Evaluating the Necessity of Adaptive RT and the Role of Deformable Image Registration in Lung Cancer with Different Pathologic Classifications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Grouping
2.2. Patient Simulation and Treatment Planning Process
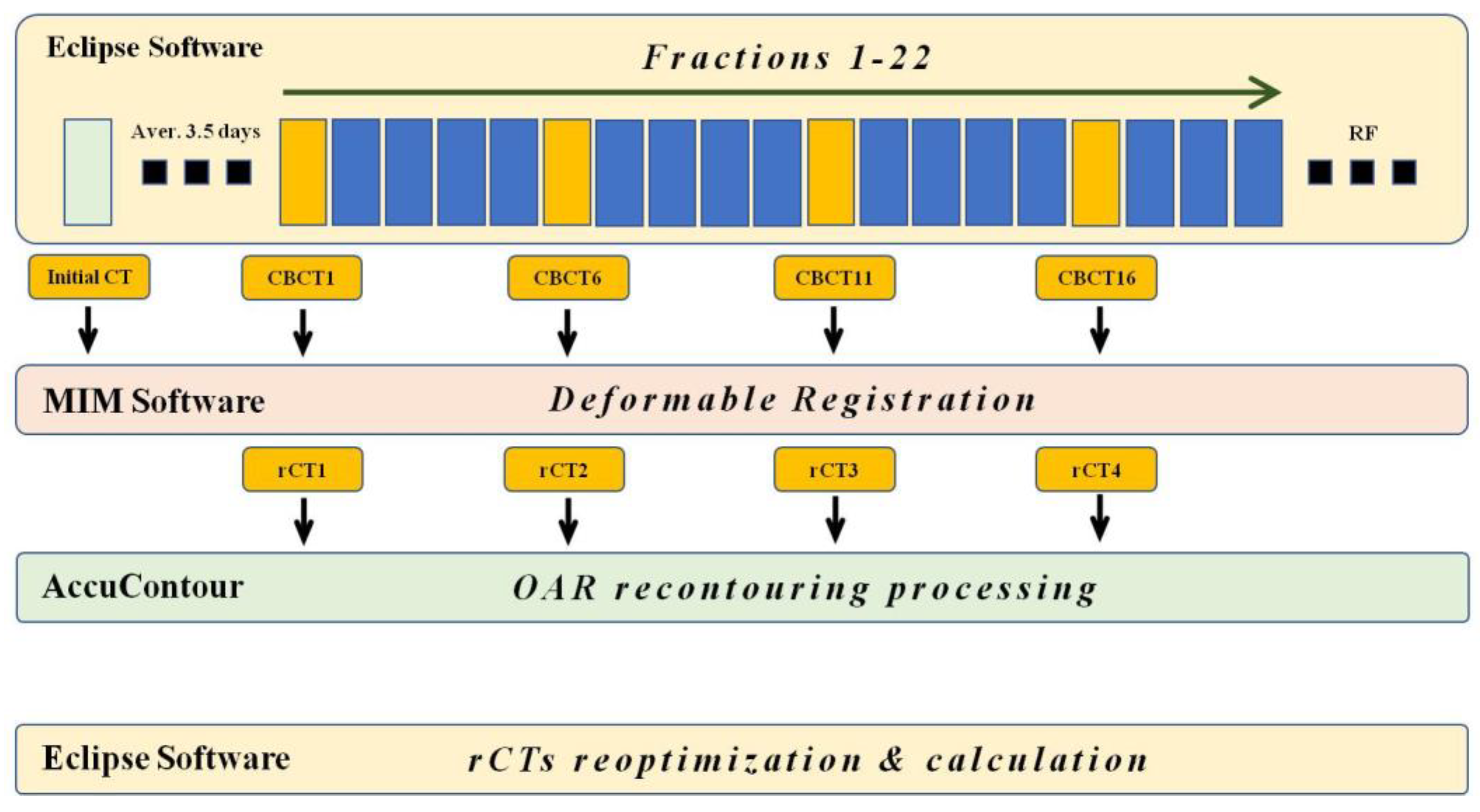
2.3. Imaging Acquisition and Registration Process
2.4. Treatment Plan Application and Recalculation
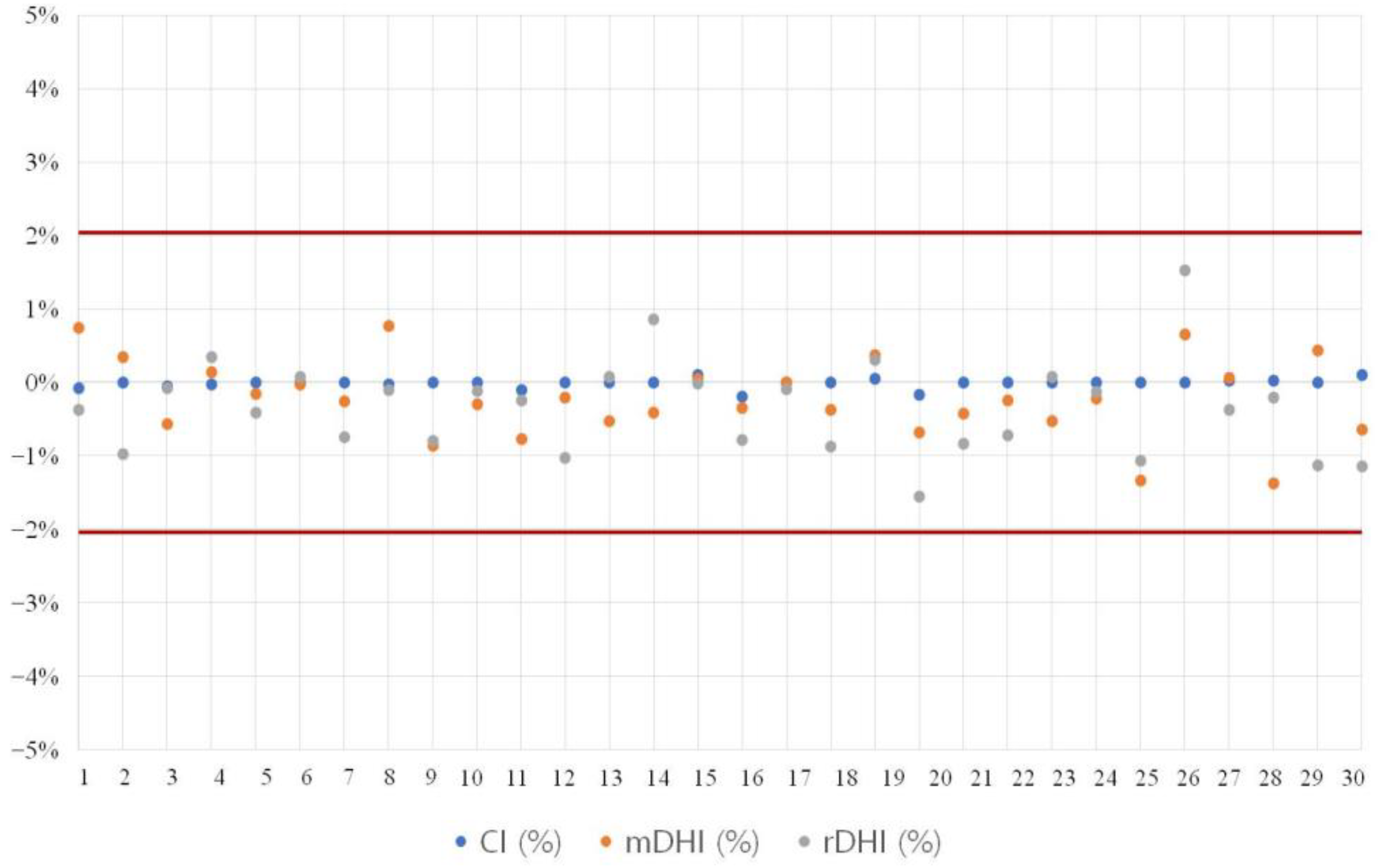
2.5. Evaluation of Treatment Plan Consistency
2.6. Data Collection and Parameter Setting
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Evaluation of Treatment Plan Consistency
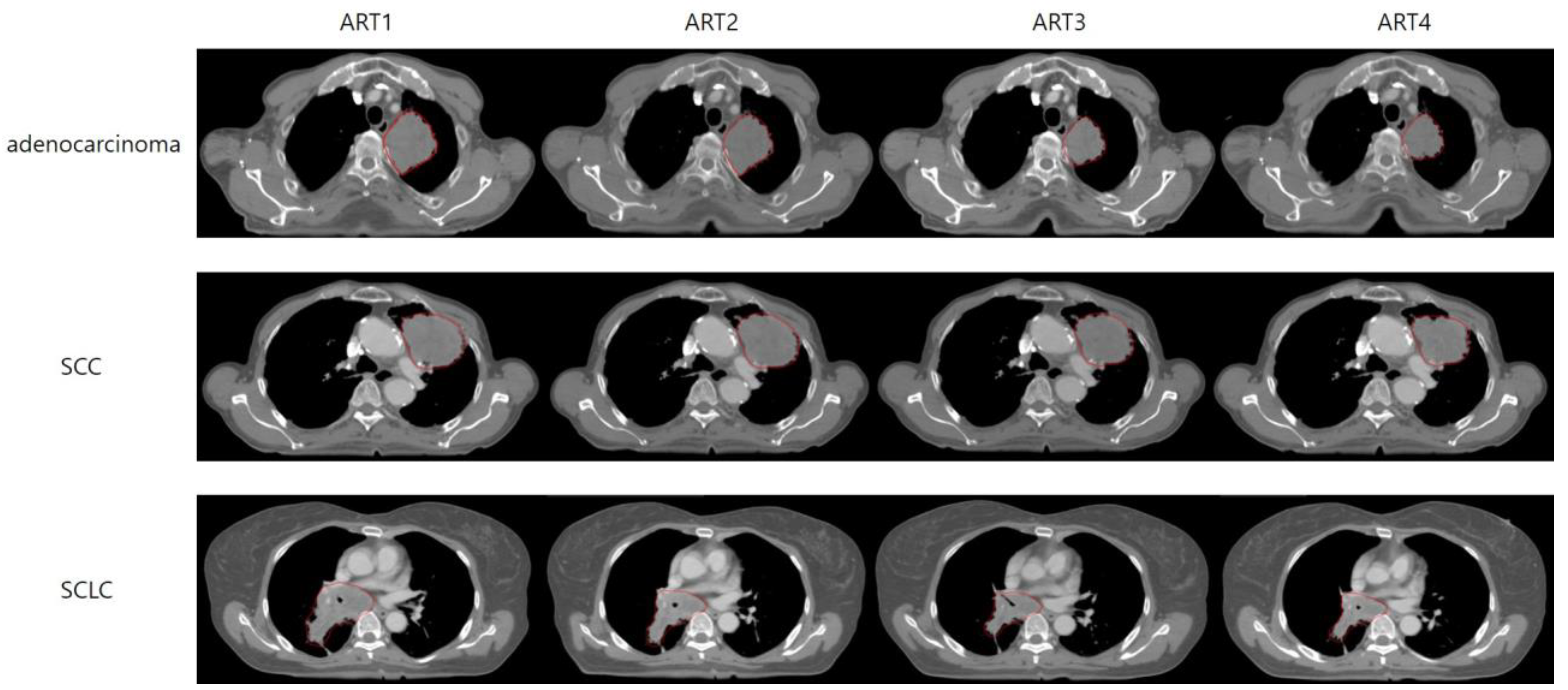
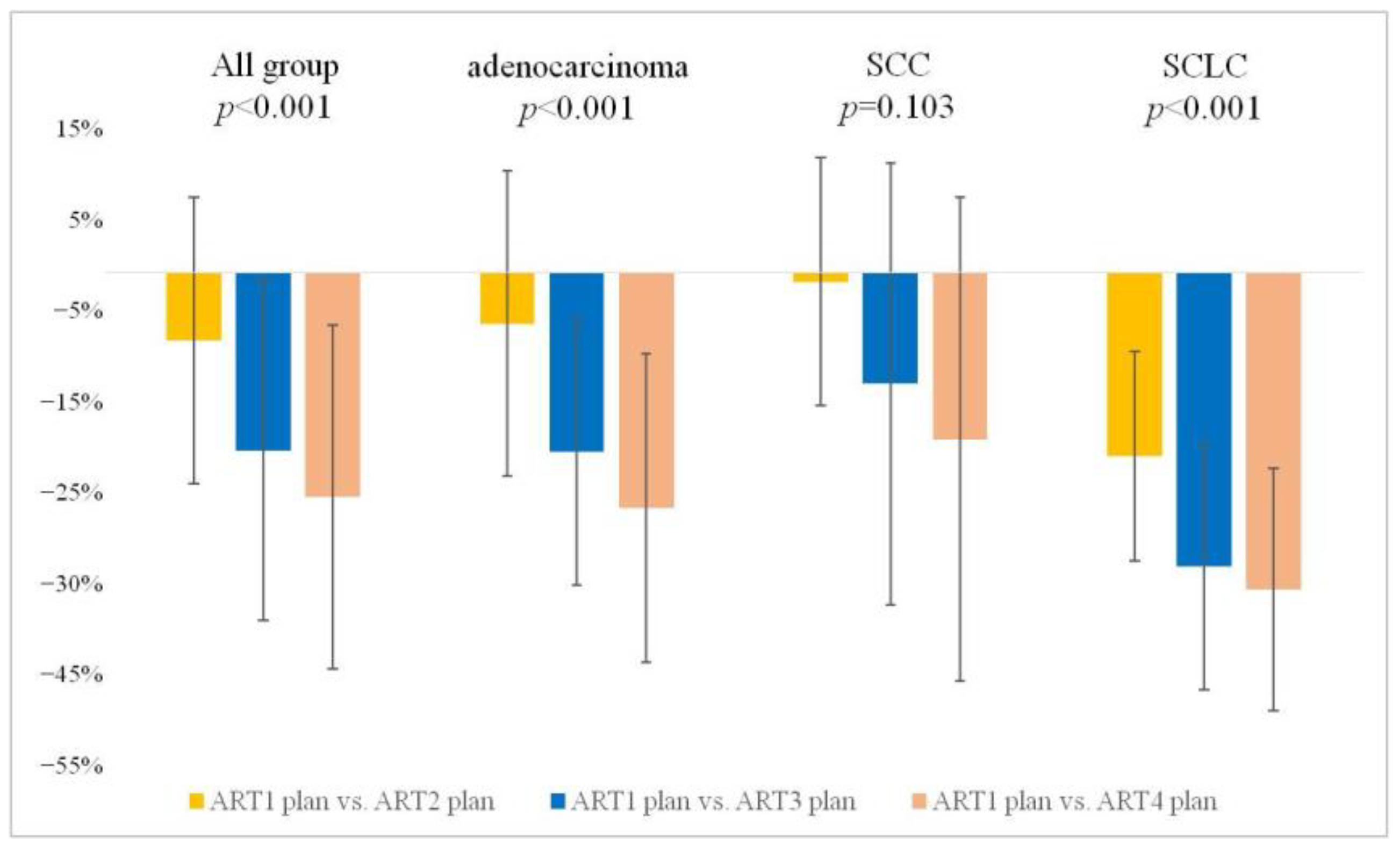
3.3. GTV Changes
3.3.1. Weekly Stepwise Tracking of GTV Changes: A Cumulative Comparison from the Start of Treatment
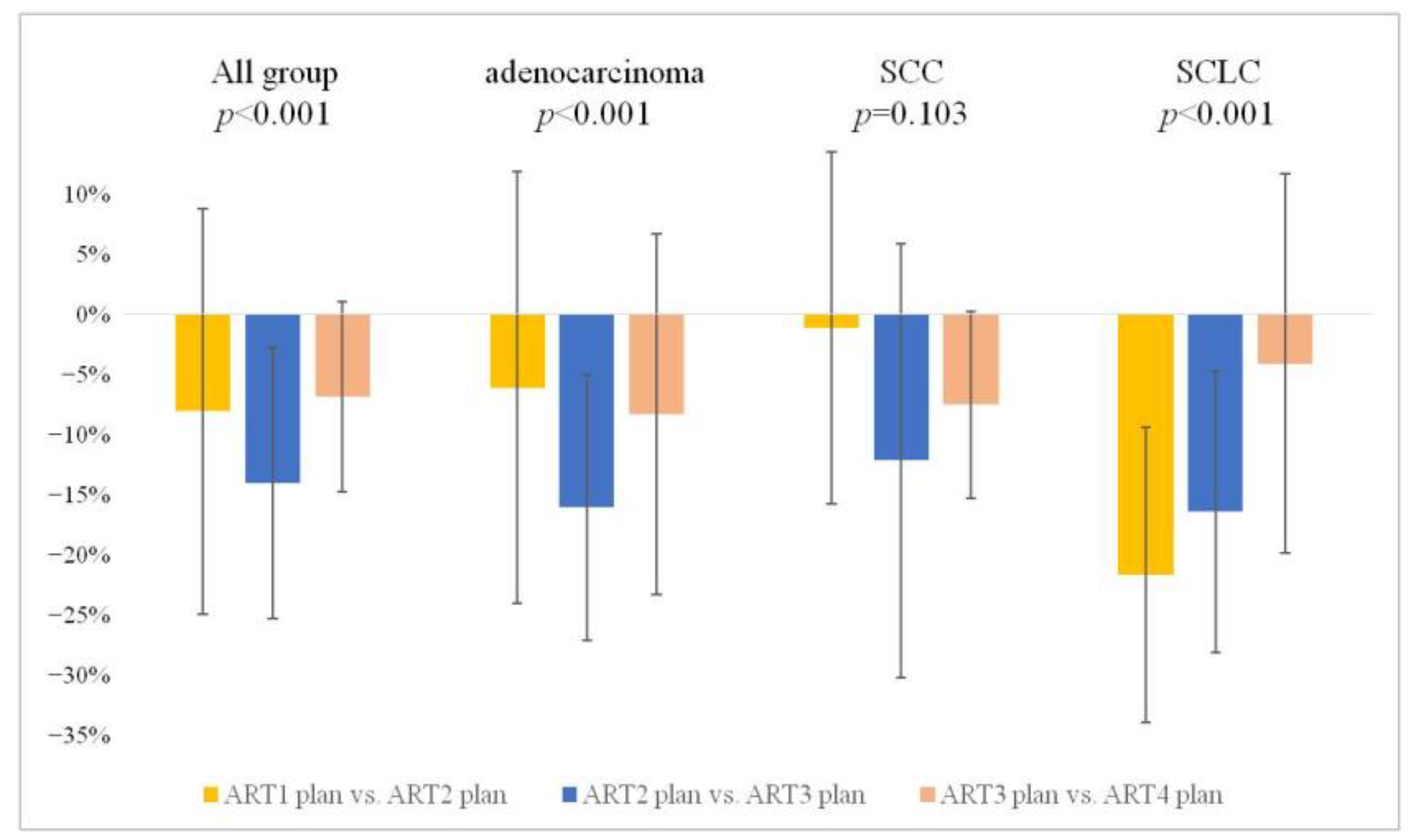
3.3.2. Weekly Interval Comparison of GTV Alterations
3.4. OAR
3.4.1. Whole Lung
3.4.2. Esophagus
3.4.3. Heart
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barta, J.A.; Powell, C.A.; Wisnivesky, J.P. Global Epidemiology of Lung Cancer. Ann. Glob. Health 2019, 85, 8. [Google Scholar] [CrossRef] [PubMed]
- Thai, A.A.; Solomon, B.J.; Sequist, L.V.; Gainor, J.F.; Heist, R.S. Lung cancer. Lancet 2021, 398, 535–554. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Canales, J.; Parra-Cuentas, E.; Wistuba, I.I. Diagnosis and Molecular Classification of Lung Cancer. Cancer Treat. Res. 2016, 170, 25–46. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, V.M.L.; Carvalho, L. Heterogeneity in Lung Cancer. Pathobiology 2018, 85, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Chan, B.A.; Hughes, B.G. Targeted therapy for non-small cell lung cancer: Current standards and the promise of the future. Transl. Lung Cancer Res. 2015, 4, 36–54. [Google Scholar] [CrossRef]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef] [PubMed]
- Davidson, M.R.; Gazdar, A.F.; Clarke, B.E. The pivotal role of pathology in the management of lung cancer. J. Thorac. Dis. 2013, 5 (Suppl. S5), S463–S478. [Google Scholar] [CrossRef]
