Update on Myocarditis: From Etiology and Clinical Picture to Modern Diagnostics and Methods of Treatment
Abstract
:1. Introduction
2. Materials and Methods
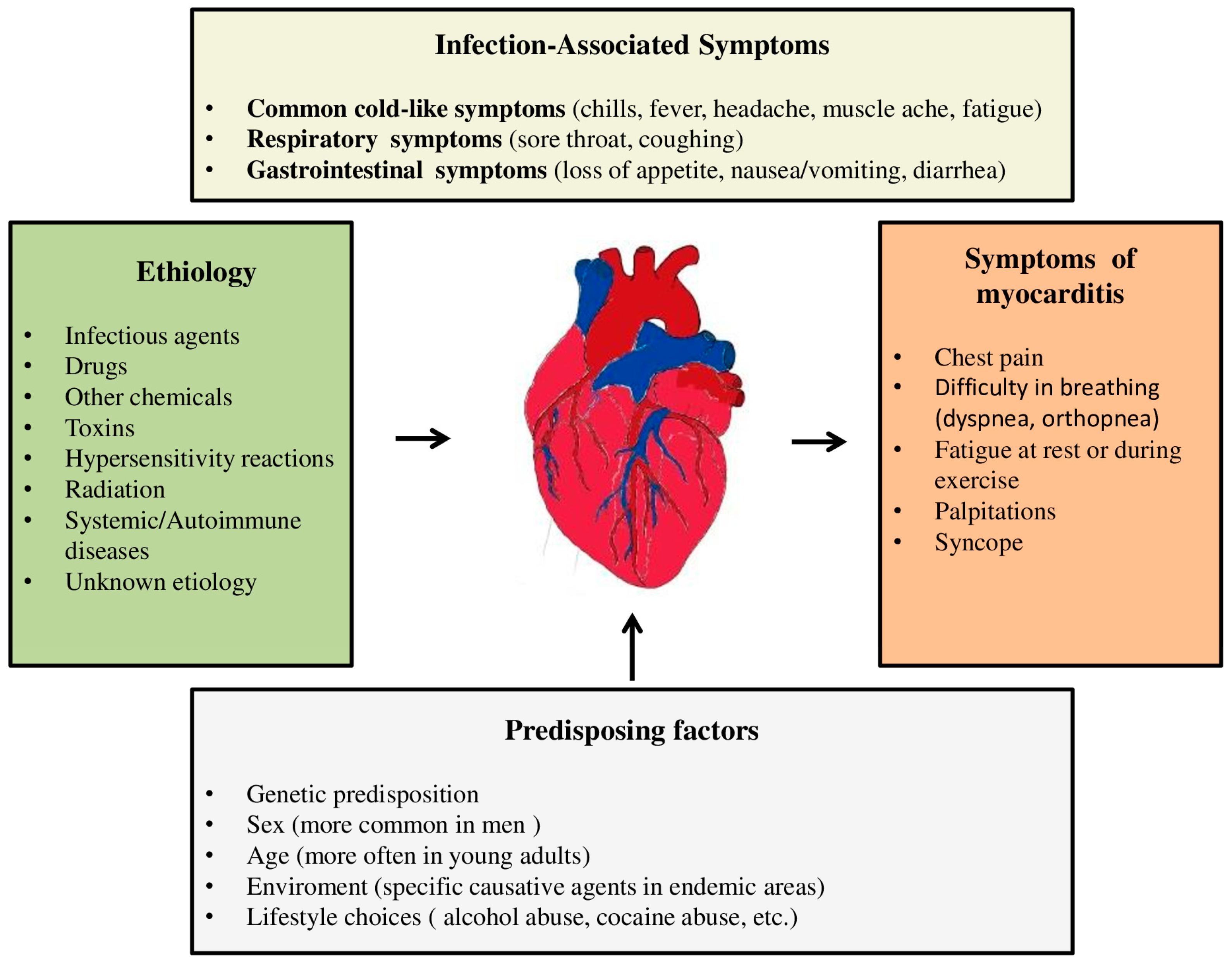
3. Etiological Factors and Pathophysiological Mechanisms of Myocarditis
3.1. Infectious Causes of Myocarditis
- (1)
- Direct cytotoxic effect (Murine model: virus penetration into myocytes, their binding to a specific receptor, virus replication, and consequent necrosis of myocites), binding to intracellular agents (myosin), and activation of the immune system characterized by the invasion of natural killer cells and macrophages accompanied by T lymphocytes.
- (2)
- Secondary phase (autoimmune reaction).
3.2. Eosinophilic Myocarditis
3.3. Giant Cell Myocarditis
3.4. Myocarditis Associated with Immune Checkpoint Inhibitors
3.5. Myocarditis Associated with Systemic Diseases
4. Division of Myocarditis
4.1. Acute Myocarditis
4.2. Subacute Myocarditis
4.3. Chronic Myocarditis
4.4. Chronic Inflammatory Cardiomyopathy
5. Clinical Picture
- Acute (non-fulminant) myocarditis—about 65% of patients have this form of myocarditis [84]. This phenotype includes asymptomatic cases and cases in which some degree of cardiac damage may occur with partial or complete regression [36]. These patients have a clinical, electrocardiographic picture and biohumoral syndrome similar to acute myocardial infarction (AMI). In rare cases, death occurs [85].
- Fulminant myocarditis (FM)—accounts for 8.6% of all patients with myocarditis [86]. It is characterized by an acute onset of the disease, which is characterized by rapid deterioration and usually death [36]. Usually, patients present with symptoms and signs of HF (up to pulmonary edema) and not infrequently up to cardiogenic shock, and the clinical course is accompanied by malignant arrhythmias. In these patients, inotropic stimulation or mechanical circulatory support is usually required [46,87]. Patients with FM compared to patients with a non-fulminant form of this disease have a higher early mortality ((28.0% vs. 1.8%, p = 0.0001) and late mortality during seven years of follow-up (47.7% vs. 10.4%, p < 0.0001) [85]. Earlier studies that monitored the prognosis of patients with FM showed conflicting results regarding the long-term prognosis [88,89,90]. Ammirati E. et al. also showed a correlation between the histological subtype of FM and patient prognosis. Giant cell FM is associated with a significantly worse patient prognosis compared to eosinophilic and lymphocytic subtypes of myocarditis [85].
- Chronic persistent myocarditis (7% of cases)—it is characterized by a mild onset of the disease, usually without cardiac decompensation [36].
5.1. Symptoms Related to the Previous Infectious Agent
5.2. Chest Pain
5.3. Symptoms and Signs of Heart Failure
5.4. Arrhythmias
5.5. Syncope
5.6. Myocarditis in Children
6. Diagnosis of Myocarditis
6.1. ECG in Myocarditis
6.2. Biomarkers
- a.
- Markers of inflammation: high-sensitivity C-reactive protein (hs-CRP), elevated leukocyte count, and accelerated sedimentation.
- b.
- Markers of myocardial damage
- c.
- Dysfunction markers
- d.
- Anti-cardiac antibodies
- e.
- Micro RNA
- f.
- Viral antibodies
6.3. Echocardiography
6.4. Cardiac Magnetic Resonance (CMR)
6.5. FDG–PET Scan
6.6. Endomyocardial Biopsy (EMB)
7. Differential Diagnosis
8. Treatment
- (A)
- Classical treatment
- (B)
- Immunomodulatory therapy
- (C)
- Immunosuppressive therapy
9. Prognosis
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ammirati, E.; Frigerio, M.; Adler, E.D.; Basso, C.; Birnie, D.H.; Brambatti, M.; Friedrich, M.G.; Klingel, K.; Lehtonen, J.; Moslehi, J.J.; et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ. Heart Fail. 2020, 13, e007405. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, Y.; Tase, C. Acute Myocarditis in Emergency Medicine. J. Am. Coll. Cardiol. 2012, 59, 779–792. [Google Scholar]
- Golpour, A.; Patriki, D.; Hanson, P.J.; McManus, B.; Heidecker, B. Epidemiological Impact of Myocarditis. J. Clin. Med. 2021, 10, 603. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Kontogeorgos, S.; Thunström, E.; Zverkova, S.T.; Kroon, C.; Bollano, E.; Schaufelberger, M.; Rosengren, A. Trends in myocarditis incidence, complications and mortality in Sweden from 2000 to 2014. Sci. Rep. 2022, 12, 1810. [Google Scholar] [CrossRef]
- Basso, C.; Calabrese, F.; Corrado, D.; Thiene, G. Postmortem diagnosis in sudden cardiac death victims: Macroscopic, microscopic and molecular findings. Cardiovasc. Res. 2001, 50, 290–300. [Google Scholar] [CrossRef]
- Maron, B.J.; Doerer, J.J.; Haas, T.S.; Tierney, D.M.; Mueller, F.O. Sudden deaths in young competitive athletes: Analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009, 119, 1085–1092. [Google Scholar] [CrossRef]
- Jouriles, N.J. Chapter 80. In Rosen’s Emergency Medicine: Concepts and Clinical Practice, 7th ed.; Marx, J.A., Hockberger, R.S., Walls, R.M., Eds.; Mosby: Philadelphia, PA, USA, 2009; pp. 1064–1068. [Google Scholar]
- Maron, B.J.; Towbin, J.A.; Thiene, G.; Antzelevitch, C.; Corrado, D.; Arnett, D.; Moss, A.J.; Seidman, C.E.; Young, J.B.; American Heart Association; et al. Contemporary definitions and classification of the cardiomyopathies: An American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006, 113, 1807–1816. [Google Scholar]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef]
- Altay, S. COVID-19 myocarditis cardiac magnetic resonance findings in symptomatic patients. Acta Radiol. 2022, 63, 1475–1480. [Google Scholar] [CrossRef]
- Voleti, N.; Reddy, S.P.; Ssentongo, P. Myocarditis in SARS-CoV-2 infection vs. COVID-19 vaccination: A systematic review and meta-analysis. Front. Cardiovasc. Med. 2022, 9, 951314. [Google Scholar] [CrossRef]
- Fairweather, D.; Beetler, D.J.; Musigk, N.; Heidecker, B.; Lyle, M.A.; Cooper, L.T., Jr.; Bruno, K.A. Sex and gender differences in myocarditis and dilated cardiomyopathy: An update. Front. Cardiovasc. Med. 2023, 10, 1129348. [Google Scholar] [CrossRef] [PubMed]
- Kytö, V.; Sipilä, J.; Rautava, P. The effects of gender and age on occurrence of clinically suspected myocarditis in adulthood. Heart 2013, 99, 1681–1684. [Google Scholar] [CrossRef] [PubMed]
- Laufer-Perl, M.; Havakuk, O.; Shacham, Y.; Steinvil, A.; Letourneau-Shesaf, S.; Chorin, E.; Keren, G.; Arbel, Y. Sex-based differences in prevalence and clinical presentation among pericarditis and myopericarditis patients. Am. J. Emerg. Med. 2017, 35, 201–205. [Google Scholar] [CrossRef]
