Assessment of Sudden Cardiac Death Risk in Pediatric Primary Electrical Disorders: A Comprehensive Overview
Abstract
:1. Introduction
2. Brugada Syndrome
3. Catecholaminergic Polymorphic Ventricular Tachycardia
4. Idiopathic Ventricular Fibrillation
5. Long QT Syndrome
6. Andersen–Tawil Syndrome
7. Short QT Syndrome
8. Early Repolarization Syndrome
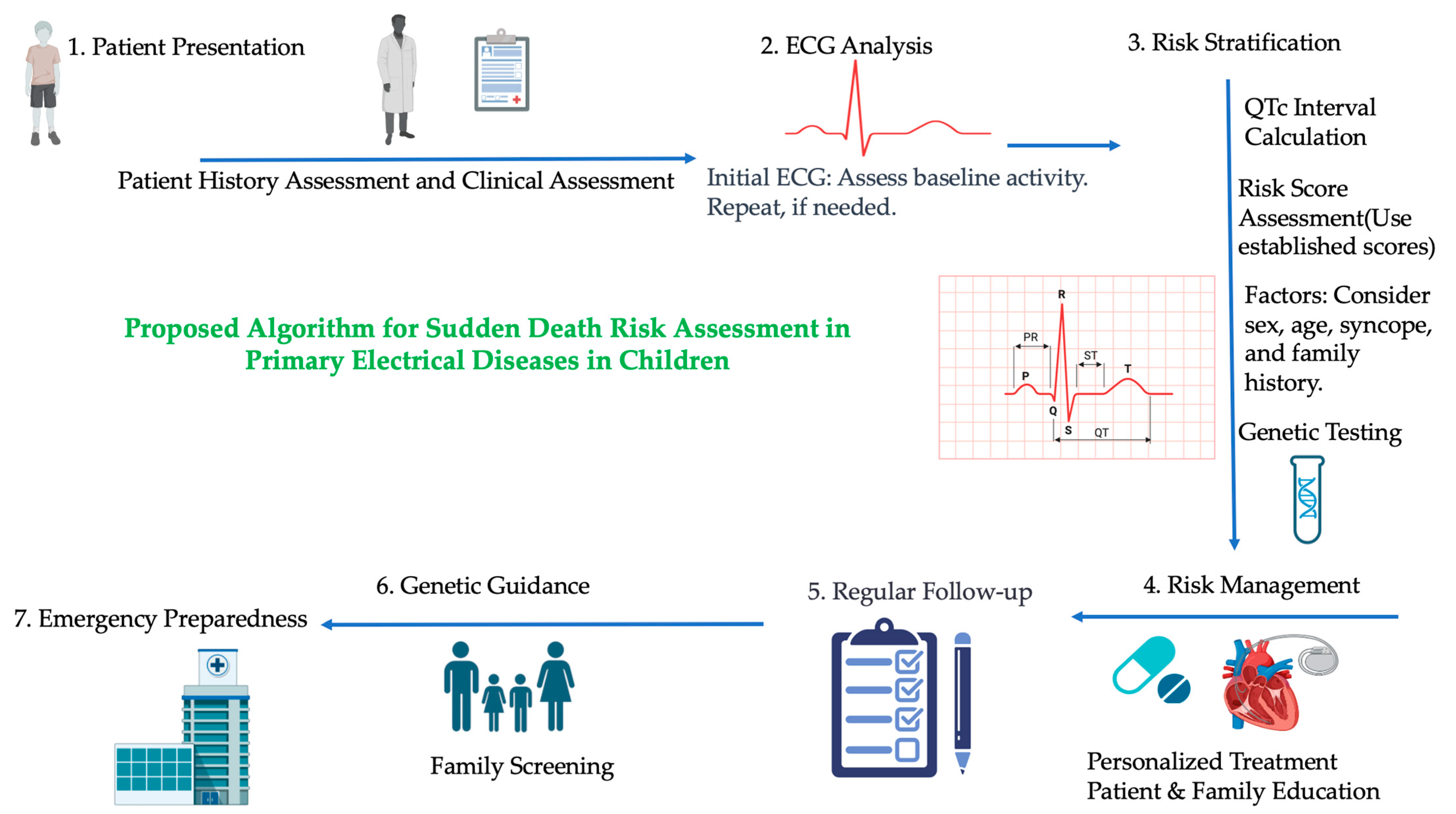
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giudicessi, J.R.; Ackerman, M.J. Role of genetic heart disease in sentinel sudden cardiac arrest survivors across the age spectrum. Int. J. Cardiol. 2018, 270, 214–220. [Google Scholar] [CrossRef]
- Saul, J.P.; Schwartz, P.J.; Ackerman, M.J.; Triedman, J.K. Rationale and objectives for ECG screening in infancy. Heart Rhythm 2014, 11, 2316–2321. [Google Scholar] [CrossRef]
- Gajewski, K.K.; Saul, J.P. Sudden cardiac death in children and adolescents (excluding Sudden Infant Death Syndrome). Ann. Pediatr. Cardiol. 2010, 3, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, P.J.; Ackerman, M.J.; Antzelevitch, C.; Bezzina, C.R.; Borggrefe, M.; Cuneo, B.F.; Wilde, A.A.M. Inherited cardiac arrhythmias. Nat. Rev. Dis. Primers 2020, 6, 58. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, C.; Roston, T.M.; van der Werf, C.; Sanatani, S.; Chen, S.R.W.; Wilde, A.A.M.; Krahn, A.D. RYR2-ryanodinopathies: From calcium overload to calcium deficiency. Europace 2023, 25, euad156. [Google Scholar] [CrossRef] [PubMed]
- Marcus, F.I.; Chugh, S.S. Unexplained sudden cardiac death: An opportunity to identify hereditary cardiac arrhythmias. Eur. Heart J. 2011, 32, 931–933. [Google Scholar] [CrossRef]
- Minier, M.; Probst, V.; Berthome, P.; Tixier, R.; Briand, J.; Geoffroy, O.; Clementy, N.; Mansourati, J.; Jesel, L.; Dupuis, J.M.; et al. Age at diagnosis of Brugada syndrome: Influence on clinical characteristics and risk of arrhythmia. Heart Rhythm 2020, 17 Pt A, 743–749. [Google Scholar] [CrossRef]
- Wang, S.; Chen, Y.; Du, J.; Wang, Z.; Lin, Z.; Hong, G.; Qu, D.; Shen, Y.; Li, L. Post-mortem genetic analysis of sudden unexplained death in a young cohort: A whole-exome sequencing study. Int. J. Legal. Med. 2023, 137, 1661–1670. [Google Scholar] [CrossRef]
- Ensam, B.; Cheung, C.C.; Almehmadi, F.; Gregers Winkel, B.; Scrocco, C.; Brennan, P.; Leong, K.; Muir, A.; Vanarva, A.; Tfelt-Hansen, J.; et al. The Utility of Sodium Channel Provocation in Unexplained Cardiac Arrest Survivors and Electrocardiographic Predictors of Ventricular Fibrillation Recurrence. Circ. Arrhythmia Electrophysiol. 2022, 15, e011263. [Google Scholar] [CrossRef]
