Characteristics of Clinically Classified Oral Lichen Planus in Optical Coherence Tomography: A Descriptive Case-Series Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. OCT Miniprobe
2.2. Study Protocol
2.3. Classification Parameter
3. Results
3.1. Reticular OLP
3.2. Reticular Atrophic OLP
3.3. Atrophic OLP
3.4. Atrophic Erosive OLP
3.5. Plaque-like OLP
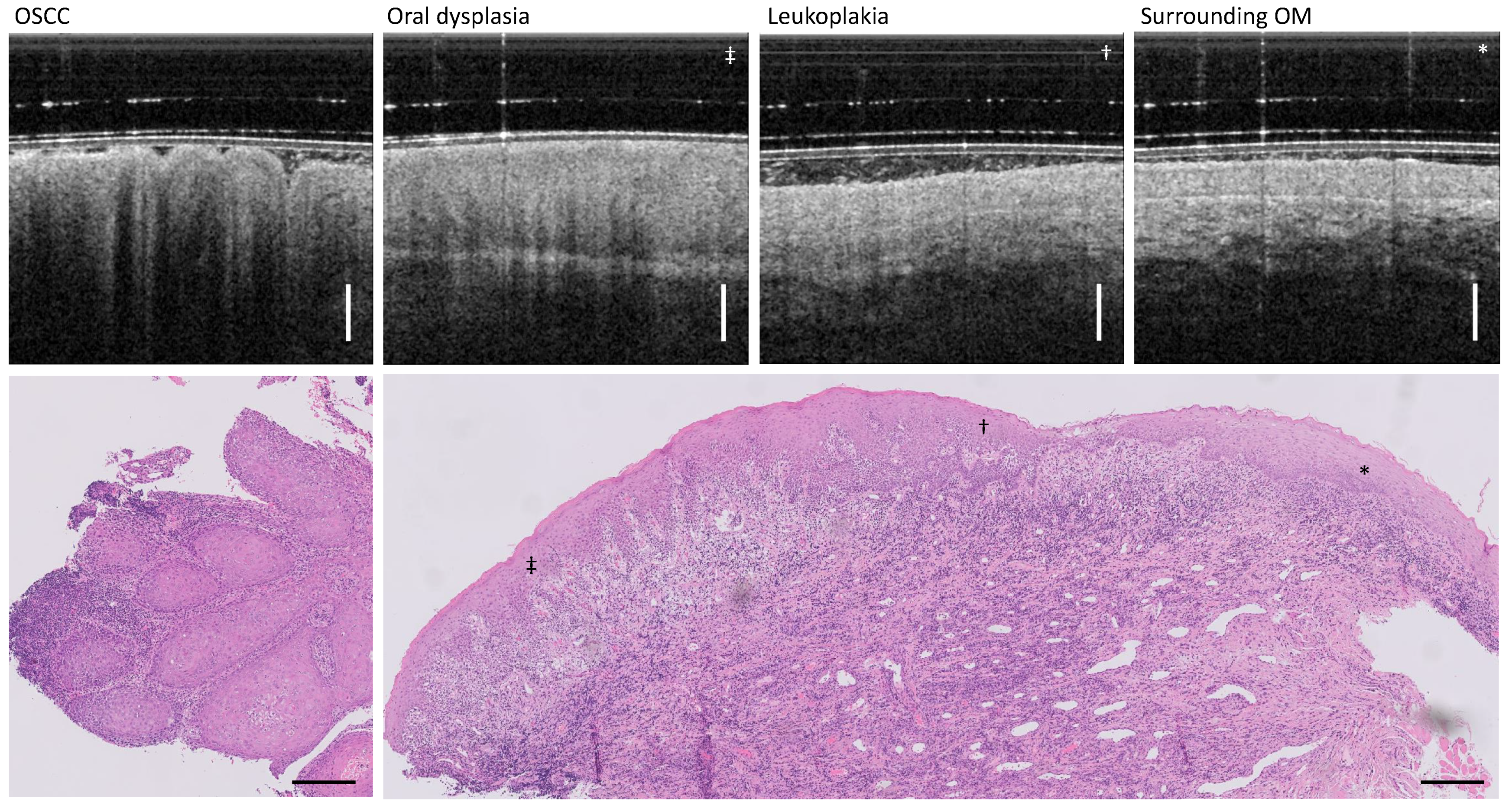
3.6. Leukoplakia and OSCC
3.7. Histological Findings
4. Discussion
5. Summary and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| A-scan | Amplitude scan (1D OCT depth scan) |
| B-scan | Brightness scan (2D OCT scan, cross-section) |
| GRIN | Gradient index |
| FOV | Field of view |
| FWHM | Full width half maximum |
| OC | Oral cancer |
| OCT | Optical coherence tomography |
| OSCC | Oral squamous cell carcinoma |
| OLP | Oral lichen planus |
| OM | Oral mucosa |
| EP | Epithelium |
| LP | Lamina propria |
| BM | Basement membrane |
Appendix A
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| I | female | 67 | OLP: left buccal mucosa mouth xerostomia (dry mouth); thrombosis; thyroid and stomach disorder; keratoconjunctivitis sicca (eye dryness); osteoporosis; removed ovaries | Hydrocortisone oral ointment |
| II | female | 60 | OLP: right buccal mucosa; hypertension; thyroid disorder; | Losartan-ratiopharm 50 mg (antihypertensive drug); Triamcinolone ointment 0.1% (glucocorticoid); Micotar ointment (antifungal drug) |
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| III | male | 77 | OLP: right buccal mucosa; hypertension; unusual bleeding or bruising; osteoporosis; asthma; COPD; birch allergy; immunodeficiency because of the prostate cancer irradiation (2011); gallbladder operation | Antihypertensive drugs; Pantoprazol |
| IV | male | 80 | OLP: right buccal mucosa; hypertension | Antihypertensive drugs; Celestone Liquidum 0.5 mg/mL N1 (glucocorticoid drug) |
| V | female | 52 | OLP: left buccal mucosa hypertension; allergy to benzoyl peroxide, adhesives, ceramic restorations, perfume fragrances | antihypertensive drug-VIACORAM 7 mg/5 mg; Celestone Liquidum 0.5 mg/mL N1 (glucocorticoid drug) |
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| VI | male | 64 | OLP: left buccal mucosa; hypertension; thyroid disorder; removal of the thyroid (1990); allergy (hay fever) | L-Thyroxin; Amlodipin; Enalapril; Simvastatin; Omeprazol; Triamcinolone injections |
| VII | male | 60 | OLP: right buccal mucosa | Triamcinolon acetat 0.1; Micotar ointment |
| VIII | female | 82 | OLP: right buccal mucosa; Hypertension; Circulatory disorder; Diabetes mellitus type 2; Osteoporosis; Rheumatoid arthritis; Allergy to analgesics and metals | Celestone Liquidum 0.5; Micotar ointment; Celebrex; Carmen; Carvedilol; Candecor; Forasamid; Dekristol; Venostatin |