- Lynge, T.H.; Nielsen, T.S.; Gregers Winkel, B.; Tfelt-Hansen, J.; Banner, J. Sudden cardiac death caused by myocarditis in persons aged 1–49 years: A nationwide study of 14 294 deaths in Denmark. Forensic Sci. Res. 2019, 4, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Durani, Y.; Egan, M.; Baffa, J.; Selbst, S.M.; Nagar, A.L. Pediatric myocarditis: Presenting clinical characteristics. Am. J. Emerg. Med. 2009, 27, 942–947. [Google Scholar] [CrossRef]
- Arola, A.; Pikkarainen, E.; Sipilä, J.O.; Pykäri, J.; Rautava, P.; Kytö, V. Occurrence and Features of Childhood Myocarditis: A Nationwide Study in Finland. J. Am. Heart Assoc. 2017, 6, e005306. [Google Scholar] [CrossRef] [PubMed]
- Tschöpe, C.; Ammirati, E.; Bozkurt, B.; Caforio, A.L.P.; Cooper, L.T.; Felix, S.B.; Hare, J.M.; Heidecker, B.; Heymans, S.; Hübner, N.; et al. Myocarditis and inflammatory cardiomyopathy: Current evidence and future directions. Nat. Rev. Cardiol. 2021, 18, 169–193. [Google Scholar] [CrossRef]
- Lévêque, N.; Garcia, M.; Bouin, A.; Nguyen, J.H.C.; Tran, G.P.; Andreoletti, L.; Semler, B.L. Functional Consequences of RNA 5′-Terminal Deletions on Coxsackievirus B3 RNA Replication and Ribonucleoprotein Complex Formation. J. Virol. 2017, 91, e00423-17. [Google Scholar] [CrossRef]
- Strabelli, T.M.; Siciliano, R.F.; Vidal Campos, S.; Bianchi Castelli, J.; Bacal, F.; Bocchi, E.A.; Uip, D.E. Toxoplasma gondii Myocarditis after Adult Heart Transplantation: Successful Prophylaxis with Pyrimethamine. J. Trop. Med. 2012, 2012, 853562. [Google Scholar] [CrossRef]
- Mylvaganam, R.; Glaser, A.; Moss, N.; Rana, M. A case of late-onset cytomegalovirus myocarditis in an orthotopic heart transplant recipient; case report and review of the literature. Diagn. Microbiol. Infect. Dis. 2018, 91, 153–155. [Google Scholar] [CrossRef]
- Massilamany, C.; Huber, S.A.; Cunningham, M.W.; Reddy, J. Relevance of molecular mimicry in the mediation of infectious myocarditis. J. Cardiovasc. Transl. Res. 2014, 7, 165–171. [Google Scholar] [CrossRef]
- Pannucci, P.; Jefferson, S.R.; Hampshire, J.; Cooper, S.L.; Hill, S.J.; Woolard, J. COVID-19-Induced Myocarditis: Pathophysiological Roles of ACE2 and Toll-like Receptors. Int. J. Mol. Sci. 2023, 24, 5374. [Google Scholar] [CrossRef]
- Lasica, R.; Djukanovic, L.; Mrdovic, I.; Savic, L.; Ristic, A.; Zdravkovic, M.; Simic, D.; Krljanac, G.; Popovic, D.; Simeunovic, D.; et al. Acute Coronary Syndrome in the COVID-19 Era-Differences and Dilemmas Compared to the Pre-COVID-19 Era. J. Clin. Med. 2022, 11, 3024. [Google Scholar] [CrossRef]
- Dennert, R.; Crijns, H.J.; Heymans, S. Acute viral myocarditis. Eur. Heart J. 2008, 29, 2073–2082. [Google Scholar] [CrossRef]
- Andréoletti, L.; Lévêque, N.; Boulagnon, C.; Brasselet, C.; Fornes, P. Viral causes of human myocarditis. Arch. Cardiovasc. Dis. 2009, 102, 559–568. [Google Scholar] [CrossRef]
- Seitz, A.; Martínez Pereyra, V.; Hubert, A.; Klingel, K.; Bekeredjian, R.; Sechtem, U.; Ong, P. Epicardial and microvascular coronary artery spasm in biopsy-proven viral myocarditis. Int. J. Cardiol. 2022, 360, 1–4. [Google Scholar] [CrossRef]
- Keramari, S.; Poutoglidis, A.; Chatzis, S.; Keramaris, M.; Savopoulos, C.; Kaiafa, G. Parvovirus B19-Associated Myocarditis: A Literature Review of Pediatric Cases. Cureus 2022, 14, e21726. [Google Scholar] [CrossRef]
- Schultheiss, H.P.; Baumeier, C.; Aleshcheva, G.; Bock, C.T.; Escher, F. Viral Myocarditis-From Pathophysiology to Treatment. J. Clin. Med. 2021, 10, 5240. [Google Scholar] [CrossRef]
- Lee, D.W.; Gardner, R.; Porter, D.L.; Louis, C.U.; Ahmed, N.; Jensen, M.; Grupp, S.A.; Mackall, C.L. Current concepts in the diagnosis and management of cytokine release syndrome. Blood 2014, 124, 188–195. [Google Scholar] [CrossRef]
- Shalabi, H.; Sachdev, V.; Kulshreshtha, A.; Cohen, J.W.; Yates, B.; Rosing, D.R.; Sidenko, S.; Delbrook, C.; Mackall, C.; Wiley, B.; et al. Impact of cytokine release syndrome on cardiac function following CD19 CAR-T cell therapy in children and young adults with hematological malignancies. J. Immunother. Cancer 2020, 8, e001159. [Google Scholar] [CrossRef]
- Afzal, A.; Farooque, U.; Gillies, E.; Hassell, L. T-cell Therapy-Mediated Myocarditis Secondary to Cytokine Release Syndrome. Cureus 2020, 12, e10022. [Google Scholar] [CrossRef] [PubMed]
- Palecek, T.; Ganame, J.; Di Salvo, G. Myocardial Diseases: Current Views on Etiopathogenesis, Diagnostic Modalities, and Therapeutic Options. Biomed. Res. Int. 2016, 2016, 1720405. [Google Scholar] [CrossRef] [PubMed]
- Saad, H.A.B.; Ntusi, N. HIV-Associated Cardiovascular Disease. Advances in HIV and AIDS Control; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef]
- Freiberg, M.S.; Chang, C.H.; Skanderson, M.; Patterson, O.V.; DuVall, S.L.; Brandt, C.A.; So-Armah, K.A.; Vasan, R.S.; Oursler, K.A.; Gottdiener, J.; et al. Association between HIV Infection and the Risk of Heart Failure with Reduced Ejection Fraction and Preserved Ejection Fraction in the Antiretroviral Therapy Era: Results from the Veterans Aging Cohort Study. JAMA Cardiol. 2017, 2, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Rroku, A.; Kottwitz, J.; Heidecker, B. Update on myocarditis–what we know so far and where we may be heading. Eur. Heart J. Acute Cardiovasc. Care 2020, 22, 2048872620910109. [Google Scholar] [CrossRef]
- Lumsden, R.H.; Bloomfield, G.S. The Causes of HIV-Associated Cardiomyopathy: A Tale of Two Worlds. Biomed. Res. Int. 2016, 2016, 8196560. [Google Scholar] [CrossRef]
- Bloomfield, G.S.; Alenezi, F.; Barasa, F.A.; Lumsden, R.; Mayosi, B.M.; Velazquez, E.J. Human Immunodeficiency Virus and Heart Failure in Low- and Middle-Income Countries. JACC Heart Fail. 2015, 3, 579–590. [Google Scholar] [CrossRef]
- Sinha, A.; Feinstein, M. Epidemiology, pathophysiology, and prevention of heart failure in people with HIV. Prog. Cardiovasc. Dis. 2020, 63, 134–141. [Google Scholar] [CrossRef]
- Kaul, S.; Fishbein, M.C.; Siegel, R.J. Cardiac manifestations of acquired immune deficiency syndrome: A 1991 update. Am. Heart J. 1991, 122, 535–544. [Google Scholar] [CrossRef]
- Yeung, C.; Baranchuk, A. Diagnosis and Treatment of Lyme Carditis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 717–726. [Google Scholar] [CrossRef]
- Woolf, P.K.; Lorsung, E.M.; Edwards, K.S.; Li, K.I.; Kanengiser, S.J.; Ruddy, R.M.; Gewitz, M.H. Electrocardiographic findings in children with Lyme disease. Pediatr. Emerg. Care 1991, 7, 334–336. [Google Scholar] [CrossRef]
- Dumic, I.; Jevtic, D.; Veselinovic, M.; Nordstrom, C.W.; Jovanovic, M.; Mogulla, V.; Veselinovic, E.M.; Hudson, A.; Simeunovic, G.; Petcu, E.; et al. Human Granulocytic Anaplasmosis-A Systematic Review of Published Cases. Microorganisms 2022, 10, 1433. [Google Scholar] [CrossRef]