- Wilde AA, M.; Semsarian, C.; Márquez, M.F.; Shamloo, A.S.; Ackerman, M.J.; Ashley, E.A.; Sternick, E.B.; Barajas-Martinez, H.; Behr, E.R.; Bezzina, C.R.; et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert Consensus Statement on the state of genetic testing for cardiac diseases. EP Eur. 2022, 24, 1307–1367. [Google Scholar] [CrossRef]
- Sieira, J.; Brugada, P. Brugada Syndrome: Defining the Risk in Asymptomatic Patients. Arrhythmia Electrophysiol. Rev. 2016, 5, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez Corcia, M.C.; Sieira, J.; Sarkozy, A.; de Asmundis, C.; Chierchia, G.B.; Hernandez Ojeda, J.; Pappaert, G.; Brugada, P. Brugada syndrome in the young: An assessment of risk factors predicting future events. Europace 2017, 19, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Michowitz, Y.; Milman, A.; Andorin, A.; Sarquella-Brugada, G.; Gonzalez Corcia, M.C.; Gourraud, J.B.; Conte, G.; Sacher, F.; Juang JJ, M.; Kim, S.H.; et al. Characterization and Management of Arrhythmic Events in Young Patients with Brugada Syndrome. J. Am. Coll. Cardiol. 2019, 73, 1756–1765. [Google Scholar] [CrossRef]
- Gonzalez Corcia, M.C.; de Asmundis, C.; Chierchia, G.B.; Brugada, P. Brugada syndrome in the paediatric population: A comprehensive approach to clinical manifestations, diagnosis, and management. Cardiol. Young 2016, 26, 1044–1055. [Google Scholar] [CrossRef]
- Scrocco, C.; Ben-Haim, Y.; Devine, B.; Tome-Esteban, M.; Papadakis, M.; Sharma, S.; Macfarlane, P.W.; Behr, E.R. Role of subcutaneous implantable loop recorder for the diagnosis of arrhythmias in Brugada syndrome: A United Kingdom single-center experience. Heart Rhythm 2022, 19, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Honarbakhsh, S.; Providencia, R.; Garcia-Hernandez, J.; Martin, C.A.; Hunter, R.J.; Lim, W.Y.; Kirkby, C.; Graham, A.J.; Sharifzadehgan, A.; Waldmann, V.; et al. A Primary Prevention Clinical Risk Score Model for Patients with Brugada Syndrome (BRUGADA-RISK). JACC. Clin. Electrophysiol. 2021, 7, 210–222. [Google Scholar] [CrossRef]
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef]
- Probst, V.; Goronflot, T.; Anys, S.; Tixier, R.; Briand, J.; Berthome, P.; Geoffroy, O.; Clementy, N.; Mansourati, J.; Jesel, L.; et al. Robustness and relevance of predictive score in sudden cardiac death for patients with Brugada syndrome. Eur. Heart J. 2021, 42, 1687–1695. [Google Scholar] [CrossRef]
- Gonzalez Corcia, M.C.; Sieira, J.; Pappaert, G.; de Asmundis, C.; Chierchia, G.B.; Sarkozy, A.; Brugada, P. A Clinical Score Model to Predict Lethal Events in Young Patients (≤19 Years) With the Brugada Syndrome. Am. J. Cardiol. 2017, 120, 797–802. [Google Scholar] [CrossRef]