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| IX | female | 69 | OLP: right buccal mucosa; Hypertension; Heart pacemaker; Secondary haemorrhage; Diabetes mellitus type 2; Asthma; Thyroid disorder; Myositis; Hephritis; Allergy to AB, Latex, food; Rheumatoid arthritis | Triamcinolon acetat 0.1%; Micotar ointment; Analgesics; Antihypertensive drugs; Antirheumatic agent |
| X | female | 84 | OLP: right buccal mucosa (erosive); unusual bleeding or bruising; artificial joints since 2009 and 2013 (hip joint); glaucoma; intestine; gallbladder operation; asthma; chronic bronchitis; allergy to latex and opiates | Cortisone spray |
| XI | female | 51 | n/a | n/a |
| XII | female | 67 | OLP: right buccal mucosa | Triamcinolone ointment 0.1% (glucocorticoid); Micotar ointment (antifungal drug) |
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| XIII | female | 48 | OLP: right buccal mucosa; operation of the right arm | Propolis; clove oil; Ceterizin (anti-histamine agent) |
| Nb | Gender | Age | Disorders | Medication |
|---|---|---|---|---|
| XIV | female | 60 | Leukoplakia: tongue (right side); hypertension; varicose veins operation (left side) | Valsacor |
| XV | male | 66 | Leukoplakia: left buccal mucosa and regio 37–38; hypertension; heart attack; apoplexy; thrombosis; unusual bleeding or bruising; secondary bleeding; diabetes mellitus type 2; thyroid disorder; artificial joints since 2014 | Insulin; Antihypertensive drug |
References
- Montero, P.H.; Patel, S.G. Cancer of the Oral Cavity. Surg. Oncol. Clin. N. Am. 2015, 24, 491–508. [Google Scholar] [CrossRef] [Green Version]
- Shield, K.D.; Ferlay, J.; Jemal, A.; Sankaranarayanan, R.; Chaturvedi, A.K.; Bray, F.; Soerjomataram, I. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J. Clin. 2017, 67, 51–64. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cancer Fact Sheets—Lip, Oral Cavity; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Radwan-Oczko, M.; Sokół, I.; Babuśka, K.; Owczarek-Drabińska, J.E. Prevalence and Characteristic of Oral Mucosa Lesions. Symmetry 2022, 14, 307. [Google Scholar] [CrossRef]
- Ikeda, N.; Handa, Y.; Khim, S.P.; Durward, C.; Axéll, T.; Mizuno, T.; Fukano, H.; Kawai, T. Prevalence study of oral mucosal lesions in a selected Cambodian population. Community Dent. Oral Epidemiol. 1995, 23, 49–54. [Google Scholar] [CrossRef]
- Li, C.; Tang, X.; Zheng, X.; Ge, S.; Wen, H.; Lin, X.; Chen, Z.; Lu, L. Global Prevalence and Incidence Estimates of Oral Lichen Planus: A Systematic Review and Meta-Analysis. JAMA Dermatol. 2020, 156, 172–181. [Google Scholar] [CrossRef]
- González-Moles, M.Á.; Warnakulasuriya, S.; González-Ruiz, I.; González-Ruiz, L.; Ayén, Á.; Lenouvel, D.; Ruiz-Ávila, I.; Ramos-García, P. Worldwide prevalence of oral lichen planus: A systematic review and meta-analysis. Oral Dis. 2021, 27, 813–828. [Google Scholar] [CrossRef]