- Malik, A.; Jameel, M.N.; Ali, S.S.; Mir, S. Human granulocytic anaplasmosis affecting the myocardium. J. Gen. Intern. Med. 2005, 20, C8–C10. [Google Scholar] [CrossRef]
- Caforio, A.L.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648a–d. [Google Scholar]
- Nagai, T.; Inomata, T.; Kohno, T.; Sato, T.; Tada, A.; Kubo, T.; Nakamura, K.; Oyama-Manabe, N.; Ikeda, Y.; Fujino, T.; et al. Japanese Circulation Society Joint Working Group. JCS 2023 Guideline on the Diagnosis and Treatment of Myocarditis. Circ. J. 2023, 87, 674–754. [Google Scholar] [CrossRef]
- Tefferi, A.; Gotlib, J.; Pardanani, A. Hypereosinophilic syndrome and clonal eosinophilia: Point-of-care diagnostic algorithm and treatment update. Mayo Clin. Proc. 2010, 85, 158–164. [Google Scholar] [CrossRef]
- Ogbogu, P.U.; Bochner, B.S.; Butterfield, J.H.; Gleich, G.J.; Huss-Marp, J.; Kahn, J.E.; Leiferman, K.M.; Nutman, T.B.; Pfab, F.; Ring, J. Hypereosinophilic syndrome: A multicenter, retrospective analysis of clinical characteristics and response to therapy. J. Allergy Clin. Immunol. 2009, 124, 1319–1325.e3. [Google Scholar] [CrossRef]
- Datta, T.; Solomon, A.J. Clozapine-induced myocarditis. Oxf. Med. Case Rep. 2018, 2018, omx080. [Google Scholar] [CrossRef]
- Radovanovic, M.; Jevtic, D.; Calvin, A.D.; Petrovic, M.; Paulson, M.; Rueda Prada, L.; Sprecher, L.; Savic, I.; Dumic, I. “Heart in DRESS”: Cardiac Manifestations, Treatment and Outcome of Patients with Drug Reaction with Eosinophilia and Systemic Symptoms Syndrome: A Systematic Review. J. Clin. Med. 2022, 11, 704. [Google Scholar] [CrossRef]
- Morikawa, D.; Hiraoka, E.; Obunai, K.; Norisue, Y. Myocarditis Associated with Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Syndrome: A Case Report and Review of the Literature. Am. J. Case Rep. 2018, 19, 978–984. [Google Scholar] [CrossRef]
- Shaughnessy, K.K.; Bouchard, S.M.; Mohr, M.R.; Herre, J.M.; Salkey, K.S. Minocycline-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome with persistent myocarditis. J. Am. Acad. Dermatol. 2010, 62, 315–318. [Google Scholar] [CrossRef]
- Bryde, R.E.; Ray, J.C.; Sacco, K.A.; Shapiro, B.; Cooper, L. Eosinophillic Myocarditis Secondary to Metastatic Melanoma. Radiol. Cardiothorac. Imaging 2019, 1, e190076. [Google Scholar] [CrossRef] [PubMed]
- Epelboin, L.; Jauréguiberry, S.; Estève, J.B.; Danis, M.; Komajda, M.; Bricaire, F.; Caumes, E. Myocarditis during acute schistosomiasis in two travelers. Am. J. Trop. Med. Hyg. 2010, 82, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Pakbaz, M.; Pakbaz, M. Cardiac Involvement in Eosinophilic Granulomatosis with Polyangiitis: A Meta-Analysis of 62 Case Reports. J. Tehran Heart Cent. 2020, 15, 18–26. [Google Scholar] [CrossRef]
- Garty, B.Z.; Offer, I.; Livni, E.; Danon, Y.L. Erythema multiforme and hypersensitivity myocarditis caused by ampicillin. Ann. Pharmacother. 1994, 28, 730–731. [Google Scholar] [CrossRef]
- Çetin, M.; Mis, M.D.; Karaman, K.; Yavuz, Í.H.; Geylan, H.; Tunçdemir, P.; Demir, F. Carbamazepine-induced DRESS syndrome leading to reversible myocarditis in a child. Cent. Eur. J. Immunol. 2019, 44, 102–105. [Google Scholar] [CrossRef]
- Ang, C.C.; Wang, Y.S.; Yoosuff, E.L.; Tay, Y.K. Retrospective analysis of drug-induced hypersensitivity syndrome: A study of 27 patients. J. Am. Acad. Dermatol. 2010, 63, 219–227. [Google Scholar] [CrossRef]
- Eshki, M.; Allanore, L.; Musette, P.; Milpied, B.; Grange, A.; Guillaume, J.C.; Chosidow, O.; Guillot, I.; Paradis, V.; Joly, P.; et al. Twelve-year analysis of severe cases of drug reaction with eosinophilia and systemic symptoms: A cause of unpredictable multiorgan failure. Arch. Dermatol. 2009, 145, 67–72. [Google Scholar] [CrossRef]
- Bourgeois, G.P.; Cafardi, J.A.; Groysman, V.; Hughey, L.C. A review of DRESS-associated myocarditis. J. Am. Acad. Dermatol. 2012, 66, e229–e236. [Google Scholar] [CrossRef]
- Xu, J.; Brooks, E.G. Giant Cell Myocarditis: A Brief Review. Arch. Pathol. Lab. Med. 2016, 140, 1429–1434. [Google Scholar] [CrossRef]
- Hu, Y.; Ren, J.; Dong, X.; Zhang, D.; Qu, Y.; Yang, C.; Sun, Y.; Li, J.; Luo, F.; Wang, W.; et al. Fulminant Giant Cell Myocarditis vs. Lymphocytic Myocarditis: A Comparison of Their Clinical Characteristics, Treatments, and Outcomes. Front. Cardiovasc. Med. 2021, 8, 770549. [Google Scholar] [CrossRef]
- Gadela, N.V.; Krishnan, A.M.; Mukarram, O.; Sthalekar, N. Giant cell myocarditis. Proc. Bayl. Univ. Med. Cent. 2021, 34, 401–402. [Google Scholar] [CrossRef] [PubMed]
- Ghaly, M.; Schiliro, D.; Stepczynski, J. Giant Cell Myocarditis: A Time Sensitive Distant Diagnosis. Cureus 2020, 12, e6712. [Google Scholar] [CrossRef]
- Al-Kindi, S.G.; Oliveira, G.H. Reporting of immune checkpoint inhibitor-associated myocarditis. Lancet 2018, 392, 382–383. [Google Scholar] [CrossRef]
- Ma, R.; Wang, Q.; Meng, D.; Li, K.; Zhang, Y. Immune checkpoint inhibitors-related myocarditis in patients with cancer: An analysis of international spontaneous reporting systems. BMC Cancer 2021, 21, 38. [Google Scholar] [CrossRef]
- Vasbinder, A.; Chen, Y.; Procureur, A.; Gradone, A.; Azam, T.U.; Perry, D.; Shadid, H.; Anderson, E.; Catalan, T.; Blakely, P.; et al. Biomarker Trends, Incidence, and Outcomes of Immune Checkpoint Inhibitor-Induced Myocarditis. JACC CardioOncol. 2022, 4, 689–700. [Google Scholar] [CrossRef]
- Lee, D.H.; Jain, M.; Lazaryan, A.; Locke, F.L.; Jeong, D.; Alomar, M. Case of Myocarditis after Chimeric Antigen Receptor T Cells with Intracardiac Lymphoma. JACC Case Rep. 2022, 8, 101634. [Google Scholar] [CrossRef]
- Lee, D.H.; Chandrasekhar, S.; Jain, M.D.; Mhaskar, R.; Reid, K.; Lee, S.B.; Corallo, S.; Hidalgo-Vargas, M.J.; Kumar, A.; Chavez, J.; et al. Cardiac and inflammatory biomarker differences in adverse cardiac events after chimeric antigen receptor T-Cell therapy: An exploratory study. Cardiooncology 2023, 1, 18. [Google Scholar] [CrossRef]
- Perel-Winkler, A.; Bokhari, S.; Perez-Recio, T.; Zartoshti, A.; Askanase, A.; Geraldino-Pardilla, L. Myocarditis in systemic lupus erythematosus diagnosed by 18F-fluorodeoxyglucose positron emission tomography. Lupus Sci. Med. 2018, 5, e000265. [Google Scholar] [CrossRef]
- Aretz, H.T. Myocarditis: The Dallas criteria. Hum. Pathol. 1987, 18, 619–624. [Google Scholar] [CrossRef]
- Brociek, E.; Tymińska, A.; Giordani, A.S.; Caforio, A.L.P.; Wojnicz, R.; Grabowski, M.; Ozierański, K. Myocarditis: Etiology, Pathogenesis, and Their Implications in Clinical Practice. Biology 2023, 12, 874. [Google Scholar] [CrossRef]
- Pandey, S.; Rajasurya, V. Nonviral Myocarditis; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK536928/ (accessed on 15 August 2023).
