Data Analysis and Systematic Scoping Review on the Pathogenesis and Modalities of Treatment of Thyroid Storm Complicated with Myocardial Involvement and Shock
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
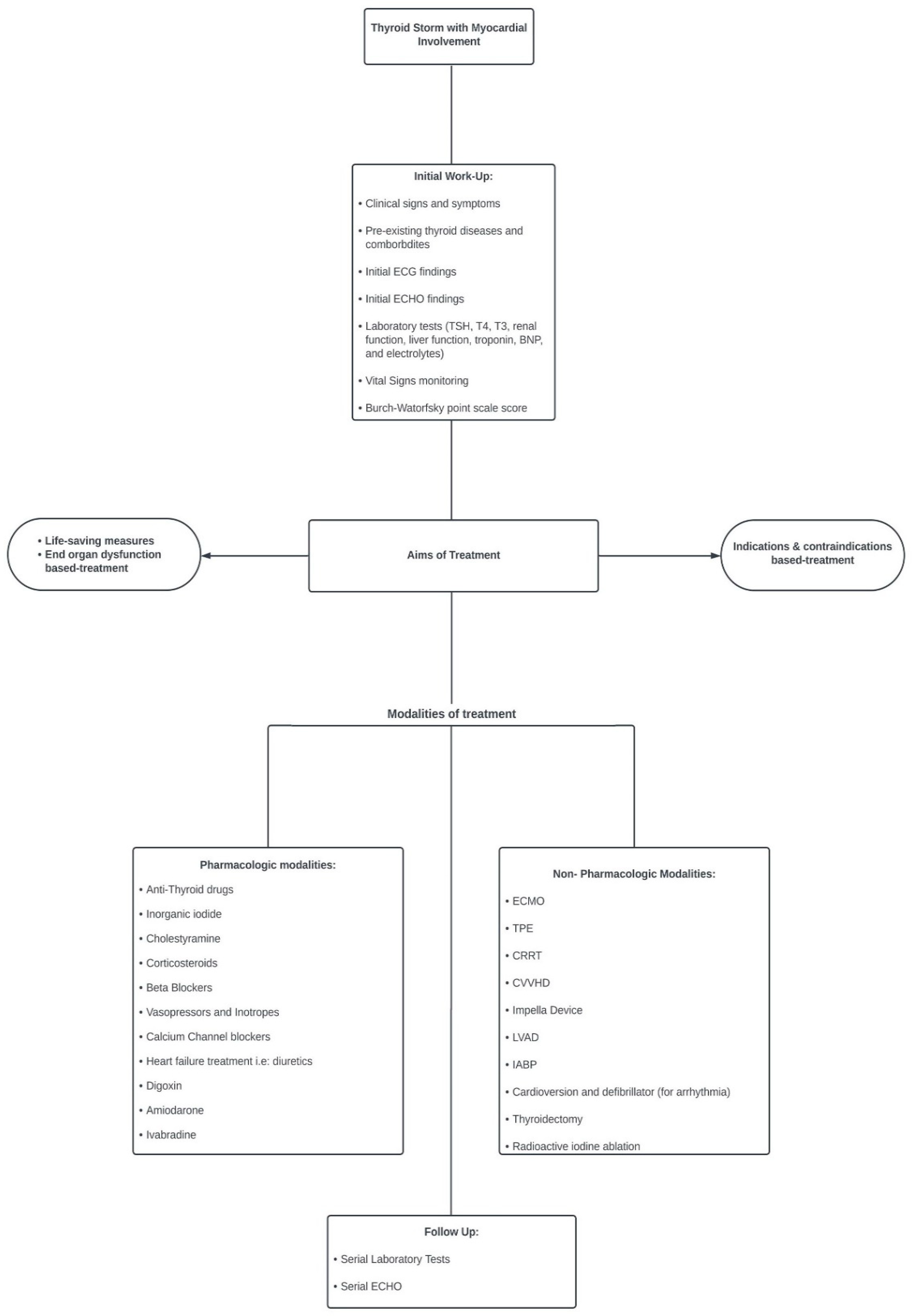
- Modalities of treatment of TS with myocardial involvement
- (A)
- Pharmacological treatment modalities
- (B)
- Non-pharmacological therapy
- (a)
- Extracorporeal Membrane Oxygenation (VA-ECMO): In 2021, Lim et al. [161] reported that there were 27 cases in the literature at the time of thyrotoxic crisis requiring ECMO, and 85% of these patients survived. In severe cases, first-line pharmacotherapy may not be sufficient to restore cardiovascular function to normal levels after TS development. When faced with this, extracorporeal modalities are implemented. Among the 256 cases, the use of ECMO was reported in 16.3% of cases; hence, it was the most used mechanical support. ECMO bypasses the heart and lungs and provides gas exchange through the external membrane [161]. This process supports the heart by temporarily relieving the heart of its functions to allow it to heal, while thyroid hormones normalize, and the euthyroid state is restored [263].
- ECMO is mainly indicated in cases of acute severe cardiac or pulmonary failure unresponsive to conventional therapy (ELSO guidelines) [264]. In addition, it has been reported in multiple cases that the use of ECMO contributes to more successful outcomes until thyroidectomy is performed because of the stabilization of myocardial function [161]. Furthermore, when used in concordance with other extracorporeal modalities, the results may be enhanced, and treatment becomes more effective [161,263].
- Despite the recent incorporation of ECMO in the management of endocrine emergencies, the overall survival rate could be unreliable because of possible publication bias, patient selection bias, and small sample size [161]. The cause of death might not directly correlate with the use of ECMO but rather with the severity of cardiomyopathy, shock, and other complications [42,161]. Common complications of ECMO include bleeding, thrombosis, limb ischemia, and stroke [77,161].
- (b)
- Therapeutic plasma exchange (TPE): it is a class II indication of TS. TPE is one of the most effective methods for eliminating excess thyroid hormones circulating in patients with TS [9]. It uses a purification technique that rapidly filters out large molecular substances from the plasma, reducing protein-bound and free T4 and T3 [161]. According to the American Society for Apheresis, TPE is a category III indication for TS and its use is based on individual cases [161]. It is important to note that during this process, clotting factors and immunoglobulins may also be filtered out; therefore, the patient should be infused with replacement colloid and blood products to avoid the risk of bleeding and infection [163]. TPE should be implemented early in the treatment course of TS to ensure the best results [163]; however, in some cases, it may be delayed owing to more pressing complications, which can cause technical difficulties, such as the need for CVVHD implementation for acute kidney injury and metabolic acidosis [48]. TPE may also be incorporated into multimodal therapeutic course [161]. TPE can be used in combination with ECMO, Impella, or CRRT [38,161]. TPE is also used as a bridging treatment until the patient becomes sufficiently stable to undergo thyroidectomy [163]. TPE can reduce all free and total thyroid hormones by 10 to 80%, reduce autoantibodies and cytokines, and remove 5-monodeiodinase to inhibit the conversion of T4 to T3 [161]. Multiple cycles of TPE are required in some cases, as thyroxine distribution is mainly in the extrahepatic tissue (34%), intravascular (26%), extracellular fluid (26%), and liver (14%) [161,265].
- (c)
- Continuous Renal Replacement therapy (CRRT) and continuous venovenous hemofiltration (CVVH): CRRT includes the use of large volumes of room-temperature fluids (dialysate and replacement fluids), which can cause hypothermia. In addition, intravenous infusion of albumin and plasma in CRRT increases the ability of proteins to bind free thyroid hormones [38]. CRRT is a treatment method that utilizes intermittent hemodialysis and peritoneal dialysis [266]. It has been used in patients with acute kidney injury (AKI) who are hemodynamically unstable secondary to TS.
- (d)
- CVVH is one of the modes of CRRT, which was described in six of this review cases. Our data showed that CRRT was significantly associated with a high mortality rate, particularly in patients with acute renal failure. CVVH uses convective clearance to remove toxins and solutes from the patient’s circulation, whereas CVVHD relies on diffusive clearance to remove the same toxins and solutes [266]. CVVH helps prevent sequelae resulting from metabolic and hemodynamic instability.
- (e)
- Intra-aortic balloon pump (IABP): This device is used in cases of acute heart failure with shock after ineffective inotropic or vasopressor administration. The IABP works by inflating the balloon during diastole and aortic valve closure and rapidly deflating before systole [267]. This results in a reduced afterload, which consequently improves cardiac output by increasing stroke volume and ejection fraction. Around nine percent of the cases used IABP, and a few patients died immediately thereafter. IABP was used alongside ECMO (nine cases used ECMO + IABP) as a means of circulatory support, whereas the underlying cause of heart failure was treated (TS). Some authors prefer ECMO for IABP [162].
- (f)
- Impella: The Impella device pumps blood from the left ventricle into the ascending aorta and helps maintain systemic circulation at an upper rate between 2.5 and 5.0 L/min. The use of the Impella over ECMO is based on the concept of ventricular unloading to allow ventricular time to recover. It is a very small catheter-based device used as ventricular support in patients with CHF and CS [268]. Impella (Bi-pella) was used in three of our cases. In one case, the patient was initiated on esmolol drip, but deteriorated immediately after signs of biventricular failure. He was placed on the CP Impella (LV), but inadequate improvement called for the use of RP Impella (RV) [168]. The use of biventricular Impella allowed the treatment of underlying heart failure and yielded significantly better outcomes.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yamamoto, H.; Monno, S.; Ohta-Ogo, K.; Ishibashi-Ueda, H.; Hashimoto, T. Delayed diagnosis of dilated thyrotoxic cardiomyopathy with coexistent multifocal atrial tachycardia: A case report. BMC Cardiovasc. Disord. 2021, 21, 124. [Google Scholar] [CrossRef]
- Chiha, M.; Samarasinghe, S.; Kabaker, A.S. Thyroid storm: An updated review. J. Intensive Care Med. 2015, 30, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Akamizu, T.; Satoh, T.; Isozaki, O.; Suzuki, A.; Wakino, S.; Iburi, T.; Tsuboi, K.; Monden, T.; Kouki, T.; Otani, H.; et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 2012, 22, 661–679. [Google Scholar] [CrossRef] [PubMed]
- Nayak, B.; Burman, K. Thyrotoxicosis and thyroid storm. Endocrinol. Metab. Clin. N. Am. 2005, 35, 661–679. [Google Scholar] [CrossRef] [PubMed]
- Kornelius, E.; Chang, K.L.; Yang, Y.S.; Huang, J.Y.; Ku, M.S.; Lee, K.Y.; Ho, S.W. Epidemiology and factors associated with mortality of thyroid storm in Taiwan: A nationwide population-based study. Intern. Emerg. Med. 2021, 16, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Galindo, R.J.; Hurtado, C.R.; Pasquel, F.J.; García Tome, R.; Peng, L.; Umpierrez, G.E. National Trends in Incidence, Mortality, and Clinical Outcomes of Patients Hospitalized for Thyrotoxicosis with and without Thyroid Storm in the United States, 2004–2013. Thyroid 2019, 29, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Sarlis, N.J.; Gourgiotis, L. Thyroid emergencies. Rev. Endocr. Metab. Disord. 2003, 4, 129–136. [Google Scholar] [CrossRef]
- Silva, J.E.; Bianco, S.D. Thyroid-adrenergic interactions: Physiological and clinical implications. Thyroid 2008, 18, 157–165. [Google Scholar] [CrossRef]
- Lorlowhakarn, K.; Kitphati, S.; Songngerndee, V.; Tanathaipakdee, C.; Sinphurmsukskul, S.; Siwamogsatham, S.; Puwanant, S.; Ariyachaipanich, A. Thyrotoxicosis-Induced Cardiomyopathy Complicated by Refractory Cardiogenic Shock Rescued by Extracorporeal Membrane Oxygenation. Am. J. Case Rep. 2022, 23, e935029. [Google Scholar] [CrossRef] [PubMed]
- Sourial, K.; Borgan, S.M.; Mosquera, J.E.; Abdelghani, L.; Javaid, A. Thyroid Storm-induced Severe Dilated Cardiomyopathy and Ventricular Tachycardia. Cureus 2019, 11, e5079. [Google Scholar] [CrossRef]
- Abera, B.T.; Abera, M.A.; Berhe, G.; Abreha, G.; Gebru, H.T.; Abraha, H.E.; Ebrahim, M.M. Thyrotoxicosis and dilated cardiomyopathy in developing countries. BMC Endocr. Disord. 2021, 21, 132. [Google Scholar] [CrossRef] [PubMed]
- Soomro, R.; Campbell, N.; Campbell, S.; Lesniak, C.; Sullivan, M.; Ong, R.; Cheng, J.; Hossain, M.A. Thyroid storm complicated by multisystem organ failure requiring plasmapheresis to bridge to thyroidectomy: A case report and literature review. Clin. Case Rep. Rev. 2019, 5, 1–4. [Google Scholar] [CrossRef]
- Burch, H.B.; Wartofsky, L. Life-threatening thyrotoxicosis. Thyroid Storm. Endocrinol. Metab. Clin. N. Am. 1993, 22, 263–277. [Google Scholar] [CrossRef]
