Reasons for Delayed Diagnosis of Pediatric Acute Appendicitis during the COVID-19 Era: A Narrative Review
Abstract
1. Introduction
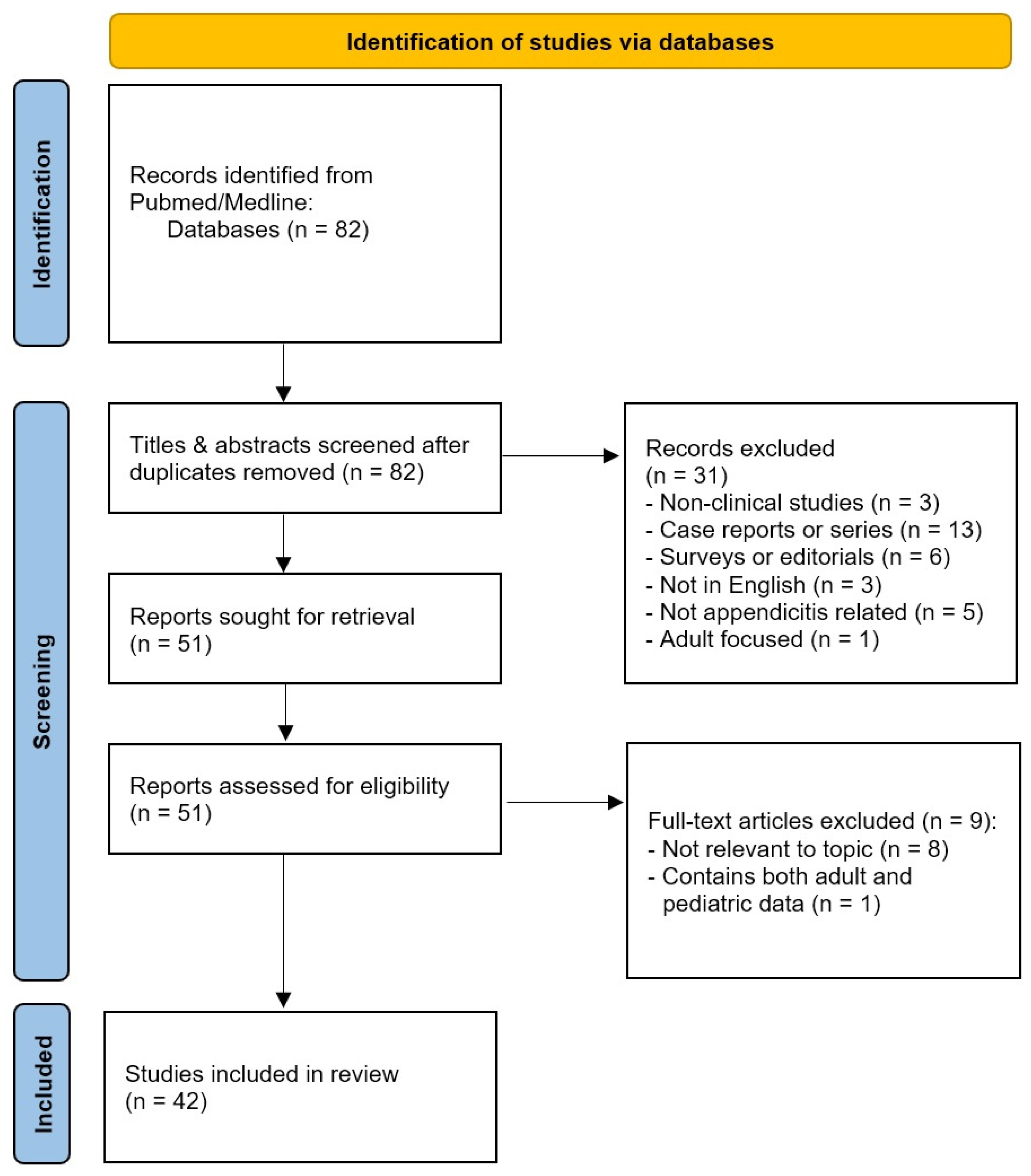
2. Materials and Methods
3. Results
4. Discussion
4.1. Key Findings
4.2. Reasons for Delayed Diagnosis
4.2.1. Public Health and Social Measures (PHSMs)
4.2.2. Fear of Exposure by Parents/Caregivers and/or Patients
4.2.3. Fear of Exposure by Medical Staff
4.2.4. Telemedicine Use
4.2.5. COVID-19-Positive Pediatric Patients with Suspected Appendicitis
4.2.6. Recurrent Appendicitis after Non-Operative Management
4.2.7. Delays in Primary Operative Management or Increased Time to Operating Room
4.3. Time to Hospital Admission, Duration of Symptoms and In-Hospital Delays
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- World Health Organization-Public Health and Social Measures. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/phsm (accessed on 15 April 2023).
