Inter- and Intra-Examiner Reliability Study of Two-Point Discrimination Test (TPD) and Two-Point Estimation Task (TPE) in the Sacral Area of Pain-Free Individuals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Examiners
2.3. Measurement Tools
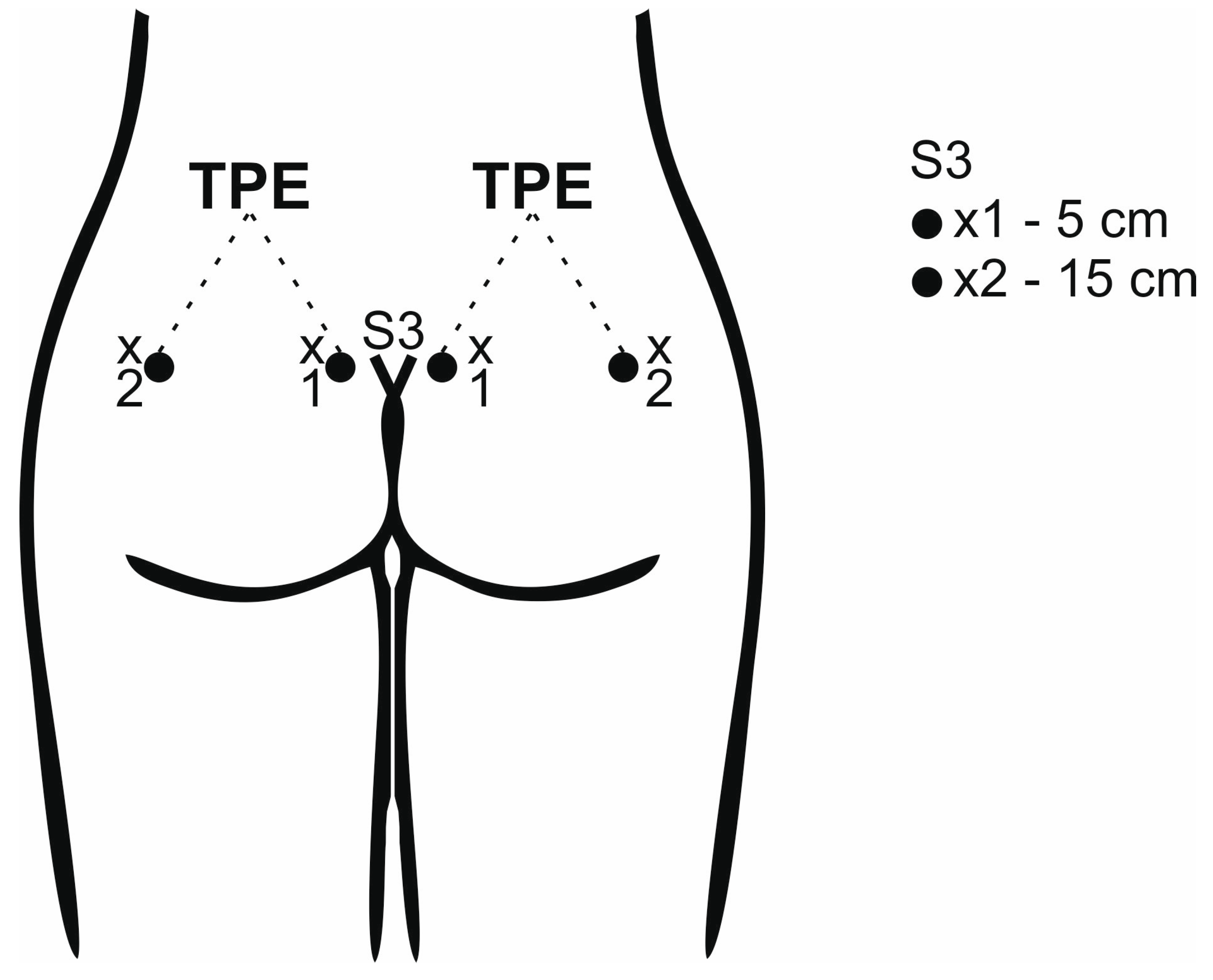
2.4. Position and Measurement Site
2.5. Randomisation
2.6. TPD Test Performance
2.7. TPE Test Performance
2.8. Statistical Analysis
3. Results
3.1. Reliability of Two-Point Discrimination (TPD) Test—One Examiner
3.2. Reliability of Two-Point Discrimination (TPD) Test—Two Examiners
3.3. Reliability of Two-Point Estimation (TPE) Test—One Examiner
3.4. Reliability of Two-Point Estimation (TPE) Test—Two Examiners
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moseley, G.L. I can’t find it! Distorted body image and tactile dysfunction in patients with chronic back pain. Pain 2008, 140, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Luomajoki, H.; Moseley, G.L. Tactile acuity and lumbopelvic motor control in patients with back pain and healthy controls. Br. J. Sports Med. 2011, 45, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.S.; Schweinhardt, P. Perceptions of the painful body: The relationship between body perception disturbance, pain and tactile discrimination in complex regional pain syndrome. Eur. J. Pain 2012, 16, 1320–1330. [Google Scholar] [CrossRef]
- Stanton, T.R.; Lin, C.W.C.; Bray, H.; Smeets, R.J.E.M.; Taylor, D.; Law, R.Y.W.; Moseley, G.L. Tactile acuity is disrupted in osteoarthritis but is unrelated to disruptions in motor imagery performance. Rheumatology 2013, 52, 1509–1519. [Google Scholar] [CrossRef]
- Catley, M.J.; O’Connell, N.E.; Berryman, C.; Ayhan, F.F.; Moseley, G.L. Is tactile acuity altered in people with chronic pain? a systematic review and meta-analysis. J. Pain 2014, 15, 985–1000. [Google Scholar] [CrossRef]
- Harvie, D.S.; Edmond-Hank, G.; Smith, A.D. Tactile acuity is reduced in people with chronic neck pain. Musculoskelet. Sci. Pract. 2017, 33, 61–66. [Google Scholar] [CrossRef]
- Fonseca, M.C.R.; Elui, V.M.C.; Lalone, E.; da Silva, N.C.; Barbosa, R.I.; Marcolino, A.M.; Ricci, F.P.F.M.; MacDermid, J.C. Functional, motor, and sensory assessment instruments upon nerve repair in adult hands: Systematic review of psychometric properties. Syst. Rev. 2018, 7, 175. [Google Scholar] [CrossRef] [PubMed]