- Mascia, G.; Della Bona, R.; Ameri, P.; Canepa, M.; Porto, I.; Brignole, M. Brugada syndrome and syncope: A systematic review. J. Cardiovasc. Electrophysiol. 2020, 31, 3334–3338. [Google Scholar] [CrossRef]
- Nademanee, K.; Veerakul, G.; Chandanamattha, P.; Chaothawee, L.; Ariyachaipanich, A.; Jirasirirojanakorn, K.; Likittanasombat, K.; Bhuripanyo, K.; Ngarmukos, T. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation 2011, 123, 1270–1279. [Google Scholar] [CrossRef] [PubMed]
- Nademanee, K.; Chung, F.P.; Sacher, F.; Nogami, A.; Nakagawa, H.; Jiang, C.; Hocini, M.; Behr, E.; Veerakul, G.; Jan Smit, J.; et al. Long-Term Outcomes of Brugada Substrate Ablation: A Report from BRAVO (Brugada Ablation of VF Substrate Ongoing Multicenter Registry). Circulation 2023, 147, 1568–1578. [Google Scholar] [CrossRef] [PubMed]
- Writing Committee Members Shah, M.J.; Silka, M.J.; Silva JN, A.; Balaji, S.; Beach, C.M.; Benjamin, M.N.; Berul, C.I.; Cannon, B.; Cecchin, F.; Cohen, M.I.; et al. 2021 PACES Expert Consensus Statement on the Indications and Management of Cardiovascular Implantable Electronic Devices in Pediatric Patients. Heart Rhythm 2021, 18, 1888–1924. [Google Scholar] [CrossRef]
- Stazi, F.; Battisti, P. When Brugada syndrome is at risk of sudden death: Clinical and anatomical aspects. Eur. Heart J. Suppl. 2022, 24 (Suppl. I), I165–I169. [Google Scholar] [CrossRef] [PubMed]
- Miyake, C.Y.; Webster, G.; Czosek, R.J.; Kantoch, M.J.; Dubin, A.M.; Avasarala, K.; Atallah, J. Efficacy of implantable cardioverter defibrillators in young patients with catecholaminergic polymorphic ventricular tachycardia: Success depends on substrate. Circ. Arrhythmia Electrophysiol. 2013, 6, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Kallas, D.; Lamba, A.; Roston, T.M.; Arslanova, A.; Franciosi, S.; Tibbits, G.F.; Sanatani, S. Pediatric Catecholaminergic Polymorphic Ventricular Tachycardia: A Translational Perspective for the Clinician-Scientist. Int. J. Mol. Sci. 2021, 22, 9293. [Google Scholar] [CrossRef]
- Sun, B.; Yao, J.; Ni, M.; Wei, J.; Zhong, X.; Guo, W.; Zhang, L.; Wang, R.; Belke, D.; Chen, Y.X.; et al. Cardiac ryanodine receptor calcium release deficiency syndrome. Sci. Transl. Med. 2021, 13, eaba7287. [Google Scholar] [CrossRef]
- Roston, T.M.; Wei, J.; Guo, W.; Li, Y.; Zhong, X.; Wang, R.; Estillore, J.P.; Peltenburg, P.J.; Noguer FR, I.; Till, J.; et al. Clinical and Functional Characterization of Ryanodine Receptor 2 Variants Implicated in Calcium-Release Deficiency Syndrome. JAMA Cardiol. 2022, 7, 84–92. [Google Scholar] [CrossRef]