- Isba, R.; Edge, R.; Jenner, R.; Broughton, E.; Francis, N.; Butler, J. Where Have All the Children Gone? Decreases in Paediatric Emergency Department Attendances at the Start of the COVID-19 Pandemic of 2020. Arch. Dis. Child. 2020, 105, 704. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed Access or Provision of Care in Italy Resulting from Fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Mantica, G.; Riccardi, N.; Terrone, C.; Gratarola, A. Non-COVID-19 Visits to Emergency Departments during the Pandemic: The Impact of Fear. Public Health 2020, 183, 40–41. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, J.A.; Kunkov, S.; Chao, J.H.; Tay, E.T.; George, J.P.; Borukhov, D.; Alerhand, S.; Harrison, P.A.; Hom, J.; Crain, E.F. Association of Delay in Appendectomy with Perforation in Children with Appendicitis. Pediatr. Emerg. Care 2019, 35, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, J.E.; Grant, H.; Pérez Coulter, A.M.; Tirabassi, M.V. Association Between the SARS-Cov2 Pandemic and Pediatric Surgical Consultations. J. Surg. Res. 2022, 279, 299–303. [Google Scholar] [CrossRef]
- Ali, S.; Khan, M.A.; Rehman, I.U.; Uzair, M. Impact of Covid 19 Pandemic on Presentation, Treatment and Outcome of Paediatric Surgical Emergencies. J. Ayub Med. Coll. Abbottabad JAMC 2020, 32 (Suppl. 1), S621–S624. [Google Scholar]
- Rethi, S.; Kairam, N.; Amato, C.S.; Allegra, J.R.; Eskin, B. Six Diagnoses of Separation: Impact of COVID-19 on Pediatric Emergency Department Visits: A Multicenter Study. J. Emerg. Med. 2022, 63, 723–728. [Google Scholar] [CrossRef]
- Bhangu, A.; Søreide, K.; Di Saverio, S.; Assarsson, J.H.; Drake, F.T. Acute Appendicitis: Modern Understanding of Pathogenesis, Diagnosis, and Management. Lancet 2015, 386, 1278–1287. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Domjanović, J.; Jukić, M.; Poklepović Peričić, T. Acute Appendicitis in Children Younger than Five Years of Age: Diagnostic Challenge for Pediatric Surgeons. Surg. Infect. 2020, 21, 239–245. [Google Scholar] [CrossRef]
- Köhler, F.; Müller, S.; Hendricks, A.; Kastner, C.; Reese, L.; Boerner, K.; Flemming, S.; Lock, J.F.; Germer, C.-T.; Wiegering, A. Changes in Appendicitis Treatment during the COVID-19 Pandemic—A Systematic Review and Meta-Analysis. Int. J. Surg. 2021, 95, 106148. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Anand, S.; Žuvela, T.; Singh, A.; Križanac, Z.; Krishnan, N. Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies. Diagnostics 2022, 12, 127. [Google Scholar] [CrossRef] [PubMed]
- Snapiri, O.; Rosenberg Danziger, C.; Krause, I.; Kravarusic, D.; Yulevich, A.; Balla, U.; Bilavsky, E. Delayed Diagnosis of Paediatric Appendicitis during the COVID-19 Pandemic. Acta Paediatr. Oslo Nor. 1992 2020, 109, 1672–1676. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Miguel, C.; Garcia Urbán, J.; Del Monte Ferrer, C.; Muñoz-Serrano, A.; Miguel-Ferrero, M.; Martínez, L. Impact of the COVID-19 Pandemic on Acute Appendicitis in Children. J. Healthc. Qual. Res. 2022, 37, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Sheath, C.; Abdelrahman, M.; MacCormick, A.; Chan, D. Paediatric Appendicitis during the COVID-19 Pandemic. J. Paediatr. Child Health 2021, 57, 986–989. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Saleh, A. Effect of COVID-19 on Pediatric Appendicitis Presentations and Complications. J. Pediatr. Surg. 2022, 57, 861–865. [Google Scholar] [CrossRef]
- Delgado-Miguel, C.; Muñoz-Serrano, A.J.; Miguel-Ferrero, M.; De Ceano-Vivas, M.; Calvo, C.; Martínez, L. Complicated Acute Appendicitis during COVID-19 Pandemic: The Hidden Epidemic in Children. Eur. J. Pediatr. Surg. 2022, 32, 268–273. [Google Scholar] [CrossRef]
- Ayyıldız, H.N.; Mirapoglu, S.; Akış Yıldız, Z.; Şahin, C.; Güvenç, F.T.; Arpacık, M.; Ilce, Z. What Has Changed in Children’s Appendicitis during the COVID-19 Pandemic? Ulus. Travma Acil Cerrahi Derg. 2022, 28, 1674–1681. [Google Scholar] [CrossRef]
- ANZSCRAFT Collaborative; Roberts, K. Impact of COVID-19 on Appendicitis Presentations in Children in Australia and New Zealand. ANZ J. Surg. 2022, 92, 736–741. [Google Scholar] [CrossRef]
- Nassiri, A.M.; Pruden, R.D.; Holan, C.A.; Guerra, A.D.; Nganga, P.W.; Wilkinson, M.H.; Lawson, K.A.; Allen, C.H.; Gregg, V.S.; Naiditch, J.A. Pediatric Appendicitis in the Time of the COVID-19 Pandemic: A Retrospective Chart Review. J. Am. Coll. Emerg. Physicians Open 2022, 3, e12722. [Google Scholar] [CrossRef]
- Toro Rodríguez, M.G.; Dore Reyes, M.; Martínez Castaño, I.; Deltell Colomer, P.; de la Sen Maldonado, C.; Díaz Díaz, V.; Encinas Goenechea, A.; Gonzálvez Piñera, J. Have Acute Appendicitis Complications Increased in Children as a Result of SARS-CoV-2? Cir. Pediatr. 2022, 35, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Motazedian, G.; Aryanpoor, P.; Rahmanian, E.; Abiri, S.; Kalani, N.; Hatami, N.; Bagherian, F.; Etezadpour, M.; Farzaneh, R.; Maleki, F.; et al. Incidence of Pediatric Perforated Appendicitis during the COVID-19 Pandemic; a Systematic Review and Meta-Analysis. Arch. Acad. Emerg. Med. 2022, 10, e3. [Google Scholar] [CrossRef] [PubMed]
- La Pergola, E.; Sgrò, A.; Rebosio, F.; Vavassori, D.; Fava, G.; Codrich, D.; Montanaro, B.; Leva, E.; Schleef, J.; Cheli, M.; et al. Appendicitis in Children in a Large Italian COVID-19 Pandemic Area. Front. Pediatr. 2020, 8, 600320. [Google Scholar] [CrossRef] [PubMed]