- Giaccone, G.; He, Y. Current knowledge of small cell lung cancer transformation from non-small cell lung cancer. In Seminars in Cancer Biology; Academic Press: Cambridge, MA, USA, 2023; Volume 94, pp. 1–10. [Google Scholar] [CrossRef]
- DeSelm, C.; Palomba, M.L.; Yahalom, J.; Hamieh, M.; Eyquem, J.; Rajasekhar, V.K.; Sadelain, M. Low-Dose Radiation Conditioning Enables CAR T Cells to Mitigate Antigen Escape. Mol. Ther. 2018, 26, 2542–2552. [Google Scholar] [CrossRef]
- Carmichael, J.; Degraff, W.G.; Gamson, J.; Russo, D.; Gazdar, A.F.; Levitt, M.L.; Minna, J.D.; Mitchell, J.B. Radiation sensitivity of human lung cancer cell lines. Eur. J. Cancer Clin. Oncol. 1989, 25, 527–534. [Google Scholar] [CrossRef]
- Luo, J.; Song, J.; Xiao, L.; Zhang, J.; Cao, Y.; Wang, J.; Wang, P.; Zhao, L.; Liu, N. Simultaneous integrated dose reduction intensity-modulated radiotherapy effectively reduces cardiac toxicity in limited-stage small cell lung cancer. Cancer Biol. Med. 2023, 20, 452–464. [Google Scholar] [CrossRef]
- Koga, K.; Kusuhara, T.; Nishikawa, K.; Asada, K.; Watanabe, K. Correlation between dose and tumor response in the radiotherapy of lung cancer of various histological types. Jpn. J. Clin. Oncol. 1984, 14, 301–306. [Google Scholar]
- Piperdi, H.; Portal, D.; Neibart, S.S.; Yue, N.J.; Jabbour, S.K.; Reyhan, M. Adaptive Radiation Therapy in the Treatment of Lung Cancer: An Overview of the Current State of the Field. Front. Oncol. 2021, 11, 770382. [Google Scholar] [CrossRef]
- Amugongo, L.M.; Green, A.; Cobben, D.; van Herk, M.; McWilliam, A.; Osorio, E.V. Identification of modes of tumor regression in non-small cell lung cancer patients during radiotherapy. Med. Phys. 2022, 49, 370–381. [Google Scholar] [CrossRef]
- Piper, J.; Nelson, A.; Harper, J. Deformable Image Registration in MIM Maestro Evaluation and Description; MiM Software Inc.: Cleveland, OH, USA, 2013. [Google Scholar]
- Feuvret, L.; Noël, G.; Mazeron, J.J.; Bey, P. Conformity index: A review. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 333–342. [Google Scholar] [CrossRef]
