Diagnostic Value of Dynamic 18F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography (18F-FDG PET-CT) in Cervical Lymph Node Metastasis of Nasopharyngeal Cancer
Abstract
:1. Introduction
2. Material and Method
2.1. Patients
2.2. Data Acquisition and Image Reconstruction
2.3. Delineation of VOIs
2.4. Efficacy Evaluation
2.5. Data Analysis
3. Result
3.1. Patients
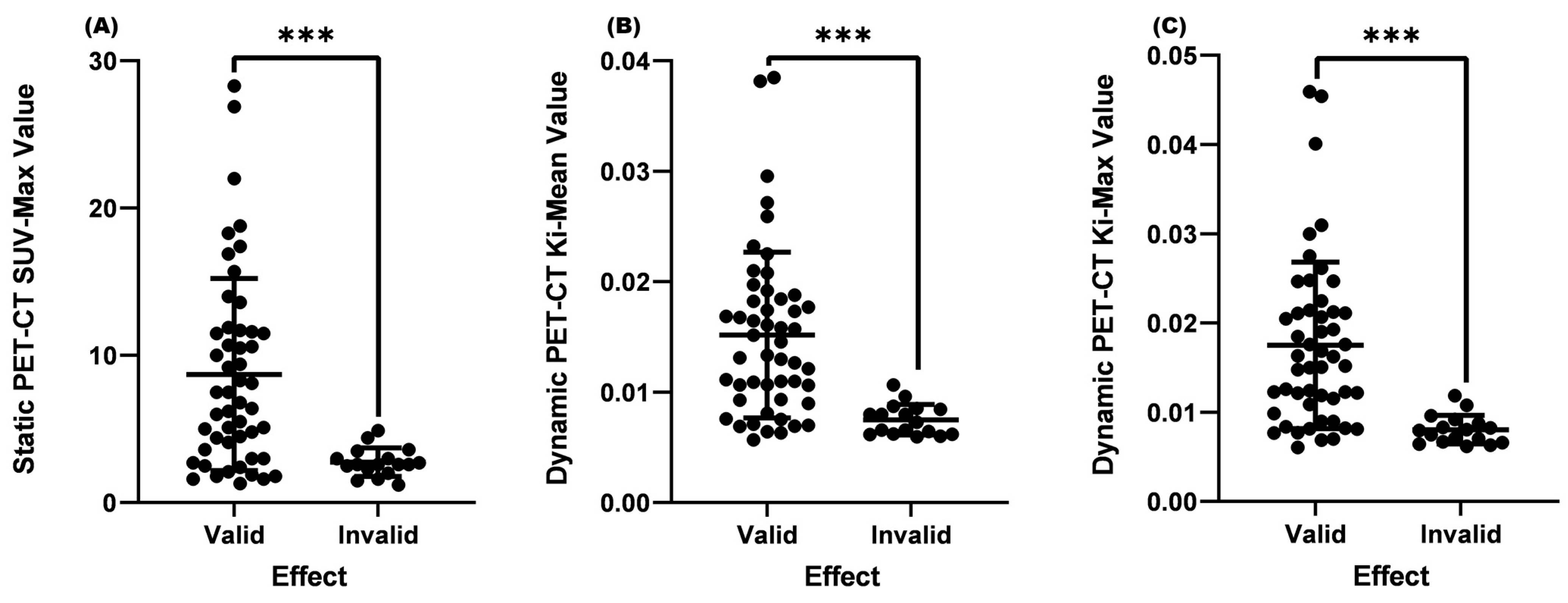
3.2. Comparison of SUVmax, Ki-Mean, and Ki-Max Values between the Valid and Invalid Groups
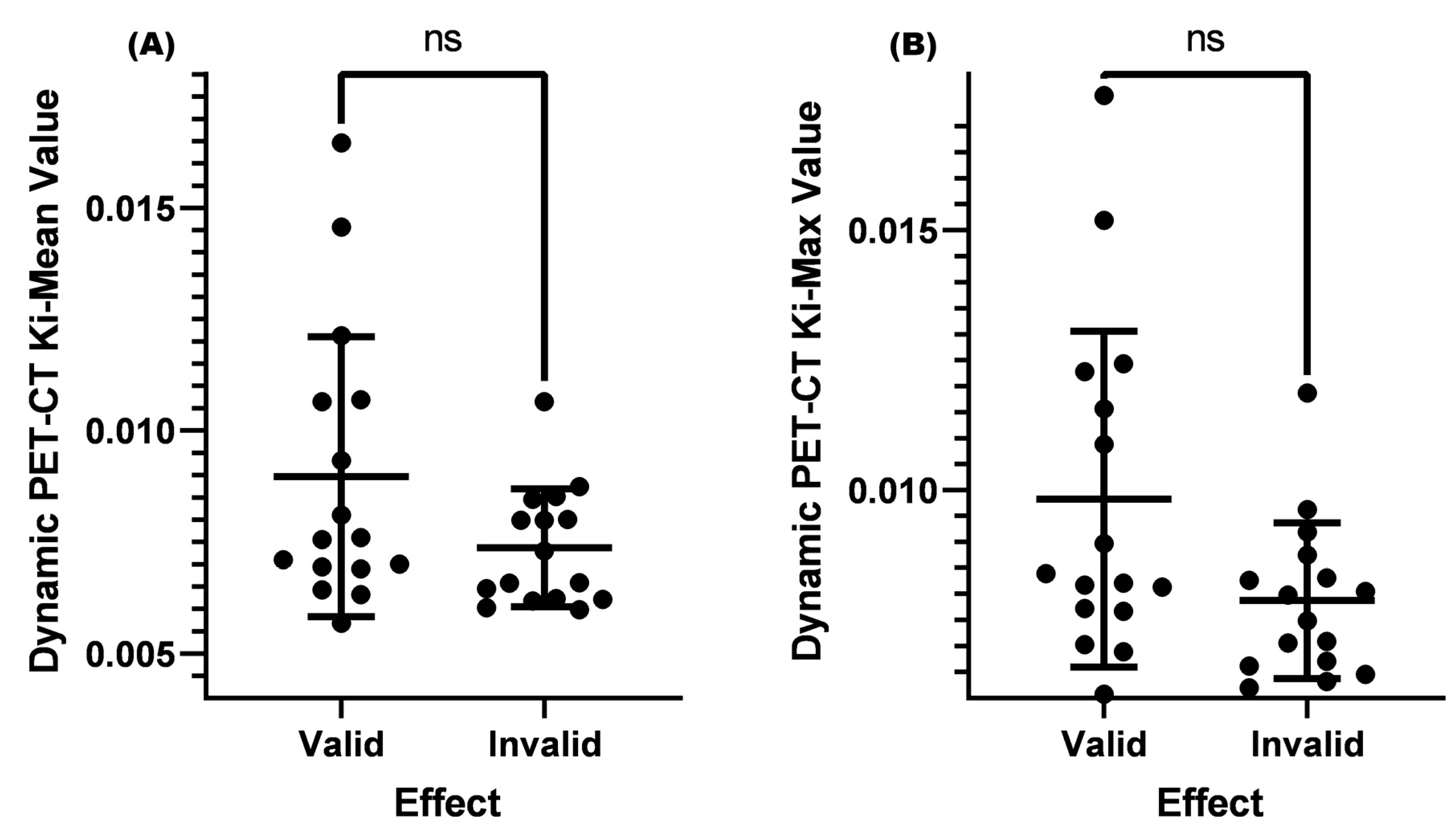
3.3. Comparison of Ki-Mean and Ki-Max Values between Valid and Invalid Groups When SUV-Max ≤ 4.5
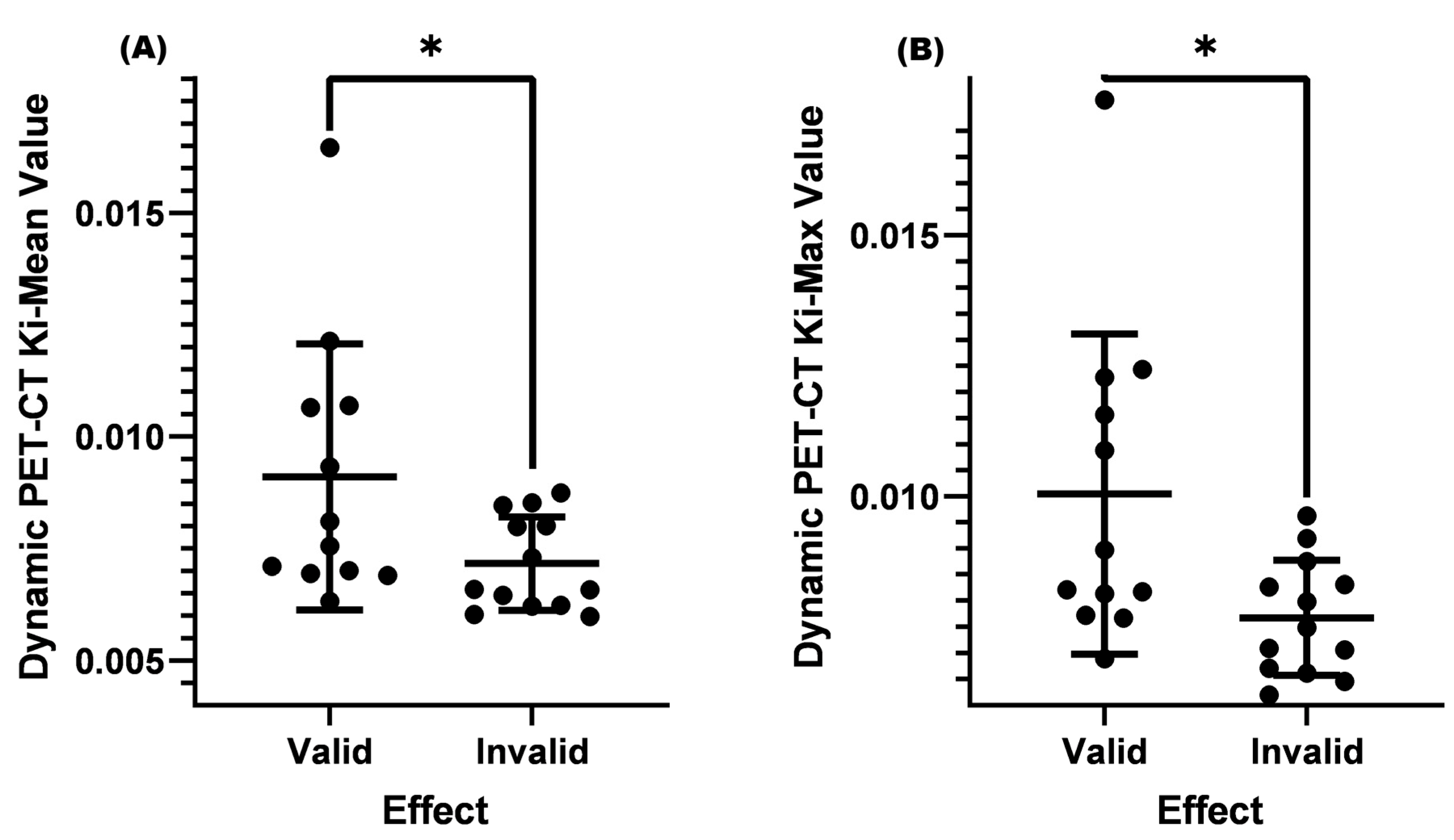
3.4. Comparison of Ki-Mean and Ki-Max between the Valid and Invalid Groups with an SUV-Max ≤ 4.5 and Lymph Nodes < 1.0 cm before Treatment
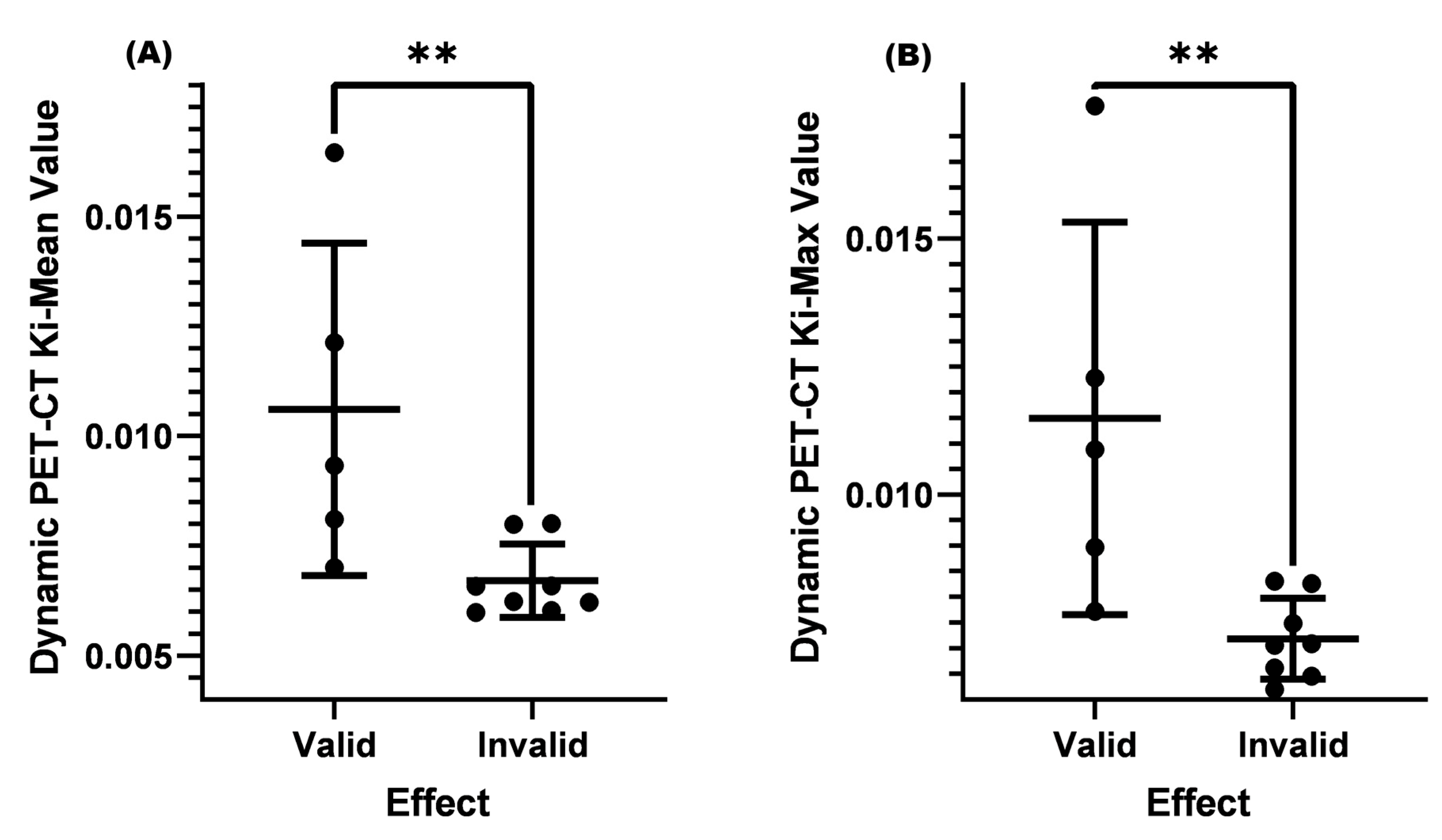
3.5. Comparison of Ki-Mean and Ki-Max between the Valid and Invalid Groups with an SUV-Max ≤ 4.5 and a Lymph Node < 1.0 cm and a Normal EBV-DNA Replication before Treatment
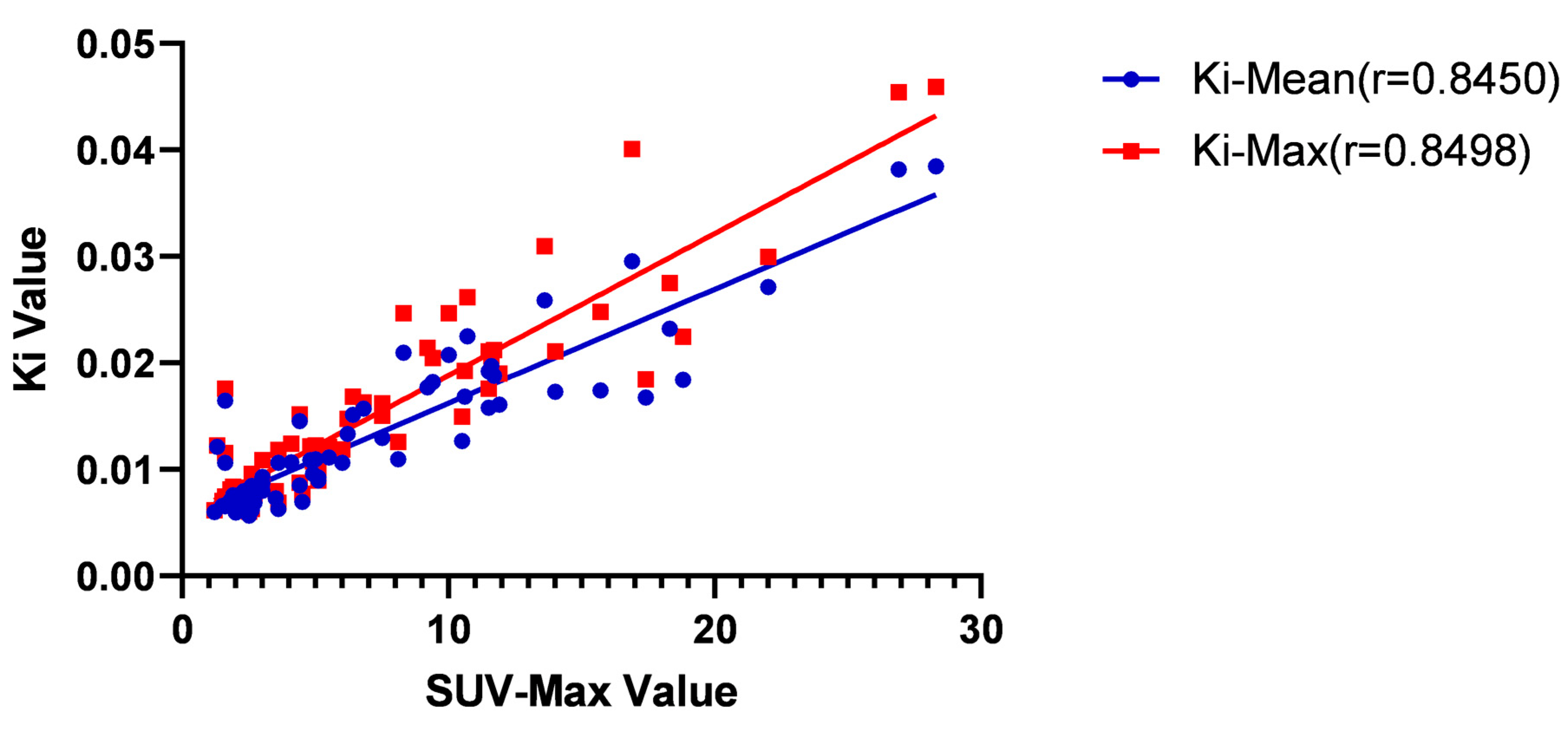
3.6. The Correlation between Different Factors and Ki-Mean and Ki-Max
3.7. Diagnostic Accuracy of SUV-Max and Ki for Cervical Lymph Node Metastasis in Nasopharyngeal Cancer
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, Y.-P.; Chan, A.T.C.; Le, Q.-T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef] [PubMed]
- Ho, F.C.; Tham, I.W.; Earnest, A.; Lee, K.M.; Lu, J.J. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: A meta-analysis of clinical evidence. BMC Cancer 2012, 12, 98. [Google Scholar] [CrossRef] [Green Version]
- Wei, W.I.; Chan, J.Y.W.; Ng, R.W.M.; Ho, W.K. Surgical salvage of persistent or recurrent nasopharyngeal carcinoma with maxillary swing approach—Critical appraisal after 2 decades. Head Neck 2011, 33, 969–975. [Google Scholar] [CrossRef]