- Gaitero Tristán, J.; Souto Romero, H.; Escalada Pellitero, S.; Espiñera, C.R.; Andina Martín, D.; Espinosa Góngora, R.; Martín Diaz, M.J.; Leónidas Espinoza, M. Acute Appendicitis in Children During the COVID-19 Pandemic: Neither Delayed Diagnosis Nor Worse Outcomes. Pediatr. Emerg. Care 2021, 37, 185–190. [Google Scholar] [CrossRef]
- Esparaz, J.R.; Chen, M.K.; Beierle, E.A.; Anderson, S.A.; Martin, C.A.; Mortellaro, V.E.; Rogers, D.A.; Mathis, M.S.; Russell, R.T. Perforated Appendicitis During a Pandemic: The Downstream Effect of COVID-19 in Children. J. Surg. Res. 2021, 268, 263–266. [Google Scholar] [CrossRef]
- Quaglietta, P.R.; Ramjist, J.K.; Antwi, J.; Kissoondoyal, A.; Lapidus-Krol, E.; Baertschiger, R.M. Unanticipated Consequences of COVID-19 Pandemic Policies on Pediatric Acute Appendicitis Surgery. J. Pediatr. Surg. 2023, 58, 931–938. [Google Scholar] [CrossRef]
- Taşçı, A.; Gürünlüoğlu, K.; Yıldız, T.; Arslan, A.K.; Akpınar, N.; Serbest Çin, E.; Demircan, M. Impact of COVID-19 Pandemic on Pediatric Appendicitis Hospital Admission Time and Length of Hospital Stay. Ulus. Travma Acil Cerrahi Derg. 2022, 28, 1095–1099. [Google Scholar] [CrossRef]
- Horst, K.K.; Kolbe, A.B.; McDonald, J.S.; Froemming, A.T.; Parvinian, A.; Klinkner, D.B.; Binkovitz, L.A. Imaging Pediatric Acute Appendicitis during the Coronavirus Disease 2019 (COVID-19) Pandemic: Collateral Damage Is Variable. Pediatr. Radiol. 2021, 51, 1991–1999. [Google Scholar] [CrossRef]
- Head, W.T.; Parrado, R.H.; Cina, R.A. Impact of the Coronavirus (COVID-19) Pandemic on the Care of Pediatric Acute Appendicitis. Am. Surg. 2023, 89, 1527–1532. [Google Scholar] [CrossRef]
- Moratilla Lapeña, L.; Delgado-Miguel, C.; Sarmiento Caldas, M.C.; Estefanía, K.; Velayos, M.; Muñoz-Serrano, A.; De Ceano-Vivas, M.; López-Santamaría, M.; Martínez, L. Impact of SARS-CoV-2 Pandemic on Emergency Department Activity at the Pediatric Surgery Unit of a Third-Level Hospital. Cir. Pediatr. 2021, 34, 85–89. [Google Scholar]
- Iantorno, S.E.; Skarda, D.E.; Bucher, B.T. Concurrent SARS-CoV-19 and Acute Appendicitis: Management and Outcomes across United States Children’s Hospitals. Surgery 2023, 173, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, F.-M.; Meyer, J.; Kellnar, S.; Warmbrunn, J.; Schuster, T.; Simon, S.; Meyer, T.; Platzer, J.; Hubertus, J.; Seitz, S.T.; et al. Increased Incidence of Perforated Appendicitis in Children During COVID-19 Pandemic in a Bavarian Multi-Center Study. Front. Pediatr. 2021, 9, 683607. [Google Scholar] [CrossRef] [PubMed]
- Yock-Corrales, A.; Lenzi, J.; Ulloa-Gutiérrez, R.; Gómez-Vargas, J.; Antúnez-Montes, O.Y.; Rios Aida, J.A.; Del Aguila, O.; Arteaga-Menchaca, E.; Campos, F.; Uribe, F.; et al. Acute Abdomen and Appendicitis in 1010 Pediatric Patients With COVID-19 or MIS-C: A Multinational Experience from Latin America. Pediatr. Infect. Dis. J. 2021, 40, e364–e369. [Google Scholar] [CrossRef]
- Tan, A.P.P.; Yap, T.-L.; Cheong, Y.L.; Rai, R.; Choo, C.; Ong, C.; Low, Y.; Jacobsen, A.; Loh, A.; Ong, L.Y.; et al. Conservative Antibiotic Treatment of Pediatric Acute Uncomplicated Appendicitis during the COVID-19 Pandemic: A Prospective Comparative Cohort Study. Pediatr. Surg. Int. 2022, 39, 60. [Google Scholar] [CrossRef] [PubMed]
- Theodorou, C.M.; Beres, A.L.; Nguyen, M.; Castle, S.L.; Faltermeier, C.; Shekherdimian, S.; Tung, C.; DeUgarte, D.A.; Brown, E.G. Statewide Impact of the COVID Pandemic on Pediatric Appendicitis in California: A Multicenter Study. J. Surg. Res. 2021, 267, 132–142. [Google Scholar] [CrossRef]
- Gerall, C.D.; DeFazio, J.R.; Kahan, A.M.; Fan, W.; Fallon, E.M.; Middlesworth, W.; Stylianos, S.; Zitsman, J.L.; Kadenhe-Chiweshe, A.V.; Spigland, N.A.; et al. Delayed Presentation and Sub-Optimal Outcomes of Pediatric Patients with Acute Appendicitis during the COVID-19 Pandemic. J. Pediatr. Surg. 2021, 56, 905–910. [Google Scholar] [CrossRef]
- Farooq, M.A.A.; Kabir, S.M.H.; Chowdhury, T.K.; Sadia, A.; Alam, M.A.; Farhad, T. Changes in Children’s Surgical Services during the COVID-19 Pandemic at a Tertiary-Level Government Hospital in a Lower Middle-Income Country. BMJ Paediatr. Open 2021, 5, e001066. [Google Scholar] [CrossRef]
- Pawelczyk, A.; Kowalska, M.; Tylicka, M.; Koper-Lenkiewicz, O.M.; Komarowska, M.D.; Hermanowicz, A.; Debek, W.; Matuszczak, E. Impact of the SARS-CoV-2 Pandemic on the Course and Treatment of Appendicitis in the Pediatric Population. Sci. Rep. 2021, 11, 23999. [Google Scholar] [CrossRef]
- Percul, C.; Cruz, M.; Curiel Meza, A.; González, G.; Lerendegui, L.; Malzone, M.C.; Liberto, D.; Lobos, P.; Imach, B.E.; Moldes, J.M.; et al. Impact of the COVID-19 Pandemic on the Pediatric Population with Acute Appendicitis: Experience at a General, Tertiary Care Hospital. Arch. Argent. Pediatr. 2021, 119, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Ergün, E.; Sözduyar, S.; Gurbanova, A.; Serttürk, F.; Çiftçi, E.; Özdemir, H.; Arga, G.; Konca, H.K.; Çınar, G.; Akdemir Kalkan, İ.; et al. An Indirect Effect of COVID-19 Pandemic: Increased Pediatric Perforated Appendicitis Rate Due to Delayed Admission. Turk. J. Surg. 2021, 37, 318–323. [Google Scholar] [CrossRef]