- Ormerod, J.O.M.; Ormondroyd, E.; Li, Y.; Taylor, J.; Wei, J.; Guo, W.; Wang, R.; Sarton, C.N.S.; McGuire, K.; Dreau, H.M.P.; et al. Provocation Testing and Therapeutic Response in a Newly Described Channelopathy: RyR2 Calcium Release Deficiency Syndrome. Circ. Genom. Precis. Med. 2022, 15, e003589. [Google Scholar] [CrossRef]
- Ohno, S.; Omura, M.; Kawamura, M.; Kimura, H.; Itoh, H.; Makiyama, T.; Ushinohama, H.; Makita, N.; Horie, M. Exon 3 deletion of RYR2 encoding cardiac ryanodine receptor is associated with left ventricular non-compaction. Europace 2014, 16, 1646–1654. [Google Scholar] [CrossRef]
- Dharmawan, T.; Nakajima, T.; Ohno, S.; Iizuka, T.; Tamura, S.; Kaneko, Y.; Horie, M.; Kurabayashi, M. Identification of a novel exon3 deletion of RYR2 in a family with catecholaminergic polymorphic ventricular tachycardia. Ann. Noninvasive Electrocardiol. 2019, 24, e12623. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Denjoy, I.; Extramiana, F.; Maltret, A.; Buisson, N.R.; Lupoglazoff, J.M.; Klug, D.; Hayashi, M.; Takatsuki, S.; Villain, E.; et al. Incidence and risk factors of arrhythmic events in catecholaminergic polymorphic ventricular tachycardia. Circulation 2009, 119, 2426–2434. [Google Scholar] [CrossRef] [PubMed]
- Peltenburg, P.J.; Kallas, D.; Bos, J.M.; Lieve KV, V.; Franciosi, S.; Roston, T.M.; Denjoy, I.; Sorensen, K.B.; Ohno, S.; Roses-Noguer, F.; et al. An International Multicenter Cohort Study on β-Blockers for the Treatment of Symptomatic Children with Catecholaminergic Polymorphic Ventricular Tachycardia. Circulation 2022, 145, 333–344. [Google Scholar] [CrossRef]
- Priori, S.G.; Mazzanti, A.; Santiago, D.J.; Kukavica, D.; Trancuccio, A.; Kovacic, J.C. Precision Medicine in Catecholaminergic Polymorphic Ventricular Tachycardia: JACC Focus Seminar 5/5. J. Am. Coll. Cardiol. 2021, 77, 2592–2612. [Google Scholar] [CrossRef] [PubMed]
- Roston, T.M.; Vinocur, J.M.; Maginot, K.R.; Mohammed, S.; Salerno, J.C.; Etheridge, S.P.; Cohen, M.; Hamilton, R.M.; Pflaumer, A.; Kanter, R.J.; et al. Catecholaminergic polymorphic ventricular tachycardia in children: Analysis of therapeutic strategies and outcomes from an international multicenter registry. Circ. Arrhythmia Electrophysiol. 2015, 8, 633–642. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, C.E.; Waddell-Smith, K.E.; Skinner, J.R.; Broadbent, E. Predictors of β-blocker adherence in cardiac inherited disease. Open Heart 2018, 5, e000877. [Google Scholar] [CrossRef] [PubMed]
- van der Werf, C.; Lieve, K.V.; Bos, J.M.; Lane, C.M.; Denjoy, I.; Roses-Noguer, F.; Aiba, T.; Wada, Y.; Ingles, J.; Leren, I.S.; et al. Implantable cardioverter-defibrillators in previously undiagnosed patients with catecholaminergic polymorphic ventricular tachycardia resuscitated from sudden cardiac arrest. Eur. Heart J. 2019, 40, 2953–2961. [Google Scholar] [CrossRef] [PubMed]