- Liu, F.-Y.; Lin, C.-Y.; Chang, J.T.; Ng, S.-H.; Chin, S.-C.; Wang, H.-M.; Liao, C.-T.; Chan, S.-C.; Yen, T.-C. 18F-FDG PET Can Replace Conventional Work-up in Primary M Staging of Nonkeratinizing Nasopharyngeal Carcinoma. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2007, 48, 1614–1619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, L.-Q.; Chen, Q.-Y.; Fan, W.; Liu, H.; Zhang, L.; Guo, L.; Luo, D.-H.; Huang, P.-Y.; Zhang, X.; Lin, X.-P.; et al. Prospective Study of Tailoring Whole-Body Dual-Modality [18F]Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography With Plasma Epstein-Barr Virus DNA for Detecting Distant Metastasis in Endemic Nasopharyngeal Carcinoma at Initial Staging. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 2861–2869. [Google Scholar] [CrossRef]
- De Jaeghere, E.A.; Laloo, F.; Lippens, L.; Van Bockstal, M.; De Man, K.; Naert, E.; Van Dorpe, J.; Van de Vijver, K.; Tummers, P.; Makar, A.; et al. Splenic 18F-FDG uptake on baseline PET/CT is associated with oncological outcomes and tumor immune state in uterine cervical cancer. Gynecol. Oncol. 2020, 159, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Furlow, B. PET-CT Cancer Imaging. Radiol. Technol. 2018, 90, 149CT–170CT. [Google Scholar]
- Yang, D.M.; Palma, D.; Louie, A.; Malthaner, R.; Fortin, D.; Rodrigues, G.; Yaremko, B.; Laba, J.; Gaede, S.; Warner, A.; et al. Assessment of tumor response after stereotactic ablative radiation therapy for lung cancer: A prospective quantitative hybrid (18) F-fluorodeoxyglucose-positron emission tomography and CT perfusion study. J. Med. Imaging Radiat. Oncol. 2019, 63, 94–101. [Google Scholar] [CrossRef] [Green Version]
- Devriese, J.; Beels, L.; Maes, A.; Van De Wiele, C.; Gheysens, O.; Pottel, H. Review of clinically accessible methods to determine lean body mass for normalization of standardized uptake values. Q. J. Nucl. Med. Mol. Imaging 2016, 60, 1–11. [Google Scholar]