- Li, J.; Xu, J.; Yang, M.; Zhou, Q. Therapeutic revolution for inoperable stage III non-small cell lung cancer in the immune era. Cancer Biol. Med. 2022, 19, 569–572. [Google Scholar] [CrossRef]
- Barros, J.M.; Rizzo, M.M.; Chiozza, J.O.; Couñago, F. Is there a place for optimizing thoracic radiotherapy in limited-stage small cell lung cancer after twenty years? World J. Clin. Oncol. 2021, 12, 1–5. [Google Scholar] [CrossRef]
- Bogart, J.A.; Waqar, S.N.; Mix, M.D. Radiation and Systemic Therapy for Limited-Stage Small-Cell Lung Cancer. J. Clin. Oncol. 2022, 40, 661–670. [Google Scholar] [CrossRef]
- Faivre-Finn, C.; Snee, M.; Ashcroft, L.; Appel, W.; Barlesi, F.; Bhatnagar, A.; Bezjak, A.; Cardenal, F.; Fournel, P.; Harden, S.; et al. Concurrent once-daily versus twice-daily chemoradiotherapy in patients with limited-stage small-cell lung cancer (CONVERT): An open-label, phase 3, randomised, superiority trial. Lancet Oncol. 2017, 18, 1116–1125. [Google Scholar] [CrossRef]
- Turrisi, A.T.; Kim, K.; Blum, R.; Sause, W.T.; Livingston, R.B.; Komaki, R.; Wagner, H.; Aisner, S.; Johnson, D.H. Twice-Daily Compared with Once-Daily Thoracic Radiotherapy in Limited Small-Cell Lung Cancer Treated Concurrently with Cisplatin and Etoposide. New Engl. J. Med. 1999, 340, 265–271. [Google Scholar] [CrossRef]
- Wurstbauer, K.; Kazil, M.; Meinschad, M.; Pinter, R.; De Vries, C.; Clemens, P.; Kreuter, C.; Hernler, T.; Hitzl, W.; Cerkl, P.; et al. Locally advanced NSCLC: A plea for sparing the ipsilateral normal lung-prospective, clinical trial with DART-bid (dose-differentiated accelerated radiation therapy, 1.8 Gy twice daily) by VMAT. Radiat. Oncol. 2022, 17, 120. [Google Scholar] [CrossRef]
- Farrell, M.J.; Yahya, J.B.; Degnin, C.; Chen, Y.; Holland, J.M.; Henderson, M.A.; Jaboin, J.J.; Harkenrider, M.M.; Thomas, C.R.; Mitin, T. Radiation Dose and Fractionation for Limited-stage Small-cell Lung Cancer: Survey of US Radiation Oncologists on Practice Patterns. Clinical Lung Cancer 2019, 20, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Brada, M.; Forbes, H.; Ashley, S.; Fenwick, J. Improving Outcomes in NSCLC: Optimum Dose Fractionation in Radical Radiotherapy Matters. J. Thorac. Oncol. 2022, 17, 532–543. [Google Scholar] [CrossRef] [PubMed]