- Clark, O.H.; Duh, Q.; Kebebew, E. Textbook of Endocrine Surgery, 2nd ed.; Elsevier Saunders: Philadelphia, PA, USA, 2005; pp. 216–219. [Google Scholar]
- Sakaan, R.A.; Poole, M.A.; Long, B. Diltiazem-Induced Reversible Cardiogenic Shock in Thyroid Storm. Cureus 2021, 13, e19261. [Google Scholar] [CrossRef] [PubMed]
- Arai, M.; Asaumi, Y.; Murata, S.; Matama, H.; Honda, S.; Otsuka, F.; Tahara, Y.; Kataoka, Y.; Nishimura, K.; Noguchi, T. Thyroid Storm Patients with Elevated Brain Natriuretic Peptide Levels and Associated Left Ventricular Dilatation May Require Percutaneous Mechanical Support. Crit. Care Explor. 2021, 3, e0599. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, B.; Aiman, W.; Bhusal, K. Thyroid Storm. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Pandey, R.; Kumar, S.; Kotwal, N. Thyroid Storm: Clinical Manifestation, Pathophysiology, and Treatment; IntechOpen: London, UK, 2020. [Google Scholar]
- Carroll, R.; Matfin, G. Endocrine and Metabolic Emergencies: Thyroid Storm. Ther. Adv. Endocrinol. Metab. 2010, 1, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Liu, S.W.; Yang, H.; Duan, R.X.; Ren, W.X. Thyrotoxicosis after a massive levothyroxine ingestion: A case report. World J. Clin. Cases 2022, 10, 3624–3629. [Google Scholar] [CrossRef]
- Uchida, N.; Suda, T.; Ishiguro, K. Thyroidectomy in a patient with thyroid storm: Report of a case. Surg. Today 2015, 45, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Ba, J.-H.; Wu, B.-Q.; Wang, Y.-H.; Shi, Y.-F. Therapeutic plasma exchange and continuous renal replacement therapy for severe hyperthyroidism and multi-organ failure: A case report. World J. Clin. Cases 2019, 7, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.M.; Pop, A.M.C.; McDowell, E.L. A case report of thyroid storm presenting as hemodynamic instability and acute kidney injury. Oxford Med. Case Rep. 2019, 2019, 252–255. [Google Scholar]
- Alahmad, M.; Al-Sulaiti, M.; Abdelrahman, H.; El-Menyar, A.; Singh, I.; Tabeb, A.; Al-Thani, H. A Rare Case of Thyroid Storm with Refractory Hypotension and Complete Atrioventricular Block. Oxf. J. Surg. Case Rep. 2022, 2022, 1–7. [Google Scholar]
- Sadiq, A.M.; Chamba, N.G. Challenges in the Management of Thyrotoxicosis Associated with Atrial Fibrillation and Heart Failure: Two Case Reports. Clin. Med. Insights Case Rep. 2021, 14, 1179547621994573. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Iguchi, M.; Nakatani, R.; Usui, T.; Takagi, D.; Hamatani, Y.; Unoki, T.; Ishii, M.; Ogawa, H.; Masunaga, N.; et al. Thyroid Storm with Heart Failure Treated with a Short-acting Beta-adrenoreceptor Blocker, Landiolol Hydrochloride. Intern. Med. 2015, 54, 1633–1637. [Google Scholar] [CrossRef]
- Nai, Q.; Ansari, M.; Pak, S.; Tian, Y.; Amzad-Hossain, M.; Zhang, Y.; Lou, Y.; Sen, S.; Islam, M. Cardiorespiratory Failure in Thyroid Storm: Case Report and Literature Review. J. Clin. Med. Res. 2018, 10, 351–357. [Google Scholar] [CrossRef]
- Ashdown, B.; Calvello Hynes, E. Thyroid Storm-induced Takotsubo Cardiomyopathy Presenting as Acute Chest Pain: A Case Report. Clin. Pract. Cases Emerg. Med. 2021, 5, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Liao, C.-P.; Lu, C.-W.; Lin, T.-Y.; Chang, Y.-Y. Thyroid Storm Superimposed on Gestational Hypertension: A Case Report and Review of Literature. Medicina 2022, 58, 450. [Google Scholar] [CrossRef] [PubMed]
- Alam, S.; Zaman, J. Case study of thyrotoxic cardiomyopathy. BMJ Case Rep. 2019, 12, e228896. [Google Scholar] [CrossRef]
- Kinoshita, H.; Sugino, H.; Oka, T.; Ichikawa, O.; Shimonaga, T.; Sumimoto, Y.; Kashiwabara, A.; Sakai, T. A case in which SGLT2 inhibitor is a contributing factor to takotsubo cardiomyopathy and heart failure. J. Cardiol. Cases 2020, 22, 177–180. [Google Scholar] [CrossRef]
- Das, B.B.; Shakti, D.; Akam-Venkata, J.; Obi, O.; Weiland, M.D.; Moskowitz, W. SARS-CoV-2 infection induced thyroid storm and heart failure in an adolescent girl. Cardiol. Young 2022, 32, 988–992. [Google Scholar] [CrossRef]
- Witczak, J.K.; Ubaysekara, N.; Ravindran, R.; Rice, S.; Yousef, Z.; Premawardhana, L.D. Significant cardiac disease complicating Graves’ disease in previously healthy young adults. Endocrinol. Diabetes Metab. Case Rep. 2019, 2020, 19-0132. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghamdi, A.S.; Aljohani, N. Graves’ Thyrotoxicosis-Induced Reversible Cardiomyopathy: A Case Report. Clin. Med. Insights Case Rep. 2013, 6, 47–50. [Google Scholar] [CrossRef]
- Omar, S.; Ali, E.; Mazek, H.; Mahmood, T.; Soontrapa, S.; Suarez, J. Takotsubo Cardiomyopathy Associated with Hyperthyroidism Treated with Thyroidectomy. Bayl. Univ. Med. Cent. Proc. 2015, 28, 194–195. [Google Scholar] [CrossRef]
- Voll, M.; Øystese, K.A.; Høiskar, E.; Johansen, O.; Nyvold, C.; Norheim, I.; von Lueder, T.G.; Andersen, G. Case report: A patient with thyroid storm, refractory cardiogenic shock, and cardiac arrest treated with Lugol’s iodine solution and veno-arterial extracorporeal membrane oxygenation support. Eur. Heart J. 2021, 5, ytab017. [Google Scholar] [CrossRef] [PubMed]
- Pong, V.; Yeung, C.-Y.; Ko, R.L.-Y.; Tse, H.-F.; Siu, C.-W. Extracorporeal Membrane Oxygenation in Hyperthyroidism-Related Cardiomyopathy: Two Case Reports. J. Endocrinol. Metab. 2013, 3, 24–28. [Google Scholar] [CrossRef]
- Park, H.S.; Kwon, S.K.; Kim, Y.N. Successful Treatment of Thyroid Storm Presenting as Recurrent Cardiac Arrest and Subsequent Multiorgan Failure by Continuous Renal Replacement Therapy. Endocrinol. Diabetes Metab. 2017, 16, 0115. [Google Scholar] [CrossRef] [PubMed]
- Genev, I.; Lundholm, M.D.; Emanuele, M.A.; McGee, E.; Mathew, V. Thyrotoxicosis-Induced Cardiomyopathy Treated with Venoarterial Extracorporeal Membrane Oxygenation. Heart Lung 2019, 49, 165–166. [Google Scholar] [CrossRef] [PubMed]
- Chao, J.; Cook, R.; Dhingra, V. Escaping a storm alive: A case report of a young woman’s acute presentation of thyroid storm leading to cardiac arrest salvaged by VA-ECMO. J. Clin. Anesth. Intensive Care 2021, 2, 26–30. [Google Scholar]
- Rana, A.; Assad, S.; Abuzaid, M.; Farooqi, A.; Nolte, J. Thyrotoxicosis-Induced Cardiogenic Shock with Encephalopathy and Acute Respiratory Distress: A Case Report and Literature Review. Cureus 2020, 12, e8213. [Google Scholar] [CrossRef] [PubMed]
- Hsu, L.-M.; Ko, W.-J.; Wang, C.-H. Extracorporeal Membrane Oxygenation Rescues Thyrotoxicosis-Related Circulatory Collapse. Thyroid 2011, 21, 439–441. [Google Scholar] [CrossRef]
- Bou Chaaya, R.G.; Saint, L.M.; Ilonze, O.J. Thyroidectomy in Mechanical Circulatory Support—A Salvage Treatment for Thyrotoxicosis-Induced Cardiogenic Shock: Case Series. VAD J. 2021, 7, e2021710. [Google Scholar]
- Kiriyama, H.; Amiya, E.; Hatano, M.; Hosoya, Y.; Maki, H.; Nitta, D.; Saito, A.; Shiraishi, Y.; Minatsuki, S.; Sato, T.; et al. Rapid Improvement of Thyroid Storm-Related Hemodynamic Collapse by Aggressive Anti-Thyroid Therapy Including Steroid Pulse. Medicine 2017, 96, e7053. [Google Scholar] [CrossRef]
- Radhakrishnan, A.; Granato, J.E. An Association Between Takotsubo Cardiomyopathy and Thyroid Storm. Postgrad. Med. 2015, 121, 126–130. [Google Scholar] [CrossRef]
- Wu, W.-T.; Hsu, P.-C.; Huang, H.-L.; Chen, Y.-C.; Chien, S.-C. A Case of Takotsubo Cardiomyopathy Precipitated by Thyroid Storm and Diabetic Ketoacidosis with Poor Prognosis. Acta Cardiol. Sin. 2014, 30, 574–577. [Google Scholar]
- Noh, K.W.; Seon, C.S.; Choi, J.W.; Cho, Y.B.; Park, J.Y.; Kim, H.J. Thyroid Storm and Reversible Thyrotoxic Cardiomyopathy After Ingestion of Seafood Stew Thought to Contain Marine Neurotoxin. Thyroid 2011, 21, 679–682. [Google Scholar] [CrossRef] [PubMed]
- Cheah, J.M.; Ng, D.; Low, M.Y.; Foo, S.H. Weathering the Crisis: A Case of Thyroid Crisis with Propranolol-Induced Circulatory Collapse Successfully Treated with Therapeutic Plasma Exchange. ASEAN Fed. Endocr. Soc. 2019, 34, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Eliades, M.; El-Maouche, D.; Choudhary, C.; Zinsmeister, B.; Burman, K.D. Takotsubo Cardiomyopathy Associated with Thyrotoxicosis: A Case Report and Review of the Literature. Thyroid 2014, 24, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Sia, R.W.J.; Sutherland, N.; Wong, C.; Sharma, N. Takotsubo cardiomyopathy in the setting of thyroid storm. BMJ Case Rep. 2022, 15, e248353. [Google Scholar] [CrossRef]
- Misumi, K.; Kodera, S.; Nagura, F.; Kushida, S.; Shiojiri, T.; Kanda, J. Cardiac arrest caused by landiolol in a patient in thyroid crisis. J. Cardiol. Cases 2016, 14, 62–64. [Google Scholar] [CrossRef]
- Dalan, R.; Leow, M. Cardiovascular Collapse Associated with Beta Blockade in Thyroid Storm. Exp. Clin. Endocrinol. Diabetes 2007, 115, 392–396. [Google Scholar] [CrossRef]
- Subahi, A.; Ibrahim, W.; Abugroun, A. Diltiazem-Associated Cardiogenic Shock in Thyrotoxic Crisis. Am. J. Ther. 2018, 25, 1075–1078. [Google Scholar] [CrossRef]
- Muscoli, S.; Lecis, D.; Prandi, F.R.; Ylli, D.; Chiocchi, M.; Cammalleri, V.; Lauro, D.; Andreadi, A. Risk of sudden cardiac death in a case of spontaneous coronary artery dissection presenting with thyroid storm. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 3712–3717. [Google Scholar] [PubMed]
- Eltahir, M.; Chaudhry, H.; Ibrahim, E.A.; Mokhtar, M.; Jaouni, H.; Hassan, I.F.; El-Menyar, A.; Shebatta, A.L. Thyroid Storm Induced Refractory Multiorgan Failure Managed by Veno-Arterial Extracorporcal Membrane Oxygenation Support: A Case-Series. Am. J. Case Rep. 2023, 24, e940672. [Google Scholar] [CrossRef] [PubMed]