- Nguyen, L.S.; Cooper, L.T.; Kerneis, M.; Funck-Brentano, C.; Silvain, J.; Brechot, N.; Hekimian, G.; Ammirati, E.; Ben M’Barek, B.; Redheuil, A.; et al. Systematic analysis of drug-associated myocarditis reported in the World Health Organization pharmacovigilance database. Nat. Commun. 2022, 13, 25. [Google Scholar] [CrossRef]
- Kounis, N.G.; Koniari, I.; Mplani, V.; Plotas, P.; Velissaris, D. Hypersensitivity Myocarditis and the Pathogenetic Conundrum of COVID-19 Vaccine-Related Myocarditis. Cardiology 2022, 147, 413–415. [Google Scholar] [CrossRef]
- Bracamonte-Baran, W.; Čiháková, D. Cardiac Autoimmunity: Myocarditis. Adv. Exp. Med. Biol. 2017, 1003, 187–221. [Google Scholar]
- Park, Y.; Ahn, S.G.; Ko, A.; Ra, S.H.; Cha, J.; Jee, Y.G.; Lee, J.H. Hypersensitivity myocarditis confirmed by cardiac magnetic resonance imaging and endomyocardial biopsy. Korean J. Intern. Med. 2014, 29, 236–240. [Google Scholar] [CrossRef]
- JCS Joint Working Group. Guidelines for diagnosis and treatment of myocarditis (JCS 2009): Digest version. Circ. J. 2011, 75, 734–743. [Google Scholar] [CrossRef]
- Ammirati, E.; Moslehi, J.J. Diagnosis and Treatment of Acute Myocarditis: A Review. JAMA 2023, 329, 1098–1113. [Google Scholar] [CrossRef]
- Ammirati, E.; Buono, A.; Moroni, F.; Gigli, L.; Power, J.R.; Ciabatti, M.; Garascia, A.; Adler, E.D.; Pieroni, M. State-of-the-Art of Endomyocardial Biopsy on Acute Myocarditis and Chronic Inflammatory Cardiomyopathy. Curr. Cardiol. Rep. 2022, 24, 597–609. [Google Scholar] [CrossRef]
- Lampejo, T.; Durkin, S.M.; Bhatt, N.; Guttmann, O. Acute myocarditis: Aetiology, diagnosis and management. Clin. Med. 2021, 21, e505–e510. [Google Scholar] [CrossRef]
- Daniels, C.J.; Rajpal, S.; Greenshields, J.T.; Rosenthal, G.L.; Chung, E.H.; Terrin, M.; Jeudy, J.; Mattson, S.E.; Law, I.H.; Borchers, J.; et al. Big Ten COVID-19 Cardiac Registry Investigators. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes with Recent SARS-CoV-2 Infection: Results from the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021, 6, 1078–1087. [Google Scholar] [CrossRef]
- Wang, D.; Li, S.; Jiang, J.; Yan, J.; Zhao, C.; Wang, Y.; Ma, Y.; Zeng, H.; Guo, X.; Wang, H.; et al. Section of Precision Medicine Group of Chinese Society of Cardiology; Editorial Board of Chinese Journal of Cardiology; Working Group of Adult Fulminant Myocarditis. Chinese society of cardiology expert consensus statement on the diagnosis and treatment of adult fulminant myocarditis. Sci. China Life Sci. 2019, 62, 187–202. [Google Scholar]
- Al-Akchar, M.; Shams, P.; Kiel, J. Acute Myocarditis; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK441847/ (accessed on 20 August 2023).
- Ammirati, E.; Veronese, G.; Brambatti, M.; Merlo, M.; Cipriani, M.; Potena, L.; Sormani, P.; Aoki, T.; Sugimura, K.; Sawamura, A.; et al. Fulminant Versus Acute Nonfulminant Myocarditis in Patients with Left Ventricular Systolic Dysfunction. J. Am. Coll. Cardiol. 2019, 74, 299–311. [Google Scholar] [CrossRef]
- Ammirati, E.; Cipriani, M.; Moro, C.; Raineri, C.; Pini, D.; Sormani, P.; Mantovani, R.; Varrenti, M.; Pedrotti, P.; Conca, C.; et al. Registro Lombardo delle Miocarditi. Clinical presentation and outcome in a contemporary cohort of patients with acute myocarditis: Multicenter lombardy registry. Circulation 2018, 138, 1088–1099. [Google Scholar] [CrossRef] [PubMed]
- Kociol, R.D.; Cooper, L.T.; Fang, J.C.; Moslehi, J.J.; Pang, P.S.; Sabe, M.A.; Shah, R.V.; Sims, D.B.; Thiene, G.; Vardeny, O. American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology. Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement from the American Heart Association. Circulation 2020, 141, e69–e92. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, R.E., 3rd; Boehmer, J.P.; Hruban, R.H.; Hutchins, G.M.; Kasper, E.K.; Hare, J.M.; Baughman, K.L. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N. Engl. J. Med. 2000, 342, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Anzini, M.; Merlo, M.; Sabbadini, G.; Barbati, G.; Finocchiaro, G.; Pinamonti, B.; Salvi, A.; Perkan, A.; Di Lenarda, A.; Bussani, R.; et al. Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation 2013, 128, 2384–2394. [Google Scholar] [CrossRef]
- Ammirati, E.; Cipriani, M.; Lilliu, M.; Sormani, P.; Varrenti, M.; Raineri, C.; Petrella, D.; Garascia, A.; Pedrotti, P.; Roghi, A.; et al. Survival and Left Ventricular Function Changes in Fulminant Versus Nonfulminant Acute Myocarditis. Circulation 2017, 136, 529–545. [Google Scholar] [CrossRef] [PubMed]
- Jeserich, M.; Konstantinides, S.; Olschewski, M.; Pavlik, G.; Bode, C.; Geibel, A. Diagnosis of early myocarditis after respiratory or gastrointestinal tract viral infection: Insights from cardiovascular magnetic resonance. Clin. Res. Cardiol. 2010, 99, 707–714. [Google Scholar] [CrossRef]
- Vohra, S.; Yadav, A.; Sharma, P.; Khan, S.; Jaiswal, V. Acute myocarditis masquerading as anterior wall myocardial infarction: A case report. Ann. Med. Surg. 2022, 84, 104884. [Google Scholar] [CrossRef]
- White, J.A.; Hansen, R.; Abdelhaleem, A.; Mikami, Y.; Peng, M.; Rivest, S.; Satriano, A.; Dykstra, S.; Flewitt, J.; Heydari, B.; et al. Natural History of Myocardial Injury and Chamber Remodeling in Acute Myocarditis. Circ. Cardiovasc. Imaging 2019, 12, e008614. [Google Scholar] [CrossRef]
- Gräni, C.; Eichhorn, C.; Bière, L.; Murthy, V.L.; Agarwal, V.; Kaneko, K.; Cuddy, S.; Aghayev, A.; Steigner, M.; Blankstein, R.; et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J. Am. Coll. Cardiol. 2017, 70, 1964–1976. [Google Scholar] [CrossRef]
- Younis, A.; Matetzky, S.; Mulla, W.; Masalha, E.; Afel, Y.; Chernomordik, F.; Fardman, A.; Goitein, O.; Ben-Zekry, S.; Peled, Y.; et al. Epidemiology characteristics and outcome of patients with clinically diagnosed acute myocarditis. Am. J. Med. 2020, 133, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Adamopoulos, S.; Miliopoulos, D.; Karavidas, A.; Nikolaou, M.; Lazaros, G.; Gkouziouta, A.; Manginas, A.; Sevastos, G.; Karvounis, H.; Karamitsos, T.D.; et al. HEllenic Registry on Myocarditis SyndromES on behalf of Hellenic Heart Failure Association: The HERMES-HF Registry. ESC Heart Fail. 2020, 7, 3676–3684. [Google Scholar] [CrossRef] [PubMed]
- Dries, D.J. Chest Pain. Air Med. J. 2016, 35, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Aquaro, G.D.; Perfetti, M.; Camastra, G.; Monti, L.; Dellegrottaglie, S.; Moro, C.; Pepe, A.; Todiere, G.; Lanzillo, C.; Scatteia, A.; et al. Cardiac Magnetic Resonance Working Group of the Italian Society of Cardiology. Cardiac MR with Late Gadolinium Enhancement in Acute Myocarditis with Preserved Systolic Function: ITAMY Study. J. Am. Coll. Cardiol. 2017, 70, 1977–1987. [Google Scholar] [CrossRef]
- Cannata, A.; Bhatti, P.; Roy, R.; Al-Agil, M.; Daniel, A.; Ferone, E.; Jordan, A.; Cassimon, B.; Bradwell, S.; Khawaja, A.; et al. Prognostic relevance of demographic factors in cardiac magnetic resonance-proven acute myocarditis: A cohort study. Front. Cardiovasc. Med. 2022, 9, 1037837. [Google Scholar] [CrossRef]
- Angelini, A.; Calzolari, V.; Calabrese, F.; Boffa, G.M.; Maddalena, F.; Chioin, R.; Thiene, G. Myocarditis mimicking acute myocardial infarction: Role of endomyocardial biopsy in the differential diagnosis. Heart 2000, 84, 245–250. [Google Scholar] [CrossRef]
- Khandaker, M.H.; Espinosa, R.E.; Nishimura, R.A.; Sinak, L.J.; Hayes, S.N.; Melduni, R.M.; Oh, J.K. Pericardial disease: Diagnosis and management. Mayo Clin. Proc. 2010, 85, 572–593. [Google Scholar] [CrossRef]
- Aota, H.; Suzuki, H.; Godo, S.; Kuniyoshi, S.; Fujishima, F.; Tahakashi, J.; Yasuda, S. A teenage boy with acute myocarditis and reversible microvascular angina: A case report. J. Cardiol. Cases 2023, 27, 254–257. [Google Scholar] [CrossRef]
- Silva, D.; Marques, P.; Martins, S.; Bordalo, E.; Sá, A.L.; Nóbrega, J.; Duarte, J.; Almeida, A.G.; Gabriel, H.M.; Correia, M.J.; et al. Coronary artery vasospasm and acute myocarditis: A rare association. Rev. Port. Cardiol. 2010, 29, 1879–1888. [Google Scholar]
- McCully, R.B.; Cooper, L.T.; Schreiter, S. Coronary artery spasm in lymphocytic myocarditis: A rare cause of acute myocardial infarction. Heart 2005, 91, 202. [Google Scholar] [CrossRef]