- Wolny, T.; Linek, P. Reliability of two-point discrimination test in carpal tunnel syndrome patients. Physiother. Theory Pract. 2019, 35, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk, W.M.; Luedtke, K.; Saulicz, E. Lumbar Tactile Acuity in Patients With Low Back Pain and Healthy Controls: Systematic Review and Meta-Analysis. Clin. J. Pain 2018, 34, 82–94. [Google Scholar] [CrossRef]
- Morf, R.; Pfeifer, F.; Hotz-Boendermaker, S.; Meichtry, A.; Luomajoki, H. Prediction and trend of tactile acuity, pain and disability in acute LBP: A six-month prospective cohort study. BMC Musculoskelet. Disord. 2021, 22, 666. [Google Scholar] [CrossRef]
- Adamczyk, W.M.; Saulicz, O.; Saulicz, E.; Luedtke, K. Tactile acuity (dys)function in acute nociceptive low back pain: A double-blind experiment. Pain 2018, 159, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk, W.M.; Sługocka, A.; Saulicz, O.; Saulicz, E. The point-to-point test: A new diagnostic tool for measuring lumbar tactile acuity? Inter and intra-examiner reliability study of pain-free subjects. Man. Ther. 2016, 22, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Ehrenbrusthoff, K.; Ryan, C.G.; Grüneberg, C.; Martin, D.J. A systematic review and meta-analysis of the reliability and validity of sensorimotor measurement instruments in people with chronic low back pain. Musculoskelet. Sci. Pract. 2018, 35, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk, W.M.; Luedtke, K.; Saulicz, O.; Saulicz, E. Sensory dissociation in chronic low back pain: Two case reports. Physiother Theory Pract. 2018, 34, 643–651. [Google Scholar] [CrossRef]
- Wang, J.; Zheng, K.; Wu, J.; Wang, R.; Zhuang, X. Correlations between Age, Pain Intensity, Disability, and Tactile Acuity in Patients with Chronic Low Back Pain. Pain Res. Manag. 2022, 25, 2907009. [Google Scholar] [CrossRef]
- Adamczyk, W.M.; Sługocka, A.; Mehlich, K.; Saulicz, E.; Luedtke, K. Preliminary validation of two-point estimation task for the measurement of sensory dissociation in patients with chronic low back pain. Pain Med. 2019, 20, 2472–2478. [Google Scholar] [CrossRef]
- Vleeming, A.; Albert, H.; Östgaard, H.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819. [Google Scholar] [CrossRef]
- Palsson, T.S.; Gibson, W.; Darlow, B.; Bunzli, S.; Lehman, G.; Rabey, M.; Moloney, N.; Vaegter, H.B.; Bagg, M.K.; Travers, M. Changing the narrative in diagnosis and management of pain in the sacroiliac joint area. Phys. Ther. 2019, 99, 1511–1519. [Google Scholar] [CrossRef]
- Schenker, A.; Schiltenwolf, M.; Schwarze, M.; Pepke, W.; Hemmer, S.; Akbar, M. Schmerzquelle Illiosakralgelenk. Funktionelle Anatomie, Symptome und klinische Bedeutung. Der Orthopäde 2020, 49, 1000–1005. [Google Scholar] [CrossRef]
