kojima, T.; Yokoyama, S.; Ito, M.; Horai, R.; Hara, S.; Nakamura, T.; Ichikawa, K. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am. J. Ophthalmol. 2012, 153, 632–637.e1. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Archer, T.J.; Vida, R.S.; Piparia, V.; Potter, J.G. New Sizing Parameters and Model for Predicting Postoperative Vault for the Implantable Collamer Lens Posterior Chamber Phakic Intraocular Lens. J. Refract. Surg. 2022, 38, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Lovisolo, C.F.; Archer, T.J.; Gobbe, M. Comparison of postoperative vault height predictability using white-to-white or sulcus diameter-based sizing for the visian implantable collamer lens. J. Refract. Surg. 2013, 29, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Han, T.; Zhao, W.; Wang, X.; Xu, Y.; Cheng, M.; Wang, X.; Zhou, X. Effect of the Difference Between the White-to-White and Sulcus-to-Sulcus on Vault and the Related Factors After ICL Implantation. Ophthalmol. Ther. 2021, 10, 947–955. [Google Scholar] [CrossRef]
- Chen, Q.; Tan, W.; Lei, X.; Pan, C.; Jin, L.; Zeng, Q.; Wang, Z. Clinical Prediction of Excessive Vault After Implantable Collamer Lens Implantation Using Ciliary Body Morphology. J. Refract. Surg. 2020, 36, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, P.J.; Rivera, R.P.; Schneider, D.; Lane, S.S.; Brown, D.; Vukich, J. Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J. Cataract. Refract. Surg. 2011, 37, 13–18. [Google Scholar] [CrossRef]
- Di, Y.; Li, Y.; Luo, Y. Prediction of Implantable Collamer Lens Vault Based on Preoperative Biometric Factors and Lens Parameters. J. Refract. Surg. 2023, 39, 332–339. [Google Scholar] [CrossRef]
- Igarashi, A.; Shimizu, K.; Kato, S. Assessment of the Vault After Implantable Collamer Lens Implantation Using the KS Formula. J. Refract. Surg. 2021, 37, 636–641. [Google Scholar] [CrossRef]
- Nakamura, T.; Isogai, N.; Kojima, T.; Yoshida, Y.; Sugiyama, Y. Optimization of implantable collamer lens sizing based on swept-source anterior segment optical coherence tomography. J. Cataract. Refract. Surg. 2020, 46, 742–748. [Google Scholar] [CrossRef]
- Oleszko, A.; Marek, J.; Muzyka-Wozniak, M. Application of a Partial Least Squares Regression Algorithm for Posterior Chamber Phakic Intraocular Lens Sizing and Postoperative Vault Prediction. J. Refract. Surg. 2020, 36, 606–612. [Google Scholar] [CrossRef]
- Rocamora, L.; Orlando, J.I.; Lwowski, C.; Kohnen, T.; Mertens, E.; Van Keer, K. Postoperative vault prediction for phakic implantable collamer lens surgery: LASSO formulas. J. Cataract. Refract. Surg. 2023, 49, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Malyugin, B.E.; Shpak, A.A.; Pokrovskiy, D.F. Posterior chamber phakic intraocular lens sizing based on iris pigment layer measurements by anterior segment optical coherence tomography. J. Cataract. Refract. Surg. 2015, 41, 1616–1622. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, A.; Shimizu, K.; Kato, S.; Kamiya, K. Predictability of the vault after posterior chamber phakic intraocular lens implantation using anterior segment optical coherence tomography. J. Cataract. Refract. Surg. 2019, 45, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Wang, L.; Jian, W.; Shang, J.; Wang, X.; Ju, L.; Li, M.; Zhao, J.; Chen, X.; Ge, Z.; et al. Big-data and artificial-intelligence-assisted vault prediction and EVO-ICL size selection for myopia correction. Br. J. Ophthalmol. 2023, 107, 201–206. [Google Scholar] [CrossRef]