- Al-Hashimi, I.; Schifter, M.; Lockhart, P.B.; Wray, D.; Brennan, M.; Migliorati, C.A.; Axéll, T.; Bruce, A.J.; Carpenter, W.; Eisenberg, E.; et al. Oral lichen planus and oral lichenoid lesions: Diagnostic and therapeutic considerations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 103, S25.e1–S25.e12. [Google Scholar] [CrossRef] [PubMed]
- Tsushima, F.; Sakurai, J.; Uesugi, A.; Oikawa, Y.; Ohsako, T.; Mochizuki, Y.; Hirai, H.; Kayamori, K.; Harada, H. Malignant transformation of oral lichen planus: A retrospective study of 565 Japanese patients. BMC Oral Health 2021, 21, 298. [Google Scholar] [CrossRef]
- Fernández-González, F.; Vázquez-Álvarez, R.; Reboiras-López, D.; Gándara-Vila, P.; García-García, A.; Gándara-Rey, J.M. Histopathological findings in oral lichen planus and their correlation with the clinical manifestations. Med. Oral Patol. Oral Cir. Bucal 2011, 16, 1–6. [Google Scholar] [CrossRef]
- Giuliani, M.; Troiano, G.; Cordaro, M.; Corsalini, M.; Gioco, G.; Lo Muzio, L.; Pignatelli, P.; Lajolo, C. Rate of malignant transformation of oral lichen planus: A systematic review. Oral Dis. 2019, 25, 693–709. [Google Scholar] [CrossRef]
- Arduino, P.G.; Magliano, A.; Gambino, A.; Macciotta, A.; Carbone, M.; Conrotto, D.; Karimi, D.; Carrozzo, M.; Broccoletti, R. Risk of malignant transformation in 3173 subjects with histopathologically confirmed oral lichen planus: A 33-year cohort study in Northern Italy. Cancers 2021, 13, 5740. [Google Scholar] [CrossRef]
- Ruiz Roca, J.A.; López Jornet, P.; Gómez García, F.J.; Marcos Aroca, P. Effect of Photobiomodulation on Atrophic–Erosive Clinical Forms of Oral Lichen Planus: A Systematic Review. Dent. J. 2022, 10, 221. [Google Scholar] [CrossRef]
- Tenore, G.; Mohsen, A.; Rocchetti, F.; Rossi, G.; Cassoni, A.; Battisti, A.; Della Monaca, M.; Di Gioia, C.R.T.; De Felice, F.; Botticelli, A.; et al. Risk of Oral Squamous Cell Carcinoma in One Hundred Patients with Oral Lichen Planus: A Follow-Up Study of Umberto I University Hospital of Rome. Cancers 2023, 15, 3004. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Ramos-García, P.; González-Moles, M.Á. Malignant Transformation of Oral Lichen Planus—Systematic Review. Oral Dis. 2023, 3, 295–306. [Google Scholar] [CrossRef]
- Van Der Meij, E.H.; Schepman, K.P.; Smeele, L.E.; Van Der Wal, J.E.; Bezemer, P.D.; Van Der Waal, I. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 307–310. [Google Scholar] [CrossRef]
- Scully, C.; Beyli, M.; Ferreiro, M.C.; Ficarra, G.; Gill, Y.; Griffiths, M.; Holmstrup, P.; Mutlu, S.; Porter, S.; Wray, D. Update on oral lichen planus: Etiopathogenesis and management. Crit. Rev. Oral Biol. Med. 1998, 9, 86–122. [Google Scholar] [CrossRef] [PubMed]
- Haqiqi, M.A.; Pourmoshir, N.; Bereshneh, A.H. Clinical and Genetic Aspects of Oral Lichen Planus. Int. J. Biomed. Adv. Res. 2016, 7, 251–256. [Google Scholar] [CrossRef]