- Wang, Z.; Wu, Y.; Li, X.; Bai, Y.; Chen, H.; Ding, J.; Shen, C.; Hu, Z.; Liang, D.; Liu, X.; et al. Comparison between a dual-time-window protocol and other simplified protocols for dynamic total-body 18F-FDG PET imaging. EJNMMI Phys. 2022, 9, 63. [Google Scholar] [CrossRef]
- Zaidi, H.; Karakatsanis, N. Towards enhanced PET quantification in clinical oncology. Br. J. Radiol. 2018, 91, 20170508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, M.C.; Turkington, T.G.; Wilson, J.M.; Wong, T.Z. A Systematic Review of the Factors Affecting Accuracy of SUV Measurements. AJR Am. J. Roentgenol. 2010, 195, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Lin, Z.; Xu, Z.; Li, D.; Lv, W.; Yang, S.; Liu, Y.; Cao, Y.; Cao, Q.; Jin, H. Influx rate constant of 18F-FDG increases in metastatic lymph nodes of non-small cell lung cancer patients. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1198–1208. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Xiao, L.; Wang, Y.; Liu, C.; Cao, L.; Zhai, W.; Wang, B.; Yu, S.; Xin, J. Diagnostic value of dynamic 18F-FDG PET/CT imaging in non-small cell lung cancer and FDG hypermetabolic lymph nodes. Quant. Imaging Med. Surg. 2023, 13, 2556–2567. [Google Scholar] [CrossRef]
- Wumener, X.; Zhang, Y.; Wang, Z.; Zhang, M.; Zang, Z.; Huang, B.; Liu, M.; Huang, S.; Huang, Y.; Wang, P.; et al. Dynamic FDG-PET imaging for differentiating metastatic from non-metastatic lymph nodes of lung cancer. Front. Oncol. 2022, 12, 1005924. [Google Scholar] [CrossRef]
- Zhuang, M.; Karakatsanis, N.A.; Dierckx, R.A.J.O.; Zaidi, H. Impact of Tissue Classification in MRI-Guided Attenuation Correction on Whole-Body Patlak PET/MRI. Mol. Imaging Biol. 2019, 21, 1147–1156. [Google Scholar] [CrossRef] [Green Version]
- Zhuang, M.; Karakatsanis, N.A.; Dierckx, R.; Zaidi, H. Quantitative Analysis of Heterogeneous [18F]FDG Static (SUV) vs. Patlak (Ki) Whole-body PET Imaging Using Different Segmentation Methods: A Simulation Study. Mol. Imaging Biol. 2019, 21, 317–327. [Google Scholar] [CrossRef] [Green Version]