| Study | Year | pIOL Model | Number of Eyes | Mean ± SD Preoperative ECD (cells/mm2) | ECD at 1 Year Postoperatively (cells/mm2) | ECD at 5 Years Postoperatively (cells/mm2) | ECD at 10 Years Postoperatively (cells/mm2) |
|---|---|---|---|---|---|---|---|
| Anterior chamber iris-fixated phakic intraocular lenses | |||||||
| Benedetti et al. [16] | 2007 | Artisan | 49 | 2616 (median value) | 2523 (median value) | 2379 (median value) | - |
| Bouheraoua et al. [59] | 2015 | Artisan | 68 | 2629 ± 366 | 2464 ± 334 | 2250 ± 454 | - |
| Castro de Luna et al. [14] | 2019 | Artiflex | 53 | 3107 ± 428 | 3028 ± 436 | 2867 ± 460 | 2673 ± 453 (n = 18) |
| Eldanasoury et al. [17] | 2019 | Artisan, Artiflex | 90 | 2645 ± 200 | - | - | Approx. 12 years: 1751 ± 730 |
| Güell et al. [18] | 2008 | Artisan | Group 1: Artisan Myopia Model 204, n = 101. Group 2: Artisan Myopia Model 206, n = 173. Group 3: Artisan Hyperopia Model 203, n = 41. Group 4: Artisan Toric, n = 84. | Group 1: 2836 ± 398 Group 2: 2755 ± 362 Group 3: 2735 ± 355 Group 4: 2632 ± 543 | Group 1: 2598 ± 350 Group 2: 2643 ± 414 Group 3: 2600 ± 442 Group 4: 2673 ± 439 | Group 1: 2514 ± 529 Group 2: 2454 ± 588 No data from groups 3 and 4 | - |
| Jonker et al. [20] | 2018 | Artiflex | Artiflex Myopia: n = 293 Artiflex Toric: n = 188 | Artiflex Myopia: 2739 ± 286 Artiflex Toric: 2769 ± 370 | Artiflex Myopia: 2657 ± 352 (n = 202) Artiflex Toric: 2669 ± 426 (n = 131) | Artiflex Myopia: 2480 ± 369 (n = 137) Artiflex Toric: 2488 ± 360 (n = 63) | - |
| Jonker et al. [19] | 2018 | Artisan | 507 | Artisan Myopia: 2670 ± 365, n = 381 Artisan Toric: 2695 ± 359, n = 126 | - | Artisan Myopia: 2588 ± 425, n = 193 Artisan Toric: 2270 ± 406, n = 40 | Artisan Myopia: 2302 ± 451, n = 127 Artisan Toric: 2009 ± 475, n = 20 |
| Kwitko et al. [12] | 2021 | Artisan, Artiflex | 195 | Myopia: 2515 ± 371 Hyperopia: 2556 ± 457 | - | - | Approx. 7 years: Myopia: 2377 ± 353 Hyperopia: 2436 ± 190 |
| Marta et al. [82] | 2022 | Artiflex | 217 | 2849 ± 393 | - | 2693 ± 446 | 15 years: 2113 ± 446 |
| Morral et al. [79] | 2016 | Artisan, Artiflex | 58 in total (2 study groups of equal size, with both lens models analyzed together) | 2836 ± 379 and 2759 ± 365 | 2827 ± 234 and 2845 ± 438 | 2723 ± 278 and 2649 ± 398 | 2654 ± 409 and 2543 ± 419 |
| Nemcova et al. [24] | 2021 | Verisyse, Veriflex | 85 | 2588 ± 285 | 2430 ± 312 | 2175 ± 298 | 12 years: 2091 ± 312 |
| Papa-Vettorazzi et al. [28] | 2022 | Artiflex | 76 | 2935 ± 359 | 2818 ± 350 | - | Approx. 11 years: 2620 ± 453 |
| Saxena et al. [64] | 2008 | Artiflex | 318 | 2817 ± 356 | 2813 ± 426, n = 251 | 2581 ± 293, n = 51 | 7 years: 2451 ± 256, n = 13 |
| Tahzib et al. [80] | 2007 | Artisan | 89 | 2817 ± 359 | 2928 ± 351 | - | 2800 ± 292 |
| Yaşa and Ağca [81] | 2018 | Verisyse, Veriflex | Verisyse: n = 47 Veriflex n = 50 | Verisyse: 2681 ± 275 Veriflex: 2656 ± 270 | Verisyse: 2599 ± 242 Veriflex: 2575 ± 253 | Verisyse: 2482 ± 242 Veriflex: 2460 ± 282 | - |