- Khan, Z.; Pabani, U.K.; Gul, A.; Muhammad, S.A.; Yousif, Y.; Abumedian, M.; Elmahdi, O.; Gupta, A. COVID-19 Vaccine-Induced Myocarditis: A Systemic Review and Literature Search. Cureus 2022, 14, e27408. [Google Scholar] [CrossRef]
- Bonanni, M.; Angelini, G.; Leo, L.A.; Schlossbauer, S.A.; Bergamaschi, L.; Landi, A.; Sangiorgi, G.M.; Forleo, C.; Pasotti, E.; Pedrazzini, G.; et al. Multimodality Imaging Evaluation to Detect Subtle Right Ventricular Involvement in Patients with Acute Myocarditis and Preserved Left Ventricular Ejection Fraction. J. Clin. Med. 2023, 12, 4308. [Google Scholar] [CrossRef] [PubMed]
- Duncan, B.W.; Bohn, D.J.; Atz, A.M.; French, J.W.; Laussen, P.C.; Wessel, D.L. Mechanical circulatory support for the treatment of children with acute fulminant myocarditis. J. Thorac. Cardiovasc. Surg. 2001, 122, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Pages, O.N.; Aubert, S.; Combes, A.; Luyt, C.E.; Pavie, A.; Léger, P.; Gandjbakhch, I.; Leprince, P. Paracorporeal pulsatile biventricular assist device versus extracorporal membrane oxygenation-extracorporal life support in adult fulminant myocarditis. J. Thorac. Cardiovasc. Surg. 2009, 137, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Peretto, G.; Sala, S.; Rizzo, S.; De Luca, G.; Campochiaro, C.; Sartorelli, S.; Benedetti, G.; Palmisano, A.; Esposito, A.; Tresoldi, M.; et al. Arrhythmias in myocarditis: State of the art. Heart Rhythm 2019, 16, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Karki, R.; Janga, C.; Deshmukh, A.J. Arrhythmias Associated with Inflammatory Cardiomyopathies. Curr Treat Options Cardiovasc. Med. 2020, 22, 76. [Google Scholar] [CrossRef]
- Kragholm, K.H.; Lindgren, F.L.; Zaremba, T.; Freeman, P.; Andersen, N.H.; Riahi, S.; Pareek, M.; Køber, L.; Torp-Pedersen, C.; Søgaard, P.; et al. Mortality and ventricular arrhythmia after acute myocarditis: A nationwide registry-based follow-up study. Open Heart 2021, 8, e001806. [Google Scholar] [CrossRef]
- Sozzi, F.B.; Gherbesi, E.; Faggiano, A.; Gnan, E.; Maruccio, A.; Schiavone, M.; Iacuzio, L.; Carugo, S. Viral Myocarditis: Classification, Diagnosis, and Clinical Implications. Front. Cardiovasc. Med. 2022, 9, 908663. [Google Scholar] [CrossRef]
- Law, Y.M.; Lal, A.K.; Chen, S.; Čiháková, D.; Cooper, L.T., Jr.; Deshpande, S.; Godown, J.; Grosse-Wortmann, L.; Robinson, J.D.; Towbin, J.A. American Heart Association Pediatric Heart Failure and Transplantation Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young and Stroke Council. Diagnosis and Management of Myocarditis in Children: A Scientific Statement from the American Heart Association. Circulation 2021, 144, e123–e135. [Google Scholar]
- Subahi, A.; Akintoye, E.; Yassin, A.S.; Abubakar, H.; Adegbala, O.; Mishra, T.; Abdelrahman, M.; Shokr, M.; Afonso, L. Impact of atrial fibrillation on patients hospitalized for acute myocarditis: Insights from a nationally-representative United States cohort. Clin. Cardiol. 2019, 42, 26–31. [Google Scholar] [CrossRef]
- Rosier, L.; Zouaghi, A.; Barré, V.; Martins, R.; Probst, V.; Marijon, E.; Sadoul, N.; Chauveau, S.; Da Costa, A.; Badoz, M.; et al. High Risk of Sustained Ventricular Arrhythmia Recurrence after Acute Myocarditis. J. Clin. Med. 2020, 9, 848. [Google Scholar] [CrossRef]
- Okura, Y.; Dec, G.W.; Hare, J.M.; Kodama, M.; Berry, G.J.; Tazelaar, H.D.; Bailey, K.R.; Cooper, L.T. A clinical and histopathologic comparison of cardiac sarcoidosis and idiopathic giant cell myocarditis. J. Am. Coll. Cardiol. 2003, 41, 322–329. [Google Scholar] [CrossRef]
- Kandolin, R.; Lehtonen, J.; Kupari, M. Cardiac sarcoidosis and giant cell myocarditis as causes of atrioventricular block in young and middle-aged adults. Circ. Arrhythm. Electrophysiol. 2011, 4, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Wan, D.; Baranchuk, A. Lyme carditis and atrioventricular block. CMAJ 2018, 190, E622. [Google Scholar] [CrossRef] [PubMed]
- Alamri, A.S.; Khayat, L.T.; Alzahrani, A.J.; Kurdi, L.K.; Alkhameesi, N.F.; Bahaidarah, S.A. Clinical Presentation of Myocarditis in the Pediatric Age Group and Predictors of Poor Early and Late Outcomes: Academic Hospital Experience. Cureus 2022, 14, e31643. [Google Scholar] [CrossRef]
- Abe, T.; Tsuda, E.; Miyazaki, A.; Ishibashi-Ueda, H.; Yamada, O. Clinical characteristics and long-term outcome of acute myocarditis in children. Heart Vessel. 2013, 28, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013, 128, 1810–1852. [Google Scholar] [CrossRef]
- Károlyi, M.; Kolossváry, M.; Weber, L.; Matziris, I.; Polacin, M.; Sokolska, J.M.; Gotschy, A.; Alkadhi, H.; Manka, R. Association between ECG parameters and late gadolinium enhancement along the course of myocarditis. Int. J. Cardiovasc. Imaging 2023, 39, 1169–1178. [Google Scholar] [CrossRef]
- Cooper, L.T., Jr. Myocarditis. N. Engl. J. Med. 2009, 360, 1526–1538. [Google Scholar] [CrossRef]
- Nakashima, H.; Honda, Y.; Katayama, T. Serial electrocardiographic findings in acute myocarditis. Intern Med. 1994, 33, 659–666. [Google Scholar] [CrossRef]
- Ogunbayo, G.O.; Elayi, S.C.; Ha, L.D.; Olorunfemi, O.; Elbadawi, A.; Saheed, D.; Sorrell, V.L. Outcomes of Heart Block in Myocarditis: A Review of 31,760 Patients. Heart Lung Circ. 2019, 28, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Stulova, M.A.; Konstantinova, E.V. Ventricular extrasystole as manifestation of viral myocarditis and myopericarditis in young patients. Ter. Arkh. 2007, 79, 28–34. [Google Scholar] [PubMed]
- Baksi, A.J.; Kanaganayagam, G.S.; Prasad, S.K. Arrhythmias in viral myocarditis and pericarditis. Card. Electrophysiol. Clin. 2015, 7, 269–281. [Google Scholar] [CrossRef]
- Chen, J.; Chen, S.; Li, Z.; Zhou, P.; Huang, W.; Wang, H.; Shi, J.; Ni, Y.; Lin, L.; Lei, Y. Role of electrocardiograms in assessment of severity and analysis of the characteristics of ST elevation in acute myocarditis: A two-centre study. Exp. Ther. Med. 2020, 20, 20. [Google Scholar] [CrossRef]
- Buttà, C.; Zappia, L.; Laterra, G.; Roberto, M. Diagnostic and prognostic role of electrocardiogram in acute myocarditis: A comprehensive review. Ann. Noninvasive Electrocardiol. 2020, 25, e12726. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.C.; Brady, W.J.; Pollack, M. Electrocardiographic manifestations: Acute myopericarditis. J. Emerg. Med. 1999, 17, 865–872. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Birnbaum, Y. ST-segment elevation: Distinguishing ST elevation myocardial infarction from ST elevation secondary to nonischemic etiologies. World J. Cardiol. 2014, 6, 1067–1079. [Google Scholar] [CrossRef]
- Birnbaum, Y.; Perez Riera, A.R.; Nikus, K. PR depression with multi lead ST elevation and ST depression in aVR: Is it always acute pericarditis? J. Electrocardiol. 2019, 54, 13–17. [Google Scholar] [CrossRef]
- Sarda, L.; Colin, P.; Boccara, F.; Daou, D.; Lebtahi, R.; Faraggi, M.; Nguyen, C.; Cohen, A.; Slama, M.S.; Steg, P.G.; et al. Myocarditis in patients with clinical presentation of myocardial infarction and normal coronary angiograms. J. Am. Coll. Cardiol. 2001, 37, 786–792. [Google Scholar] [CrossRef]
- Yang, D.; Dai, Q.; Wu, H.; Chen, J.; Zhang, J.; Wei, Z. The diagnostic capability of electrocardiography on the cardiogenic shock in the patients with acute myocarditis. BMC Cardiovasc. Disord. 2020, 20, 502. [Google Scholar] [CrossRef]
- Di Bella, G.; Florian, A.; Oreto, L.; Napolitano, C.; Todaro, M.C.; Donato, R.; Calamelli, S.; Camastra, G.S.; Zito, C.; Carerj, S.; et al. Electrocardiographic findings and myocardial damage in acute myocarditis detected by cardiac magnetic resonance. Clin. Res. Cardiol. 2012, 101, 617–624. [Google Scholar] [CrossRef] [PubMed]
- De Lazzari, M.; Zorzi, A.; Baritussio, A.; Siciliano, M.; Migliore, F.; Susana, A.; Giorgi, B.; Lacognata, C.; Iliceto, S.; Perazzolo Marra, M.; et al. Relationship between T-wave inversion and transmural myocardial edema as evidenced by cardiac magnetic resonance in patients with clinically suspected acute myocarditis: Clinical and prognostic implications. J. Electrocardiol. 2016, 49, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, M.; O’Quinn, R.; Ky, B.; Callans, D.; Kucharczuk, J.; Carver, J.R. Persistent PR segment change in malignant pericardial disease. Cardiooncology 2016, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Madias, J.E. Transient attenuation of the amplitude of the QRS complexes in the diagnosis of Takotsubo syndrome. Eur. Heart J. Acute Cardiovasc. Care 2014, 3, 28–36. [Google Scholar] [CrossRef]