- Yap, T.-L.; Li, F.X.; Lee, I.N.; Chen, Y.; Choo, C.S.; Sim, S.W.; Rai, R.; Ong, L.Y. COVID-19 Pandemic Strategy for Treatment of Acute Uncomplicated Appendicitis with Antibiotics- Risk Categorization and Shared Decision-Making. J. Pediatr. Surg. 2023, 58, 1285–1290. [Google Scholar] [CrossRef] [PubMed]
- Bethell, G.S.; Gosling, T.; Rees, C.M.; Sutcliffe, J.; Hall, N.J.; CASCADE Study Collaborators and the RIFT Study Collaborators. Impact of the COVID-19 Pandemic on Management and Outcomes of Children with Appendicitis: The Children with AppendicitiS during the CoronAvirus PanDEmic (CASCADE) Study. J. Pediatr. Surg. 2022, 57, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Vansevičienė, I.; Bučinskaitė, D.; Malcius, D.; Lukošiūtė-Urbonienė, A.; Beržanskis, M.; Čekanauskas, E.; Barauskas, V. Did the COVID-19 Pandemic Prolong the Time Till Diagnosis and Worsen Outcomes for Children with Acute Appendicitis? Med. Kaunas Lith. 2021, 57, 1234. [Google Scholar] [CrossRef]
- Patel, M.; Thomas, J.J.; Sarwary, H. We Can Reduce Negative Paediatric Appendicectomy Rate: A Cohort Study. Ann. Med. Surg. 2021, 71, 102901. [Google Scholar] [CrossRef]
- Montalva, L.; Haffreingue, A.; Ali, L.; Clariot, S.; Julien-Marsollier, F.; Ghoneimi, A.E.; Peycelon, M.; Bonnard, A. The Role of a Pediatric Tertiary Care Center in Avoiding Collateral Damage for Children with Acute Appendicitis during the COVID-19 Outbreak. Pediatr. Surg. Int. 2020, 36, 1397–1405. [Google Scholar] [CrossRef]
- Öztaş, T.; Bilici, S.; Dursun, A. Has the Frequency of Complicated Appendicitis Changed in Children in the First Year of the COVID-19 Pandemic? Ann. Pediatr. Surg. 2023, 19, 3. [Google Scholar] [CrossRef] [PubMed]
- Dass, D.; Hotonu, S.; McHoney, M.; Munro, F. Prospective Study of Laparoscopic Management of Appendicitis during the COVID Pandemic in a Single Paediatric Centre. Afr. J. Paediatr. Surg. AJPS 2023, 20, 40–45. [Google Scholar] [CrossRef]
- Gürünlüoglu, K.; Zararsiz, G.; Aslan, M.; Akbas, S.; Tekin, M.; Gürünlüoglu, S.; Bag, H.G.; Cin, E.S.; Macit, B.; Demircan, M. Investigation of Serum Interleukin 6, High-Sensitivity C-Reactive Protein and White Blood Cell Levels during the Diagnosis and Treatment of Paediatric Appendicitis Patients Before and during the COVID-19 Pandemic. Afr. J. Paediatr. Surg. 2023, 20, 130–137. [Google Scholar] [CrossRef]
- Del Giorgio, F.; Habti, M.; Merckx, J.; Kaufman, J.S.; Gravel, J.; Piché, N.; Osmanlliu, E.; Drouin, O. Investigating Changes in Incidence and Severity of Pediatric Appendicitis during the COVID-19 Pandemic in Canada: An Interrupted Time Series Analysis. World J. Pediatr. WJP 2023, 19, 288–292. [Google Scholar] [CrossRef]
- Matava, C.T.; Tighe, N.T.G.; Baerschiger, R.; Wilder, R.T.; Correll, L.; Staffa, S.J.; Zurakowski, D.; Kato, M.A.; Meier, P.M.; Raman, V.; et al. Patient and Process Outcomes Among Pediatric Patients Undergoing Appendectomy During the COVID-19 Pandemic—An International Retrospective Cohort Study. Anesthesiology 2023, 139, 35–48. [Google Scholar] [CrossRef]
- Li, J.; Lai, S.; Gao, G.F.; Shi, W. The Emergence, Genomic Diversity and Global Spread of SARS-CoV-2. Nature 2021, 600, 408–418. [Google Scholar] [CrossRef]
- Ligo, A.K.; Mahoney, E.; Cegan, J.; Trump, B.D.; Jin, A.S.; Kitsak, M.; Keenan, J.; Linkov, I. Relationship among State Reopening Policies, Health Outcomes and Economic Recovery through First Wave of the COVID-19 Pandemic in the U.S. PLoS ONE 2021, 16, e0260015. [Google Scholar] [CrossRef] [PubMed]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of Public Health Measures in Reducing the Incidence of COVID-19, SARS-CoV-2 Transmission, and COVID-19 Mortality: Systematic Review and Meta-Analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef] [PubMed]
- Mirante, V.G.; Mazzi, G.; Bevivino, G.; Parmeggiani, F.; Iori, G.; Sassatelli, R. How an Endoscopy Unit Changed and Was Partially Converted into an ICU during COVID-19 Emergency in a Tertiary Referral Hospital of Northern Italy. Dig. Liver Dis. 2021, 53, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef]
- Elliott, B.M.; Witcomb Cahill, H.; Harmston, C. Paediatric Appendicitis: Increased Disease Severity and Complication Rates in Rural Children. ANZ J. Surg. 2019, 89, 1126–1132. [Google Scholar] [CrossRef]
- To, T.; Langer, J.C. Does Access to Care Affect Outcomes of Appendicitis in Children?—A Population-Based Cohort Study. BMC Health Serv. Res. 2010, 10, 250. [Google Scholar] [CrossRef][Green Version]
- Putnam, L.R.; Tsao, K.; Nguyen, H.T.; Kellagher, C.M.; Lally, K.P.; Austin, M.T. The Impact of Socioeconomic Status on Appendiceal Perforation in Pediatric Appendicitis. J. Pediatr. 2016, 170, 156–160.e1. [Google Scholar] [CrossRef]
- Wang, L.; Haberland, C.; Thurm, C.; Bhattacharya, J.; Park, K.T. Health Outcomes in US Children with Abdominal Pain at Major Emergency Departments Associated with Race and Socioeconomic Status. PLoS ONE 2015, 10, e0132758. [Google Scholar] [CrossRef][Green Version]
- Neufeld, M.Y.; Bauerle, W.; Eriksson, E.; Azar, F.K.; Evans, H.L.; Johnson, M.; Lawless, R.A.; Lottenberg, L.; Sanchez, S.E.; Simianu, V.V.; et al. Where Did the Patients Go? Changes in Acute Appendicitis Presentation and Severity of Illness during the Coronavirus Disease 2019 Pandemic: A Retrospective Cohort Study. Surgery 2021, 169, 808–815. [Google Scholar] [CrossRef]