- Boccalandro, C.; Boccalandro, F.; Orlander, P.; Wei, C.F. Severe Reversible Dilated Cardiomyopathy and Hyperthyroidism: Case Report and Review of the Literature. Endocr. Pract. 2002, 9, 140–146. [Google Scholar] [CrossRef]
- Kumar, S.; Moorthy, N.; Yadav, S.; Kapoor, A.; Dale, D.C. Thyroid Storm Presenting as Congestive Heart Failure and Protein-S Deficiency-Induced Biventricular and Internal Jugular Venous Thrombii. Postgrad. Med. 2013, 59, 229–231. [Google Scholar] [CrossRef]
- Fan, X.; Liu, P.; Bai, B. Cardiogenic shock due to Takotsubo cardiomyopathy associated with thyroid crisis: A case report. Eur. Heart J. 2022, 6, ytac381. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.; Wang, C.H.; You, H.C.; Chou, N.K.; Yu, H.Y.; Chi, N.H.; Huang, S.C.; Wu, I.H.; Tseng, L.J.; Lin, M.H.; et al. Highlighting Indication of extracorporeal membrane oxygenation in endocrine emergencies. Sci. Rep. 2015, 5, 13361. [Google Scholar] [CrossRef] [PubMed]
- Meza-González, Y.A.; Alfosno-Arrieta, N.; Florez-García, V. Takotsubo syndrome and impending thyroid storm: A case report and brief review of the literature. Iberoam. J. Med. 2022, 4, 169–173. [Google Scholar] [CrossRef]
- Fu, Y.; Ge, H.; Zhang, Y.; Li, Y.; Mu, B.; Shang, W.; Li, S.; Ma, Q. Targeted Temperature Management for In-hospital Cardiac Arrest Caused by Thyroid Storm: A Case Report. Front. Cardiovasc. Med. 2021, 8, 634987. [Google Scholar] [CrossRef] [PubMed]
- Frenkel, A.; Bichovsky, Y.; Arotsker, N.; Besser, L.; Joshua, B.Z.; Fraenkel, M.; Zahger, D.; Klein, M. Ivabradine for Uncontrolled Sinus Tachycardia in Thyrotoxic Cardiomyopathy–Case Report. Endocr. Metab. Immune Disord. Drug Targets 2023, 23, 992–995. [Google Scholar] [CrossRef] [PubMed]
- Palkar, A.V.; Shrivastava, M.S.; Moulick, N.D. An unusual cause of flash pulmonary oedema. BMJ Case Rep. 2012, 2012, bcr0320126087. [Google Scholar] [CrossRef]
- Iwańczuk, W. Myocardial infarction and shock associated with thyrotoxicosis. Anestezjol. Intens. Ter. 2010, 42, 142–146. [Google Scholar]
- Jao, Y.T.F.N.; Chen, Y.; Lee, W.-H.; Tai, F.-T. Thyroid storm and ventricular tachycardia. South. Med. J. 2004, 97, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Koball, S.; Hickstein, H.; Gloger, M.; Hinz, M.; Henschel, J.; Stange, J.; Mitzner, S. Treatment of thyrotoxic crisis with plasmapheresis and single pass albumin dialysis: A case report. Artif. Organs 2010, 34, E55–E58. [Google Scholar] [CrossRef] [PubMed]
- Eyadiel, L.; Amjad, A.; Pisani, B.; Miller, P.; Jain, R. Use of Therapeutic Plasma Exchange and ECMO Support with Impella for LV Vent as Treatment for Cardiogenic Shock in Acute Thyrotoxicosis/Thyroid Storm. J. Card. Fail. 2018, 24, S84–S85. [Google Scholar] [CrossRef]
- Karahalios, B.A.; Singh, R.; Boyd, K.; Ogbonna, M. A Perfect Storm: A Case Of Managing Cardiogenic Shock Due To Thyrotoxic Cardiomyopathy with Extracorporeal Membrane Oxygenation. J. Hosp. Med. 2020, 796, Abstract published at Hospital Medicine 2020, Virtual Competition. [Google Scholar]
- Neary, N.M.; Fountain, A.E.C.; Hatfield, E.C.I.; Fox, K.F.; Meeran, K. Thyroid storm induced cardiomyopathy is reversible. Endocr. Abstr. 2006, 11, 993. [Google Scholar]
- Sugiyama, Y.; Tanaka, R.; Yoshiyama, Y.; Ichino, T.; Hishinuma, N.; Shimizu, S.; Imai, N.; Mitsuzawa, K.; Kawamata, M. A case of sudden onset of thyroid storm just before cesarean section manifesting congestive heart failure and pulmonary edema. JA Clin. Rep. 2017, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, S.; Galan, Y.; Tripathi, S.; Cardinale, M.; Van Hoven, A.M.; Yegneswaran, B. Thyrotoxic crisis and heart failure: An approach to navigate the storm. CHEST Annu. Meet. 2018, 154, 264. [Google Scholar] [CrossRef]
- Schwab, K.; Stretch, R.; Zeidler, M. Shock from the storm: A case of contrast-induced thyroid storm and cardiogenic shock. Chest J. 2018, 154, 299. [Google Scholar] [CrossRef]
- Ahmad, K.; Nazir, U.; Rachid, M.; Yasmeen, T. A deadly storm: Catastrophic thyroid storm with DIC and cardiomyopathy. Am. J. Respir. Crit. Care Med. 2017, 195, A3819. [Google Scholar]
- Komiyama, C.; Tomita, Y.; Kodama, T.; Ishiwata, S.; Ohno, M. A case of thyroid storm diagnosed with severe heart failure complicated by DIC. In Proceedings of the 20th Annual Scientific Meeting, Yokohama City, Japan, 16–19 September 2016. Abstract number P5–4. [Google Scholar]
- Al-Hilal, M.Y.; Putra, M.M.R.; Ummah, K. Thyroid heart disease presenting thyrotoxic crisis with jaundice. Clin. Res. J. Intern. Med. 2023, 4, 426–433. [Google Scholar]
- Wald, D.A.; Silver, A. Cardiovascular manifestations of thyroid storm: A case report. J. Emerg. Med. 2003, 25, 23–28. [Google Scholar] [CrossRef]
- White, A.; Bozso, S.J.; Moon, M.C. Thyrotoxicosis induced cardiomyopathy requiring support with extracorporeal membrane oxygenation. J. Crit. Care 2018, 45, 140–143. [Google Scholar] [CrossRef] [PubMed]
- AlShehri, S.; Alajmi, S.; Ekhzaimy, A.; Aldawas, S.; Alalwan, M. Thyroid Storm in a Patient with Alemtuzumab-Induced Graves’ Disease: A Case Report. Cureus 2022, 14, e24570. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.-Y.; Yu, W.-L. A case report of thyroid storm induced by acute sepsis. J. Acute Dis. 2016, 5, 160–161. [Google Scholar] [CrossRef]
- Sundar, R.; Ramaswamy, M. Thyroid storm—A case report. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 559–560. [Google Scholar] [CrossRef] [PubMed]
- Fatima, S.; Puri, R.; Patnaik, S.; Mora, J. When A Toxic Thyroid Makes The Liver Toxic: A Case Of Thyroid Storm Complicated By Acute Liver Failure. AACE Clin. Case Rep. 2017, 3, e200–e204. [Google Scholar] [CrossRef]
- Balachandran, V. Acute medical thyroid storm—A report of 7 cases. Thyroid. Res. Pract. 2007, 4, 84–88. [Google Scholar]
- Jiang, S.; Hernande, E. A Case of Thyroid Storm: Unusual Presentation in a Young Man. Proc. UCLA Health 2019, 23. [Google Scholar]
- Khanna, N.; Peralta, S.; Zhang, R.; Thiesen, J.; Ranasinghe, L. Schistosomiasis of the Cervix: Thyroid Storm: An Elusive but Deadly Diagnosis—A Case Report. Int. J. Biomed Res. 2022, 2. [Google Scholar] [CrossRef]
- Kwon, S.H.; Kim, M.J.; Jung, S.Y.; Jeon, J.H. Thyroid storm caused by metastatic papillary thyroid carcinoma tissue after total thyroidectomy: A case report. J. Yeungnam Med. Sci. 2023. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.A.; Baek, Y.H.; Park, T.S.; Lee, K.A. A Case of Acute Cerebral Infarction and Thyroid Storm Associated with Moyamoya Disease. Int. J. Thyroidol. 2017, 10, 56–60. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Takahashi, A.; Shirakami, A.; Kageyama, N.; Kitazoe, K.; Fujinaga, H. A case of thyroid crisis with worsening jaundice despite improvements in heart failure. J. Endocrinol. Metab. 2016, 6, 59–63. [Google Scholar] [CrossRef]
- Talwalkar, P.G. Thyroid storm presenting with severe hypoglycemia: A case report. Clin. Diabetol. 2022, 11, 57–59. [Google Scholar] [CrossRef]
- Seffah, K.; Lamptey, R.; Ibrahim, S.; Agyeman, W.Y.; Addo, B. The Thyroid Forecast: A Case of a Thyroid Storm Diagnosed Under Unforeseen Circumstances. Cureus 2023, 15, e37707. [Google Scholar] [CrossRef]
- Onsoi, W.; Srilanchakon, K.; Aroonparkmongkol, S.; Supornsilchai, V. Coexistence of Graves’ disease with acute rheumatic fever treated as thyroid storm in young Thai patient. J. Pediatr. Endocrinol. Metab. 2023, 36, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, J.; Li, Z. PICU treatment of 3 cases of pediatric thyroid storm: Case series and literature review. Medicine 2023, 102, e33447. [Google Scholar] [CrossRef]
- Herzallah, Z.N.; Gupta, S.; Abdulhamid, M.D.; Muhammed Noori, O.Q. Esmolol Is Not the Solution: Thyroid Storm with Atrial Fibrillation. Cureus 2023, 15, e35201. [Google Scholar] [CrossRef] [PubMed]
- Obi, M.F.; Namireddy, V.; Garg, Y.; Sharma, M. Benefit and Preference of Propranolol Over Metoprolol in Thyrotoxicosis-Induced Atrial Fibrillation: A Case Report and Review of Literature. Cureus 2023, 15, e34474. [Google Scholar] [CrossRef]
- Yan, B.C.; Luo, R.R. Thyrotoxicosis in patients with a history of Graves’ disease after SARS-CoV-2 vaccination (adenovirus vector vaccine): Two case reports. World J. Clin. Cases 2023, 11, 1122–1128. [Google Scholar] [CrossRef]
- Ohya, A.; Ohtake, M.; Kawamura, Y.; Akimoto, T.; Iwashita, M.; Yamamoto, T.; Takeuchi, I. Diagnosis and treatment approaches for simultaneous onset of subarachnoid hemorrhage and thyroid storm: A case report. Int. J. Emerg. Med. 2023, 16, 15. [Google Scholar] [CrossRef]
- Kataoka, S.; Matsuno, K.; Sugano, K.; Takahashi, K. Thyroid storm induced by combined nivolumab and ipilimumab immunotherapy in advanced non-small cell lung cancer. BMJ Case Rep. 2022, 15, e250696. [Google Scholar] [CrossRef]
- Hanson, V.; Khalid, S.N.; Ratmeyer, G.; Sheikh, A.B. Thyroid storm secondary to acute Streptococcus pyogenes pharyngitis. Proceedings 2022, 35, 691–692. [Google Scholar] [CrossRef] [PubMed]
- Rocha, M.H.; Conde, A.; Nogueira-Silva, L.; Nogueira, F.; Almeida, J.S. Flash Pulmonary Edema: A Rare Presentation of Graves’ Disease. Cureus 2022, 14, e25833. [Google Scholar] [CrossRef]
- Jiménez-Labaig, P.; Mañe, J.M.; Rivero, M.P.; Lombardero, L.; Sancho, A.; López-Vivanco, G. Just an Acute Pulmonary Edema? Paraneoplastic Thyroid Storm Due to Invasive Mole. Case Rep. Oncol. 2022, 15, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Thakur, C.; Kumar, P.; Goyal, J.P.; Vyas, V. Thyroid Storm in an Adolescent Girl Precipitated by Empyema Thoracis. Oman Med. J. 2022, 37, e371. [Google Scholar] [CrossRef]