- van Sluis, J.; van Snick, J.H.; Brouwers, A.H.; Noordzij, W.; Dierckx, R.A.J.O.; Borra, R.J.H.; Lammertsma, A.A.; Glaudemans, A.W.J.M.; Slart, R.H.J.A.; Yaqub, M.; et al. Shortened duration whole body 18F-FDG PET Patlak imaging on the Biograph Vision Quadra PET/CT using a population-averaged input function. EJNMMI Phys. 2022, 9, 74. [Google Scholar] [CrossRef]
- Karakatsanis, N.A.; Lodge, M.A.; Zhou, Y.; Wahl, R.L.; Rahmim, A. Dynamic whole-body PET parametric imaging: II. Task-oriented statistical estimation. Phys. Med. Biol. 2013, 58, 7419–7445. [Google Scholar] [CrossRef] [Green Version]
- Karakatsanis, N.A.; Lodge, M.A.; Tahari, A.K.; Zhou, Y.; Wahl, R.L.; Rahmim, A. Dynamic whole-body PET parametric imaging: I. Concept, acquisition protocol optimization and clinical application. Phys. Med. Biol. 2013, 58, 7391–7418. [Google Scholar] [CrossRef] [Green Version]
- Lv, W.; Yang, M.; Zhong, H.; Wang, X.; Yang, S.; Bi, L.; Xian, J.; Pei, X.; He, X.; Wang, Y.; et al. Application of Dynamic 18F-FDG PET/CT for Distinguishing Intrapulmonary Metastases from Synchronous Multiple Primary Lung Cancer. Mol. Imaging 2022, 2022, 8081299. [Google Scholar] [CrossRef] [PubMed]
- Minocha, J.; Lewandowski, R.J. Assessing Imaging Response to Therapy. Radiol. Clin. N. Am. 2015, 53, 1077–1088. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, R.; Kawano, S.; Chikui, T.; Kiyosue, T.; Goto, Y.; Hirano, M.; Jinno, T.; Nagata, T.; Oobu, K.; Abe, K.; et al. Clinical Significance of Combined Assessment of the Maximum Standardized Uptake Value of F-18 FDG PET with Nodal Size in the Diagnosis of Cervical Lymph Node Metastasis of Oral Squamous Cell Carcinoma. Acad. Radiol. 2012, 19, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Vogl, T.; Bisdas, S. Lymph node staging. Top. Magn. Reson. Imaging 2007, 18, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Tsao, S.W.; Tsang, C.M.; Lo, K.W. Epstein-Barr virus infection and nasopharyngeal carcinoma. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2017, 372, 20160270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Z.; Tsai, M.-H.; Shumilov, A.; Baccianti, F.; Tsao, S.W.; Poirey, R.; Delecluse, H.-J. Epstein-Barr virus ncRNA from a nasopharyngeal carcinoma induces an inflammatory response that promotes virus production. Nat. Microbiol. 2019, 4, 2475–2486. [Google Scholar] [CrossRef]
- Vasudevan, H.N.; Yom, S.S. Nasopharyngeal Carcinoma and Its Association with Epstein-Barr Virus. Hematol. Oncol. Clin. N. Am. 2021, 35, 963–971. [Google Scholar] [CrossRef]
- Zhao, C.-X.; Zhu, W.; Ba, Z.-Q.; Xu, H.-J.; Liu, W.-D.; Zhu, B.; Wang, L.; Song, Y.-J.; Yuan, S.; Ren, C.-P. The regulatory network of nasopharyngeal carcinoma metastasis with a focus on EBV, lncRNAs and miRNAs. Am. J. Cancer Res. 2018, 8, 2185–2209. [Google Scholar]
- Otrante, A.; Bounafaa, A.; Berrougui, H.; Essamadi, A.-K.; Nguyen, M.; Fülöp, T.; Khalil, A. Small Dense LDL Level and LDL/HDL Distribution in Acute Coronary Syndrome Patients. Biomedicines 2023, 11, 1198. [Google Scholar] [CrossRef]
- Wang, X.S.; Yan, C.; Hu, C.S.; Ying, H.M.; He, X.Y.; Zhou, Z.R.; Ding, J.H. Study of the medial group retropharyngeal node metastasis from nasopharyngeal carcinoma based on 3100 newly diagnosed cases. Oral Oncol. 2014, 50, 1109–1113. [Google Scholar] [CrossRef]
- Fang, F.M.; Tsai, W.L.; Chen, H.C.; Hsu, H.C.; Hsiung, C.Y.; Chien, C.Y.; Ko, S.F. Intensity-modulated or conformal radiotherapy improves the quality of life of patients with nasopharyngeal carcinoma: Comparisons of four radiotherapy techniques. Cancer 2007, 109, 313–321. [Google Scholar] [CrossRef]