- Köhler, F.; Acar, L.; van den Berg, A.; Flemming, S.; Kastner, C.; Müller, S.; Diers, J.; Germer, C.-T.; Lock, J.F.; L’hoest, H.; et al. Impact of the COVID-19 Pandemic on Appendicitis Treatment in Germany-a Population-Based Analysis. Langenbecks Arch. Surg. 2021, 406, 377–383. [Google Scholar] [CrossRef] [PubMed]
- van Amstel, P.; El Ghazzaoui, A.; Hall, N.J.; Wester, T.; Morini, F.; van der Lee, J.H.; Singer, G.; Pierro, A.; Zani, A.; Gorter, R.R.; et al. Paediatric Appendicitis: International Study of Management in the COVID-19 Pandemic. Br. J. Surg. 2022, 109, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Baker, T.; Schell, C.O.; Petersen, D.B.; Sawe, H.; Khalid, K.; Mndolo, S.; Rylance, J.; McAuley, D.F.; Roy, N.; Marshall, J.; et al. Essential Care of Critical Illness Must Not Be Forgotten in the COVID-19 Pandemic. Lancet Lond. Engl. 2020, 395, 1253–1254. [Google Scholar] [CrossRef] [PubMed]
- Sachs, J.D.; Karim, S.S.A.; Aknin, L.; Allen, J.; Brosbøl, K.; Colombo, F.; Barron, G.C.; Espinosa, M.F.; Gaspar, V.; Gaviria, A.; et al. The Lancet Commission on Lessons for the Future from the COVID-19 Pandemic. Lancet Lond. Engl. 2022, 400, 1224–1280. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial Impact of COVID-19. Diabetes Metab. Syndr. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Salö, M.; Friman, G.; Stenström, P.; Ohlsson, B.; Arnbjörnsson, E. Appendicitis in Children: Evaluation of the Pediatric Appendicitis Score in Younger and Older Children. Surg. Res. Pract. 2014, 2014, 438076. [Google Scholar] [CrossRef]
- Omling, E.; Salö, M.; Saluja, S.; Bergbrant, S.; Olsson, L.; Persson, A.; Björk, J.; Hagander, L. Nationwide Study of Appendicitis in Children. Br. J. Surg. 2019, 106, 1623–1631. [Google Scholar] [CrossRef]
- Dexter, F.; Parra, M.C.; Brown, J.R.; Loftus, R.W. Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management. Anesth. Analg. 2020, 131, 37–42. [Google Scholar] [CrossRef]
- Myles, P.S.; Maswime, S. Mitigating the Risks of Surgery during the COVID-19 Pandemic. Lancet 2020, 396, 2–3. [Google Scholar] [CrossRef]
- Kim, W.G.; Brown, S.D.; Johnston, P.R.; Nagler, J.; Jarrett, D.Y. Emergency Pediatric Radiology Imaging Trends for Non-COVID-19-Related Illnesses through Different Stages of the Pandemic. Emerg. Radiol. 2022, 29, 1–8. [Google Scholar] [CrossRef]
- Sideris, G.A.; Nikolakea, M.; Karanikola, A.-E.; Konstantinopoulou, S.; Giannis, D.; Modahl, L. Imaging in the COVID-19 Era: Lessons Learned during a Pandemic. World J. Radiol. 2021, 13, 192–222. [Google Scholar] [CrossRef] [PubMed]
- Keesara, S.; Jonas, A.; Schulman, K. COVID-19 and Health Care’s Digital Revolution. N. Engl. J. Med. 2020, 382, e82. [Google Scholar] [CrossRef] [PubMed]
- Hjelm, N.M. Benefits and Drawbacks of Telemedicine. J. Telemed. Telecare 2005, 11, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Tankel, J.; Keinan, A.; Blich, O.; Koussa, M.; Helou, B.; Shay, S.; Zugayar, D.; Pikarsky, A.; Mazeh, H.; Spira, R.; et al. The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-Centre Study. World J. Surg. 2020, 44, 2458–2463. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Mehl, S.C.; Hawes, E.E.; Lino, A.S.; Rialon, K.L.; Murray, K.O.; Ronca, S.E. SARS-CoV-2 Infection Is Not Associated with Pediatric Appendicitis. Pediatr. Infect. Dis. J. 2022, 41, e321–e323. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, A.; Sturgill, M.; Whitley-Williams, P.; Lee, Y.-H.; Esochaghi, C.; Rajasekhar, H.; Olson, B.; Gaur, S. Pediatric COVID-19 and Appendicitis: A Gut Reaction to SARS-CoV-2? Pediatr. Infect. Dis. J. 2021, 40, e49–e55. [Google Scholar] [CrossRef]
- Nepogodiev, D.; Bhangu, A.; Glasbey, J.C.; Li, E.; Omar, O.M.; Simoes, J.F.; Abbott, T.E.; Alser, O.; Arnaud, A.P.; Bankhead-Kendall, B.K.; et al. Mortality and Pulmonary Complications in Patients Undergoing Surgery with Perioperative SARS-CoV-2 Infection: An International Cohort Study. Lancet 2020, 396, 27–38. [Google Scholar] [CrossRef]
- Nepogodiev, D. Favourable Perioperative Outcomes for Children with SARS-CoV-2. Br. J. Surg. 2020, 107, e644–e645. [Google Scholar] [CrossRef]
- Mehl, S.C.; Loera, J.M.; Shah, S.R.; Vogel, A.M.; Fallon, S.C.; Glover, C.D.; Monson, L.A.; Enochs, J.A.; Hollier, L.H.; Lopez, M.E. Favorable Postoperative Outcomes for Children with COVID-19 Infection Undergoing Surgical Intervention: Experience at a Free-Standing Children’s Hospital. J. Pediatr. Surg. 2021, 56, 2078–2085. [Google Scholar] [CrossRef]
- Saynhalath, R.; Alex, G.; Efune, P.N.; Szmuk, P.; Zhu, H.; Sanford, E.L. Anesthetic Complications Associated with Severe Acute Respiratory Syndrome Coronavirus 2 in Pediatric Patients. Anesth. Analg. 2021, 133, 483–490. [Google Scholar] [CrossRef]
- Glasbey, J.; The COVIDSurg and GlobalSurg Collaboratives. Peri-operative Outcomes of Surgery in Children with SARS-CoV-2 Infection. Anaesthesia 2022, 77, 108–109. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization-Multisystem Inflammatory Syndrome in Children and Adolescents with COVID-19. Available online: https://www.who.int/publications-detail-redirect/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (accessed on 15 April 2023).