- Fransen, S.; Do, T.; Alaie, M. The Perfect Storm: A Case of Thyrotoxic Crisis Masking as Altered Mental Status in the South Bronx. Cureus 2022, 14, e24510. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Asaumi, Y.; Kataoka, Y.; Noguchi, T. Continuous improvement of both hepatic and cardiac dysfunction by sequential plasma exchange in a patient with thyrotoxicosis and cardiogenic shock: A case report indicating the potential role of cardiohepatic interactions during thyroid storm. Eur. Heart J. Case Rep. 2022, 6, ytac197. [Google Scholar] [CrossRef] [PubMed]
- Raza, M.A.; Jain, A.; Mumtaz, M.; Mehmood, T. Thyroid Storm in a Patient on Chronic Amiodarone Treatment. Cureus 2022, 14, e24164. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.H.; Lian, H.W.; Sung, Y.F. Cystic Encephalomalacia in a Young Woman After Cardiac Arrest Due to Diabetic Ketoacidosis and Thyroid Storm. Cureus 2022, 14, e23707. [Google Scholar] [CrossRef]
- Pranasakti, M.E.; Talirasa, N.; Rasena, H.A.; Purwanto, R.Y.; Anwar, S.L. Thyrotoxicosis occurrence in SARS-CoV-2 infection: A case report. Ann. Med. Surg. 2022, 78, 103700. [Google Scholar] [CrossRef] [PubMed]
- Rushing, M.W.; Rebolledo, M.A.; Lahoti, A.; Alemzadeh, R. Acute febrile illness in a teenage female with history of Graves’ disease. Oxf. Med. Case Rep. 2023, 2023, omad050. [Google Scholar] [CrossRef]
- Jayasuriya, A.; Muthukuda, D.; Dissanayake, P.; Subasinghe, S. Recurrent Thyroid Storm Caused by a Complete Hydatidiform Mole in a Perimenopausal Woman. Case Rep. Endocrinol. 2020, 2020, 8842987. [Google Scholar] [CrossRef] [PubMed]
- Daffini, L.; Pirola, I.; Saccà, G.; Salvetti, M.; Cappelli, C. Graves’ disease treated by complementary medicine leading to thyroid storm: A case report. Casp. J. Intern. Med. 2021, 12 (Suppl. 2), S371–S375. [Google Scholar] [CrossRef]
- Gill, J.H.; Nam, T.K.; Jung, H.K.; Jang, K.M.; Choi, H.H.; Park, Y.S.; Kwon, J.T. Acute cerebral infarction combined with a thyroid storm in a patient with both Moyamoya syndrome and Graves’ disease. J. Cerebrovasc. Endovasc. Neurosurg. 2022, 24, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Takedani, K.; Notsu, M.; Adachi, N.; Tanaka, S.; Yamamoto, M.; Yamauchi, M.; Yamauchi, N.; Maruyama, R.; Kanasaki, K. Thyroid crisis caused by metastatic thyroid cancer: An autopsy case report. BMC Endocr. Disord. 2021, 21, 213. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Sarfraz, S.; Hassan, L.; Ali, H. Atrial Fibrillation as an Initial Presentation of Apathetic Thyroid Storm. Cureus 2021, 13, e17786. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, S.; Sarwani, A.; Al Fardan, R.; Maki, M.; Al Saeed, M. A Uniquely Challenging Case of Poorly Controlled Hyperthyroidism with a Coexisting Thyroglossal Cyst. Cureus 2021, 13, e14271. [Google Scholar] [CrossRef]
- Vinan-Vega, M.; Mantilla, B.; Jahan, N.; Peminda, C.; Nugent, K.; Lado-Abeal, J.; Rivas, A. Usefulness of plasmapheresis in patients with severe complicated thyrotoxicosis. Proceedings 2020, 34, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Tee, H.C.; Khoo, S.S.K.; Fung, Y.K. Thyroid Storm with Acute Flaccid Quadriparesis due to Thyrotoxic Myopathy: A Case Report. J. ASEAN Fed. Endocr. Soc. 2020, 35, 118–121. [Google Scholar] [CrossRef]
- Shang, W.; Ma, Q.B. Malignant Arrhythmias as the Unmasked Manifestation of Thyroid Storm. Int. J. Gen. Med. 2020, 13, 693–698. [Google Scholar] [CrossRef]
- Higaki, T.; Tsukahara, K.; Obara, T.; Nojima, T.; Yamamoto, H.; Osako, T.; Naito, H.; Nakao, A. Pediatric airway compromise due to thyroid storm associated with influenza A infection: A case report. Respir. Med. Case Rep. 2020, 31, 101182. [Google Scholar] [CrossRef] [PubMed]
- Mathai, C.; Coppola, A.; Vaz, C.L. Thyroid abscess after injection of heroin into the neck complicated by thyroid storm. AACE Clin. Case Rep. 2020, 6, e183–e188. [Google Scholar] [CrossRef]
- Chauhan, J.C.; Frizzola, M.; McMahon, K.; Perry, S.; Hertzog, J.H. Thyroid storm with encephalopathy and cardiovascular symptoms refractory to medical management in an adolescent. Int. J. Crit. Illn. Inj. Sci. 2020, 10, 38–41. [Google Scholar] [CrossRef]
- Pandya, M.; Garcia, R.A.; Awori, J. Thyrotoxicosis in a pediatric patient with supraventricular tachycardia and borderline features of thyroid storm. AACE Clin. Case Rep. 2019, 5, e393–e395. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.W.; Wee, H.C.; Sonawane, V. Flail mitral valve: A rare complication of a thyroid storm. AACE Clin. Case Rep. 2019, 5, e4–e6. [Google Scholar] [CrossRef]
- Lee, J.H. Thyroid storm after coronary artery bypass surgery: A case report. J. Cardiothorac. Surg. 2020, 15, 22. [Google Scholar] [CrossRef]
- Conte, J.I.; Arosemena, M.A.; Kapoor, K.; Dempsey, N.G.; Zaleski, M.L.; Kargi, A.Y. Thyroid Storm Triggered by Strangulation in a Patient with Undiagnosed Graves’ Disease. Case Rep. Endocrinol. 2018, 2018, 4190629. [Google Scholar] [CrossRef]
- Kalpakam, H.; Dhooria, S.; Agarwal, R.; Mukherjee, S.; Sehgal, I.S. A rare complication of bedside tracheotomy: Thyroid crisis. Lung India 2019, 36, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Neiva, J.; Fernandes, G.; Carvalho, D.; Ferreira, B.; Duarte, R.; Araújo, R. Thyroid storm and myxoedema: Two reversible causes of acute heart failure. Acute Med. 2018, 17, 229–231. [Google Scholar] [CrossRef]
- Godo, S.; Kawazoe, Y.; Ozaki, H.; Fujita, M.; Kudo, D.; Nomura, R.; Shimokawa, H.; Kushimoto, S. Switching Therapy from Intravenous Landiolol to Transdermal Bisoprolol in a Patient with Thyroid Storm Complicated by Decompensated Heart Failure and Gastrointestinal Dysfunction. Intern. Med. 2017, 56, 2603–2609. [Google Scholar] [CrossRef] [PubMed]
- Ikeoka, T.; Otsuka, H.; Fujita, N.; Masuda, Y.; Maeda, S.; Horie, I.; Ando, T.; Abiru, N.; Kawakami, A. Thyroid Storm Precipitated by Diabetic Ketoacidosis and Influenza A: A Case Report and Literature Review. Intern. Med. 2017, 56, 181–185. [Google Scholar] [CrossRef]
- Ishihara, Y.; Sugawa, T.; Kaneko, H.; Hiroshima-Hamanaka, K.; Amano, A.; Umakoshi, H.; Tsuiki, M.; Kusakabe, T.; Satoh-Asahara, N.; Shimatsu, A.; et al. The Delayed Diagnosis of Thyroid Storm in Patients with Psychosis. Intern. Med. 2019, 58, 2195–2199. [Google Scholar] [CrossRef]
- Chantra, M.; Limsuwan, A.; Mahachoklertwattana, P. Low cardiac output thyroid storm in a girl with Graves’ disease. Pediatr. Int. 2016, 58, 1080–1083. [Google Scholar] [CrossRef] [PubMed]
- Nakabayashi, K.; Nakazawa, N.; Suzuki, T.; Asano, R.; Saito, H.; Nomura, H.; Isomura, D.; Okada, H.; Sugiura, R.; Oka, T. Thyroid Echography-induced Thyroid Storm and Exacerbation of Acute Heart Failure. Intern. Med. 2016, 55, 2209–2212. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.D.; Seak, C.J.; Lin, C.C.; Lin, L.J. Thyroid storm precipitated by organophosphate intoxication. Am. J. Emerg. Med. 2007, 25, 861.e1–861.e3. [Google Scholar] [CrossRef] [PubMed]
- Opdahl, H.; Eritsland, J.; Søvik, E. Acute myocardial infarction and thyrotoxic storm--a difficult and dangerous combination. Acta Anaesthesiol. Scand. 2005, 49, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, C.; Sasaki, H.; Kosuge, K.; Miyakita, Y.; Hayakawa, M.; Suzuki, A.; Abe, E.; Suzuki, K.; Aizawa, Y. Severe starvation hypoglycemia and congestive heart failure induced by thyroid crisis, with accidentally induced severe liver dysfunction and disseminated intravascular coagulation. Intern. Med. 2005, 44, 234–239. [Google Scholar] [CrossRef]
- Lin, C.H.; Chen, S.C.; Lee, C.C.; Ko, P.C.; Chen, W.J. Thyroid storm concealing diabetic ketoacidosis leading to cardiac arrest. Resuscitation 2004, 63, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Shimizu, Y.; Nakata, J.; Kameda, T.; Muto, M.; Ohsawa, I.; Io, H.; Hamada, C.; Horikoshi, S.; Tomino, Y. Thyroid storm masked by hemodialysis and glucocorticoid therapy in a patient with rheumatoid arthritis. Case Rep. Nephrol. Urol. 2012, 2, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Amos, S.; Pollack, R.; Sarig, I.; Rudis, E.; Hirshoren, N.; Weinberger, J.; Arad, A.; Fischer, M.; Talmon, A.; Stokar, J. VA-ECMO for Thyroid Storm: Case Reports and Review of the Literature. Isr. Med. Assoc. J. 2023, 25, 349–350. [Google Scholar] [PubMed]
- Samra, T.; Kaur, R.; Sharma, N.; Chaudhary, L. Peri-operative concerns in a patient with thyroid storm secondary to molar pregnancy. Indian J. Anaesth. 2015, 59, 739–742. [Google Scholar] [CrossRef]
- Kitazawa, C.; Aoki, S.; Takahashi, T.; Hirahara, F. Acute respiratory failure due to thyroid storm developing immediately after delivery. Clin. Case Rep. 2015, 3, 997–999. [Google Scholar] [CrossRef] [PubMed]
- Lane, A.S.; Tarvade, S. Thyroid storm causing placental abruption: Cardiovascular and management complications for the Intensivist. J. Intensive Care Soc. 2015, 16, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Moraco, A.H.; Banauch, G.; Kopec, S. A 46-Year-Old Woman with Dyspnea From an Inhalational Exposure Triggering Thyroid Storm and Subsequent Multi-Organ System Failure. J. Intensive Care Med. 2015, 30, 518–520. [Google Scholar] [CrossRef]
- Shrum, J.M.; Byers, B.; Parhar, K. Thyroid storm following suicide attempt by hanging. BMJ Case Rep. 2014, 2014, bcr2014204589. [Google Scholar] [CrossRef]
- Agabiti Rosei, C.; Cappelli, C.; Salvetti, M.; Castell, M.; Muiesan, M.L.; Agabiti Rosei, E. The unusual clinical manifestation of thyroid storm. Intern. Emerg. Med. 2011, 6, 385–387. [Google Scholar] [CrossRef]