- Dufour, S.; Vandyken, B.; Forget, M.-J.; Vandyken, C. Association between lumbopelvic pain and pelvic floor dysfunction in women: A cross sectional study. Musculoskelet. Sci. Pract. 2018, 34, 47–53. [Google Scholar] [CrossRef]
- Park, J.W.; Lee, Y.-K.; Lee, J.; Shin, S.; Kang, Y.; Koo, K.-H. Deep gluteal syndrome as a cause of posterior hip pain and sciatica-like pain. Bone Jt. J. 2020, 102, 556–567. [Google Scholar] [CrossRef] [PubMed]
- Possover, M.; Forman, A. Voiding Dysfunction Associated with Pudendal Nerve Entrapment. Curr. Bladder Dysfunct. Rep. 2012, 7, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Ghizzani, A.; Carta, S.; Casoni, A.; Ferrata, P.; Luisi, S.; Fortina, M. Differentiating overlapping symptoms of vulvodynia and pudendal neuralgia. Br. J. Pain 2019, 13, 54–58. [Google Scholar] [CrossRef]
- Liyew, W.A. Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions. Int. J. Rheumatol. 2020, 2020, 2919625. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, J.W.; Frost, C. Reliability, repeatability and reproducibility: Analysis of measurement errors in continuous variables. Ultrasound Obstet. Gynecol. 2008, 31, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Catley, M.J.; Tabor, A.; Wand, B.M.; Moseley, G.L. Assessing tactile acuity in rheumatology and musculoskeletal medicine how reliable are two-point discrimination tests at the neck, hand, back and foot? Rheumatology 2013, 52, 1454–1461. [Google Scholar] [CrossRef]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar]
- Wang, J.; Chen, C.; Peng, M.; Wang, Y.; Wu, B.; Zheng, Y.; Wang, X. Intra- and inter-rater reliability of three measurements for assessing tactil acuity in individuals with chronic low back pain. Evid.-Based Complement. Altern. Med. 2020, 2020, 8367095. [Google Scholar] [CrossRef]
- Karnath, H.O.; Schenkel, P.; Fischer, B. Trunk orientation as the determining factor of the “contralateral” deficit in the neglect syndrome and as the physical anchor of the internal representation of body orientation in space. Brain 1991, 114, 1997–2014. [Google Scholar] [CrossRef]
- Beschin, N.; Cubelli, R.; Della Salla, S.; Spinazzola, L. Left of what? The role of egocentric coordinates in neglect. J. Neurol. Neurosurg. Psychiatry 1997, 63, 483–489. [Google Scholar] [CrossRef][Green Version]