- Ahmed, M.; Advani, S.; Moreira, A.; Zoretic, S.; Martinez, J.; Chorath, K.; Acosta, S.; Naqvi, R.; Burmeister-Morton, F.; Burmeister, F.; et al. Multisystem Inflammatory Syndrome in Children: A Systematic Review. EClinicalMedicine 2020, 26, 100527. [Google Scholar] [CrossRef] [PubMed]
- Son, M.B.F.; Burns, J.C.; Newburger, J.W. A New Definition for Multisystem Inflammatory Syndrome in Children. Pediatrics 2023, 151, e2022060302. [Google Scholar] [CrossRef]
- Hameed, S.; Elbaaly, H.; Reid, C.E.L.; Santos, R.M.F.; Shivamurthy, V.; Wong, J.; Jogeesvaran, K.H. Spectrum of Imaging Findings at Chest Radiography, US, CT, and MRI in Multisystem Inflammatory Syndrome in Children Associated with COVID-19. Radiology 2021, 298, E1–E10. [Google Scholar] [CrossRef] [PubMed]
- Nurnaningsih; Danudibroto, G.I.; Rusmawatiningtyas, D.; Kumara, I.F.; Makrufardi, F.; Widowati, T. Acute Appendicitis in Pediatric Patients with Coronavirus Disease 2019 (COVID-19): A Case Series from a Developing Country’s Tertiary Hospital. Ann. Med. Surg. 2012 2022, 74, 103315. [Google Scholar] [CrossRef]
- Lo Vecchio, A.; Garazzino, S.; Smarrazzo, A.; Venturini, E.; Poeta, M.; Berlese, P.; Denina, M.; Meini, A.; Bosis, S.; Galli, L.; et al. Factors Associated with Severe Gastrointestinal Diagnoses in Children With SARS-CoV-2 Infection or Multisystem Inflammatory Syndrome. JAMA Netw. Open 2021, 4, e2139974. [Google Scholar] [CrossRef]
- Alotaibi, M.A.; Alhumaidan, W.; Alotaibi, A.; Alotaibi, A.M. Pediatric Appendicitis in Times of COVID-19: Think MIS-C. J. Pediatr. Surg. Case Rep. 2022, 77, 102151. [Google Scholar] [CrossRef]
- Trevisan, M.; Amaddeo, A.; Taddio, A.; Boscarelli, A.; Barbi, E.; Cozzi, G. Case Report: Simil-Appendicitis Presentation May Precede Cardiac Involvement in MIS-C Patient. Front. Pediatr. 2022, 10, 832391. [Google Scholar] [CrossRef]
- Öcal Demir, S.; Tosun, Ö.; Öztürk, K.; Duyu, M.; Bucak, A.; Akkuş, G.; Bayraktar, A.C.; Demirel, H.N.; Arslanoğlu, S.; Ovali, F. SARS-CoV-2 Associated Multisystem Inflammatory Syndrome in Children (MIS-C). A Single Center’s Experience. Minerva Pediatr. 2021. [Google Scholar] [CrossRef]
- Drake, F.T.; Mottey, N.E.; Farrokhi, E.T.; Florence, M.G.; Johnson, M.G.; Mock, C.; Steele, S.R.; Thirlby, R.C.; Flum, D.R. Time to Appendectomy and Risk of Perforation in Acute Appendicitis. JAMA Surg. 2014, 149, 837–844. [Google Scholar] [CrossRef]
- American College of Surgeons-COVID-19 Guidelines for Triage of Emergency General Surgery Patients. Available online: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/elective-case/emergency-surgery/ (accessed on 15 April 2023).
- Kvasnovsky, C.L.; Shi, Y.; Rich, B.S.; Glick, R.D.; Soffer, S.Z.; Lipskar, A.M.; Dolgin, S.; Bagrodia, N.; Hong, A.; Prince, J.M.; et al. Limiting Hospital Resources for Acute Appendicitis in Children: Lessons Learned from the U.S. Epicenter of the COVID-19 Pandemic. J. Pediatr. Surg. 2021, 56, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Ghazwani, S.M. Moving to Medical Treatment for COVID-19 Influence on Pediatric Appendicitis: A Meta-Analysis. Cureus 2022, 14, e32601. [Google Scholar] [CrossRef]
- De Simone, B.; Chouillard, E.; Di Saverio, S.; Pagani, L.; Sartelli, M.; Biffl, W.L.; Coccolini, F.; Pieri, A.; Khan, M.; Borzellino, G.; et al. Emergency Surgery during the COVID-19 Pandemic: What You Need to Know for Practice. Ann. R. Coll. Surg. Engl. 2020, 102, 323–332. [Google Scholar] [CrossRef] [PubMed]
- The Surgical Royal Colleges of the United Kingdom and Ireland-Guidance for Surgeons Working during the COVID-19 Pandemic. Available online: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/ (accessed on 15 April 2023).
- RIFT Study Group on behalf of the West Midlands Research Collaborative. Appendicitis Risk Prediction Models in Children Presenting with Right Iliac Fossa Pain (RIFT Study): A Prospective, Multicentre Validation Study. Lancet Child Adolesc. Health 2020, 4, 271–280. [Google Scholar] [CrossRef]
- Royal Australasian College of Surgeons-Guidelines for Safe Surgery: Open Versus Laparoscopic. A Rapid Review Commissioned by RACS. Available online: https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/news/covid19-information-hub/2020-04-15-recommendations-on-safe-surgery-laparoscopic-vs-open.pdf?rev=9f8f4faa7af243ccbd541b22b3efe27d&hash=CE951688EEC4654CFE59C02132CF5C3A (accessed on 15 April 2023).
