Incidental Diagnosis of Rheumatic Myocarditis during Cardiac Surgery—Impact on Late Prognosis
Abstract
:1. Introduction
2. Methods
2.1. Aim of the Study
- Clinical manifestations of rheumatic myocarditis/valvulitis:
- Evaluation of indicative clinical manifestations such as fever, tachycardia and progressive cardiac failure.
- Monitoring the utilization of dobutamine and corticoids for management during the immediate postoperative period.
- Assessment of the efficacy of secondary prophylaxis with benzathine penicillin.
- Laboratory indicators of inflammation and infection:
- Analysis of key laboratory markers including C-reactive protein (CRP) levels.
- Measurement of erythrocyte sedimentation rate (ESR).
- Leukocytosis to assess inflammatory and/or infectious status.
- Clinical follow-up and patient’s characteristics:
- Age.
- Gender.
- Early in-hospital mortality.
- Ten-year follow-up after surgery, either through medical records or phone calls.
- Echocardiographic parameters:
- Quantification of left ventricle ejection fraction (LVEF).
- Identification of specific valvular heart disease disorders.
- Pathology:
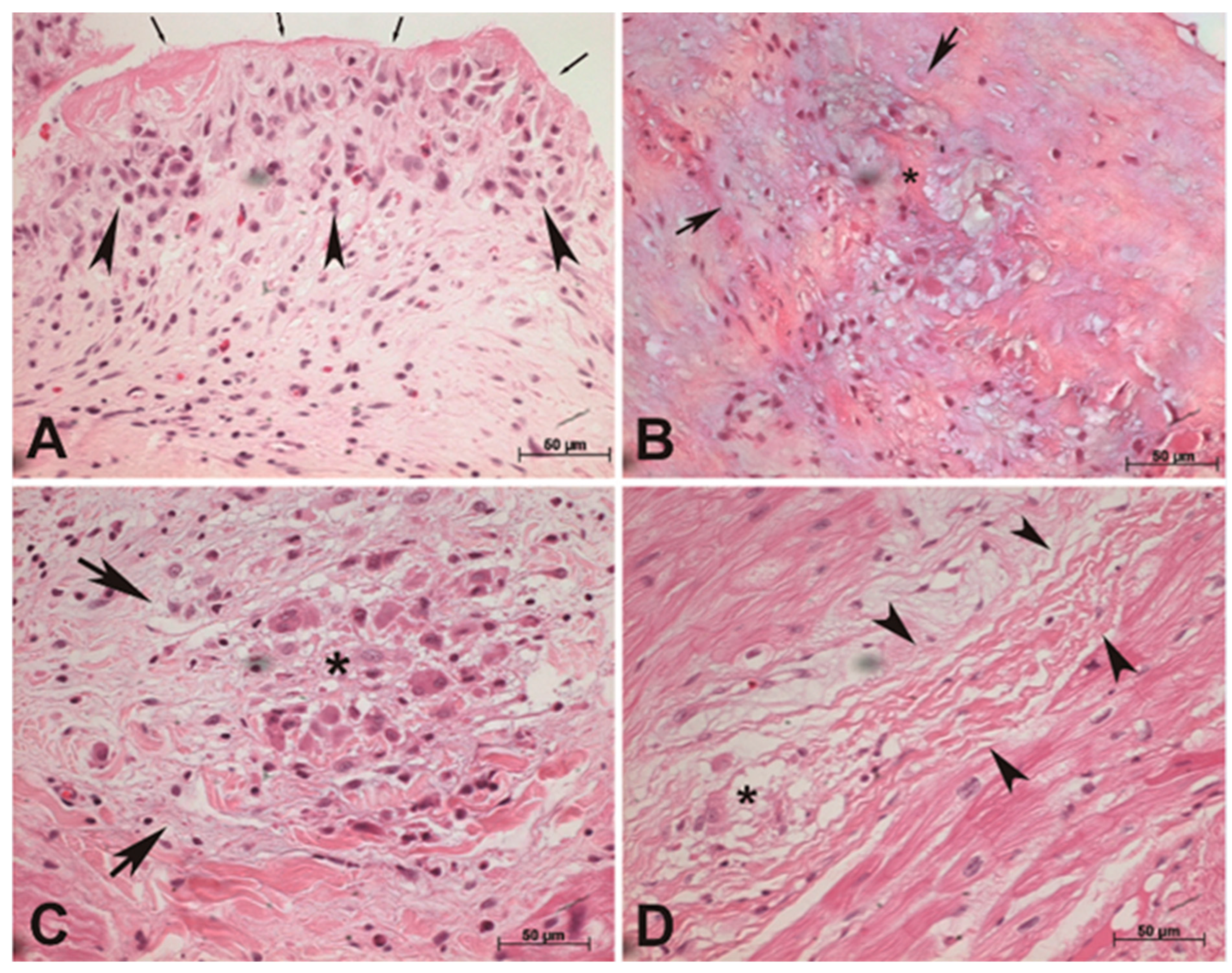
- Characterization of pathological findings encompassing the inflammatory stage.