- Cholewiak, R.W.; Brill, J.C.; Schwab, A. Vibrotactile localization on the abdomen: Effects of place and space. Percept. Psychophys. 2004, 66, 970–987. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Mawla, I.; Lee, J.; Gerbera, J.; Walker, K.; Kim, J.; Ortiza, A.; Chana, S.; Loggia, M.L.; Wasan, A.D.; et al. Reduced tactile acuity in chronic low back pain is linked with structural neuroplasticity in primary somatosensory cortex and is modulated by acupuncture therapy. Neuroimage 2020, 217, 116899. [Google Scholar] [CrossRef] [PubMed]
- Flor, H.; Elbert, T.; Knecht, S.; Wienbruch, C.; Pantev, C.; Birbaumer, N.; Taub, E. Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature 1995, 375, 482–484. [Google Scholar] [CrossRef] [PubMed]
- Flor, H.; Braun, C.; Elbert, T.; Birbaumer, N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci. Lett. 1997, 224, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Wilcke, T.; Leinisch, E.; Gänssbauer SDraganski, B.; Bogdahn, U.; May, A. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain 2006, 125, 89–97. [Google Scholar] [CrossRef]
- Wand, B.M.; Parkitny, L.; O’Connell, N.E.; Luomajoki, H.; McAuley, J.H.; Thacker, M.; Moseley, G.L. Cortical changes in chronic low back pain: Current state of the art and implications for clinical practice. Man. Ther. 2011, 16, 15–20. [Google Scholar] [CrossRef]
- Kregel, J.; Meeus, M.; Malfliet, A.; Dolphens, M.; Danneels, L.; Nijs, J.; Cagnie, B. Structural and functional brain abnormalities in chronic low back pain: A systematic review. Semin. Arthritis Rheum. 2015, 45, 229–237. [Google Scholar] [CrossRef]
- Beales, D.; Lutz, A.; Thompson, J.; Wand, B.M.; O’Sullivan, P. Disturbed body perception, reduced sleep, and kinesiophobia in subjects with pregnancy-related persistent lumbopelvic pain and moderate levels of disability: An exploratory study. Man. Ther. 2016, 21, 69–75. [Google Scholar] [CrossRef]
- Wand, B.M.; James, M.; Abbaszadeh, S.; George, P.J.; Formby, P.M.; Smith, A.J.; O’Connell, N.E. Assessing self-perception in patients with chronic low back pain: Development of a back-specific body perception questionnaire. J. Back Musculoskelet. Rehabil. 2014, 27, 463–473. [Google Scholar] [CrossRef]
- Nishigami, T.; Mibu, A.; Osumi, M.; Son, K.; Yamamoto, S.; Kajiwara STanaka KMatsuya, A.; Tanabe, A. Are tactile acuity and clinical symptoms related to differences in perceived body image in patients with chronic nonspecific lower back pain? Man. Ther. 2015, 20, 63–67. [Google Scholar] [CrossRef]
- Wand, B.M.; Catley, M.J.; Rabey, M.I.; O’Sullivan, P.B.; O’Connell, N.E.; Smith, A.J. Disrupted Self-Perception in People with Chronic Low Back Pain. Further Evaluation of the Fremantle Back Awareness Questionnaire. J. Pain 2016, 17, 1001–1012. [Google Scholar] [CrossRef]