- Andersson, R.E. The Natural History and Traditional Management of Appendicitis Revisited: Spontaneous Resolution and Predominance of Prehospital Perforations Imply That a Correct Diagnosis Is More Important than an Early Diagnosis. World J. Surg. 2007, 31, 86–92. [Google Scholar] [CrossRef]
- Livingston, E.H.; Woodward, W.A.; Sarosi, G.A.; Haley, R.W. Disconnect between Incidence of Nonperforated and Perforated Appendicitis: Implications for Pathophysiology and Management. Ann. Surg. 2007, 245, 886–892. [Google Scholar] [CrossRef] [PubMed]
- van den Bogaard, V.A.B.; Euser, S.M.; van der Ploeg, T.; de Korte, N.; Sanders, D.G.M.; de Winter, D.; Vergroesen, D.; van Groningen, K.; de Winter, P. Diagnosing Perforated Appendicitis in Pediatric Patients: A New Model. J. Pediatr. Surg. 2016, 51, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Öztaş, T.; Dursun, A.; Söğütçü, N.; Bilici, S. Unusual Histopathological Findings in Appendectomy Specimens Obtained from 1683 Pediatric Patients with Suspected Acute Appendicitis. Indian J. Surg. 2019, 81, 344–349. [Google Scholar] [CrossRef]
- Raffaele, A.; Cervone, A.; Ruffoli, M.; Cereda, E.; Avolio, L.; Parigi, G.B.; Riccipetitoni, G. Critical Factors Conditioning the Management of Appendicitis in Children during COVID-19 Pandemic: Experience from the Outbreak Area of Lombardy, Italy. Br. J. Surg. 2020, 107, e529–e530. [Google Scholar] [CrossRef]
- Fisher, J.C.; Tomita, S.S.; Ginsburg, H.B.; Gordon, A.; Walker, D.; Kuenzler, K.A. Increase in Pediatric Perforated Appendicitis in the New York City Metropolitan Region at the Epicenter of the COVID-19 Outbreak. Ann. Surg. 2021, 273, 410–415. [Google Scholar] [CrossRef]
- Di Mauro, A.; Di Mauro, F.; De Nitto, S.; Rizzo, L.A.; Greco, C.; Stefanizzi, P.; Tafuri, S.; Baldassarre, M.T.; Laforgia, N. Social Media Interventions Strengthened COVID-19 Immunization Campaign. Front. Pediatr. 2022, 10, 869893. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X.; et al. Association of Public Health Interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020, 323, 1915. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, M.E.A.; Macias-Carlos, D.; Montoya, J.A.; Plant, A.; Neffa-Creech, D. Integrated Multicultural Media Campaign to Increase COVID-19 Education and Vaccination among Californians, 2021. Am. J. Public Health 2022, 112, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.C.; Backer, T.E.; Brubach, A. Creating the HHS COVID-19 Public Education Media Campaign: Applying Systems Change Learnings. J. Health Commun. 2022, 27, 201–207. [Google Scholar] [CrossRef] [PubMed]

| Author | Type of Study | Study Period | Year | Journal | Country | |
|---|---|---|---|---|---|---|
| 1 | Köhler et al. [11] | Systematic Review and Meta-analysis | February 2021 (date of search) | 2021 | Int. J. Surg.; 95:106148 | Germany |
| 2 | Delgado-Miguel et al. [15] | Retrospective Cohort | January 2017–March 2020 (C) * March–December 2020 | 2021 | J. Healthc. Qual. Res.; 37(4):225–230 | Spain |
| 3 | Sheath et al. [16] | Retrospective Cohort | March–June 2019 (C) March–June 2020 | 2021 | J. Paediatr. Child Health; 57(7):986–989 | United Kingdom (UK) |
| 4 | Li et al. [17] | Retrospective Cohort | 1 March–30 June 2019 (C) 1 March–30 June 2020 | 2022 | J. Pediatr. Surg.; 57(5):861–865 | Canada |
| 5 | Delgado-Miguel et al. [18] | Retrospective Cohort | 9 March–13 April 2015–2019 (C) 9 March–13 April 2020 | 2022 | Eur. J. Pediatr. Surg.; 32(3):268–273 | Spain |
| 6 | Ayyıldız et al. [19] | Retrospective Cohort | 1 May 2019–29 February 2020 (C) 1 March–31 December 2020 | 2022 | Ulus Travma Acil Cerrahi Derg; 28(12):1674–1681 | Turkey |
| 7 | ANZSCRAFT Collaborative [20] | Retrospective Cohort | 20 March–30 April 2018, 2019 (C) 20 March–30 April 2020 | 2022 | ANZ J. Surg.; 92(4):736–741 | Australia, New Zealand |
| 8 | Nassiri et al. [21] | Retrospective Cohort | 23 March–31 August 2019 (C) 23 March–31 August 2020 | 2022 | J. Am. Coll. Emerg. Physicians Open; 3(2):e12722 | United States of America (USA) |
| 9 | Toro Rodríguez et al. [22] | Retrospective Cohort | January 2019–February 2020 (C) March 2020–December 2020 | 2022 | Cir. Pediatr.; 35(3):131–134 | Spain |
| 10 | Sullivan et al. [6] | Retrospective Cohort | 18 March–31 May 2019 (C) 18 March–31 May 2020 | 2022 | J. Surg. Res.; 279:299–303 | USA |
| 11 | Motazedian et al. [23] | Systematic Review and Meta-analysis | 1995–December 2019 (C) December 2019–January 2021 | 2021 | Arch. Acad. Emerg. Med.; 10(1):e3 | Iran |
| 12 | La Pergola et al. [24] | Retrospective Cohort | 20 February–20 April 2017–2019 (C) 20 February–20 April 2020 | 2020 | Front. Pediatr.; 8:600320 | Italy |
| 13 | Gaitero Tristán et al. [25] | Retrospective Cohort | January–September 2019 (C) 21 March 2020–6 May 2020 | 2021 | Pediatr. Emerg. Care; 37(3):185–190 | Spain |
| 14 | Esparaz et al. [26] | Retrospective Cohort | October 2019–February 2020 (C) March–May 2020 | 2021 | J. Surg. Res.; 268:263–266 | USA |
| 15 | Ali et al. [7] | Retrospective Cohort | March–May 2019 (C) March–May 2020 | 2020 | J. Ayub Med. Coll. Abbottabad; 32(Suppl 1)(4):S621–S624 | Pakistan |
| 16 | Quaglietta et al. [27] | Retrospective Cohort | February 2018–June 2019 (C) February 2020–June 2021 | 2023 | J. Pediatr. Surg.; 58(5):931–938 | Canada |
| 17 | Taşçı et al. [28] | Retrospective Cohort | 20 December 2019–10 March 2020 (C) 11 March 2020–1 June 2020 | 2022 | Ulus Travma Acil Cerrahi Derg; 28(8):1095–1099 | Turkey |