- Roston, T.M.; Jones, K.; Hawkins, N.M.; Bos, J.M.; Schwartz, P.J.; Perry, F.; Ackerman, M.J.; Laksman ZW, M.; Kaul, P.; Lieve KV, V.; et al. Implantable cardioverter-defibrillator use in catecholaminergic polymorphic ventricular tachycardia: A systematic review. Heart Rhythm 2018, 15, 1791–1799. [Google Scholar] [CrossRef]
- Conte, G.; Caputo, M.L.; Regoli, F.; Marcon, S.; Klersy, C.; Adjibodou, B.; Del Bufalo, A.; Moccetti, T.; Auricchio, A. True idiopathic ventricular fibrillation in out-of-hospital cardiac arrest survivors in the Swiss Canton Ticino: Prevalence, clinical features, and long-term follow-up. Europace 2017, 19, 259–266. [Google Scholar] [CrossRef]
- Conte, G.; Giudicessi, J.R.; Ackerman, M.J. Idiopathic ventricular fibrillation: The ongoing quest for diagnostic refinement. Europace 2021, 23, 4–10. [Google Scholar] [CrossRef]
- Stampe, N.K.; Jespersen, C.B.; Glinge, C.; Bundgaard, H.; Tfelt-Hansen, J.; Winkel, B.G. Clinical characteristics and risk factors of arrhythmia during follow-up of patients with idiopathic ventricular fibrillation. J. Cardiovasc. Electrophysiol. 2020, 31, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Frontera, A.; Vlachos, K.; Kitamura, T.; Mahida, S.; Pillois, X.; Fahy, G.; Marquie, C.; Cappato, R.; Stuart, G.; Defaye, P.; et al. Long-Term Follow-Up of Idiopathic Ventricular Fibrillation in a Pediatric Population: Clinical Characteristics, Management, and Complications. J. Am. Heart Assoc. 2019, 8, e011172. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, V.; Bougouin, W.; Karam, N.; Dumas, F.; Sharifzadehgan, A.; Gandjbakhch, E.; Algalarrondo, V.; Narayanan, K.; Zhao, A.; Amet, D.; et al. Characteristics and clinical assessment of unexplained sudden cardiac arrest in the real-world setting: Focus on idiopathic ventricular fibrillation. Eur. Heart J. 2018, 39, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Mellor, G.J.; Blom, L.J.; Groeneveld, S.A.; Winkel, B.G.; Ensam, B.; Bargehr, J.; van Rees, B.; Scrocco, C.; Krapels IP, C.; Volders PG, A.; et al. Familial Evaluation in Idiopathic Ventricular Fibrillation: Diagnostic Yield and Significance of J Wave Syndromes. Circ. Arrhythmia Electrophysiol. 2021, 14, e009089. [Google Scholar] [CrossRef] [PubMed]
- Honarbakhsh, S.; Srinivasan, N.; Kirkby, C.; Firman, E.; Tobin, L.; Finlay, M.; Hunter, R.J.; Murphy, C.; Lowe, M.D.; Schilling, R.J.; et al. Medium-term outcomes of idiopathic ventricular fibrillation survivors and family screening: A multicentre experience. Europace 2017, 19, 1874–1880. [Google Scholar] [CrossRef] [PubMed]