- Ukena, C.; Mahfoud, F.; Kindermann, I.; Kandolf, R.; Kindermann, M.; Böhm, M. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur. J. Heart Fail. 2011, 13, 398–405. [Google Scholar] [CrossRef]
- Sawamura, A.; Okumura, T.; Ito, M.; Ozaki, Y.; Ohte, N.; Amano, T.; Murohara, T. CHANGE PUMP Investigators. Prognostic Value of Electrocardiography in Patients with Fulminant Myocarditis Supported by Percutaneous Venoarterial Extracorporeal Membrane Oxygenation—Analysis from the CHANGE PUMP Study. Circ. J. 2018, 82, 2089–2095. [Google Scholar] [CrossRef]
- Brambatti, M.; Matassini, M.V.; Adler, E.D.; Klingel, K.; Camici, P.G.; Ammirati, E. Eosinophilic Myocarditis: Characteristics, Treatment, and Outcomes. J. Am. Coll. Cardiol. 2017, 70, 2363–2375. [Google Scholar] [CrossRef]
- Viwe, M.; Nery, P.; Birnie, D.H. Management of ventricular tachycardia in patients with cardiac sarcoidosis. Heart Rhythm O2 2021, 2, 412–422. [Google Scholar] [CrossRef]
- Morgera, T.; Di Lenarda, A.; Dreas, L.; Pinamonti, B.; Humar, F.; Bussani, R.; Silvestri, F.; Chersevani, D.; Camerini, F. Electrocardiography of myocarditis revisited: Clinical and prognostic significance of electrocardiographic changes. Am. Heart J. 1992, 124, 455–467. [Google Scholar] [CrossRef]
- Bhattacharya, I.S.; Dweck, M.; Francis, M. Lyme carditis: A reversible cause of complete atrioventricular block. J. R. Coll. Physicians Edinb. 2010, 40, 121–122. [Google Scholar] [CrossRef]
- Kandolin, R.; Lehtonen, J.; Salmenkivi, K.; Räisänen-Sokolowski, A.; Lommi, J.; Kupari, M. Diagnosis, treatment, and outcome of giant-cell myocarditis in the era of combined immunosuppression. Circ. Heart Fail. 2013, 6, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Sekhri, V.; Sanal, S.; Delorenzo, L.J.; Aronow, W.S.; Maguire, G.P. Cardiac sarcoidosis: A comprehensive review. Arch. Med. Sci. 2011, 7, 546–554. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, K.A.; Szwabe, K.; Urbanek, I.; Ptaszynski, P.; Strzelecki, A.; Wranicz, J.K.; Cygankiewicz, I. Prevalence of Lyme Carditis in Patients with Atrioventricular Blocks. Int. J. Environ. Res. Public Health 2022, 19, 14893. [Google Scholar] [CrossRef]
- Suresh, A.; Martens, P.; Tang, W.H.W. Biomarkers for Myocarditis and Inflammatory Cardiomyopathy. Curr. Heart Fail. Rep. 2022, 19, 346–355. [Google Scholar] [CrossRef]
- Amioka, N.; Nakamura, K.; Kimura, T.; Ohta-Ogo, K.; Tanaka, T.; Toji, T.; Akagi, S.; Nakagawa, K.; Toh, N.; Yoshida, M.; et al. Pathological and clinical effects of interleukin-6 on human myocarditis. J. Cardiol. 2021, 78, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Fuse, K.; Kodama, M.; Okura, Y.; Ito, M.; Hirono, S.; Kato, K.; Hanawa, H.; Aizawa, Y. Predictors of disease course in patients with acute myocarditis. Circulation 2000, 102, 2829–2835. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Zhang, X.; Shen, J.; Jiang, B.; Hu, D.; Zhao, M. Heparin-Binding Protein: A Novel Biomarker Linking Four Different Cardiovascular Diseases. Cardiol Res. Pract. 2020, 15, 9575373. [Google Scholar] [CrossRef]
- Müller, I.; Vogl, T.; Kühl, U.; Krannich, A.; Banks, A.; Trippel, T.; Noutsias, M.; Maisel, A.S.; van Linthout, S.; Tschöpe, C. Serum alarmin S100A8/S100A9 levels and its potential role as biomarker in myocarditis. ESC Heart Fail. 2020, 7, 1442–1451. [Google Scholar] [CrossRef]
- Coronado, M.J.; Bruno, K.A.; Blauwet, L.A.; Tschöpe, C.; Cunningham, M.W.; Pankuweit, S.; van Linthout, S.; Jeon, E.S.; McNamara, D.M.; Krejčí, J.; et al. Elevated Sera sST2 Is Associated with Heart Failure in Men ≤50 Years Old with Myocarditis. J. Am. Heart Assoc. 2019, 8, e008968. [Google Scholar] [CrossRef]
- Mirna, M.; Schmutzler, L.; Topf, A.; Hoppe, U.C.; Lichtenauer, M. Neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio predict length of hospital stay in myocarditis. Sci. Rep. 2021, 11, 18101. [Google Scholar] [CrossRef]
- Kanda, T.; Kobayashi, I.; Suzuki, T.; Murata, K.; Radio, S.J.; McManus, B.M. Elevation of ALT to AST ratio in patients with enteroviral myocarditis. J. Med. 1995, 26, 153–162. [Google Scholar] [PubMed]
- Omran, F.; Kyrou, I.; Osman, F.; Lim, V.G.; Randeva, H.S.; Chatha, K. Cardiovascular Biomarkers: Lessons of the Past and Prospects for the Future. Int. J. Mol. Sci. 2022, 23, 5680. [Google Scholar] [CrossRef]
- Jeremias, A.; Gibson, C.M. Narrative review: Alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann. Intern. Med. 2005, 142, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Wang, Z.; Chen, K.; Cui, G.; Chen, C.; Wang, L.; Jiang, J. The absolute and relative changes in high-sensitivity cardiac troponin I are associated with the in-hospital mortality of patients with fulminant myocarditis. BMC Cardiovasc. Disord. 2021, 21, 571. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, L.H.; Heckmann, M.B.; Bailly, G.; Finke, D.; Procureur, A.; Power, J.R.; Stein, F.; Bretagne, M.; Ederhy, S.; Fenioux, C.; et al. Cardiomuscular Biomarkers in the Diagnosis and Prognostication of Immune Checkpoint Inhibitor Myocarditis. Circulation 2023, 148, 473–486. [Google Scholar] [CrossRef]
- Sara, B.; Monteiro, J.; Carvalho, P.; Ribeiro Carvalho, C.; Chemba, J.; Ferreira, C.; Moreira, J.I. Are high NT-proBNP levels more related to inflammation than to left ventricular systolic dysfunction in acute myocarditis? Eur. Heart J. Acute Cardiovasc. Care. 2021, 10, zuab020.189. [Google Scholar] [CrossRef]
- Ukena, C.; Kindermann, M.; Mahfoud, F.; Geisel, J.; Lepper, P.M.; Kandolf, R.; Böhm, M.; Kindermann, I. Diagnostic and prognostic validity of different biomarkers in patients with suspected myocarditis. Clin. Res. Cardiol. 2014, 103, 743–751. [Google Scholar] [CrossRef]
- Li, Y.; Heuser, J.S.; Cunningham, L.C.; Kosanke, S.D.; Cunningham, M.W. Mimicry and antibody-mediated cell signaling in autoimmune myocarditis. J. Immunol. 2006, 177, 8234–8240. [Google Scholar] [CrossRef]
- Tymińska, A.; Ozierański, K.; Skwarek, A.; Kapłon-Cieślicka, A.; Baritussio, A.; Grabowski, M.; Marcolongo, R.; Caforio, A.L. Personalized Management of Myocarditis and Inflammatory Cardiomyopathy in Clinical Practice. J. Pers. Med. 2022, 12, 183. [Google Scholar] [CrossRef]
- Blagova, O.; Varionchik, N.; Zaidenov, V.; Savina, P.; Sarkisova, N. Anti-heart antibodies levels and their correlation with clinical symptoms and outcomes in patients with confirmed or suspected diagnosis COVID-19. Eur. J. Immunol. 2021, 51, 893–902. [Google Scholar] [CrossRef]
- Caforio, A.L.; Tona, F.; Bottaro, S.; Vinci, A.; Dequal, G.; Daliento, L.; Thiene, G.; Iliceto, S. Clinical implications of anti-heart autoantibodies in myocarditis and dilated cardiomyopathy. Autoimmunity 2008, 41, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, L.; Tirosh-Wagner, T.; Vardi, A.; Abbas, H.; Pillar, N.; Shomron, N.; Nevo-Caspi, Y.; Paret, G. Circulating MicroRNAs: A Potential Biomarker for Cardiac Damage, Inflammatory Response, and Left Ventricular Function Recovery in Pediatric Viral Myocarditis. J. Cardiovasc. Transl. Res. 2018, 11, 319–328. [Google Scholar] [CrossRef]
- Besler, C.; Urban, D.; Watzka, S.; Lang, D.; Rommel, K.P.; Kandolf, R.; Klingel, K.; Thiele, H.; Linke, A.; Schuler, G.; et al. Endomyocardial miR-133a levels correlate with myocardial inflammation, improved left ventricular function, and clinical outcome in patients with inflammatory cardiomyopathy. Eur. J. Heart Fail. 2016, 18, 1442–1451. [Google Scholar] [CrossRef]
- Blanco-Domínguez, R.; Sánchez-Díaz, R.; de la Fuente, H.; Jiménez-Borreguero, L.J.; Matesanz-Marín, A.; Relaño, M.; Jiménez-Alejandre, R.; Linillos-Pradillo, B.; Tsilingiri, K.; Martín-Mariscal, M.L.; et al. A Novel Circulating MicroRNA for the Detection of Acute Myocarditis. N. Engl. J. Med. 2021, 384, 2014–2027. [Google Scholar] [CrossRef] [PubMed]
- Aleshcheva, G.; Pietsch, H.; Escher, F.; Schultheiss, H.P. MicroRNA profiling as a novel diagnostic tool for identification of patients with inflammatory and/or virally induced cardiomyopathies. ESC Heart Fail. 2021, 8, 408–422. [Google Scholar] [CrossRef] [PubMed]