- Tariq, S.; Kim, S.Y.; Monteiro de Oliveira Novaes, J.; Cheng, H. Update 2021: Management of Small Cell Lung Cancer. Lung 2021, 199, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Shue, Y.T.; Lim, J.S.; Sage, J. Tumor heterogeneity in small cell lung cancer defined and investigated in pre-clinical mouse models. Transl. Lung Cancer Res. 2018, 7, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.L.; Su, Y.G.; Yu, L.; Bai, Z.L.; Bai, X.H.; Chen, X.Z.; Yang, X.; Zhao, R.; He, J.X.; Wang, Y.Y. Clinical characteristics and patient outcomes of molecular subtypes of small cell lung cancer (SCLC). World J. Surg. Oncol. 2022, 20, 54. [Google Scholar] [CrossRef]
- Shaw, E.; Kline, R.; Gillin, M.; Souhami, L.; Hirschfeld, A.; Dinapoli, R.; Martin, L. Radiation Therapy Oncology Group: Radiosurgery quality assurance guidelines. Int. J. Radiat. Oncol. Biol. Phys. 1993, 27, 1231–1239. [Google Scholar] [CrossRef]
- Li, Z. Prescribing, Recording, and Reporting Proton-Beam Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1602. [Google Scholar] [CrossRef]
- Patel, G.; Mandal, A.; Choudhary, S.; Mishra, R.; Shende, R. Plan evaluation indices: A journey of evolution. Rep. Pract. Oncol. Radiother. 2020, 25, 336–344. [Google Scholar] [CrossRef]
- Martel, M.K.; Ten Haken, R.K.; Hazuka, M.B.; Turrisi, A.T.; Fraass, B.A.; Lichter, A.S. Dose-volume histogram and 3-D treatment planning evaluation of patients with pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 1994, 28, 575–581. [Google Scholar] [CrossRef]
- Palma, D.A.; Senan, S.; Tsujino, K.; Barriger, R.B.; Rengan, R.; Moreno, M.; Bradley, J.D.; Kim, T.H.; Ramella, S.; Marks, L.B.; et al. Predicting radiation pneumonitis after chemoradiation therapy for lung cancer: An international individual patient data meta-analysis. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 444–450. [Google Scholar] [CrossRef]