- Avon, S.L.; Klieb, H.B. Oral-Soft-Tissue Biopsy Overv. J. Can. Dent. Assoc. 2012, 78, 1–9. [Google Scholar]
- Rivera, C. Essentials of oral cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 11884–11894. [Google Scholar] [CrossRef]
- Kumaraswamy, K.L.; Vidhya, M.; Rao, P.K.; Mukanda, A. Oral biopsy: Oral pathologist’s perspective. J. Cancer Res. Ther. 2012, 8, 192–198. [Google Scholar] [CrossRef]
- Ridgeway, J.M.; Armstrong, W.B.; Guo, S.; Mahmood, U.; Su, J.; Jackson, R.P.; Shibuya, T.; Crumley, R.L.; Gu, M.; Chen, Z.; et al. In vivo optical coherence tomography of the human oral cavity and oropharynx. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 1074–1081. [Google Scholar]
- Leuci, S.; Coppola, N.; Turkina, A.; Bizzoca, M.E.; Favia, G.; Spagnuolo, G.; Mignogna, M.D. May velscope be deemed an opportunistic oral cancer screening by general dentists? A pilot study. J. Clin. Med. 2020, 9, 1754. [Google Scholar] [CrossRef]
- Ansari, U.H.; Wong, E.; Smith, M.; Singh, N.; Palme, C.E.; Smith, M.C.; Riffat, F. Validity of narrow band imaging in the detection of oral and oropharyngeal malignant lesions: A systematic review and meta-analysis. Head Neck 2019, 41, 2430–2440. [Google Scholar] [CrossRef]
- Bhatia, N.; Lalla, Y.; Vu, A.N.; Farah, C.S. Advances in optical adjunctive aids for visualisation and detection of oral malignant and potentially malignant lesions. Int. J. Dent. 2013, 2013, 194029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wessels, R.; De Bruin, D.M.; Faber, D.J.; Van Leeuwen, T.G.; Van Beurden, M.; Ruers, T.J. Optical biopsy of epithelial cancers by optical coherence tomography (OCT). Lasers Med. Sci. 2014, 29, 1297–1305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, R.S.; Sai Praveen, K.N. Optical coherence tomography in oral cancer: A transpiring domain. J. Cancer Res. Ther. 2017, 13, 883–888. [Google Scholar] [CrossRef] [PubMed]
- Gentile, E.; Maio, C.; Romano, A.; Laino, L.; Lucchese, A. The potential role of in vivo optical coherence tomography for evaluating oral soft tissue: A systematic review. J. Oral Pathol. Med. 2017, 46, 864–876. [Google Scholar] [CrossRef]
- Albrecht, M.; Schnabel, C.; Mueller, J.; Golde, J.; Koch, E.; Walther, J. In vivo endoscopic optical coherence tomography of the healthy human oral mucosa: Qualitative and quantitative image analysis. Diagnostics 2020, 10, 827. [Google Scholar] [CrossRef]
- Tsai, M.T.; Lee, C.K.; Lee, H.C.; Chen, H.M.; Chiang, C.P.; Wang, Y.M.; Yang, C.C. Differentiating oral lesions in different carcinogenesis stages with optical coherence tomography. J. Biomed. Opt. 2009, 14, 044028. [Google Scholar] [CrossRef] [Green Version]