- Moseley, G.L.; Flor, H. Targeting cortical representations in the treatment of chronic pain: A review. Neurorehabilit. Neural Repair 2012, 26, 646–652. [Google Scholar] [CrossRef]
- Flor, H.; Denke, C.; Schaefer, M.; Grüsser, S. Effect of sensory discrimination training on cortical reorganisation and phantom limb pain. Lancet 2001, 357, 1763–1764. [Google Scholar] [CrossRef]
- Moseley, G.L.; Zalucki, N.M.; Wiech, K. Tactile discrimination, but not tactile stimulation alone, reduces chronic limb pain. Pain 2008, 137, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Moseley, L.G.; Wiech, K. The efect of tactile discrimination training is enhanced when patients watch the refected image of their unafected limb during training. Pain 2009, 144, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Wand, B.M.; O’Connell, N.E.; Di Pietro, F.; Bulsara, M. Managing chronic nonspecific low back pain with a sensorimotor retraining approach: Exploratory multiple-baseline study of 3 participants. Phys. Ther. 2011, 91, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Kälin, S.; Rausch-Osthoff, A.K.; Bauer, C.M. What is the effect of sensory discrimination training on chronic low back pain? A systematic review. BMC Musculoskelet. Disord. 2016, 17, 143. [Google Scholar] [CrossRef]
- Wand, B.M.; Abbaszadeh, S.; Smith, A.J.; Catley, M.J.; Moseley, G.L. 2013 Acupuncture applied as a sensory discrimination training tool decreases movement-related pain in patients with chronic low back pain more than acupuncture alone: A randomised cross-over experiment. Br. J. Sports Med. 2013, 47, 1085–1089. [Google Scholar] [CrossRef]
- Barbosa, M.B.; Montebelo, M.I.L.; Guirro, E.C.O. Determination of sensory perception and motor response thresholds in different phases of the menstrual cycle. Rev. Bras. Fisioter. 2007, 11, 443–449. [Google Scholar] [CrossRef]
- Barbosa, M.B.; Guirro, E.C.; Nunes, F.R. Evaluation of sensitivity, motor and pain thresholds across the menstrual cycle through medium-frequency transcutaneous electrical nerve stimulation. Clinics 2013, 68, 901–908. [Google Scholar] [CrossRef]

| Examiner | Measurement | TPD [5 cm] | TPD [15 cm] | TPE | |||
|---|---|---|---|---|---|---|---|
| Right (mm) | Left (mm) | Right (mm) | Left (mm) | Right (mm) | Left (mm) | ||
| 1 | 45.1 (9.2) 41.7–48.5 | 46.8 (9.2) 43.3–49.9 | 60.1 (13.4) 55.1–65.1 | 58.6 (14.1) 53.4–63.9 | 71.3 (25.2) 61.9–80.7 | 72.8 (25.8) 63.2–82.5 | |
| A [session 1] | 2 | 44.9 (8.8) 41.6–48.2 | 46.1 (10.2) 42.3–49.9 | 59.2 (12.1) 54.6–63.7 | 58.5 (12.1) 53.9–63.0 | 73.8 (23.3) 65.1–82.4 | 74.9 (22.1) 66.6–83.1 |