- Claude, L.; Pérol, D.; Ginestet, C.; Falchero, L.; Arpin, D.; Vincent, M.; Martel, I.; Hominal, S.; Cordier, J.F.; Carrie, C. A prospective study on radiation pneumonitis following conformal radiation therapy in non-small-cell lung cancer: Clinical and dosimetric factors analysis. Radiother. Oncol. 2004, 71, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, Y.; Kadoya, N.; Kanai, T.; Saito, M.; Kito, S.; Hashimoto, S.; Karasawa, K.; Jingu, K. Evaluation of the effect of user-guided deformable image registration of thoracic images on registration accuracy among users. Med. Dosim. 2020, 45, 206–212. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Cazoulat, G.; Wu, C.; Peterson, C.; McCulloch, M.; Anderson, B.; Pollard-Larkin, J.; Balter, P.; Liao, Z.; Mohan, R.; et al. Geometric and dosimetric accuracy of deformable image registration between average-intensity images for 4DCT-based adaptive radiotherapy for non-small cell lung cancer. J. Appl. Clin. Med. Phys. 2021, 22, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Vickress, J.R.; Battista, J.; Barnett, R.; Yartsev, S. Online daily assessment of dose change in head and neck radiotherapy without dose-recalculation. J. Appl. Clin. Med. Phys. 2018, 19, 659–665. [Google Scholar] [CrossRef] [PubMed]
| Total n = 30 | NSCLC n = 20 | SCLC n = 10 | p-Value | Analysis Method | |
|---|---|---|---|---|---|
| Age | 75 (54–89) | 71 (54–89) | 75 (56–87) | 0.227 | Student t-test |
| Sex | >0.999 | Fisher’s exact test | |||
| Male | 25 (83.33%) | 17 (85.00%) | 8 (80.00%) | ||
| Female | 5 (16.6%) | 3 (15.00%) | 2 (20.00%) | ||
| Smoking | 0.682 | Fisher’s exact test | |||
| Yes | 22 (73.3%) | 14 (70.0%) | 8 (80.0%) | ||
| No | 8 (26.7%) | 6 (30.0%) | 2 (20.0%) | ||
| T stage | 0.052 | Fisher’s exact test | |||
| 1 | 9 (30.00%) | 4 (20.00%) | 5 (50.00%) | ||
| 2 | 8 (26.67%) | 5 (25.00%) | 3 (30.00%) | ||
| 3 | 9 (30.00%) | 9 (45.00%) | 0 (0.00%) | ||
| 4 | 4 (13.3%) | 2 (10.00%) | 2 (20.00%) | ||
| N stage | 0.663 | Fisher’s exact test | |||
| 0 | 14 (46.67%) | 9 (45.00%) | 5 (50.00%) | ||