- Wilder-Smith, P.; Lee, K.; Guo, S.; Zhang, J.; Osann, K.; Chen, Z.; Messadi, D. In vivo diagnosis of oral dysplasia and malignancy using optical coherence tomography: Preliminary studies in 50 patients. Lasers Surg. Med. 2009, 41, 353–357. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.K.; Chi, T.T.; Wu, C.T.; Tsai, M.T.; Chiang, C.P.; Yang, C.C.C.C. Diagnosis of oral precancer with optical coherence tomography. Biomed. Opt. Express 2012, 3, 1632. [Google Scholar] [CrossRef]
- Volgger, V.; Stepp, H.; Ihrler, S.; Kraft, M.; Leunig, A.; Patel, P.M.; Susarla, M.; Jackson, K.; Betz, C.S. Evaluation of optical coherence tomography to discriminate lesions of the upper aerodigestive tract. Head Neck 2012, 35, 1558–1566. [Google Scholar] [CrossRef]
- Jerjes, W.; Hamdoon, Z.; Yousif, A.A.; Al-Rawi, N.H.; Hoppper, C. Epithelial tissue thickness improves optical coherence tomography’s ability in detecting oral cancer. Photodiagnosis Photodyn Ther. 2019, 28, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, S.W.; Hwang, S.H. Efficacy of optical coherence tomography in the diagnosing of oral cancerous lesion: Systematic review and meta-analysis. Head Neck 2022, 45, 473–481. [Google Scholar] [CrossRef] [PubMed]
- James, B.L.; Sunny, S.P.; Heidari, A.E.; Ramanjinappa, R.D.; Lam, T.; Tran, A.V.; Kankanala, S.; Sil, S.; Tiwari, V.; Patrick, S.; et al. Validation of a point-of-care optical coherence tomography device with machine learning algorithm for detection of oral potentially malignant and malignant lesions. Cancers 2021, 13, 3583. [Google Scholar] [CrossRef]
- Carrard, V.C.; Van Der Waal, I. A clinical diagnosis of oral leukoplakia; A guide for dentists. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e59–e64. [Google Scholar] [CrossRef]
- Gambino, A.; Cabras, M.; Cafaro, A.; Broccoletti, R.; Carossa, S.; Hopper, C.; Chiusa, L.; El Haddad, G.; Porter, S.R.; Arduino, P.G. In-vivo usefulness of optical coherence tomography in atrophic-erosive oral lichen planus: Comparison between histopathological and ultrastructural findings. J. Photochem. Photobiol. B Biol. 2020, 211, 112009. [Google Scholar] [CrossRef] [PubMed]
- Gambino, A.; Cabras, M.; Cafaro, A.; Broccoletti, R.; Carossa, S.; Hopper, C.; Conrotto, D.; Porter, S.R.; Arduino, P.G. Preliminary evaluation of the utility of optical coherence tomography in detecting structural changes during photobiomodulation treatment in patients with atrophic-erosive oral lichen planus. Photodiagnosis Photodyn. Ther. 2021, 34, 102255. [Google Scholar] [CrossRef]
- Walther, J.; Golde, J.; Albrecht, M.; Quirk, B.C.; Scolaro, L.; Kirk, R.W.; Gruda, Y.; Schnabel, C.; Tetschke, F.; Joehrens, K.; et al. A Handheld Fiber-Optic Probe to Enable Optical Coherence Tomography of Oral Soft Tissue. IEEE Trans. Biomed. Eng. 2022, 69, 2276–2282. [Google Scholar] [CrossRef]