- Lu, H.; Peng, L.; Yuan, X.; Hao, Y.; Lu, Z.; Chen, J.; Chang, J.; Geng, S.; Gu, J.; Pang, Q.; et al. Concurrent chemoradiotherapy in locally advanced nasopharyngeal carcinoma: A treatment paradigm also applicable to patients in Southeast Asia. Cancer Treat. Rev. 2009, 35, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Luo, T.; Jin, T.; Zhang, J.; Xiang, Z.; Yan, R.; Xie, L.; Wu, X.; Zhang, H.; Wang, F.; et al. Advantages of using reduced-volume intensity modulated radiation therapy for the treatment of nasopharyngeal carcinoma: A retrospective paired study. BMC Cancer 2019, 19, 554. [Google Scholar] [CrossRef] [Green Version]
- Paiar, F.; Di Cataldo, V.; Zei, G.; Pasquetti, E.M.; Cecchini, S.; Meattini, I.; Mangoni, M.; Agresti, B.; Iermano, C.; Bonomo, P.; et al. Role of chemotherapy in nasopharyngeal carcinoma. Oncol. Rev. 2012, 6, e1. [Google Scholar] [CrossRef] [PubMed]
- Muzi, M.; O’Sullivan, F.; Mankoff, D.A.; Doot, R.K.; Pierce, L.A.; Kurland, B.F.; Linden, H.M.; Kinahan, P.E. Quantitative assessment of dynamic PET imaging data in cancer imaging. Magn. Reson. Imaging 2012, 30, 1203–1215. [Google Scholar] [CrossRef] [Green Version]
- Laffon, E.; de Clermont, H.; Begueret, H.; Vernejoux, J.-M.; Thumerel, M.; Marthan, R.; Ducassou, D. Assessment of dual-time-point 18F-FDG-PET imaging for pulmonary lesions. Nucl. Med. Commun. 2009, 30, 455–461. [Google Scholar] [CrossRef]
- Huang, X.; Zhuang, M.; Yang, S.; Wang, Y.; Liu, Q.; Xu, X.; Xiao, M.; Peng, Y.; Jiang, P.; Xu, W.; et al. The valuable role of dynamic 18F FDG PET/CT-derived kinetic parameter Ki in patients with nasopharyngeal carcinoma prior to radiotherapy: A prospective study. Radiother. Oncol. 2023, 179, 109440. [Google Scholar] [CrossRef]
- Kojima, I.; Takanami, K.; Ogawa, T.; Ishikawa, K.; Morishita, Y.; Ishii, R.; Ohkoshi, A.; Nakanome, A.; Odagiri, H.; Iikubo, M. High diagnostic accuracy for lymph node metastasis of oral squamous cell carcinoma using PET/CT with a silicon photomultiplier. Oral Radiol. 2022, 38, 540–549. [Google Scholar] [CrossRef]