| 1 | 4 (13.33%) | 2 (10.00%) | 2 (20.00%) | ||
| 2 | 10 (33.33%) | 8 (40.00%) | 2 (20.00%) | ||
| 3 | 2 (6.67%) | 1 (5.00%) | 1 (5.00%) | ||
| Chemo | 0.101 | Fisher’s exact test | |||
| Yes | 20 (66.67%) | 11 (55.00%) | 9 (90.00%) | ||
| No | 10 (33.33%) | 9 (45.00%) | 1 (10.00%) | ||
| GTV location | 0.588 | Fisher’s exact test | |||
| LUL | 8 (26.7%) | 7 (35%) | 1 (10%) | ||
| LLL | 4 (13.3%) | 2 (10%) | 2 (20%) | ||
| RUL | 9 (30%) | 6 (30%) | 3 (30%) | ||
| RML | 2 (6.7%) | 1 (5%) | 1 (10%) | ||
| RLL | 7 (23.3%) | 4 (20%) | 3 (30%) | ||
| PlanCT to RT interval (days) | 3.5 (2–6) | 3 (2–6) | 4.5 (3–6) | 0.177 | Student t-test |
| p-Value (All) * | Initial Plan vs. ART1 Plan p-Value | Initial Plan vs. ART2 Plan p-Value | Initial Plan vs. ART3 Plan p-Value | Initial Plan vs. ART4 Plan p-Value | |
|---|---|---|---|---|---|
| CI | 0.437 | >0.999 | >0.999 | >0.999 | >0.999 |
| mDHI | 0.191 | 0.655 | 0.123 | >0.999 | 0.554 |
| rDHI | 0.211 | >0.999 | >0.999 | 0.320 | 0.686 |
| All Group | Adenocarcinoma Group | SCC Group | SCLC Group | |
|---|---|---|---|---|
| rCT1 GTV abs. (cm3) | 56.68 ± 66.65 | 34.21 ± 32.46 | 86.80 ± 96.91 | 49.03 ± 47.29 |
| rCT2 GTV rel. (%) | −7.77 ± 16.31 | −5.86 ± 17.39 | −1.07 ± 14.14 | −20.95 ± 11.88 |
| rCT3 GTV rel. (%) | −20.26 ± 19.34 | −20.47 ± 15.11 | −12.68 ± 25.15 | −33.51 ± 14.05 |
| rCT4 GTV rel. (%) | −25.54 ± 19.56 | −26.86 ± 17.53 | −19.03 ± 27.56 | −36.14 ± 13.77 |
| p-value All (abs.) | <0.001 | 0.034 | 0.023 | 0.034 |
| p-value All (rel.) | <0.001 | <0.001 | 0.103 | <0.001 |
| p-value rCT1 vs. rCT2 (rel.) | 0.010 | >0.999 | >0.999 | 0.001 |
| p-value rCT1 vs. rCT3 (rel.) | <0.001 | 0.015 | >0.999 | <0.001 |
| p-value rCT1 vs. rCT4 (rel.) | <0.001 | 0.009 | 0.758 | <0.001 |
| p-value rCT2 vs. rCT3 (rel.) | <0.001 | 0.031 | 0.250 | 0.076 |
| p-value rCT3 vs. rCT4 (rel.) | 0.134 | >0.999 | >0.999 | >0.999 |
| ART1 Plan | ART2 Plan | ART3 Plan | ART4 Plan | p-Value (All) | |
|---|---|---|---|---|---|
| ALL Group | |||||
| V20Gy (cm3) | 340.85 ± 158.75 | 326.22 ± 145.19 | 309.14 ± 150.94 | 301.96± 135.19 | 0.002 |