| 3 | 45.5 (9.1) 42.1–48.9 | 46.1 (9.7) 42.5–49.8 | 59.4 (13.6) 54.4–64.5 | 58.8 (11.7) 54.4–63.2 | 76.2 (25.2) 66.8–85.6 | 74.7 (24.5) 65.6–83.9 | |
| 1 | 45.1 (10.3) 41.2–48.9 | 50.6 (9.7) 46.9–54.2 | 63.5 (15.4) 57.8–69.3 | 64.5 (13.4) 59.5–69.5 | 71.3 (24.1) 62.3–80.3 | 73.3 (24.7) 64.0–82.5 | |
| B [session 1] | 2 | 47.7 (10.9) 43.6–51.8 | 49.4 (10.3) 45.6–53.3 | 63.2 (14.6) 57.8–68.7 | 64.6 (11.7) 60.2–68.7 | 73.8 (26.3) 64.0–83.7 | 73.6 (22.9) 65.0–82.1 |
| 3 | 46.6 (11.1) 42.4–50.7 | 50.6 (9.7) 47.0–54.3 | 63.1 (13.9) 57.9–68.2 | 62.4 (13.4) 57.4–67.5 | 75.3 (25.5) 65.8–84.8 | 73.6 (23.7) 64.8–82.5 | |
| 1 | 46.7 (9.1) 43.3–50.1 | 48.9 (8.3) 45.8–51.9 | 60.4 (10.6) 56.4–64.3 | 59.9 (12.0) 55.4–64.4 | 78.8 (25.1) 69.4–88.2 | 80.5 (27.0) 70.4–90.6 | |
| A [session 2] | 2 | 47.2 (8.9) 43.9–50.5 | 48.4 (9.1) 44.9–51.8 | 61.0 (10.6) 57.1–64.9 | 59.4 (12.5) 54.7–64.0 | 78.3 (25.1) 68.9–87.7 | 79.8 (26.7) 69.8–89.8 |
| 3 | 47.4 (8.3) 44.3–50.5 | 48.9 (8.5) 45.8–52.1 | 60.2 (10.0) 56.4–63.9 | 59.7 (12.0) 55.2–64.2 | 79.0 (25.0) 69.7–88.3 | 78.4 (25.1) 69.0–87.8 | |
| 1 | 48.6 (7.4) 45.8–51.3 | 50.6 (8.3) 47.5–53.7 | 62.7 (9.2) 59.2–66.1 | 59.4 (9.5) 55.9–63.0 | 79.7 (27.2) 69.5–89.8 | 81.2 (29.5) 70.2–92.2 | |
| A [session 2] | 2 | 49.1 (7.9) 46.1–52.0 | 50.2 (7.5) 47.4–53.0 | 59.9 (9.3) 56.4–63.4 | 61.7 (10.3) 57.8–65.5 | 81.9 (27.5) 71.6–92.1 | 81.6 (28.1) 71.1–92.0 |
| 3 | 48.8 (8.0) 45.8–51.8 | 49.8 (7.7) 46.9–52.7 | 60.0 (9.1) 56.7–63.4 | 61.3 (10.1) 57.6–65.1 | 81.6 (28.1) 71.1–92.1 | 81.9 (27.8) 71.5–92.3 | |
| Side | Measurement | Distance | ICC3.1 (95% CI) | SEM | ICC3.2 (95% CI) | SEM | ICC3.3 (95% CI) | SEM |
|---|---|---|---|---|---|---|---|---|
| direct | 5 cm | 0.67 (0.42–0.83) | 0.5 | 0.76 (0.55–0.88) | 0.33 | 0.8 (0.63–0.90) | 0.27 | |
| 15 cm | 0.59 (0.30–0.78) | 0.41 | 0.74 (0.51–0.86) | 0.35 | 0.76 (0.56–0.88) | 0.35 | ||
| Right | late | 5 cm | 0.61 (0.33–0.80) | 0.21 | 0.75 (0.54–0.87) | 0.32 | 0.75 (0.54–0.87) | 0.25 |
| 15 cm | 0.67 (0.42–0.83) | 0.33 | 0.69 (0.44–0.84) | 0.02 | 0.68 (0.42–0.83) | 0.004 | ||
| direct | 5 cm | 0.74 (0.52–0.87) | 0.003 | 0.8 (0.62–0.90) | 0.01 | 0.82 (0.65–0.91) | 0.04 | |
| Left | 15 cm | 0.78 (0.60–0.89) | 0.41 | 0.86 (0.74–0.93) | 0.33 | 0.92 (0.83–0.96) | 0.22 | |
| late | 5 cm | 0.63 (0.36–0.81) | 0.17 | 0.71 (0.47–0.85) | 0.06 | 0.71 (0.48–0.85) | 0.11 | |
| 15 cm | 0.76 (0.56–0.88) | 0.28 | 0.78 (0.58–0.89) | 0.005 | 0.77 (0.58–0.89) | 0.06 |
| Side | Distance | ICC2.1 (95% CI) | SEM | ICC2.2 (95% CI) | SEM | ICC2.3 (95% CI) | SEM |