- Umezu, T.; Ashitani, K.; Toda, T.; Yanagawa, T. A patient who experienced thyroid storm complicated by rhabdomyolysis, deep vein thrombosis, and a silent pulmonary embolism: A case report. BMC Res. Notes 2013, 6, 198. [Google Scholar] [CrossRef]
- Han, K.S.; Kim, J.Y.; Choi, S.H.; Yoon, Y.H. A report of therapeutic hypothermia for postcardiac arrest care due to thyroid storm. Kaohsiung J. Med. Sci. 2014, 30, 539–540. [Google Scholar] [CrossRef] [PubMed]
- Kofinas, J.D.; Kruczek, A.; Sample, J.; Eglinton, G.S. Thyroid storm-induced multi-organ failure in the setting of gestational trophoblastic disease. J. Emerg. Med. 2015, 48, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Karkowski, K.; Carroll, J.L., Jr. A Case of Thyroid Storm Induced by Iodine-Containing Dietary Supplements and Homeopathic Remedies. J. Pharm. Technol. 2014, 30, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Alkhuja, S.; Pyram, R.; Odeyemi, O. In the eye of the storm: Iodinated contrast medium induced thyroid storm presenting as cardiopulmonary arrest. Heart Lung 2013, 42, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Anjo, D.; Maia, J.; Carvalho, A.C.; Castro, H.; Aragão, I.; Vieira, A.P.; Reis, A.H.; Borges, F.; Torres, S. Thyroid storm and arrhythmic storm: A potentially fatal combination. Am. J. Emerg. Med. 2013, 31, 1418.e3–1418.e5. [Google Scholar] [CrossRef] [PubMed]
- Nakatani, Y.; Monden, T.; Sato, M.; Domeki, N.; Matsumura, M.; Banba, N.; Nakamoto, T. Severe hypoglycemia accompanied with thyroid crisis. Case Rep. Endocrinol. 2012, 2012, 168565. [Google Scholar] [CrossRef] [PubMed]
- Harada, Y.; Akiyama, H.; Yoshimoto, T.; Urao, Y.; Ryuzaki, M.; Handa, M. Thyroid storm with multiple organ failure, disseminated intravascular coagulation, and stroke with a normal serum FT3 level. Intern. Med. 2012, 51, 2379–2383. [Google Scholar] [CrossRef]
- Al Bannay, R.; Husain, A.; Khalaf, S. Complete heart block in thyrotoxicosis, is it a manifestation of thyroid storm? A case report and review of the literature. Case Rep. Endocrinol. 2012, 2012, 318398. [Google Scholar] [CrossRef]
- Kibirige, D.; Kiggundu, D.S.; Sanya, R.; Mutebi, E. Cholestatic hepatic injury due to a thyroid storm: A case report from a resource limited setting. Thyroid. Res. 2012, 5, 6. [Google Scholar] [CrossRef]
- Deng, Y.; Zheng, W.; Zhu, J. Successful treatment of thyroid crisis accompanied by hypoglycemia, lactic acidosis, and multiple organ failure. Am. J. Emerg. Med. 2012, 30, 2094.e5–2094.e6. [Google Scholar] [CrossRef]
- Yoshino, T.; Kawano, D.; Azuhata, T.; Kuwana, T.; Kogawa, R.; Sakurai, A.; Tanjoh, K.; Yanagawa, T. A patient with Graves’ disease who survived despite developing thyroid storm and lactic acidosis. Upsala J. Med. Sci. 2010, 115, 282–286. [Google Scholar] [CrossRef]
- Vyas, A.A.; Vyas, P.; Fillipon, N.L.; Vijayakrishnan, R.; Trivedi, N. Successful treatment of thyroid storm with plasmapheresis in a patient with methimazole-induced agranulocytosis. Endocr. Pract. 2010, 16, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.T.; Yang, G.G.; Hsu, Y.H. Thyroid storm and lymphocytic myocarditis. Intern. Med. 2010, 49, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Torigoe, K.; Suzuki, H.; Nakajima, W.; Takahashi, M.; Aoyagi, M. Masui. Jpn. J. Anesthesiol. 2010, 59, 257–259. [Google Scholar]
- Chong, H.W.; See, K.C.; Phua, J. Thyroid storm with multiorgan failure. Thyroid 2010, 20, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.J.; Wilson, C.M.; Dolan, S.J.; Kennedy, A.; McCance, D.R. Reversible dilated cardiomyopathy associated with post-partum thyrotoxic storm. QJM 2009, 102, 217–219. [Google Scholar] [CrossRef]
- Izumi, K.; Kondo, S.; Okada, T. A case of atypical thyroid storm with hypoglycemia and lactic acidosis. Endocr. J. 2009, 56, 747–752. [Google Scholar] [CrossRef]
- Wong, I.M.J.; Lim, J.Y.; Goh, J.T.K.; Tan, Q.L.; Tay, C.K. Thyroid storm rescued by extracorporeal membrane oxygenation support, plasmapheresis and thyroidectomy: A case report. J. Emerg. Crit. Care Med. 2021, 5, 19. [Google Scholar] [CrossRef]
- Lim, S.L.; Wang, K.; Lui, P.L.; Ramanathan, K.; Yang, S.P. Crash Landing of Thyroid Storm: A Case Report and Review of the Role of Extra-Corporeal Systems. Front. Endocrinol. 2021, 12, 725559. [Google Scholar] [CrossRef]
- Allencherril, J.; Birnbaum, I. Heart Failure in Thyrotoxic Cardiomyopathy: Extracorporeal Membrane Oxygenation Treatment for Graves’ Disease. JECT 2015, 47, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Manuel, L.; Fong, L.; Lahanas, A.; Grant, P. How to do it: Plasmapheresis via venoarterial extracorporeal membrane oxygenation circuit for thyroid storm. Ann. Med. Surg. 2021, 67, 102485. [Google Scholar] [CrossRef] [PubMed]
- Koh, H.; Kaushik, M.; Loh, J.K.; Chng, C.L. Plasma exchange and early thyroidectomy in thyroid storm requiring extracorporeal membrane oxygenation. Endocrinol. Diabetes Metab. Case Rep. 2019, 2019, EDM190051. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Cham, M.D.; Huang, G.S. Storm and STEMI: A case report of unexpected cardiac complications of thyrotoxicosis. Eur. Heart J. Case Rep. 2020, 4, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Mostafa, W.; Fernandez, C.; Ahmad, H.; Htwe, N. Apathetic Thyroid Storm with Cardiorespiratory Failure, Pulmonary Embolism, and Coagulopathy in a Young Male with Graves’ Disease and Myopathy. Case Rep. Endocrinol. 2020, 2020, 8896777. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, M.; Tanaka, T.; Wakamiya, A.; Tamanaha, T.; Makino, H.; Tanei, T.; Aiba, T.; Kusano, K.; Hosoda, K. First Case Report of Arrhythmogenic Right Ventricular Cardiomyopathy Showing Refractory Ventricular Tachycardia Induced by Thyroid Storm due to Graves’ Disease. Case Rep. Endocrinol. 2022, 2022, 6078148. [Google Scholar] [CrossRef]
- Caruso, E.; Iliadis, E. Cardiogenic shock in thyroid storm: A biventricular impella (Bi-Pella) approach. Clin. Case Rep. 2021, 9, 1104–1109. [Google Scholar] [CrossRef]
- Abbasi, A.A.; Chandar, P.; Shankar, S.; Gupta, S.S.; Kupfer, Y. Thyrotoxic Periodic Paralysis and Cardiomyopathy in a Patient with Graves’ Disease. Cureus 2018, 10, e2837. [Google Scholar] [CrossRef] [PubMed]
- Meregildo Rodriguez, E.D.; Gordillo Velásquez, L.I.; Alvarado Moreno, J.G. Diabetic Ketoacidosis Associated with Thyroxine (T4) Toxicosis and Thyrotoxic Cardiomyopathy. Medicina 2018, 54, 93. [Google Scholar] [CrossRef]
- Mathew, G.M.; Rodriguez, A.; Lawrence, L.; Krishnasamy, K.P.; Marok, R.S.; Pauwaa, S.; Dia, M.; Macaluso, G.P.; Drever, E.D.; Yasmeen, T. A Unique Presentation of Thyroid Storm and Myopericarditis in a Young Muscular Man. AACE Clin. Case Rep. 2017, 3, e74–e78. [Google Scholar] [CrossRef]
- Underland, L.J.; Villeda, G.A.; Pal, A.; Lam, L. A Case of Thyroid Storm Associated with Cardiomyopathy and Poststreptococcal Glomerulonephritis. Case Rep. Pediatr. 2016, 2016, 7192359. [Google Scholar] [CrossRef]
- Nakashima, Y.; Kenzaka, T.; Okayama, M.; Kajii, E. A Case of Thyroid Storm with Cardiac Arrest. Int. Med. Case Rep. J. 2019, 12, 413–416. [Google Scholar]
- Ozcan, E.E.; Dogdus, M.; Yilancioglu, R.Y.; Adiyman, S.C.; Turan, O.E. Invasive Heart Rate Control as a Salvage Therapy in Amiodarone-induced Thyroid Storm. Medeniyet Med. J. 2022, 37, 119–122. [Google Scholar] [CrossRef]
- Çiçek, V.; Çınar, T.; Selçuk, M.; Orhan, A.L. Acute Thyrotoxicosis Induced Reversible Cardiomyopathy in an Adult Patient. Hamidiye Med. J. 2021, 2, 138–140. [Google Scholar] [CrossRef]
- Bokhari, S.F.H.; Sattar, H.; Abid, S.; Vohra, R.R.; Sajid, S. Cardiovascular Collapse Secondary to Beta-Blocker Administration in a Setting of Coexisting Thyroid Storm and Atrial Fibrillation: A Case Report. Cureus 2022, 14, e29321. [Google Scholar] [CrossRef] [PubMed]
- Tolu-Akinnawo, O.Z.; Abiade, J.; Awosanya, T.; Okafor, H.E. Thyrotoxicosis-Induced Cardiogenic Shock: Acute Management Using a Multidisciplinary Approach. Cureus 2022, 14, e32841. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, H.; Singh, V.; Arora, A.; Alsunaid, S. Propranolol-Induced Circulatory Collapse in a Patient with Thyroid Crisis and Underlying Thyrocardiac Disease: A Word of Caution. J. Investig. Med. High Impact Case Rep. 2017, 5, 2324709617747903. [Google Scholar] [CrossRef]
- Zayour, M.; Yasmin, F.A.; Baydoun, A.; Tawk, M.; Sleiman, D.; Shatila, W.; Chamoun, C. Cardiac Arrest as First Presentation of Thyroid Storm. Cureus 2023, 15, e37057. [Google Scholar] [CrossRef] [PubMed]
- Ngo, A.S.-Y.; Tan, D.C.L. Thyrotoxic heart disease. Resuscitation 2006, 70, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Ueno, A.; Yamamoto, T.; Sato, N.; Tanaka, K. Ventricular fibrillation associated with early repolarization in a patient with thyroid storm. J. Interv. Card. Electrophysiol. 2010, 29, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Omar, A.M.A.; Knott, K.; Saba, M.M.; Lim, P.O. Cardiac arrest in myocardial infarction with non-obstructive coronary artery (MINOCA) secondary to thyroid dysfunction. BMJ Case Rep. 2023, 16, e253500. [Google Scholar] [CrossRef]
- Chan, V.; Minalyan, A.; Raza, A.; Christensen, G. A heartbreaking case of emotional stress-induced thyroid storm. In Proceedings of the CHEST Annual Meeting, Chicago, IL, USA, 18–21 October 2020. Abstract number A867. [Google Scholar]
- Kauth, M.; Sheikh, A.; Hinkle, L. In the "I" of the Storm: Thyroid Storm Induced by Iodine Contrast in Thyrotoxicosis. Am. J. Respir. Crit. Care Med. 2019, 199, A1713. [Google Scholar] [CrossRef]