- Grodzka, O.; Procyk, G.; Gąsecka, A. The Role of MicroRNAs in Myocarditis-What Can We Learn from Clinical Trials? Int. J. Mol. Sci. 2022, 23, 16022. [Google Scholar] [CrossRef] [PubMed]
- Adeboye, A.; Alkhatib, D.; Butt, A.; Yedlapati, N.; Garg, N. A Review of the Role of Imaging Modalities in the Evaluation of Viral Myocarditis with a Special Focus on COVID-19-Related Myocarditis. Diagnostics 2022, 12, 549. [Google Scholar] [CrossRef]
- Felker, G.M.; Boehmer, J.P.; Hruban, R.H.; Hutchins, G.M.; Kasper, E.K.; Baughman, K.L.; Hare, J.M. Echocardiographic findings in fulminant and acute myocarditis. J. Am. Coll. Cardiol. 2000, 36, 227–232. [Google Scholar] [CrossRef]
- Hameed, A.; Condliffe, R.; Swift, A.J.; Alabed, S.; Kiely, D.G.; Charalampopoulos, A. Assessment of Right Ventricular Function-a State of the Art. Curr. Heart Fail. Rep. 2023, 20, 194–207. [Google Scholar] [CrossRef]
- Grossman, S.M.; Pravda, N.S.; Orvin, K.; Hamdan, A.; Vaturi, M.; Bengal, T.; Kornowski, R.; Weissler-Snir, A. Characterization and long-term outcomes of patients with myocarditis: A retrospective observational study. Postep. Kardiol Interwencyjnej 2021, 17, 60–67. [Google Scholar] [CrossRef]
- Meindl, C.; Paulus, M.; Poschenrieder, F.; Zeman, F.; Maier, L.S.; Debl, K. Patients with acute myocarditis and preserved systolic left ventricular function: Comparison of global and regional longitudinal strain imaging by echocardiography with quantification of late gadolinium enhancement by CMR. Clin. Res. Cardiol. 2021, 110, 1792–1800. [Google Scholar] [CrossRef] [PubMed]
- Tünnemann-Tarr, A.; Stöbe, S.; Laufs, U.; Hagendorff, A.; Tayal, B. Speckle tracking echocardiography in a patient with viral myocarditis and acute myocardial infarction. J. Cardiol. Cases 2020, 22, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Løgstrup, B.B.; Nielsen, J.M.; Kim, W.Y.; Poulsen, S.H. Myocardial oedema in acute myocarditis detected by echocardiographic 2D myocardial deformation analysis. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Sturmberger, T.; Niel, J.; Aichinger, J.; Ebner, C. Acute myocarditis with normal wall motion detected with 2D speckle tracking echocardiography. Echo. Res. Pract. 2016, 3, K15-9. [Google Scholar] [CrossRef]
- Chinali, M.; Franceschini, A.; Ciancarella, P.; Lisignoli, V.; Curione, D.; Ciliberti, P.; Esposito, C.; Del Pasqua, A.; Rinelli, G.; Secinaro, A. Echocardiographic two-dimensional speckle tracking identifies acute regional myocardial edema and sub-acute fibrosis in pediatric focal myocarditis with normal ejection fraction: Comparison with cardiac magnetic resonance. Sci. Rep. 2020, 10, 11321. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Marcotte, F. Cardiac magnetic resonance assessment of myocarditis. Circ. Cardiovasc. Imaging 2013, 6, 833–839. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Luetkens, J.A.; Faron, A.; Isaak, A.; Dabir, D.; Kuetting, D.; Feisst, A.; Schmeel, F.C.; Sprinkart, A.M.; Thomas, D. Comparison of Original and 2018 Lake Louise Criteria for Diagnosis of Acute Myocarditis: Results of a Validation Cohort. Radiol Cardiothorac Imaging 2019, 1, e190010. [Google Scholar] [CrossRef]
- Francone, M.; Chimenti, C.; Galea, N.; Scopelliti, F.; Verardo, R.; Galea, R.; Carbone, I.; Catalano, C.; Fedele, F.; Frustaci, A. CMR sensitivity varies with clinical presentation and extent of cell necrosis in biopsy-proven acute myocarditis. JACC Cardiovasc. Imaging 2014, 7, 254–263. [Google Scholar] [CrossRef]
- Polte, C.L.; Bobbio, E.; Bollano, E.; Bergh, N.; Polte, C.; Himmelman, J.; Lagerstrand, K.M.; Gao, S.A. Cardiovascular Magnetic Resonance in Myocarditis. Diagnostics 2022, 12, 399. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Piechnik, S.K.; Robson, M.D.; Neubauer, S.; Karamitsos, T.D. Myocardial tissue characterization by magnetic resonance imaging: Novel applications of T1 and T2 mapping. J. Thorac. Imaging 2014, 29, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Mewton, N.; Liu, C.Y.; Croisille, P.; Bluemke, D.; Lima, J.A. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 2011, 57, 891–903. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Zuo, H.; Liu, J.; Wang, J.; Zhang, K.; Zhang, C.; Peng, X.; Liu, Y.; Wang, D.; Li, H.; et al. The pattern of late gadolinium enhancement by cardiac MRI in fulminant myocarditis and its prognostic implication: A two-year follow-up study. Front. Cardiovasc. Med. 2023, 10, 1144469. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.G.; Strohm, O.; Schulz-Menger, J.; Marciniak, H.; Luft, F.C.; Dietz, R. Noninvasive diagnosis of acute myocarditis by contrast-enhanced magnetic resonance imaging–response to the author. Circulation 1999, 99, 459–460. [Google Scholar]
- Menacho, K.D.; Ramirez, S.; Perez, A.; Dragonetti, L.; Perez de Arenaza, D.; Katekaru, D.; Illatopa, V.; Munive, S.; Rodriguez, B.; Shimabukuro, A. Improving cardiovascular magnetic resonance access in low- and middle-income countries for cardiomyopathy assessment: Rapid cardiovascular magnetic resonance. Eur. Heart J. 2022, 43, 2496–2507. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.; Batrice, A.; Rischpler, C.; Eiber, M.; Ibrahim, T.; Nekolla, S.G. Utility of multimodal cardiac imaging with PET/MRI in cardiac sarcoidosis: Implications for diagnosis, monitoring and treatment. Eur. Heart J. 2014, 35, 312. [Google Scholar] [CrossRef]
- von Olshausen, G.; Hyafil, F.; Langwieser, N.; Laugwitz, K.L.; Schwaiger, M.; Ibrahim, T. Detection of acute inflammatory myocarditis in Epstein Barr virus infection using hybrid 18F-fluoro-deoxyglucose-positron emission tomography/magnetic resonance imaging. Circulation 2014, 130, 925–926. [Google Scholar] [CrossRef]
- Lamacie, M.M.; Almufleh, A.; Nair, V.; Stadnick, E.; Birnie, D.; Beanlands, R.; Chih, S. Serial 18F-Fluorodeoxyglucose Positron Emission Tomography Imaging in a Patient with Giant Cell Myocarditis. Circ. Cardiovasc. Imaging 2020, 13, e009940. [Google Scholar] [CrossRef]
- Mathijssen, H.; Tjoeng, T.W.H.; Keijsers, R.G.M.; Bakker, A.L.M.; Akdim, F.; van Es, H.W.; van Beek, F.T.; Veltkamp, M.V.; Grutters, J.C.; Post, M.C. The usefulness of repeated CMR and FDG PET/CT in the diagnosis of patients with initial possible cardiac sarcoidosis. EJNMMI Res. 2021, 11, 129. [Google Scholar] [CrossRef]
- Nensa, F.; Kloth, J.; Tezgah, E.; Poeppel, T.D.; Heusch, P.; Goebel, J.; Nassenstein, K.; Schlosser, T. Feasibility of FDG-PET in myocarditis: Comparison to CMR using integrated PET/MRI. J. Nucl. Cardiol. 2018, 25, 785–794. [Google Scholar] [CrossRef]
- Castiglione, V.; Aimo, A.; Todiere, G.; Barison, A.; Fabiani, I.; Panichella, G.; Genovesi, D.; Bonino, L.; Clemente, A.; Cademartiri, F. Role of Imaging in Cardiomyopathies. Card Fail Rev. 2023, 9, e08. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Jeudy, J. Assessment of Myocarditis: Cardiac MR, PET/CT, or PET/MR? Curr. Cardiol. Rep. 2019, 21, 76. [Google Scholar] [CrossRef]
- Vita, T.; Okada, D.R.; Veillet-Chowdhury, M.; Bravo, P.E.; Mullins, E.; Hulten, E.; Agrawal, M.; Madan, R.; Taqueti, V.R.; Steigner, M.; et al. Complementary Value of Cardiac Magnetic Resonance Imaging and Positron Emission Tomography/Computed Tomography in the Assessment of Cardiac Sarcoidosis. Circ. Cardiovasc. Imaging 2018, 11, e007030. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Veronese, G.; Bottiroli, M.; Wang, D.W.; Cipriani, M.; Garascia, A.; Pedrotti, P.; Adler, E.D.; Frigerio, M. Update on acute myocarditis. Trends Cardiovasc. Med. 2021, 31, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Imanaka-Yoshida, K.; Hiroe, M.; Yasutomi, Y.; Toyozaki, T.; Tsuchiya, T.; Noda, N.; Maki, T.; Nishikawa, T.; Sakakura, T.; Yoshida, T. Tenascin-C is a useful marker for disease activity in myocarditis. J. Pathol. 2002, 197, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, S.; Imanaka-Yoshida, K.; Hiramitsu, S.; Kato, S.; Ohtsuki, M.; Uemura, A.; Kato, Y.; Nishikawa, T.; Toyozaki, T.; Hishida, H. Diagnostic utility of tenascin-C for evaluation of the activity of human acute myocarditis. J. Pathol. 2005, 205, 460–467. [Google Scholar] [CrossRef]
- Fox, S.E.; Falgout, L.; Vander Heide, R.S. COVID-19 myocarditis: Quantitative analysis of the inflammatory infiltrate and a proposed mechanism. Cardiovasc. Pathol. 2021, 54, 107361. [Google Scholar] [CrossRef]