|---|---|---|---|---|---|---|---|
| 5 cm | 0.71 (0.47–0.85) | 0.26 | 0.85 (0.71–0.92) | 0.34 | 0.86 (0.73–0.93) | 0.38 | |
| Right | 15 cm | 0.79 (0.61–0.89) | 0.27 | 0.84 (0.70–0.92) | 0.23 | 0.85 (0.70–0.93) | 0.16 |
| 5 cm | 0.6 (0.32–0.79) | 0.19 | 0.79 (0.60–0.89) | 0.13 | 0.82 (0.63–0.91) | 0.17 | |
| Left | 15 cm | 0.77 (0.57–0.88) | 0.04 | 0.78 (0.58–0.89) | 0.02 | 0.81 (0.63–0.91) | 0.08 |
| Side | Measurement | ICC3.1 (95% CI) | SEM | ICC3.2 (95% CI) | SEM | ICC3.3 (95% CI) | SEM |
|---|---|---|---|---|---|---|---|
| direct | 0.83 (0.68–0.92) | 0.82 | 0.88 (0.77–0.94) | 0.69 | 0.88 (0.77–0.94) | 0.75 | |
| Right | late | 0.69 (0.44–0.84) | 0.95 | 0.72 (0.49–0.86) | 0.51 | 0.75 (0.54–0.87) | 0.51 |
| direct | 0.88 (0.77–0.94) | 0.85 | 0.92 (0.84–0.96) | 0.58 | 0.94 (0.87–0.97) | 0.49 | |
| Left | late | 0.59 (0.29–0.78) | 1.04 | 0.65 (0.39–0.82) | 0.22 | 0.73 (0.51–0.86) | 0.17 |
| Side | ICC2.1 (95% CI) | SEM | ICC2.2 (95% CI) | SEM | ICC2.3 (95% CI) | SEM |
|---|---|---|---|---|---|---|
| Right | 0.86 (0.73–0.93) | 0.78 | 0.85 (0.73–0.93) | 0.83 | 0.87 (0.74–0.94) | 0.8 |
| Left | 0.85 (0.71–0.93) | 1.41 | 0.86 (0.73–0.93) | 1.14 | 0.89 (0.79–0.95) | 0.84 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saulicz, E.; Saulicz, O.; Koterba, J.; Sikora, D.; Saulicz, A.; Saulicz, M. Inter- and Intra-Examiner Reliability Study of Two-Point Discrimination Test (TPD) and Two-Point Estimation Task (TPE) in the Sacral Area of Pain-Free Individuals. Diagnostics 2023, 13, 3438. https://doi.org/10.3390/diagnostics13223438
Saulicz E, Saulicz O, Koterba J, Sikora D, Saulicz A, Saulicz M. Inter- and Intra-Examiner Reliability Study of Two-Point Discrimination Test (TPD) and Two-Point Estimation Task (TPE) in the Sacral Area of Pain-Free Individuals. Diagnostics. 2023; 13(22):3438. https://doi.org/10.3390/diagnostics13223438
Chicago/Turabian StyleSaulicz, Edward, Oskar Saulicz, Jakub Koterba, Damian Sikora, Aleksandra Saulicz, and Mariola Saulicz. 2023. "Inter- and Intra-Examiner Reliability Study of Two-Point Discrimination Test (TPD) and Two-Point Estimation Task (TPE) in the Sacral Area of Pain-Free Individuals" Diagnostics 13, no. 22: 3438. https://doi.org/10.3390/diagnostics13223438
APA StyleSaulicz, E., Saulicz, O., Koterba, J., Sikora, D., Saulicz, A., & Saulicz, M. (2023). Inter- and Intra-Examiner Reliability Study of Two-Point Discrimination Test (TPD) and Two-Point Estimation Task (TPE) in the Sacral Area of Pain-Free Individuals. Diagnostics, 13(22), 3438. https://doi.org/10.3390/diagnostics13223438