- Patel, S.; Gong, A.O.; Shah, S.; Rodrigues, S.; Barajas, S.; Pizula, J.; LoPresti, J.; Garg, P. Management of cardiogenic shock in a patient with thyroid storm and methamphetamine associated cardiomyopathy. J. Am. Coll. Cardiol. 2021, 77, 2322. [Google Scholar] [CrossRef]
- Starobin, B.; Afari, M. Through The Storm: Veno-Arterial Extracorporeal Membranous Oxygenation Therapy For Treatment of Thyroid Storm Induced Cardiogenic Shock. J. Am. Coll. Cardiol. 2021, 77 (Suppl. 1), 215. [Google Scholar] [CrossRef]
- Methvin, L.; Warner, J.; Gilstrap, L.G. Cardiogenic shock in thyroid storm: The importance of EF assessment prior to initiation of treatment. J. Am. Coll. Cardiol. 2022, 79, 2594. [Google Scholar] [CrossRef]
- Abdelrahman, H.; Davoodi, K.; Coppinger, A.; Chen, K.; Sullivan, J. The Calm Before the Storm: Cardiogenic Shock in Graves’ Disease. Endocr. Pract. 2023, 29, S114. [Google Scholar] [CrossRef]
- Naik, S.K.; Hallak, N.; Patel, R.; Esan, A.; Saleh, A.; Sung, A.; Raoof, S. Reversible thyrotoxic cardiomyopathy: Prompt. Chest 2009, 136, 37S. [Google Scholar] [CrossRef]
- Choi, Y.J.; Jang, J.H.; Park, S.H.; Oh, J.-H.; Koh, D.K. Dilated cardiomyopathy with Graves disease in a young child. Ann. Pediatr. Endocrinol. Metab. 2016, 21, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Seol, S.-H.; Kim, Y.-S.; Kim, D.-K.; Kim, K.-H.; Kim, D.-I. Thyrotoxicosis induced cardiogenic shock rescued by extracorporeal membrane oxygenation. J. Geriatr. Cardiol. 2018, 15, 203–204. [Google Scholar] [PubMed]
- Shimoda, Y.; Satoh, T.; Takahashi, H.; Katano-Toki, A.; Ozawa, A.; Tomaru, T.; Horiguchi, N.; Kaira, K.; Nishioka, M.; Shibusawa, N.; et al. A case of thyroid storm with a markedly elevated level of circulating soluble interleukin-2 receptor complicated by multiple organ failure and disseminated intravascular coagulation syndrome. Endocr. J. 2014, 61, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Carhill, A.; Gutierrez, A.; Lakhia, R.; Nalini, R. Surviving the storm: Two cases of thyroid storm successfully treated with plasmapheresis. BMJ Case Rep. 2012, 2012, bcr2012006696. [Google Scholar] [CrossRef]
- Koritarov, T.; Coppinger, A.; Krasnow, D.; DeMoranville, B. Abstract #1184827: Thyroid Storm Presenting as Acute Decompensated Biventricular Heart Failure in a Young Male. Endocr. Pract. 2022, 28, S155. [Google Scholar]
- Al Khodari, K.; Tahtouh, R.A.; Hamid, T. Acute ST-Elevation Myocardial Infarction in Patient with Severe Uncontrolled Hyperthyroidism Complicated by Thyroid Storm. Heart Views 2022, 23, 221–225. [Google Scholar]
- Milani, N.; Najafpour, M.; Mohebbi, M. Case series: Rare cases of thyroid storm in COVID-19 patients. Clin. Case Rep. 2021, 9, e04772. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Sengul, A.; Güvener, N. Trauma induced thyroid storm complicated by multiple organ failure. Chin. Med. J. 2005, 118, 963–965. [Google Scholar] [PubMed]
- Khurana, K.; Kumar, S.; Acharya, S.; Toshniwal, S.; Pantbalekundri, N. Thyroid Storm Masquerading as Multiple Organ Dysfunction Syndrome: Catch Me if You Can. Cureus 2023, 15, e39584. [Google Scholar] [CrossRef] [PubMed]
- Oredegbe, A.A.; Awad, M. Catecholamine Mega Storm Triggered by Cocaine Use and Thyrotoxicosis Crisis. Cureus 2023, 15, e38299. [Google Scholar] [CrossRef] [PubMed]
- Sneyers Closa, M.; Pérez Requena, A.; Sánchez García, S.; Sistac Ballarín, J. Anaesthetic management of thyroid storm in a patient with Friederich’s ataxia. A case report. Rev. Esp. Anestesiol. Reanim. 2023, 70, 362–365. [Google Scholar] [CrossRef]
- Makino, M.; Koriyama, N.; Kojima, N.; Nishio, Y. A Rare Case of Painless Destructive Thyroiditis Resulting in Thyroid Storm. Intern. Med. 2023. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, D.; Osaki, Y.; Suzuki, H.; Shimano, H. Takotsubo cardiomyopathy with left ventricle thrombus caused by subacute thyroiditis. BMJ Case Rep. 2023, 16, e250540. [Google Scholar] [CrossRef]
- Dhir, N.; Haneke, T.; Mixon, T. Mechanical circulatory support for thyrotoxicosis-induced cardiomyopathy. Proceedings 2022, 36, 211–212. [Google Scholar] [CrossRef]
- Newman, K.; Walthall, L. A Case of Thyroid Storm Caused by Thyroiditis. J. Investig. Med. High Impact Case Rep. 2022, 10, 23247096221129468. [Google Scholar] [CrossRef]
- Amin, T.; Austin, C.P.; Udongwo, N.; Wiseman, K.; Parhar, A.S.; Chaughtai, S. Iodinated Contrast-Induced Thyroid Storm with Concomitant Cardiac Tamponade: A Case Report. Cureus 2022, 14, e28001. [Google Scholar] [CrossRef] [PubMed]
- Patra, S.; Kaliyappan, A.; Kaushik, A.; Roy, A. Impending myocardial ischaemia during thyroid storm diagnosed through Wellens’ syndrome. BMJ Case Rep. 2022, 15, e250488. [Google Scholar] [CrossRef] [PubMed]
- Hamed, M.; Palumbo, S.; Mendha, T. Severe Cardiovascular Effects of Prolonged Untreated Hyperthyroidism Manifesting As Thyroid Storm. Cureus 2022, 14, e26289. [Google Scholar] [CrossRef]
- Austin, C.P.; Odak, M.; Douedi, S.; Patel, S.V. Supraventricular Tachycardia: An Atypical Presentation of Thyroid Storm. Cureus 2022, 14, e25449. [Google Scholar] [CrossRef] [PubMed]
- Iino, T.; Akatsuka, M.; Yamamoto, S. Case Report: Occurrence of Thyroid Storm in a Young Patient with Recurrent Diabetic Ketoacidosis. Front. Endocrinol. 2022, 13, 834505. [Google Scholar] [CrossRef] [PubMed]
- Nakao, T.; Takeshima, K.; Ariyasu, H.; Kurimoto, C.; Uraki, S.; Morita, S.; Furukawa, Y.; Iwakura, H.; Akamizu, T. Thyroid storm with delayed hyperbilirubinemia and severe heart failure: Indication and contraindication of plasma exchange. Endocrinol. Diabetes Metab. Case Rep. 2020, 2020, 20-0036. [Google Scholar] [CrossRef] [PubMed]
- Albehair, M.A.; Alagga, A.A.; Ghulam, W.Z.; Alomair, A.M.; AlFaraj, D. Thyroid Storm: Unusual Presentation and Complication. Cureus 2021, 13, e12483. [Google Scholar] [CrossRef] [PubMed]
- Takemoto, K.; Takada, S. Thyroid storm associated with type 2 amiodarone-induced thyrotoxicosis due to long-term administration: A case report. Acute Med. Surg. 2020, 7, e616. [Google Scholar] [CrossRef] [PubMed]
- Snyder, S.; Joseph, M. The Perfect Storm: A Case of Ischemic Stroke in the Setting of Thyroid Storm. Cureus 2020, 12, e7992. [Google Scholar] [CrossRef]
- Miller, A.; Silver, K.D. Thyroid Storm with Multiorgan Failure Treated with Plasmapheresis. Case Rep. Endocrinol. 2019, 2019, 2475843. [Google Scholar] [CrossRef] [PubMed]
- Kusuki, K.; Mizuno, Y. Hungry bone syndrome after thyroidectomy for thyroid storm. BMJ Case Rep. 2019, 12, e231411. [Google Scholar] [CrossRef]
- Tanaka, Y.; Uchida, T.; Yamaguchi, H.; Kudo, Y.; Yonekawa, T.; Nakazato, M. Fulminant hepatitis and elevated levels of sIL-2R in thyroid storm. Endocrinol. Diabetes Metab. Case Rep. 2019, 2019, 19-0078. [Google Scholar] [CrossRef] [PubMed]
- Wallington, D.; Schauer, M.; Bauler, L.D. Simultaneous presentation of thyroid storm and diabetic ketoacidosis in a previously healthy 21-year-old man. BMJ Case Rep. 2019, 12, bcr-2018-227554. [Google Scholar] [CrossRef]
- Andrade Luz, I.; Pereira, T.; Catorze, N. Thyroid storm: A case of haemodynamic failure promptly reversed by aggressive medical therapy with antithyroid agents and steroid pulse. BMJ Case Rep. 2018, 11, e226669. [Google Scholar] [CrossRef] [PubMed]
- Yonezaki, K.; Kobayashi, T.; Imachi, H.; Yoshimoto, T.; Kikuchi, F.; Fukunaga, K.; Sato, S.; Ibata, T.; Yamaji, N.; Lyu, J.; et al. Combination therapy of ipilimumab and nivolumab induced thyroid storm in a patient with Hashimoto’s disease and diabetes mellitus: A case report. J. Med. Case Rep. 2018, 12, 171. [Google Scholar] [CrossRef] [PubMed]
- Namatame, C.; Sonoo, T.; Fukushima, K.; Naraba, H.; Hashimoto, H.; Nakamura, K. A thyroid storm patient with protracted disturbance of consciousness and reversible lesion in the splenium of corpus callosum: A case report. Medicine 2018, 97, e9949. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Takaya, T.; Yoshida, N.; Ito, T.; Suto, M.; Hatani, Y.; Sano, H.; Ito, J.; Fukuoka, H.; Yamashita, T.; et al. A case of fatal heart and liver failure accompanied by thyroid storm treated with prompt plasma exchange. J. Cardiol. Cases 2017, 15, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Bossolo, A.; Gonzalez-Rivera, A.; Coste-Sibilia, S. Cerebrovascular Accident due to Thyroid Storm: Should We Anticoagulate? Case Rep. Endocrinol. 2016, 2016, 5218985. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, R.D.; Luke, W.A.; Sebastiampillai, B.S.; Gunathilake, M.P.; Premaratna, R. Thyrotoxic crisis presenting with jaundice. BMC Res. Notes 2016, 9, 320. [Google Scholar] [CrossRef] [PubMed]
- Korte, A.K.; Derde, L.; van Wijk, J.; Tjan, D.H. Sudden cardiac arrest as a presentation of Brugada syndrome unmasked by thyroid storm. BMJ Case Rep. 2015, 2015, bcr2015212351. [Google Scholar] [CrossRef]
- Soleimanpour, S.A. Fulminant liver failure associated with delayed identification of thyroid storm due to heterophile antibodies. Clin. Diabetes Endocrinol. 2015, 1, 12. [Google Scholar] [CrossRef]
- Kulaksizoglu, M.; Gonen, M.S.; Kebapcilar, L.; Sahin, F.; Acikgoz, B.; Demir, T.; Dincturk, E. Multiorgan dysfunction accompanied with metimazole and thyroid storm. Transfus. Apher. Sci. 2012, 46, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Natsuda, S.; Nakashima, Y.; Horie, I.; Ando, T.; Kawakami, A. Thyroid storm precipitated by duodenal ulcer perforation. Case Rep. Endocrinol. 2015, 2015, 750390. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.; Vandenberghe, H.; Thompson, M. Thyroid storm caused by a chinese herb contaminated with thyroid hormones. Am. J. Case Rep. 2015, 16, 57–59. [Google Scholar] [CrossRef] [PubMed]