- Identification and analysis of the presence of Aschoff bodies.
2.2. Patients
2.3. Histopathological Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sampaio, R.O.; Fae, K.C.; Demarchi, L.M.F.; Pomerantzeff, P.M.A.; Aiello, V.D.; Spina, G.S.; Tanaka, A.C.; Oshiro, S.E.; Grinberg, M.; Kalil, J.; et al. Rheumatic heart disease: 15 years of clinical and immunological follow-up. Vasc. Health Risk Manag. 2007, 3, 1007–1017. [Google Scholar] [PubMed]
- Watkins, D.A.; Johnson, C.O.; Colquhoun, S.M.; Karthikeyan, G.; Beaton, A.; Bukhman, G.; Forouzanfar, M.H.; Longenecker, C.T.; Mayosi, B.M.; Mensah, G.A.; et al. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015. N. Engl. J. Med. 2017, 377, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Ralph, A.P.; Noonan, S.; Wade, V.; Currie, B.J. The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease. Med. J. Aust. 2020, 214, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Spina, G.S.; Sampaio, R.O.; Branco, C.E.; Miranda, G.B.; Rosa, V.E.E.; Tarasoutchi, F. Incidental histological diagnosis of acute rheumatic myocarditis: Case report and review of the literature. Front. Pediatr. 2014, 2, 126. [Google Scholar] [CrossRef] [PubMed]
- Reményi, B.; Wilson, N.; Steer, A.; Ferreira, B.; Kado, J.; Kumar, K.; Lawrenson, J.; Maguire, G.; Marijon, E.; Mirabel, M.; et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease-an evidence-based guideline. Nat. Rev. Cardiol. 2012, 9, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Branco, C.E.D.B.; Sampaio, R.O.; Bracco, M.M.; Morhy, S.S.; Vieira, M.L.C.; Guilherme, L.; Rizzo, L.V.; Tarasoutch, F. Rheumatic fever: A neglected and underdiagnosed disease. New perspective on diagnosis and prevention. Arq. Bras. Cardiol. 2016, 107, 482–484. [Google Scholar] [CrossRef] [PubMed]
- Fraser, W.; Haffejee, Z.; Jankelow, D.; Wadee, A.; Cooper, K. Rheumatic Aschoff nodules revisited. II: Cytokine expression corroborates recently proposed sequential stages. Histopathology 1997, 31, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Gross, L.; Ehrlich, J.C. Studies on the Myocardial Aschoff Body: II. Life Cycle, Sites of Predilection and Relation to Clinical Course of Rheumatic Fever. Am. J. Pathol. 1934, 10, 489–504.1. [Google Scholar]
- Roberts, W.C.; Virmani, R. Aschoff bodies at necropsy in valvular heart disease. Evidence from an analysis of 543 patients over 14 years of age that rheumatic heart disease, at least anatomically, is a disease of the mitral valve. Circulation 1978, 57, 803–807. [Google Scholar] [CrossRef]
- Guilherme, L.; Kalil, J. Rheumatic Heart Disease: Molecules Involved in Valve Tissue Inflammation Leading to the Autoimmune Process and Anti-S. pyogenes Vaccine. Front. Immunol. 2013, 4, 352. [Google Scholar] [CrossRef]