- Andreasen, J.O. Oral Lichen Planus: I. A clinical evaluation of 115 cases. Oral Surg. Oral Med. Oral Pathol. 1968, 25, 31–42. [Google Scholar] [CrossRef]
- Krupaa, R.J.; Sankari, S.L.; Masthan, K.M.; Rajesh, E. Oral lichen planus: An overview. J. Pharm. Bioallied Sci. 2015, 7, S158–S161. [Google Scholar] [CrossRef] [PubMed]
- Rotaru, D.I.; Sofineti, D.; Bolboacă, S.D.; Bulboacă, A.E. Diagnostic Criteria of oral lichen planus: A narrative review. Acta Clin. Croat. 2020, 59, 513–522. [Google Scholar] [CrossRef] [PubMed]
- Boorghani, M.; Gholizadeh, N.; Taghavi Zenouz, A.; Vatankhah, M.; Mehdipour, M. Oral lichen planus: Clinical features, etiology, treatment and management; a review of literature. J. Dent. Res. Dent. Clin. Dent. Prospect. 2010, 4, 3–9. [Google Scholar] [CrossRef]
- Andabak-Rogulj, A.; Vindiš, E.; Aleksijević, L.H.; Škrinjar, I.; Juras, D.V.; Aščić, A.; Brzak, B.L. Different Treatment Modalities of Oral Lichen Planus—A Narrative Review. Dent. J. 2023, 11, 26. [Google Scholar] [CrossRef]
- Di Stasio, D.; Lauritano, D.; Iquebal, H.; Romano, A.; Gentile, E.; Lucchese, A. Measurement of oral epithelial thickness by optical coherence tomography. Diagnostics 2019, 9, 90. [Google Scholar] [CrossRef] [Green Version]
- Panzarella, V.; Bartolone, A.; Coniglio, R.; Rodolico, V.; Maniscalco, L.; Capocasale, G.; Carbone, M.I.; Campisi, G. Diagnostic concordance between optical coherence tomography and histological investigations for immune-mediated desquamative gingivitis: Observational study. Int. J. Environ. Res. Public Health 2021, 18, 9095. [Google Scholar] [CrossRef]
- Tsai, M.T.; Chen, Y.; Lee, C.Y.; Huang, B.H.; Trung, N.H.; Lee, Y.J.; Wang, Y.L. Noninvasive structural and microvascular anatomy of oral mucosae using handheld optical coherence tomography. Biomed. Opt. Express 2017, 8, 5001–5012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walther, J.; Li, Q.; Villiger, M.; Farah, C.S.; Koch, E.; Karnowski, K.; Sampson, D.D. Depth-resolved birefringence imaging of collagen fiber organization in the human oral mucosa in vivo. Biomed. Opt. Express 2019, 10, 1942. [Google Scholar] [CrossRef]









| Parameter | Normal OM | Pathological OM |
|---|---|---|
| EP thickness 1 | distinct thickness | reduced thickness |
| Basement membrane | distinct demarcation | less/none demarcation |
| EP reflectivity 2 | highly translucent | altered backscattering |
| LP reflectivity 3 | highly reflective | reduced backreflection |
| Vascular network in LP | identifiable vascularization | altered vascularization |
| Pathology | Clinical Appearance | OCT Features |
|---|---|---|
| Reticular OLP | increased EP surface reflectivity | |
| homogeneous smooth surface | reduced LP reflectivity | |
| whitish keratinization | limited BM visibility | |
| inconspicious vessel network | ||
| Reticular atrophic OLP | EP surface hyperreflectivity | |