| 18 | Horst et al. [29] | Retrospective Cohort | 1 March–31 May 2019 (C) 1 March–31 May 2020 | 2021 | Pediatr. Radiol.; 51(11):1991–1999 | USA |
| 19 | Head et al. [30] | Retrospective Cohort | December 2019–15 March 2020 (C) 15 March 2020–June 2020 | 2021 | Am. Surg.; 26:31348211067995 | USA |
| 20 | Snapiri et al. [13] | Case Series/Retrospective Cohort | 1 March–30 April 2019 (C) 1 March–30 April 2020 | 2020 | Acta Paediatr.; 109(8):1672–1676 | Israel |
| 21 | Moratilla Lapeña et al. [31] | Retrospective Cohort | 14 March–20 April 2019 (C) 14 March–20 April 2020 | 2021 | Cir. Pediatr.; 34(2):85–89 | Spain |
| 22 | Iantorno et al. [32] | Retrospective Cohort | 1 April 2020–31 March 2021 | 2023 | Surgery; 173(4):936–943 | USA |
| 23 | Schäfer et al. [33] | Retrospective Cohort | 20 March–31 May 2018, 2019 (C) 20 March–31 May 2020 | 2021 | Front. Pediatr.; 9:683607 | Germany |
| 24 | Yock-Corrales et al. [34] | Prospective Multinational Multicenter Cohort | 1 July–11 August 2020 | 2021 | Pediatr. Infect. Dis. J.; 40(10):e364–e369 | Peru, Costa Rica, Argentina, Colombia, Mexico |
| 25 | Tan et al. [35] | Prospective Comparative Cohort | April 2020–January 2022 | 2022 | Pediatr. Surg. Int.; 39(1):60 | Singapore |
| 26 | Rethi et al. [8] | Retrospective Cohort | 1 March–30 November 2019 (C) 1 March–30 November 2019 | 2022 | J. Emerg. Med.; 63(6):723–728 | USA |
| 27 | Theodorou et al. [36] | Retrospective Cohort | 19 March–19 September 2019 (C) 19 March–19 September 2020 | 2021 | J. Surg. Res.; 267:132–142 | USA |
| 28 | Gerall et al. [37] | Retrospective Cohort | 1 March–31 May 2019 (C) 1 March–31 May 2020 | 2021 | J. Pediatr. Surg.; 56(5):905–910 | USA |
| 29 | Farooq et al. [38] | Case-Control Study | April–September 2019 (C) April–September 2020 | 2021 | BMJ Paediatr. Open; 5(1):e001066 | Bangladesh |
| 30 | Pawelczyk et al. [39] | Retrospective Cohort | 1 January–31 December 2019 (C) 1 January–December 2020 | 2021 | Sci. Rep.; 11(1):23999 | Poland |
| 31 | Percul et al. [40] | Retrospective Cohort | 20 March–20 August 2019 (C) 20 March–20 August 2020 | 2021 | Arch Argent Pediatr.; 119(4):224–229 | Argentina |
| 32 | Ergün et al. [41] | Retrospective Cohort | 11 March–30 September 2017–2019 (C) 11 March–30 September 2020 | 2021 | Turk. J. Surg.; 37(4):318–323 | Turkey |
| 33 | Yap et al. [42] | Prospective Comparative Study | 1 May 2020–31 January 2021 | 2023 | J. Pediatr. Surg.: S0022–3468(23)00172–0 | Singapore |
| 34 | Bethell et al. [43] | Prospective Multicenter Observational Cohort | 13 March–18 June 2017 (C) 1 April–31 July 2020 | 2022 | J. Pediatr. Surg.; 57(10):380–385 | UK, Ireland |
| 35 | Vansevičienė et al. [44] | Retrospective Cohort | 16 March–16 June 2019 (C) 16 March–16 June 2020 | 2021 | Medicina (Kaunas); 57(11):1234 | Lithuania |
| 36 | Patel et al. [45] | Retrospective Cohort | 3 March–30 June 2019 (C) 3 March–30 June 2020 | 2021 | Ann. Med. Surg. (Lond.); 71:102901 | UK |
| 37 | Montalva et al. [46] | Retrospective Cohort | 20 January–17 March 2020 (C) 17 March 2020–11 May 2020 | 2020 | Pediatr. Surg. Int.; 36(12):1397–1405 | France |
| 38 | Öztaş et al. [47] | Retrospective Cohort | March 2019–February 2020 (C) March 2020–February 2021 | 2023 | Ann. Pediatr. Surg.; 19(1):3 | Turkey |
| 39 | Dass et al. [48] | Prospective Cohort | 1 April–August 2019 (C) 1 April–31 August 2020 | 2023 | Afr. J. Paediatr. Surg.; 20(1):40–45 | UK |
| 40 | Gürünlüoglu et al. [49] | Prospective Cohort | December 2018–May 2021 | 2023 | Afr. J. Paediatr. Surg.; 20(2):130–137 | Turkey |
| 41 | Del Giorgio et al. [50] | Retrospective Cohort | March 2016–March 2020 (C) April 2020–March 2021 | 2023 | World J. Pediatr.; 19(3):288–292 | Canada |
| 42 | Matava et al. [51] | Retrospective, International Multicenter Cohort | April–May 2019 (C) April–May 2020 | 2023 | Anesthesiology; Online ahead of print | Canada, Australia, USA |
| 1 | Public health and social measures |
| 2 | Fear of exposure by parents/caregivers/patients/medical staff |
| 3 | Telemedicine use |
| 4 | COVID-19-positive children with suspected appendicitis |
| 5 | Recurrent appendicitis after non-operative management |
| 6 | Delayed primary operative management |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantalos, G.; Papachristidou, S.; Mavrigiannaki, E.; Zavras, N.; Vaos, G. Reasons for Delayed Diagnosis of Pediatric Acute Appendicitis during the COVID-19 Era: A Narrative Review. Diagnostics 2023, 13, 2571. https://doi.org/10.3390/diagnostics13152571
Pantalos G, Papachristidou S, Mavrigiannaki E, Zavras N, Vaos G. Reasons for Delayed Diagnosis of Pediatric Acute Appendicitis during the COVID-19 Era: A Narrative Review. Diagnostics. 2023; 13(15):2571. https://doi.org/10.3390/diagnostics13152571
Chicago/Turabian StylePantalos, George, Smaragda Papachristidou, Eleftheria Mavrigiannaki, Nikolaos Zavras, and George Vaos. 2023. "Reasons for Delayed Diagnosis of Pediatric Acute Appendicitis during the COVID-19 Era: A Narrative Review" Diagnostics 13, no. 15: 2571. https://doi.org/10.3390/diagnostics13152571
APA StylePantalos, G., Papachristidou, S., Mavrigiannaki, E., Zavras, N., & Vaos, G. (2023). Reasons for Delayed Diagnosis of Pediatric Acute Appendicitis during the COVID-19 Era: A Narrative Review. Diagnostics, 13(15), 2571. https://doi.org/10.3390/diagnostics13152571