| V30Gy (cm3) | 180.20 ± 87.77 | 169.20 ± 78.05 | 161.17 ± 75.50 | 155.45 ± 72.34 | <0.001 |
| Dmean (Gy) | 8.93 ± 3.84 | 8.41 ± 3.23 | 8.05 ± 3.26 | 8.00 ± 3.19 | 0.004 |
| Adenocarcinoma | |||||
| V20Gy (cm3) | 301.05 ± 156.68 | 292.07 ± 164.91 | 273.77 ± 183.51 | 272.25 ± 149.34 | 0.188 |
| V30Gy (cm3) | 162.11 ± 67.00 | 159.14 ± 71.77 | 153.95 ± 70.48 | 145.47 ± 65.90 | <0.001 |
| Dmean (Gy) | 7.97 ± 3.41 | 7.88 ± 3.12 | 7.43 ± 3.34 | 7.43 ± 3.57 | 0.125 |
| SCC | |||||
| V20Gy (cm3) | 357.44 ± 135.99 | 345.66 ± 108.04 | 332.24 ± 119.01 | 312.24 ± 107.71 | 0.051 |
| V30Gy (cm3) | 191.19 ± 85.05 | 182.67 ± 72.26 | 171.76 ± 74.17 | 164.53 ± 70.63 | 0.071 |
| Dmean (Gy) | 9.89 ± 3.50 | 9.28 ± 2.95 | 8.59 ± 2.61 | 8.50 ± 2.44 | 0.202 |
| SCLC | |||||
| V20Gy (cm3) | 364.07 ± 188.39 | 340.94 ± 164.64 | 321.42 ± 153.04 | 321.38 ± 153.20 | 0.007 |
| V30Gy (cm3) | 187.31 ± 112.01 | 165.80 ± 94.49 | 157.81 ± 87.77 | 156.34 ± 85.61 | 0.002 |
| Dmean (Gy) | 8.95 ± 4.64 | 8.07 ± 3.71 | 8.13 ± 3.95 | 8.08 ± 3.65 | 0.052 |
| ART1 Plan | ART2 Plan | ART3 Plan | ART4 Plan | p-Value (All) | |
|---|---|---|---|---|---|
| ALL Group | |||||
| Dmax (Gy) | 29.16 ± 15.51 | 29.43 ± 15.57 | 28.71 ± 15.25 | 28.59 ± 15.18 | 0.933 |
| Dmean (Gy) | 12.57 ± 11.63 | 13.05 ± 11.35 | 10.59 ± 9.16 | 10.78 ± 9.50 | 0.731 |
| Adenocarcinoma | |||||
| Dmax (Gy) | 22.46 ± 13.87 | 23.28 ± 14.03 | 23.31 ± 14.67 | 22.49 ± 14.40 | 0.391 |
| Dmean (Gy) | 8.34 ± 8.60 | 10.71 ± 10.65 | 8.05 ± 8.86 | 8.06 ± 8.96 | 0.197 |
| SCC | |||||
| Dmax (Gy) | 29.00 ± 13.50 | 27.91 ± 13.78 | 28.02 ± 13.15 | 28.62 ± 12.71 | 0.451 |
| Dmean (Gy) | 12.83 ± 11.20 | 12.48 ± 9.63 | 11.96 ± 9.62 | 12.39 ± 9.81 | 0.738 |
| SCLC | |||||
| Dmax (Gy) | 36.01 ± 17.27 | 37.11 ± 16.85 | 34.81 ± 16.93 | 34.65 ± 17.05 | 0.687 |
| Dmean (Gy) | 16.53 ± 14.11 | 15.97 ± 13.89 | 11.77 ± 9.42 | 11.88 ± 10.08 | 0.828 |
| ART1 Plan | ART2 Plan | ART3 Plan | ART4 Plan | p-Value (All) | |
|---|---|---|---|---|---|
| ALL Group | |||||
| V20Gy (cm3) | 40.23 ± 57.88 | 39.21 ± 55.63 | 35.91 ± 55.33 | 37.60 ± 56.79 | 0.025 |