- Pasupathy, S.; Air, T.; Dreyer, R.P.; Tavella, R.; Beltrame, J.F. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation 2015, 131, 861–870. [Google Scholar] [CrossRef]
- Taghavi, S.; Chenaghlou, M.; Mirtajaddini, M.; Naderi, N.; Amin, A. Takotsubo syndrome without major stress mimicking myocarditis. Anatol. J. Cardiol. 2020, 23, 349–350. [Google Scholar] [CrossRef]
- Lasica, R.; Spasic, J.; Djukanovic, L.; Trifunovic-Zamaklar, D.; Orlic, D.; Nedeljkovic-Arsenovic, O.; Asanin, M. Case report: Acute toxic myocardial damage caused by 5-fluorouracil-from enigma to success. Front. Cardiovasc. Med. 2022, 9, 991886. [Google Scholar] [CrossRef]
- Rapezzi, C.; Arbustini, E.; Caforio, A.L.; Charron, P.; Gimeno-Blanes, J.; Heliö, T.; Linhart, A.; Mogensen, J.; Pinto, Y.; Ristic, A.; et al. Diagnostic work-up in cardiomyopathies: Bridging the gap between clinical phenotypes and final diagnosis. A position statement from the ESC Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 1448–1458. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Peretto, G.; Sala, S.; Rizzo, S.; Palmisano, A.; Esposito, A.; De Cobelli, F.; Campochiaro, C.; De Luca, G.; Foppoli, L.; Dagna, L. Ventricular Arrhythmias in Myocarditis: Characterization and Relationships with Myocardial Inflammation. J. Am. Coll. Cardiol. 2020, 75, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Mirna, M.; Schmutzler, L.; Topf, A.; Boxhammer, E.; Sipos, B.; Hoppe, U.C.; Lichtenauer, M. Treatment with Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Does Not Affect Outcome in Patients with Acute Myocarditis or Myopericarditis. J. Cardiovasc. Dev. Dis. 2022, 19, 32. [Google Scholar] [CrossRef]
- Berg, J.; Lovrinovic, M.; Baltensperger, N.; Kissel, C.K.; Kottwitz, J.; Manka, R.; Patriki, D.; Scherff, F.; Schmied, C.; Landmesser, U.; et al. Non-steroidal anti-inflammatory drug use in acute myopericarditis: 12-month clinical follow-up. Open Heart 2019, 6, e000990. [Google Scholar] [CrossRef]
- Montero, S.; Abrams, D.; Ammirati, E.; Huang, F.; Donker, D.W.; Hekimian, G.; García-García, C.; Bayes-Genis, A.; Combes, A.; Schmidt, M. Fulminant myocarditis in adults: A narrative review. J. Geriatr. Cardiol. 2022, 19, 137–151. [Google Scholar]
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. ESC Scientific Document Group. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef]
- Bang, V.; Ganatra, S.; Shah, S.P.; Dani, S.S.; Neilan, T.G.; Thavendiranathan, P.; Resnic, F.S.; Piemonte, T.C.; Barac, A.; Patel, R.; et al. Management of Patients with Giant Cell Myocarditis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2021, 77, 1122–1134. [Google Scholar] [CrossRef]
- Maury, P.; Chilon, T.; Dumonteil, N.; Fontan, A. Complete atrioventricular block persisting after regression of infectious myocarditis. J. Electrocardiol. 2008, 41, 665–667. [Google Scholar] [CrossRef]
- Pelargonio, G.; Pinnacchio, G.; Narducci, M.L.; Pieroni, M.; Perna, F.; Bencardino, G.; Comerci, G.; Dello Russo, A.; Casella, M.; Bartoletti, S.; et al. Long-Term Arrhythmic Risk Assessment in Biopsy-Proven Myocarditis. JACC Clin. Electrophysiol. 2020, 6, 574–582. [Google Scholar] [CrossRef]
- Bardy, G.H.; Lee, K.L.; Mark, D.B.; Poole, J.E.; Packer, D.L.; Boineau, R.; Domanski, M.; Troutman, C.; Anderson, J.; Johnson, G.; et al. Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. Engl. J. Med. 2005, 352, 225–237. [Google Scholar] [CrossRef]
- Pelliccia, A.; Solberg, E.E.; Papadakis, M.; Adami, P.E.; Biffi, A.; Caselli, S.; La Gerche, A.; Niebauer, J.; Pressler, A.; Schmied, C.M.; et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: Position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2019, 40, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Kühl, U.; Pauschinger, M.; Schwimmbeck, P.L.; Seeberg, B.; Lober, C.; Noutsias, M.; Poller, W.; Schultheiss, H.P. Interferon-beta treatment eliminates cardiotropic viruses and improves left ventricular function in patients with myocardial persistence of viral genomes and left ventricular dysfunction. Circulation 2003, 107, 2793–2798. [Google Scholar] [CrossRef] [PubMed]
- Abdenasser, D.; Amine, E. Rare case of subacute herpetic myocarditis. IDCases 2023, 33, e01828. [Google Scholar] [CrossRef] [PubMed]
- Deonarain, R.; Cerullo, D.; Fuse, K.; Liu, P.P.; Fish, E.N. Protective role for interferon-beta in coxsackievirus B3 infection. Circulation 2004, 110, 3540–3543. [Google Scholar] [CrossRef]
- Goland, S.; Czer, L.S.; Siegel, R.J.; Tabak, S.; Jordan, S.; Luthringer, D.; Mirocha, J.; Coleman, B.; Kass, R.M.; Trento, A. Intravenous immunoglobulin treatment for acute fulminant inflammatory cardiomyopathy: Series of six patients and review of literature. Can. J. Cardiol. 2008, 24, 571–574. [Google Scholar] [CrossRef]
- Kishimoto, C.; Shioji, K.; Hashimoto, T.; Nonogi, H.; Lee, J.D.; Kato, S.; Hiramitsu, S.; Morimoto, S.I. Therapy with immunoglobulin in patients with acute myocarditis and cardiomyopathy: Analysis of leukocyte balance. Heart Vessel. 2014, 29, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, K.; Rummler, S.; Ries, W.; Helmschrott, M.; Selbach, J.; Ernst, F.; Morath, C.; Gauly, A.; Atiye, S.; Stauss-Grabo, M.; et al. Performance, clinical effectiveness, and safety of immunoadsorption in a wide range of indications. Ther. Apher. Dial. 2022, 26, 229–241. [Google Scholar] [CrossRef]
- Zhong, Z.; Yang, Z.; Peng, Y.; Wang, L.; Yuan, X. Diagnosis and treatment of eosinophilic myocarditis. J. Transl. Autoimmun. 2021, 4, 100118. [Google Scholar] [CrossRef]
- Chowdhury, M.; Azari, B.M.; Desai, N.R.; Ahmad, T. A Novel Treatment for a Rare Cause of Cardiogenic Shock. JACC Case Rep. 2020, 22, 1461–1465. [Google Scholar] [CrossRef]
- Song, T.; Jones, D.M.; Homsi, Y. Therapeutic effect of anti-IL-5 on eosinophilic myocarditis with large pericardial effusion. BMJ Case Rep. 2017, 2017, bcr2016218992. [Google Scholar] [CrossRef] [PubMed]
- Hossein Heydari, A.; Ghaffari, S.; Khani, Z.; Heydari, S.; Eskandari, Z.; Esmaeil Heidari, M. MiR-21 and Tocilizumab interactions improve COVID-19 myocarditis outcomes. Ther. Adv. Cardiovasc. Dis. 2023, 17, 17539447231182548. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Zhu, Q.; Zhang, C.; Li, J.; Wei, M.; Qin, Y.; Chen, G.; Wang, K.; Yu, J.; Wu, Z.; et al. Tocilizumab combined with favipiravir in the treatment of COVID-19: A multicenter trial in a small sample size. Biomed. Pharmacother. 2021, 133, 110825. [Google Scholar] [CrossRef]
- Ruiz-Ortiz, M.; Anguita-Sánchez, M.; Bonilla-Palomas, J.L.; Fernández-Pérez, C.; Bernal-Sobrino, J.L.; Cequier-Fillat, A.; Bueno-Zamora, H.; Marín, F.; Elola-Somoza, F.J. Incidence and outcomes of hospital treated acute myocarditis from 2003 to 2015 in Spain. Eur. J. Clin. Investig. 2021, 51, e13444. [Google Scholar] [CrossRef] [PubMed]
- ABadrinath, A.; Bhatta, S.; Kloc, A. Persistent viral infections and their role in heart disease. Front. Microbiol. 2022, 24, 1030440. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lasica, R.; Djukanovic, L.; Savic, L.; Krljanac, G.; Zdravkovic, M.; Ristic, M.; Lasica, A.; Asanin, M.; Ristic, A. Update on Myocarditis: From Etiology and Clinical Picture to Modern Diagnostics and Methods of Treatment. Diagnostics 2023, 13, 3073. https://doi.org/10.3390/diagnostics13193073
Lasica R, Djukanovic L, Savic L, Krljanac G, Zdravkovic M, Ristic M, Lasica A, Asanin M, Ristic A. Update on Myocarditis: From Etiology and Clinical Picture to Modern Diagnostics and Methods of Treatment. Diagnostics. 2023; 13(19):3073. https://doi.org/10.3390/diagnostics13193073
Chicago/Turabian StyleLasica, Ratko, Lazar Djukanovic, Lidija Savic, Gordana Krljanac, Marija Zdravkovic, Marko Ristic, Andjelka Lasica, Milika Asanin, and Arsen Ristic. 2023. "Update on Myocarditis: From Etiology and Clinical Picture to Modern Diagnostics and Methods of Treatment" Diagnostics 13, no. 19: 3073. https://doi.org/10.3390/diagnostics13193073
APA StyleLasica, R., Djukanovic, L., Savic, L., Krljanac, G., Zdravkovic, M., Ristic, M., Lasica, A., Asanin, M., & Ristic, A. (2023). Update on Myocarditis: From Etiology and Clinical Picture to Modern Diagnostics and Methods of Treatment. Diagnostics, 13(19), 3073. https://doi.org/10.3390/diagnostics13193073