- Virmani, R.; Roberts, W.C. Aschoff bodies in operatively excised atrial appendages and in papillary muscles: Frequency and clinical significance. Circulation 1977, 55, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Rosa, V.; Lopes, A.S.S.; Accorsi, T.A.D.; Fernandes, J.R.C.; Spina, G.S.; Sampaio, R.; Bacal, F.; Tarasoutchi, F. Heart Transplant in Patients with Predominantly Rheumatic Valvular Heart Disease. J. Heart Valve Dis. 2015, 24, 629–634. [Google Scholar] [PubMed]
- Kumar, R.K.; Antunes, M.J.; Beaton, A.; Mirabel, M.; Nkomo, V.T.; Okello, E.; Regmi, P.R.; Reményi, B.; Sliwa-Hähnle, K.; Zühlke, L.J.; et al. Contemporary Diagnosis and Management of Rheumatic Heart Disease: Implications for Closing the Gap A Scientific Statement From the American Heart Association. Circulation 2020, 142, E337–E357. [Google Scholar] [CrossRef] [PubMed]
- Guadalajara, J.F.; Gual, J.J.; Valvuena, N.; Vera, A.; Laplaza, I.; Salinas, L. Rheumatic carditis in the adult. Anatomoclinical correlation. Arch. Inst. Cardiol. Mex. 1990, 60, 541–546. [Google Scholar] [PubMed]
- Calegaro, J.U.; De Carvalho, A.C.; Campos, E.R.; Medeiros, M.; Gomes, E.D.F. Gallium-67 in rheumatic fever: Preliminary report. Arq. Bras. Cardiol. 1991, 56, 487–492. [Google Scholar] [PubMed]
- Cooper, L.T., Jr. Myocarditis. N. Engl. J. Med. 2018, 360, 1526–1538. [Google Scholar] [CrossRef] [PubMed]
- Younis, A.; Matetzky, S.; Mulla, W.; Masalha, E.; Afel, Y.; Chernomordik, F.; Fardman, A.; Goitein, O.; Ben-Zekry, S.; Peled, Y.; et al. Epidemiology Characteristics and Outcome of Patients With Clinically Diagnosed Acute Myocarditis. Am. J. Med. 2020, 133, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.E. Evidence that Aschoff bodies of rheumatic myocarditis develop from injured myofibers. J. Exp. Med. 1952, 95, 319–332. [Google Scholar] [CrossRef]
- Buonacera, A.; Stancanelli, B.; Colaci, M.; Malatino, L. Neutrophil to Lymphocyte Ratio: An Emerging Marker of the Relationships between the Immune System and Diseases. Int. J. Mol. Sci. 2022, 23, 3636. [Google Scholar] [CrossRef]
- Regolo, M.; Sorce, A.; Vaccaro, M.; Colaci, M.; Stancanelli, B.; Natoli, G.; Motta, M.; Isaia, I.; Castelletti, F.; Giangreco, F.; et al. Assessing Humoral Immuno-Inflammatory Pathways Associated with Respiratory Failure in COVID-19 Patients. J. Clin. Med. 2023, 12, 4057. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef]
- Ferri, C.; Raimondo, V.; Gragnani, L.; Giuggioli, D.; Dagna, L.; Tavoni, A.; Ursini, F.; L’Andolina, M.; Caso, F.; Ruscitti, P.; et al. Prevalence and Death Rate of COVID-19 in Autoimmune Systemic Diseases in the First Three Pandemic Waves. Relationship with Disease Subgroups and Ongoing Therapies. Curr. Pharm. Des. 2022, 28, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