| V30Gy (cm3) | 14.84 ± 23.37 | 14.41 ± 23.62 | 13.47 ± 22.84 | 14.08 ± 24.87 | 0.182 |
| Dmean (Gy) | 6.31 ± 5.85 | 5.78 ± 5.35 | 5.65 ± 5.33 | 5.56 ± 5.38 | 0.646 |
| Adenocarcinoma | |||||
| V20Gy (cm3) | 17.58 ± 34.08 | 20.59 ± 42.71 | 21.20 ± 43.89 | 20.13 ± 41.07 | 0.865 |
| V30Gy (cm3) | 7.36 ± 16.83 | 8.80 ± 20.29 | 9.38 ± 22.14 | 8.60 ± 19.60 | 0.171 |
| Dmean (Gy) | 3.72 ± 4.80 | 3.27 ± 3.54 | 3.17 ± 3.73 | 3.04 ± 4.29 | 0.166 |
| SCC | |||||
| V20Gy (cm3) | 49.70 ± 67.66 | 48.49 ± 60.78 | 44.80 ± 62.21 | 51.75 ± 72.88 | 0.457 |
| V30Gy (cm3) | 16.00 ± 25.42 | 15.64 ± 26.49 | 15.29 ± 24.38 | 18.44 ± 33.36 | 0.731 |
| Dmean (Gy) | 7.47 ± 6.02 | 7.20 ± 6.02 | 6.69 ± 5.78 | 6.72 ± 6.02 | 0.868 |
| SCLC | |||||
| V20Gy (cm3) | 53.43 ± 64.75 | 48.54 ± 62.26 | 41.73 ± 60.86 | 40.92 ± 53.11 | 0.009 |
| V30Gy (cm3) | 21.14 ± 26.89 | 18.80 ± 25.01 | 15.75 ± 23.84 | 15.20 ± 20.99 | 0.003 |
| Dmean (Gy) | 7.73 ± 6.29 | 6.88 ± 5.75 | 7.08 ± 5.82 | 6.93 ± 5.28 | 0.644 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.C.; Won, Y.K.; Lee, S.M.; Heo, N.H.; Yeo, S.-G.; Chang, A.R.; Bae, S.H.; Kim, J.S.; Yoo, I.D.; Hong, S.-p.; et al. Evaluating the Necessity of Adaptive RT and the Role of Deformable Image Registration in Lung Cancer with Different Pathologic Classifications. Diagnostics 2023, 13, 2956. https://doi.org/10.3390/diagnostics13182956
Kim WC, Won YK, Lee SM, Heo NH, Yeo S-G, Chang AR, Bae SH, Kim JS, Yoo ID, Hong S-p, et al. Evaluating the Necessity of Adaptive RT and the Role of Deformable Image Registration in Lung Cancer with Different Pathologic Classifications. Diagnostics. 2023; 13(18):2956. https://doi.org/10.3390/diagnostics13182956
Chicago/Turabian StyleKim, Woo Chul, Yong Kyun Won, Sang Mi Lee, Nam Hun Heo, Seung-Gu Yeo, Ah Ram Chang, Sun Hyun Bae, Jae Sik Kim, Ik Dong Yoo, Sun-pyo Hong, and et al. 2023. "Evaluating the Necessity of Adaptive RT and the Role of Deformable Image Registration in Lung Cancer with Different Pathologic Classifications" Diagnostics 13, no. 18: 2956. https://doi.org/10.3390/diagnostics13182956