| Yildirim et al. [83] | 2021 | Artiflex | 52 | 2712 ± 272 | 2610 | 2440 | 6 years: 2411 ± 281 |
| Implantable Collamer lenses | |||||||
| Alfonso et al. [58] | 2011 | V4 | 188 (5-year data: n = 50) | 2695 ± 467 | - | 2495 ± 357 (n = 50) | - |
| Alfonso et al. [15] | 2019 | V4c | 146 | 2657 ± 362 | 2696 ± 358 | 2645 ± 359 | - |
| Choi et al. [70] | 2019 | V4 | 110 | 2889 ± 239 | 2893 ± 303 | - | 2749 ± 300 (n = 71) |
| Guber et al. [72] | 2016 | V4 | 133 | 2300 (median value) | 2300 (median value), n = 100 | 2200 (median value), n = 106 | 2393 (median value), n = 75 |
| Igarashi et al. [73] | 2014 | V4 | 41 | 2819 ± 295 | 2756 ± 337 | - | 8 years: 2626 ± 207 |
| Lee et al. [74] | 2016 | V4 | 281 | 2898 ± 404 | 2835 ± 337 | 2726 ± 227 | 7 years: 2712 ± 369 |
| Moya et al. [61] | 2015 | V3, V4 | 144 | 2587 ± 320, n = 85 | 2434 ± 290, n = 73 | - | 12 years: 2071 ± 362, n = 104 |
| Nakamura et al. [75] | 2019 | V4 | 114 | 2740 ± 362 | 2766 ± 339 | 2725 ± 298 | 2581 ± 345 |
| Papa-Vettorazzi et al. [62] | 2022 | V4b | 45 | 2930 ± 441 | 2943 ± 475 | - | Approx. 11 years: 2731 ± 623 |
| Pesando et al. [77] | 2007 | V1, V2, V3, V4 | 59 | 2696 ± 298 | - | - | 2437 ± 243 |
| Study | Year | pIOL Model | Follow-Up (Years) | Number of Eyes (n) | Mean ± SD Anterior Chamber Depth * | Yearly Chronic Endothelial Cell Loss + | Endothelial Cell Loss at 5 Years Postoperatively + | Endothelial Cell Loss at 10 Years Postoperatively + | Endothelial Cell Loss of 25% or More |
|---|---|---|---|---|---|---|---|---|---|
| Minimum preoperative anterior chamber depth lower than 3.0 mm * | |||||||||
| Jonker et al. [20] | 2018 | Artiflex | 5 | Artiflex Myopia: n = 293 Artiflex Toric: n = 188 | Artiflex Myopia: approx. 2.73 mm (3.27 ± 0.31 mm, measured from the epithelium) Artiflex Toric: approx. 2.70 mm (3.24 ± 0.35 mm, measured from the epithelium) | Artiflex Myopia: approx. 2.3% Artiflex Toric: approx. 2.2% | In comparison with 6-month data: Artiflex Myopia: 10.5%, n = 137 Artiflex Toric: 10.2%, n = 63 | n/a | Artiflex Myopia: 5 years—4.4% Artiflex Toric: 5 years—4.3% |
| Bouheraoua et al. [59] | 2015 | Artisan | 5 | 68 | Approx. 2.90 mm (3.44 ± 0.41 mm, measured from the epithelium) | 1.7% | 15.2% | n/a | n/a |
| Eldanasoury et al. [17] | 2019 | Artisan, Artiflex | 9–17 | 90 | 2.91 ± 0.33 mm | 2.3% | n/a | Mean follow-up of 12 years: 26.7 ± 27.6% | n/a (an explantation rate of 26% due to endothelial cell loss) |
| Jonker et al. [19] | 2018 | Artisan | 10 | 507 | Artisan Myopia: approx. 3.14 mm (3.68 ± 0.34 mm, measured from the epithelium) Artisan Toric: approx. 2.95 mm (3.49 ± 0.35 mm, measured from the epithelium) | Artisan Myopia: approx. 1.8% Artisan Toric: approx. 2.3% | Artisan Myopia: 4.1%, n = 193 Artisan Toric: 11.9%, n = 40 | Artisan Myopia: 11.5%, n = 127 Artisan Toric: 18.5%, n = 20 | Artisan Myopia: 5 years—1.8% 10 years—7.9% Artisan Toric: 5 years—3.2% 10 years—6.3% |
| Saxena et al. [64] | 2008 | Artiflex | ≤7 | 318 | Approx. 3.16 mm (3.70 ± 0.30 mm, measured from the epithelium) | n/a | 8.3%, n = 5 | n/a | n/a |
| Papa-Vettorazzi et al. [28] | 2022 | Artiflex | ≥10 | 76 | 3.21 ± 0.26 mm | 1.0% | n/a | In comparison with 1-year data: 8.9 ± 11.9% | n/a |