- Mancano, M.A. Sorafenib-induced thyroid storm; ceftaroline-induced eosinophilic pneumonia; imatinib-induced osteonecrosis of the tibia; visual and auditory hallucinations with citalopram. Hosp. Pharm. 2014, 49, 121–126. [Google Scholar] [CrossRef]
- Min, T.; Benjamin, S.; Cozma, L. Thromboembolic complications of thyroid storm. Endocrinol. Diabetes Metab. Case Rep. 2014, 2014, 130060. [Google Scholar] [CrossRef]
- Kandil, E.; Khalek, M.A.; Thethi, T.; Abd Elmageed, Z.; Khan, A.; Jaffe, B.M. Thyroid storm in a patient with fulminant hepatic failure. Laryngoscope 2011, 121, 164–166. [Google Scholar] [CrossRef]
- Martinez-Diaz, G.J.; Formaker, C.; Hsia, R. Atrial fibrillation from thyroid storm. J. Emerg. Med. 2012, 42, e7–e9. [Google Scholar] [CrossRef]
- Cho, R.; Leclaire, M.; Kempainen, R. Heparin-induced hyperkalemia in a patient diagnosed with thyroid storm. Ann. Pharmacother. 2013, 47, 1213–1217. [Google Scholar] [CrossRef]
- Gong, P.H.; Dong, X.S.; Li, C.; Bao, J.; Cao, Z.L.; Yuan, Y.; Zheng, Y.L.; Gao, Z.C. Acute severe asthma with thyroid crisis and myasthenia: A case report and literature review. Clin. Respir. J. 2017, 11, 671–676. [Google Scholar] [CrossRef]
- Rohr, A.; Kovaleski, A.; Hill, J.; Johnson, P. Thyroid Embolization as an Adjunctive Therapy in a Patient with Thyroid Storm. J. Vasc. Interv. Radiol. 2016, 27, 449–451. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.I.; Yiang, G.T.; Hsu, C.W.; Wang, J.C.; Lee, C.H.; Chen, Y.L. Thyroid Storm in a Patient with Trauma—A Challenging Diagnosis for the Emergency Physician: Case Report and Literature Review. J. Emerg. Med. 2017, 52, 292–298. [Google Scholar] [CrossRef]
- Wyble, A.J.; Moore, S.C.; Yates, S.G. Weathering the storm: A case of thyroid storm refractory to conventional treatment benefiting from therapeutic plasma exchange. J. Clin. Apher. 2018, 33, 678–681. [Google Scholar] [CrossRef] [PubMed]
- Niles, D.; Boguniewicz, J.; Shakeel, O.; Margolin, J.; Chelius, D.; Gupta, M.; Paul, D.; King, K.Y.; McNeil, J.C. Candida tropicalis Thyroiditis Presenting with Thyroid Storm in a Pediatric Patient with Acute Lymphocytic Leukemia. Pediatr. Infect. Dis. J. 2019, 38, 1051–1053. [Google Scholar] [CrossRef]
- Ricciardo, S.; Hastings, S. Fatal Thyroid Storm in the Setting of Untreated Graves Disease and Use of the Synthetic Cannabinoid MDMB-4en-PINACA. Am. J. Forensic Med. Pathol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Tokushima, Y.; Sakanishi, Y.; Nagae, K.; Tokushima, M.; Tago, M.; Tomonaga, M.; Yoshioka, T.; Hyakutake, M.; Sugioka, T.; Yamashita, S. Thyroid storm complicated by bicytopenia and disseminated intravascular coagulation. Am. J. Case Rep. 2014, 15, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Waqar, Z.; Avula, S.; Shah, J.; Ali, S.S. Cardiovascular Events in Patients with Thyroid Storm. J. Endocr. Soc. 2021, 5, bvab040. [Google Scholar] [CrossRef] [PubMed]
- Bourcier, S.; Coutrot, M.; Kimmoun, A.; Sonneville, R.; de Montmollin, E.; Persichini, R.; Schnell, D.; Charpentier, J.; Aubron, C.; Morawiec, E.; et al. Thyroid storm in the ICU: A retrospective multicenter study. Crit. Care Med. 2020, 48, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Idowu, A.O.; Adesegun, O.A.; Osibowale, B.; Ajiro, T.; Ezuduemoih, D.; Osonuga, A. A case of thyroxine (T4) toxicosis complicated by thyroid storm with an unusual precipitant. Casp. J. Intern. Med. 2020, 11, 231–234. [Google Scholar]
- Martino, E.; Bartalena, L.; BogazziI, F.; Braveman, L.E. The Effects of Amiodarone on the Thyroid. Endocr. Soc. 2001, 22, 240–254. [Google Scholar]
- Razvi, S.; Jabbar, A.; Pingitore, A.; Danzi, S.; Biondi, B.; Klein, I.; Peeters, R.P.; Zaman, A.; Iervasi, G. Thyroid Hormones and Cardiovascular Function and Diseases. J. Am. Coll. Cardiol. 2018, 71, 1781–1796. [Google Scholar] [CrossRef]
- Albakri, A. Thyrotoxic heart failure: A review of clinical status and meta-analysis of electrocardiogram diagnosis and medical clinical management methods. Integr. Mol. Med. 2018, 5, 2–11. [Google Scholar] [CrossRef]
- Satoh, T.; Isozaki, O.; Suzuki, A.; Wakino, S.; Iburi, T.; Tsuboi, K.; Kanamoto, N.; Otani, H.; Furukawa, Y.; Teramukai, S.; et al. 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr. J. 2016, 63, 1025–1064. [Google Scholar] [CrossRef] [PubMed]
- Osuna, P.M.; Udovcic, M.; Sharma, M. DHyperthyroidism and the Heart. Methodist DeBakey Cardiovasc. J. 2017, 13, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Chaker, L.; van den Berg, M.E.; Niemeijer, M.N.; Franco, O.H.; Dehghan, A.; Hofman, A.; Rijnbeek, P.R.; Deckers, J.W.; Eijgelsheim, M.; Stricker, B.H.; et al. Thyroid Function and Sudden Cardiac Death: A Prospective Population-Based Cohort Study. Circulation 2016, 134, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Lencu, C.; Alexescu, T.; Petrulea, M.; Lencu, M. Respiratory manifestations in endocrine diseases. Clujul Med. 2016, 89, 459–463. [Google Scholar] [CrossRef]
- Klomp, M.; Siegelaar, S.E.; van de Hoef, T.P.; Beijk, M.A.M. A case report of myocardial infarction with non-obstructive coronary artery disease: Graves’ disease-induced coronary artery vasospasm. Eur. Heart J. Case Rep. 2020, 4, 1–5. [Google Scholar] [CrossRef]
- El-Menyar, A.A. Drug-induced myocardial infarction secondary to coronary artery spasm in teenagers and young adults. J. Postgrad. Med. 2006, 52, 51–56. [Google Scholar] [PubMed]
- Zheng, W.; Zhang, Y.J.; Li, S.Y.; Liu, L.-L.; Sun, J. Painless thyroiditis-induced acute myocardial infarction with normal coronary arteries. Am. J. Emerg. Med. 2015, 33, 983. [Google Scholar] [CrossRef]
- Hammond, H.K.; White, F.C.; Buxton, I.L.; Saltzstein, P.; Brunton, L.L.; Longhurst, J.C. Increased myocardial beta-receptors and adrenergic responses in hyperthyroid pigs. Am. J. Physiol. 1987, 252, H283–H290. [Google Scholar] [CrossRef] [PubMed]
- Lassnig, E.; Berent, R.; Auer, J.; Eber, B. Cardiogenic shock due to myocardial infarction caused by coronary vasospasm associated with hyperthyroidism. Int. J. Cardiol. 2003, 90, 333–335. [Google Scholar] [CrossRef]
- Dahl, P.; Danzi, S.; Klein, I. Thyrotoxic cardiac disease. Curr. Heart Fail. Rep. 2008, 5, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Chariyawong, P.; Rao, A.; Panikkath, D.; Panikkath, R. Hyperthyroidism-induced dilated cardiomyopathy. Southwest Respir. Crit. Care Chron. 2019, 7, 64–66. [Google Scholar] [CrossRef]
- Ozturk, T.C.; Unluer, E.; Denizbasi, A.; Guneysel, O.; Onur, O. Can NT-proBNP be used as a criterion for heart failure hospitalization in emergency room? J. Res. Med. Sci. 2011, 16, 1564–1571. [Google Scholar]
- Bui, P.V.; Zaveri, S.N.; Pierce, J.R. Sanguinous pericardial effusion and cardiac tamponade in the setting of Graves’ disease: Report of a case and review of previously reported cases. Case Rep. Med. 2016, 2016, 9653412. [Google Scholar] [CrossRef]
- Mohananey, D.; Smilowitz, N.; Villablanca, P.A.; Bhatia, N.; Agrawal, S.; Baruah, A.; Ali, M.S.; Bangalore, S.; Ramakrishna, H. Trends in the Incidence and In-Hospital Outcomes of Cardiogenic Shock Complicating Thyroid Storm. Am. J. Med. Sci. 2017, 354, 159–164. [Google Scholar] [CrossRef]
- Lin, H.C.; Yang, L.Y.; Kang, J.H. Increased risk of pulmonary embolism among patients with hyperthyroidism: A 5-year follow-up study. J. Thromb. Haemost. 2010, 8, 2176–2181. [Google Scholar] [CrossRef]
- Suwa, M.; Seino, Y.; Nomachi, Y.; Matsuki, S.; Funahashi, K. Multicenter prospective investigation on efficacy and safety of carperitide for acute heart failure in the ‘real world’ of therapy. Circ J. 2005, 69, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Dyer, M.; Neal, M.D.; Rollins-Raval, M.A.; Raval, J.S. Simultaneous Extracorporeal membrane oxygenation and therapeutic plasma exchange procedures are tolerable in both pediatric and adult patients. Transfusion 2014, 54, 1158–1165. [Google Scholar] [CrossRef]
- Gajkowski, E.F.; Herrera, G.; Hatton, L.; Velia Antonini, M.; Vercaemst, L.; Cooley, E. ELSO Guidelines for Adult and Pediatric Extracorporeal Membrane Oxygenation Circuits. ASAIO J. 2022, 68, 133–152. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Perrin, P.; Faller, B.; Richter, S.; Chantrel, F. Role of plasma exchange in the thyroid storm. Ther. Apher. Dial. 2011, 15, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Tandukar, S.; Palevsky, P.M. Continuous Renal Replacement Therapy: Who, When, Why, and How. Chest 2019, 155, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.M.; Siddiqui, A.H. Intra-Aortic Balloon Pump. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Glazier, J.J.; Kaki, A. The Impella Device: Historical Background, Clinical Applications and Future Directions. Int. J. Angiol. 2019, 28, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Biello, A.; Kinberg, E.C.; Wirtz, E.D. Thyroidectomy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Klubo-Gwiezdzinska, J.; Wartofsky, L. Thyroid emergencies. Med. Clin. N. Am. 2012, 96, 385–403. [Google Scholar] [CrossRef] [PubMed]
- Elseviers, M.M.; Lins, R.L.; Van der Niepen, P.; Hoste, E.; Malbrain, M.L.; Damas, P.; Devriendt, J.; SHARF investigators. Renal replacement therapy is an independent risk factor for mortality in critically ill patients with acute kidney injury. Crit. Care. 2010, 14, R221. [Google Scholar] [CrossRef]
- The Difference between a Systematic Review & Scoping Review. Available online: https://www.covidence.org/blog/the-difference-between-a-systematic-review-and-a-scoping-review/ (accessed on 15 September 2023).