- Luzuriaga, K.; Sullivan, J.L. Infectious mononucleosis. N. Engl. J. Med. 2010, 362, 1993–2000. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.Y.; Le, Q.-T.; Yom, S.S.; Ng, R.H.; Chan, K.A.; Bratman, S.V.; Welch, J.J.; Divi, R.L.; Petryshyn, R.A.; Conley, B.A. Clinical Utility of Epstein-Barr Virus DNA Testing in the Treatment of Nasopharyngeal Carcinoma Patients. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 996–1001. [Google Scholar] [CrossRef]
- Hsu, C.-L.; Chang, K.-P.; Lin, C.-Y.; Chang, H.-K.; Wang, C.-H.; Lin, T.-L.; Liao, C.-T.; Tsang, N.-M.; Lee, L.-Y.; Chan, S.-C.; et al. Plasma epstein-barr virus DNA concentration and clearance rate as novel prognostic factors for metastatic nasopharyngeal carcinoma. Head Neck 2012, 34, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Duffy, M.J.; Sturgeon, C.; Lamerz, R.; Haglund, C.; Holubec, V.L.; Klapdor, R.; Nicolini, A.; Topolcan, O.; Heinemann, V. Tumor markers in pancreatic cancer: A European Group on Tumor Markers (EGTM) status report. Ann. Oncol. 2010, 21, 441–447. [Google Scholar] [CrossRef] [PubMed]



| Variable | Number (%) |
|---|---|
| Median Age(years) | 48 |
| Sex | |
| Male | 36 (71) |
| Female | 15 (29) |
| T Stage | |
| T1 | 7 (14) |
| T2 | 9 (17) |
| T3 | 28 (55) |
| T4 | 7 (14) |
| N Stage | |
| N1 | 21 (41) |
| N2 | 27 (53) |
| N3 | 3 (6) |
| M Stage | |
| Mx | 3 (6) |
| M0 | 43 (86) |
| M1 | 3 (8) |
| Clinical Stage | |
| I | 0 (0) |
| II | 8 (16) |
| III | 27 (53) |
| IV | 15 (29) |
| Not Identified | 1 (2) |
| EBV-DNA Status | |
| High Level | 23 (45) |
| Normal Level | 28 (55) |
| Clinical Efficacy | Number (%) | Mean SUV-Max | p Value | Mean Ki-Mean | p Value | Mean Ki-Max | p Value |
|---|---|---|---|---|---|---|---|
| Valid | 50 (75) | 7.2 | <0.001 | 0.01323 | <0.001 | 0.01510 | <0.001 |
| Invalid | 17 (25) | 4.3 | 0.00978 | 0.01077 |
| Clinical Efficacy | Mean Ki-Mean | p Value | Mean Ki-Max | p Value |
|---|---|---|---|---|
| Valid | 0.00897 | >0.05 | 0.00982 | >0.05 |
| Invalid | 0.00737 | 0.00787 |