| Marta et al. [82] | 2022 | Artiflex | ≤15 | 217 | 3.25 ± 0.26 mm | 1.0–1.7% | Artiflex Myopia: 7.1 ± 15.6% Artiflex Toric: 1.3 ± 13.8% | Artiflex Myopia: 17.3 ± 16.4% Artiflex Toric: 16.5 ± 12.8% | 5 years—7.2% 10 years—24.3% 15 years—35.1% |
| Monteiro et al. [22] | 2021 | Artiflex | 6 | 177 | 3.26 ± 0.24 mm | Approx. 1.2% | 6-year data, in comparison with 1-year data: 6.0% | n/a | n/a |
| Royo et al. [63] | 2022 | Artiflex | 8 | Artiflex Myopia: n = 47 Artiflex Toric: n = 20 | Artiflex Myopia: 3.35 ± 0.23 mm Artiflex Toric: 3.19 ± 0.21 mm | n/a | Artiflex Myopia: 5.3%, n = 36 Artiflex Toric: 6.7%, n = 13 | n/a | 0% |
| Nemcova et al. [24] | 2021 | Verisyse, Veriflex | 12 | 85 | 3.30 ± 0.23 mm | n/a | 15.8% | 12-year data: 19.1% | 5 years—15% 12 years—20% |
| Güell et al. [18] | 2008 | Artisan | 5 | Artisan Myopia: n = 274; Artisan Hyperopia n = 41; Artisan Toric, n = 84. | n/a | n/a | 10.9–11.3% Artisan Hyperopia/Toric: n/a | n/a | n/a |
| Morral et al. [79] | 2016 | Artisan, Artiflex | 10 | Group 1 *: n = 29 Group 2 *: n = 29 | n/a | n/a | Group 1: 4.0 ± 6.3% Group 2: 4.0 ± 5.3% | Group 1: 6.4 ± 8.0% Group 2: 7.8 ± 6.8% | n/a |
| Minimum preoperative anterior chamber depth of 3.0 mm or higher * | |||||||||
| Yaşa and Ağca [81] | 2018 | Verisyse, Veriflex | 5 | Verisyse: n = 47 Veriflex n = 50 | Verisyse: 3.27 ± 0.21 mm Veriflex: 3.32 ± 0.26 mm | Verisyse: 1.0–1.2% Veriflex: 1.1–1.2% | Verisyse: 7.4% Veriflex: 7.6% | n/a | 0% |
| Chebli et al. [60] | 2018 | Artisan | 5.4 ± 3.0 | 113 | 3.42 ± 0.26 mm | 0.9% | n/a | 12.1% (n = 16) | n/a |
| Yildirim et al. [83] | 2021 | Artiflex | 6 | 52 | n/a | n/a | 6-year data: 11.1%, n = 42 | n/a | 0% |
| Kwitko et al. [12] | 2021 | Artisan, Artiflex | 1–17 | 195 | n/a | Myopia: 0.8% Hyperopia: no statistically significant loss | Mean follow-up of 7 years: Myopia: 5.5%. Hyperopia: no statistically significant loss. | n/a | n/a |
| Study | Year | Number of Patients and Eyes | ICL Model | The Actual ICL-Sizing Method Used in the Surgeries | Formula Development Method | Parameters Used in Calculation | Diagnostic Modalities Used to Obtain the Parameters Used in the Final Formula | Main Results |
|---|---|---|---|---|---|---|---|---|
| Dougherty et al. [160] | 2010 | 73 eyes of 48 patients (nomogram development) | ICL * | ICL size according to UBM measurements | Multiple regression analysis | STS, ICL power | High-frequency UBM VuMax-II (Sonomed, Inc.) | Mean ±SD vault: 340 ± 174 µm (range 90–952 µm); vault between 100 µm and 700 µm in 93.1% of eyes. |
| Kojima et al. [155] | 2012 | Development dataset: 47 eyes of 25 patients in development Validation dataset: 81 eyes of 43 patients | ICL * | Manufacturer’s nomogram in the development stage and the developed formula in the validation stage | Stepwise multiple regression analysis | ACD, STS, STSL | ACD obtained using IOL Master (Carl Zeiss Meditec), STS and STSL obtained using high-frequency UBM VuMax-II | Mean ± SD prediction error: 60 ± 290 µm +; vault between 150 µm and 1000 µm in 88.9% of eyes; vault between 250 µm and 750 µm in 74.1% of eyes; no eyes with a vault of <150 µm and 11.1% with a vault of >1000 µm. |