| Variable | Overall (n = 256) | Female (n = 154) 60% | Male (n = 102) 40% | p Value |
|---|---|---|---|---|
| Age; median and IQR | 42.5 (31–58) | 43 (31–52) | 42 (29–53) | 0.77 |
| BWS point; median and IQR | 60 (50–75) | 60 (50–75) | 60 (45–75) | 0.67 |
| Non-compliant to treatment | 80/252 (32%) | 31% | 33% | 0.56 |
| High serum natriuretic peptide level | 56/256 (22%) | 26% | 16% | 0.05 |
| Positive cardiac troponin | 19/250 (7.6%) | 12% | 7% | 0.48 |
| Acute myocardial infarction | 25/250 (10%) | 8% | 7% | 0.48 |
| Presented with cardiac arrest | 14/246 (5.7%) | 7.5% | 3.0% | 0.13 |
| Initial LVEF%; median and IQR | 25 (19–40) | 30 (20–43) | 23 (15–32) | 0.05 |
| Follow-up LVEF% | 50 (36–58) | 51 (43–59) | 48 (35–57) | 0.17 |
| Acute heart failure (any grade) * | 112/239 (47%) | 41% | 46.5% | 0.02 |
| Dilated cardiomyopathy | 31/249 (12.4%) | 11% | 23% | 0.01 |
| Heart failure with preserved EF | 5/233 (2.1%) | 2.2% | 2.0% | 0.91 |
| Pulmonary edema | 49/236 (21%) | 26% | 13% | 0.01 |
| Takotsubo cardiomyopathy | 11/234 (4.7%) | 7.1% | 1.1% | 0.03 |
| Pericardial effusion | 7/254 (2.8%) | 2.6% | 3.0% | 0.88 |
| Cardiogenic shock | 78/242 (32%) | 28% | 38% | 0.27 |
| Cardiac arrest | 61/238 (25.6%) | 23% | 29% | 0.23 |
| Pulseless electrical activity | 9/243 (3.7%) | 2.7% | 5.2% | 0.33 |
| Asystole | 1/238 (0.4%) | 0.7% | 0.0% | 0.42 |
| Ventricular fibrillation | 12/244 (4.9%) | 4.1% | 6.2% | 0.48 |
| Ventricular tachycardia | 6/245 (2.4%) | 2.7% | 2.0% | 0.72 |
| Beta-blocker-induced collapse | 63/244 (25.8%) | 25% | 27% | 0.66 |
| Atrial fibrillation | 123/249 (49%) | 44% | 58% | 0.02 |
| Atrial flutter | 16/245 (6.5%) | 5.4% | 8.2% | 0.39 |
| Sinus tachycardia | 69/246 (28%) | 35% | 17% | 0.002 |
| Multifocal atrial tachycardia | 3/245 (1.2%) | 1.4% | 1.0% | 0.80 |
| Supraventricular tachycardia | 14/246 (5.7%) | 7.5% | 3.0% | 0.13 |
| Multiorgan failure | 120/250 (48%) | 47.4% | 49% | 0.80 |
| Respiratory failure | 39/227 (17.2%) | 15.9% | 19.1% | 0.54 |
| Renal failure | 47/227 (20.7%) | 37%% | 49% | 0.06 |
| Liver failure | 95/229 (41.5%) | 47% | 53% | 0.03 |
| Heart failure/cardiomyopathy | 161/229 (70%) | 74% | 65% | 0.14 |
| Mortality | 34/255 (13.5%) | 11.8% | 16.2% | 0.33 |
| Variable | Overall (n = 256) | Female (n = 154) | Male (n = 102) | p Value |
|---|---|---|---|---|
| Pharmacological treatment | ||||
| Amiodarone | 19/235 (8.1%) | 8.8% | 6.5% | 0.34 |
| Inotropes/vasopressor | 81/241 (33.6%) | 28.6% | 41.5% | 0.08 |
| Digoxin | 25/241 (10.4%) | 9.7% | 11.5% | 0.65 |
| Steroids | 172/247 (70%) | 65.5% | 75.8% | 0.05 |
| Calcium channel blockers | 30/238 (12.6%) | 11.8% | 13.8% | 0.64 |
| Beta blockers | 191/232 (82%) | 60% | 40% | 0.84 |
| Anti-thyroid drugs | 228/251 (91%) | 90% | 92% | 0.57 |
| Ivabradine | 2/253 (0.8%) | 0.7% | 1.0% | 0.877 |
| Non-pharmacological treatment | ||||
| CRRT/CVVHD/dialysis | 34/245 (13.8%) | 16% | 8.6% | 0.12 |
| Implantable cardioverter-defibrillator | 5/244 (2%) | 0.7% | 4.2% | 0.05 |
| VA-ECMO | 40/246 (16.3%) | 13.3% | 21% | 0.12 |
| Left ventricular assist device | 3/245 (1.2%) | 0.7% | 2.2% | 0.31 |
| Impella device | 5/245 (2%) | 1.3% | 3.2% | 0.32 |
| Intra-aortic balloon pump | 23/246 (9.3%) | 8.0% | 12.5% | 0.29 |
| Therapeutic plasma exchange (TPE) | 40/246 (16.3%) | 13.9% | 20.1% | 0.21 |
| Radioactive Iodine ablation | 8/245 (3.3%) | 4.0% | 2.1% | 0.42 |
| Thyroidectomy | 46/247 (18.6%) | 17.2% | 21% | 0.47 |
| Variable | Alive (n = 217) 86.86% | Dead (n = 34) 13.5% | p Value |
|---|---|---|---|
| Age, median and IQR | 42 (30–53) | 43 (32–49) | 0.91 |
| BWS points median and IQR | 60 (50–75) | 65 (55–75) | 0.78 |
| Initial ejection fraction % median and IQR | 27 (20–40) | 20 (15–37) | 0.37 |
| Female gender | 62% | 53% | 0.43 |
| Male gender | 38% | 47% | 0.43 |
| Graves’ disease | 29% | 21% | 0.41 |
| Not known to have thyroid disease before admission | 6.5% | 12% | 0.45 |
| Non-compliant to ATD before admission | 31% | 37.5% | 0.72 |
| Atrial fibrillation after admission | 52% | 33.3% | 0.06 |
| Beta blocker (BB) use | 82% | 87% | 0.49 |
| Shock after admission | 42% | 55% | 0.19 |
| Pulmonary edema on admission | 21% | 17% | 0.56 |
| Takotsubo cardiomyopathy | 4.0% | 7.0% | 0.50 |
| Acute myocardial infarction | 7.1% | 9.1% | 0.46 |
| Acute liver failure | 40% | 56% | 0.12 |
| Acute renal failure | 18.4% | 41% | 0.008 |
| Ventricular fibrillation | 3.8% | 13.3% | 0.02 |
| Ventricular tachycardia | 2.4% | 3.3% | 0.78 |
| BB-induced circulatory collapse | 21.3% | 57.6% | 0.001 |
| Mechanical therapy (any) | 47% | 57% | 0.30 |
| ECMO | 15% | 28% | 0.056 |
| CRRT | 5.0% | 26% | 0.001 |
| Thyroidectomy | 21% | 6.5% | 0.05 |
| Therapeutic plasma exchange | 15% | 26% | 0.14 |
| Measures of Treatment | Strength of Recommendation | Quality of Evidence |
|---|---|---|
| Antithyroid drugs (ATDs) | High | Low |
| Inorganic iodide | High | Moderate |
| Corticosteroids | High | Moderate |
| Cooling with acetaminophen and mechanical cooling | High | Low |
| Therapeutic plasmapheresis | Weak | Low |
| Central nervous system manifestations treatment | Strong | Low |
| Tachycardia treatment | High | Low |
| Atrial fibrillation treatment | High | Low |
| Acute congestive heart failure | High | Low |
| Treatment Modalities | N of Cases | Doses | Mechanism of Action/Indications | Side Effects and Contraindications |
|---|---|---|---|---|
| Anti-thyroid drugs (ATD) Carbimazole (CBZ) Methimazole (MMI) Propylthiouracil (PTU) | 228 | - MMI and CBZ oral 20–30 mg/day every 6–4 h. - PTU: 200 mg every 4 h. | First line of treatment to control TS.
| Agranulocytosis.
Rash. Thrombocytopenia (CBZ may be switched to PTU). Antineutrophilic cytoplasmic antibody vasculitis (PTU). Antithyroid arthritis syndrome (CBZ/MMI). |
| Inorganic iodide Saturated solution of Potassium iodide (SSKI) Lugol iodine | 111 | SKKI: 200 mg/day. Lugol Iodine: 5–10 drops orally once in 6–8 h. | Wolff–Chaikoff effect
- Decreases blood flow to thyroid gland and so can be given prior to thyroidectomy. | Hyperkalemia (potassium iodide). Due to the transient action:
|
| Cholestyramine | 33 | A total of 4 g oral intake 2–4 times a day. | - Elimination of thyroid hormone in enterohepatic circulation by binding to iodothyronines. - Indications:
| |
| Corticosteroids Hydrocortisone/Dexamethasone prednisone | 172 | -IV/IM hydrocortisone: 150. mg/day every 6 h. -IV dexamethasone; 2 mg every 6 h. | - When given in high doses, it inhibits thyroid hormone release, T4 and T3 conversion inhibition, and prevents adrenal insufficiency related to the hypermetabolic state of TS. - Increases vasomotor stability. - Given until TS resolves. | |
| Beta Blockers Propranolol (NCBB) Metoprolol Esmolol (SC) Bisoprolol Landiolol (USC) Sotalol | 191 | -Propranolol: 1. oral or NGT 60–80 mg, 2. IV: 0.5–1 mg over 10 min followed by 1–2 mg over 10 every few hours. -Short-acting (Esmolol): a loading dose of 250–500 mcg/kg, followed by 50–100 mcg/kg infusion. |
| Cardiogenic shock
Circulatory collapse. Hypotension. Refractory hypotension - Bronchoconstriction with bisoprolol. |
| Calcium channel blockers Verapamil Diltiazem | 30 | IV diltiazem push: 20 mg. | - Inhibit Ca2+ into excitable cells, resulting in smooth muscle dilation. - Negative inotropes in cardiac cells. - Indications:
- Was given for AF prior to TS diagnosis then discontinued when diagnosis made. | - Cardiogenic shock. - Asystole. |
| Digoxin | 25 | IV: 0.125–0.25 mg. | Increases cardiac contractility as it binds and inhibits the Na/K-ATPase pump within cardiac myocytes. Positive inotropic effect:
| Avoid in case of renal dysfunction as it increases renal clearance. - Worsening hypotension. |
| Inotropes (Vasopressors) Dopamine Dobutamine Epinephrine Levosimendan Noraderanline Milrinone | 81 | Dobutamine: infusion 2 (ug/kg/min) Noradrenaline. | Dobutamine/dopamine: Inotrope with high affinity to B1 adrenergic receptors.
Milrinone:
|
|
| Amiodarone | 19 | IV: 125 mg over 10 min followed by a 0.8 mg infusion for 6 h. | - An iodine-rich class III antiarrhythmic - Blocks 5′mono-deiodination of t4 in peripheral tissues as the liver and pituitary gland.
- Most common antiarrhythmic in ICU due to stable properties.
| - Hyperthyroid activity and thyrotoxic precipitant (Jod- Basedow phenomenon). - Amiodarone-induced thyrotoxicosis. - Hepatotoxicity; worsened ischemic hepatic failure. - Worsening hypotension |
| Mechanical Modality | Cases | Mechanism of Action/Indications | Side Effects and Contraindications |
|---|---|---|---|
| Extracorporeal membrane oxygenation (ECMO) | 40 |
|
-Thromboembolism. -Strokes.
-Arterial dissection -Distal ischemia |
| Therapeutic plasma exchange (TPE) | 40 |
|
|
| Continuous renal replacement therapy (CRRT) | 25 |
|
|
| Continuous ven o-venous hemodialysis (CVVHD) | 10 |
|
|
| Biventricular Impella Device | 5 |
Increases cardiac output in cases of biventricular failure.
|
Long-term use causes:
|
| Left ventricular Assist Device (LVAD) | 3 |
|
|
| Intra-Aortic balloon pump (IABP) | 23 |
|
|
| Thyroidectomy | 46 |
| |
| Radioactive iodine ablation/therapy (RAI) | 8 |
|
-Recurrent laryngeal nerve damage.
|
| Extracorporeal albumin dialysis (continuous and Single-pass albumin dialysis (SPAD) | 1 |
-Hepatorenal syndrome.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elmenyar, E.; Aoun, S.; Al Saadi, Z.; Barkumi, A.; Cander, B.; Al-Thani, H.; El-Menyar, A. Data Analysis and Systematic Scoping Review on the Pathogenesis and Modalities of Treatment of Thyroid Storm Complicated with Myocardial Involvement and Shock. Diagnostics 2023, 13, 3028. https://doi.org/10.3390/diagnostics13193028
Elmenyar E, Aoun S, Al Saadi Z, Barkumi A, Cander B, Al-Thani H, El-Menyar A. Data Analysis and Systematic Scoping Review on the Pathogenesis and Modalities of Treatment of Thyroid Storm Complicated with Myocardial Involvement and Shock. Diagnostics. 2023; 13(19):3028. https://doi.org/10.3390/diagnostics13193028
Chicago/Turabian StyleElmenyar, Eman, Sarah Aoun, Zain Al Saadi, Ahmed Barkumi, Basar Cander, Hassan Al-Thani, and Ayman El-Menyar. 2023. "Data Analysis and Systematic Scoping Review on the Pathogenesis and Modalities of Treatment of Thyroid Storm Complicated with Myocardial Involvement and Shock" Diagnostics 13, no. 19: 3028. https://doi.org/10.3390/diagnostics13193028
APA StyleElmenyar, E., Aoun, S., Al Saadi, Z., Barkumi, A., Cander, B., Al-Thani, H., & El-Menyar, A. (2023). Data Analysis and Systematic Scoping Review on the Pathogenesis and Modalities of Treatment of Thyroid Storm Complicated with Myocardial Involvement and Shock. Diagnostics, 13(19), 3028. https://doi.org/10.3390/diagnostics13193028