| Clinical Efficacy | Mean Ki-Mean Value | p Value | Mean Ki-Max Value | p Value |
|---|---|---|---|---|
| Valid | 0.00910 | 0.0457 | 0.01004 | 0.0298 |
| Invalid | 0.00716 | 0.00767 |
| Clinical Efficacy | Mean Ki-Mean Value | p Value | Mean Ki-Max Value | p Value |
|---|---|---|---|---|
| Valid | 0.01060 | 0.0062 | 0.01149 | 0.0062 |
| Invalid | 0.00670 | 0.00719 |
| Factors | Ki-Mean | Ki-Max | ||
|---|---|---|---|---|
| r | p Value | r | p Value | |
| SUV-Max | 0.8450 | <0.01 | 0.8498 | <0.01 |
| T-Stage | 0.0659 | 0.60 | 0.0517 | 0.68 |
| Normal EBV-DNA level | 0.2171 | 0.08 | 0.2318 | 0.06 |
| Age | 0.0558 | 0.65 | 0.0739 | 0.55 |
| Lymph node < 1.0 cm | 0.6369 | <0.01 | 0.6416 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, G.; Yang, S.; Wang, S.; Jiang, R.; Xu, X. Diagnostic Value of Dynamic 18F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography (18F-FDG PET-CT) in Cervical Lymph Node Metastasis of Nasopharyngeal Cancer. Diagnostics 2023, 13, 2530. https://doi.org/10.3390/diagnostics13152530
Li G, Yang S, Wang S, Jiang R, Xu X. Diagnostic Value of Dynamic 18F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography (18F-FDG PET-CT) in Cervical Lymph Node Metastasis of Nasopharyngeal Cancer. Diagnostics. 2023; 13(15):2530. https://doi.org/10.3390/diagnostics13152530
Chicago/Turabian StyleLi, Guanglie, Shuai Yang, Siyang Wang, Renwei Jiang, and Xiwei Xu. 2023. "Diagnostic Value of Dynamic 18F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography (18F-FDG PET-CT) in Cervical Lymph Node Metastasis of Nasopharyngeal Cancer" Diagnostics 13, no. 15: 2530. https://doi.org/10.3390/diagnostics13152530
APA StyleLi, G., Yang, S., Wang, S., Jiang, R., & Xu, X. (2023). Diagnostic Value of Dynamic 18F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography (18F-FDG PET-CT) in Cervical Lymph Node Metastasis of Nasopharyngeal Cancer. Diagnostics, 13(15), 2530. https://doi.org/10.3390/diagnostics13152530