| Malyugin et al. [166] | 2015 | 29 eyes of 16 patients (sizing evaluation) | ICL * | Distance from iris pigment end to iris pigment end | ICL size selected according to the distance from iris pigment end to iris pigment end | Iris pigment end to iris pigment end | AS-OCT Visante (Carl Zeiss Meditec) | Mean ±SD vault: 0.53 ± 0.18 mm (range 0.24–0.84 mm); 55.2% had a vault of 0.35 to 0.70 mm; 20.1% had a vault of 0.24 to 0.34 mm. |
| Oleszko et al. [164] | 2020 | 81 eyes of 43 patients | V4c | Manufacturer’s nomogram | Partial least squares regression algorithm | ATA, ACD, LE, Km, LT, AL, Rm, ACV, ICL size, MRSE | ATA, ACD, lens elevation obtained with AS-OCT (Visante); Km, LT, AL obtained with SS-OCT biometer (IOLMaster 700; Carl Zeiss Meditec); Rm, ACV obtained with Scheimpflug camera (Pentacam AXL; Oculus Optikgeräte) | Mean ±SD prediction error: 2 ± 110 µm. Prediction error: within ±100 μm in 73% of eyes, within ±200 μm in 90% of eyes, within ±300 μm in 100% of eyes. |
| Nakamura et al. [163] | 2020 | 81 eyes of 41 patients for formula development; 68 eyes of 42 patients for formula validation | V4c | NK formula | Stepwise multiple regression analyses | ACW, CLR | AS-OCT CASIA2 (Tomey) | NK-formula V2: mean ± SD absolute prediction error: 201 ± 146 µm, mean ± SD achieved vault: 670 ± 223 µm (range 235 to 1293 µm), a vault of <250 µm in 1.5% of eyes, a vault of >1000 µm in 7.3% of eyes. |
| Igarashi et al. [162] | 2021 | 121 eyes of 65 patients | ICL with central port | KS formula | KS formula, based on multiple regression analysis [167] | ATA, ICL size | AS-OCT CASIA2 | Mean ±SD prediction error: 2.6 ± 184.9 µm Mean ± SD vault: 423.6 ± 183.3 μm (range 39 to 862 μm) |
| Kamiya et al. [152] | 2021 | 1745 eyes of 1745 patients | V4c and V5 | Manufacturer’s nomogram | Machine learning: 1—support vector regressor; 2—gradient boost regressor; 3—random forest regressor; 4—linear regressor. | Age, sex, sphere, cylinder, MRSE, best-corrected visual acuity, ICL model (non-toric/toric), ICL size, WTW, ACD, ATA, CLR, ACW, LV, central corneal thickness, AOD500, TIA500 | AS-OCT CASIA2 | Mean prediction error ±95% limits of agreement: 1—14.6 ± 174.4 µm; 2—0.8 ± 137.1 µm; 3—0.9 ± 134.3 µm; 4—0.1 ± 142.2 µm. Mean ± SD absolute prediction error: 1—131.4 µm; 2—103.0 µm; 3—99.6 µm; 4—107.2 µm. |
| manufacturer’s nomogram | ACD, WTW | Mean ± SD vault: 508.5 ± 188.0 µm | ||||||
| Reinstein et al. [156] | 2022 | 147 eyes in total: 42 eyes in stage 1; 36 eyes in stage 2; 69 eyes in stage 3. | V4c | Kojima nomogram [155] in stage 1; Reinstein formula v1.0 in stage 2; Reinstein formula v2.0 in stage 3. | Stepwise multivariate regression analysis | Stage 1: STS, STSL, ACD; Stages 2 and 3: ICL size, CBID, STSL, ICL power, SPD. | STS, STSL, CBID measured using very high-frequency digital ultrasound robotic scanner Artemis Insight 100 (ArcScan, Inc., Golden, CO, USA); SPD measured using the Procyon P3000 Dynamic Binocular Pupillometer (Keeler Instruments, Inc., Malvern, PA, USA); WTW, ACD measured using the MS-39 OCT (CSO). | Mean ± SD prediction error: 47 ± 124 µm Achieved vault within ±100, ±200, and ±300 μm of target: Stage 1: 33%, 50%, and 74% of eyes; Stage 2: 58%, 89%, and 100% of eyes; Stage 3: 62%, 84%, and 94% of eyes. Vault <250 or >1000 µm: Stage 1: 12% of eyes; Stage 2: 0% of eyes; Stage 3: 1% of eyes. |