- Javadi, H.; Jallalat, S.; Pourbehi, G.; Semnani, S.; Mogharrabi, M.; Nabipour, I.; Ravanbod, M.; Amini, A.; Assadi, M. The role of gated myocardial perfusion scintigraphy (GMPS) in myocarditis: A case report and review of the literature. Nucl. Med. Rev. Cent. East. Eur. 2011, 14, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aty, H.; Boyé, P.; Zagrosek, A.; Wassmuth, R.; Kumar, A.; Messroghli, D.; Bock, P.; Dietz, R.; Friedrich, M.G.; Schulz-Menger, J. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: Comparison of different approaches. J. Am. Coll. Cardiol. 2005, 45, 1815–1822. [Google Scholar] [CrossRef] [PubMed]
- Reina-Couto, M.; Pereira-Terra, P.; Quelhas-Santos, J.; Silva-Pereira, C.; Albino-Teixeira, A.; Sousa, T. Inflammation in Human Heart Failure: Major Mediators and Therapeutic Targets. Front. Physiol. 2021, 12, 746494. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, R.; Sood, A. Clinical Profile of Acute Rheumatic Fever Patients in a Tertiary Care Institute in Present Era. J. Assoc. Physicians India 2015, 63, 22–24. [Google Scholar] [PubMed]
- Gözü Pirinççioğlu, A.; Alyan, O.; Kanğın, M.; Taşkesen, M.; Fidan, M.; Mermutoğlu, N.; Sen, V.; Ali Tas, M. A retrospective investigation of clinical and laboratory findings in children with acute rheumatic fever, reactivation and compliance with prophylaxis. Turk. Kardiyol. Dern. Ars. 2012, 40, 427–435. [Google Scholar] [CrossRef]
- Lue, H.C.; Wu, M.H.; Wang, J.K.; Wu, F.F.; Wu, Y.N. Three- versus four-week administration of benzathine penicillin G: Effects on incidence of streptococcal infections and recurrences of rheumatic fever. Pediatrics 1996, 97 Pt 2, 984–988. [Google Scholar] [CrossRef]
- Sheikh, A.M.; Sadiq, M.; Rehman, A.U. Changing Clinical Profile of Acute Rheumatic Fever and Rheumatic Recurrence. J. Ayub Med. Coll. Abbottabad. 2016, 28, 141–145. [Google Scholar] [PubMed]
- Marijon, E.; Ou, P.; Celermajer, D.S.; Ferreira, B.; Mocumbi, A.O.; Jani, D.; Paquet, C.; Jacob, S.; Sidi, D.; Jouven, X. Prevalence of Rheumatic Heart Disease Detected by Echocardiographic Screening. N. Engl. J. Med. 2007, 357, 470–476. [Google Scholar] [CrossRef]
- Brown, A.; Mcdonald, M.I.; Calma, T. Rheumatic fever and social justice. Med. J. Aust. 2007, 186, 557–558. [Google Scholar] [CrossRef]
- Costa, L.P.; Domiciano, D.S.; Maria, R.; Pereira, R. Fever in Brazil: Systematic review. Rev. Bras. Reumatol. 2009, 49, 617–622. [Google Scholar] [CrossRef]
| Baseline Characteristics | n = 118 | ABG (n = 73) | NABG (n = 45) | p |
|---|---|---|---|---|
| Age in years | 23 (13–35) | 27 (17–37) | 13 (11–24) | 0.001 |
| More than 40 years % | 18.6 | 22.9 | 10.5 | 0.188 |
| Female sex % | 61 | 63.5 | 56.8 | 0.599 |
| Penicillin prophylaxis % | 85 | 74.2 | 91.4 | 0.072 |
| Aschoff bodies % | 61.8 | 100 | 0 | 0.0001 |
| Elective surgery % | 81.4 | 89.9 | 67.7 | 0.015 |
| Tachycardia % | 39 | 30.4 | 53.1 | 0.049 |
| High levels of CRP or ESR % | 27.5 | 31.7 | 20.8 | 0.093 |
| Leukocytosis % | 27.1 | 18.3 | 41.7 | 0.093 |
| Increase in PR interval % | 13 | 11.5 | 15.4 | 1 |