| inhomogeneous OM surface | reduced EP thickness | |
| whitish reticular keratinization | reduced LP reflectivity | |
| marginal reddened surface | vague BM visibility | |
| reduced layer differentiation | ||
| reduced nb. of large vessels | ||
| Atrophic OLP | EP hyporeflectivity | |
| inhomogeneous OM surface | no BM visibility | |
| predominant reddened surface | no layer differentiation | |
| enhanced vessel network | ||
| Atrophic erosive OLP | EP hyperreflectivity | |
| hyperkeratinization | reduced EP thickness | |
| ulcerative open wounds | limited BM visibility | |
| fibrin layer | reduced layer differentiation | |
| reduced nb. of large vessels | ||
| Plaque-like OLP | hyperreflective layer at EP | |
| hyperkeratinization | no BM visibility | |
| large whitish homogenous OM | no layer differentiation | |
| no vessel network identification | ||
| Leukoplakia | hyporeflective surface | |
| homogenous/inhomogeneous | distinct shadowing | |
| closed hyperkeratinization/ | no BM visibility | |
| interrupted hyperkeratinization | no layer differentiation | |
| no vessel network identification | ||
| OSCC | hyperreflective EP surface | |
| uneven interrupted surface | strongly reduced imaging depth | |
| floe-like hyperkeratinization | cloud-like layered structure | |
| distinct ulceration | distinct shadowing | |
| no BM and layer visibility | ||
| no vessel network identification |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gruda, Y.; Albrecht, M.; Buckova, M.; Haim, D.; Lauer, G.; Koch, E.; Joehrens, K.; Schnabel, C.; Golde, J.; Li, J.; et al. Characteristics of Clinically Classified Oral Lichen Planus in Optical Coherence Tomography: A Descriptive Case-Series Study. Diagnostics 2023, 13, 2642. https://doi.org/10.3390/diagnostics13162642
Gruda Y, Albrecht M, Buckova M, Haim D, Lauer G, Koch E, Joehrens K, Schnabel C, Golde J, Li J, et al. Characteristics of Clinically Classified Oral Lichen Planus in Optical Coherence Tomography: A Descriptive Case-Series Study. Diagnostics. 2023; 13(16):2642. https://doi.org/10.3390/diagnostics13162642
Chicago/Turabian StyleGruda, Yuliia, Marius Albrecht, Michaela Buckova, Dominik Haim, Guenter Lauer, Edmund Koch, Korinna Joehrens, Christian Schnabel, Jonas Golde, Jiawen Li, and et al. 2023. "Characteristics of Clinically Classified Oral Lichen Planus in Optical Coherence Tomography: A Descriptive Case-Series Study" Diagnostics 13, no. 16: 2642. https://doi.org/10.3390/diagnostics13162642
APA StyleGruda, Y., Albrecht, M., Buckova, M., Haim, D., Lauer, G., Koch, E., Joehrens, K., Schnabel, C., Golde, J., Li, J., McLaughlin, R. A., & Walther, J. (2023). Characteristics of Clinically Classified Oral Lichen Planus in Optical Coherence Tomography: A Descriptive Case-Series Study. Diagnostics, 13(16), 2642. https://doi.org/10.3390/diagnostics13162642