| Di et al. [161] | 2023 | 300 eyes of 300 patients: 150 eyes for formula establishment and 150 eyes for validation | V4c | Manufacturer’s nomogram | Multiple linear regression analysis | ACD, ATA, ICL size | AS-OCT Visante | Mean ± SD absolute prediction error: 135.1 µm; 20.7% of eyes with mean absolute prediction error greater than 200 µm; root mean square error 157.46 µm; 95% CI −313.2 to 305.9 µm. |
| Rocamora et al. [165] | 2023 | 115 eyes of 59 patients in the training set and 37 eyes of 19 patients in the test set. | V4c | Selected at the discretion of the surgeon, guided by the manufacturer’s nomogram and the Nakamura 1 and 2 formulas | Least Absolute Shrinkage and Selection Operator (LASSO) | PD, CT, TKm, WTW, LT, ACD, posterior Km at 3 mm zone, anterior Km at 5 mm zone, CV, CLR, SS to SS distance, horizonal visible iris diameter, ICL spherical equivalent, MRSE, manifest refraction cylinder, ICL diameter, age. | PD, posterior Km at 3 mm zone, anterior Km at 5 mm zone, CV, CLR, SS to SS distance, horizonal visible iris diameter obtained using AS-OCT MS-39; CT, TKm, WTW, LT, ACD measured using optical biometer IOL Master 700. | Mean ± SD absolute prediction error: 145.6 ± 100.6 µm for AS-OCT-based model 144.1 ± 107.9 µm for optical biometer-based model 132.0 ± 86.6 µm for the combined model (AS-OCT and optical biometer parameters) Absolute prediction error <500 µm in 97.3–100% of eyes. |
| Shen et al. [168] | 2023 | 6297 eyes of 3536 patients. Data randomly divided into training set and test set (ratio of 8:2) | V4c | Selected according to the preoperative measurements by a technician | Machine learning: 1—Random Forest, 2—Gradient Boosting, 3—XGBoost. | ICL size, ACD, pupil size, ACA, CT, AL, the time after surgery, K2 value, K2 axis, K1 value, K1 axis, WTW, sphere, sphere of ICL, cylinder, cylinder of ICL, spherical equivalent of ICL, type of ICL | K1, K2, ACD, ACA, pupil size, CT WTW obtained using Pentacam HR (Oculus Optikgeräte); AL measured using IOL Master. | Accuracy (95% CI) of achieving a normal vault, defined as 250–750 µm: 1—0.828 (0.819 to 0.836); 2—0.815 (0.809 to 0.821); 3—0.802 (0.791 to 0.813). RMSE (95% CI): 1—159.026 (155.988 to 162.065); 2—161.862 (158.963 to 164.761); 3—162.527 (159.163 to 165.890). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naujokaitis, T.; Auffarth, G.U.; Łabuz, G.; Kessler, L.J.; Khoramnia, R. Diagnostic Techniques to Increase the Safety of Phakic Intraocular Lenses. Diagnostics 2023, 13, 2503. https://doi.org/10.3390/diagnostics13152503
Naujokaitis T, Auffarth GU, Łabuz G, Kessler LJ, Khoramnia R. Diagnostic Techniques to Increase the Safety of Phakic Intraocular Lenses. Diagnostics. 2023; 13(15):2503. https://doi.org/10.3390/diagnostics13152503
Chicago/Turabian StyleNaujokaitis, Tadas, Gerd U. Auffarth, Grzegorz Łabuz, Lucy Joanne Kessler, and Ramin Khoramnia. 2023. "Diagnostic Techniques to Increase the Safety of Phakic Intraocular Lenses" Diagnostics 13, no. 15: 2503. https://doi.org/10.3390/diagnostics13152503
APA StyleNaujokaitis, T., Auffarth, G. U., Łabuz, G., Kessler, L. J., & Khoramnia, R. (2023). Diagnostic Techniques to Increase the Safety of Phakic Intraocular Lenses. Diagnostics, 13(15), 2503. https://doi.org/10.3390/diagnostics13152503