| Signs of cardiac failure % | 61 | 71.2 | 78.8 | 0.572 |
| LVEF < 50% | 9.3 | 13.5 | 2.3 | 0.006 |
| ● Mitral valve % | 62.2 | 55.3 | 73.5 | 0.293 |
| ● Aortic valve % | 6.9 | 12.4 | 8.8 | 0.293 |
| ● Combined mitral + aortic valves % | 26 | 31.3 | 17.6 | 0.293 |
| Pathology and Follow-Up Data | ABG (n = 73) | NABG (n = 45) | p |
|---|---|---|---|
| Hospitalization days | 17 (14–29) | 24 (15–35) | 0.074 |
| ● Aortic valve % | 8.2 | 15 | 0.011 |
| ● Aortic + mitral valve % | 4.1 | 22.5 | 0.011 |
| ● Mitral valve % | 53.4 | 50 | 0.011 |
| ● Myocardium % | 26 | 12.5 | 0.011 |
| ● Myocardium + mitral Valve % | 5.5 | 0 | 0.011 |
| ŦProliferative % | 50.7 | 0 | 0.296 |
| ŦExudative % | 8.2 | 0 | 0.296 |
| ŦCicatricial % | 11 | 100 | 0.296 |
| ŦGranulomatous % | 4.1 | 0 | 0.296 |
| ŦVerruca % | 9.6 | 0 | 0.296 |
| ŦProliferative + exudative % | 8.2 | 0 | 0.296 |
| ŦProliferative + verruca % | 5.5 | 0 | 0.296 |
| ŦProliferative + cicatricial % | 2.7 | 0 | 0.296 |
| In-hospital mortality % | 3 | 0 | 0.532 |
| Post-Procedure | ABG (n = 73) | NABG (n = 45) | p |
|---|---|---|---|
| High levels of CRP or ERS % | 36.2 | 14.3 | 0.211 |
| Leukocytosis % | 14.9 | 28.6 | 0.211 |
| Fever % | 26.9 | 29.4 | 0.972 |
| Corticosteroids % | 50 | 38.2 | 0.368 |
| Dobutamine % | 67.2 | 64.7 | 0.981 |
| Heart surgery % | 58.7 | 68.2 | 0.597 |
| 10-Year follow-up mortality % | 22.9 | 5,4 | 0.043 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vieira, P.P.A.C.; Pereira, R.F.; Branco, C.E.B.; Rosa, V.E.E.; Vieira, M.L.C.; Demarchi, L.M.M.F.; Silva, L.S.; Guilherme, L.; Tarasoutchi, F.; Sampaio, R.O. Incidental Diagnosis of Rheumatic Myocarditis during Cardiac Surgery—Impact on Late Prognosis. Diagnostics 2023, 13, 3252. https://doi.org/10.3390/diagnostics13203252
Vieira PPAC, Pereira RF, Branco CEB, Rosa VEE, Vieira MLC, Demarchi LMMF, Silva LS, Guilherme L, Tarasoutchi F, Sampaio RO. Incidental Diagnosis of Rheumatic Myocarditis during Cardiac Surgery—Impact on Late Prognosis. Diagnostics. 2023; 13(20):3252. https://doi.org/10.3390/diagnostics13203252
Chicago/Turabian StyleVieira, Paulo Pinto Alves Campos, Rodrigo Furtado Pereira, Carlos Eduardo Barros Branco, Vitor Emer Egypto Rosa, Marcelo Luiz Campos Vieira, Lea Maria Macruz Ferreira Demarchi, Livia Santos Silva, Luiza Guilherme, Flavio Tarasoutchi, and Roney Orismar Sampaio. 2023. "Incidental Diagnosis of Rheumatic Myocarditis during Cardiac Surgery—Impact on Late Prognosis" Diagnostics 13, no. 20: 3252. https://doi.org/10.3390/diagnostics13203252
APA StyleVieira, P. P. A. C., Pereira, R. F., Branco, C. E. B., Rosa, V. E. E., Vieira, M. L. C., Demarchi, L. M. M. F., Silva, L. S., Guilherme, L., Tarasoutchi, F., & Sampaio, R. O. (2023). Incidental Diagnosis of Rheumatic Myocarditis during Cardiac Surgery—Impact on Late Prognosis. Diagnostics, 13(20), 3252. https://doi.org/10.3390/diagnostics13203252