- Bergeman, A.T.; Hoeksema, W.F.; van der Ree, M.H.; Boersma, L.V.A.; Yap, S.C.; Verheul, L.M.; Hassink, R.J.; van der Crabben, S.N.; Volders, P.G.A.; van der Werf, C.; et al. Outcomes in Dutch DPP6 risk haplotype for familial idiopathic ventricular fibrillation: A focused update. Neth. Heart J. 2023, 31, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Wedekind, H.; Burde, D.; Zumhagen, S.; Debus, V.; Burkhardtsmaier, G.; Mönnig, G.; Breithardt, G.; Schulze-Bahr, E. QT interval prolongation and risk for cardiac events in genotyped LQTS-index children. Eur. J. Pediatr. 2009, 168, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Mazzanti, A.; Trancuccio, A.; Kukavica, D.; Pagan, E.; Wang, M.; Mohsin, M.; Peterson, D.; Bagnardi, V.; Zareba, W.; Priori, S.G. Independent validation and clinical implications of the risk prediction model for long QT syndrome (1-2-3-LQTS-Risk). EP Eur. 2022, 24, 614–619. [Google Scholar] [CrossRef]
- Mazzanti, A.; Maragna, R.; Vacanti, G.; Monteforte, N.; Bloise, R.; Marino, M.; Braghieri, L.; Gambelli, P.; Memmi, M.; Pagan, E.; et al. Interplay Between Genetic Substrate, QTc Duration, and Arrhythmia Risk in Patients With Long QT Syndrome. J. Am. Coll. Cardiol. 2018, 71, 1663–1671. [Google Scholar] [CrossRef]
- Kowlgi, G.N.; Giudicessi, J.R.; Barake, W.; Bos, J.M.; Ackerman, M.J. Efficacy of intentional permanent atrial pacing in the long-term management of congenital long QT syndrome. J. Cardiovasc. Electrophysiol. 2021, 32, 782–789. [Google Scholar] [CrossRef]
- Liu, J.F.; Jons, C.; Moss, A.J.; McNitt, S.; Peterson, D.R.; Qi, M.; Zareba, W.; Robinson, J.L.; Barsheshet, A.; Ackerman, M.J.; et al. Risk factors for recurrent syncope and subsequent fatal or near-fatal events in children and adolescents with long QT syndrome. J. Am. Coll. Cardiol. 2011, 57, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, I.; Moss, A.J.; Peterson, D.R.; McNitt, S.; Zareba, W.; Andrews, M.L.; Robinson, J.L.; Locati, E.H.; Ackerman, M.J.; Benhorin, J.; et al. Risk factors for aborted cardiac arrest and sudden cardiac death in children with the congenital long-QT syndrome. Circulation 2008, 117, 2184–2191. [Google Scholar] [CrossRef] [PubMed]
- Spazzolini, C.; Mullally, J.; Moss, A.J.; Schwartz, P.J.; McNitt, S.; Ouellet, G.; Fugate, T.; Goldenberg, I.; Jons, C.; Zareba, W.; et al. Clinical implications for patients with long QT syndrome who experience a cardiac event during infancy. J. Am. Coll. Cardiol. 2009, 54, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Jons, C.; Moss, A.J.; Goldenberg, I.; Liu, J.; McNitt, S.; Zareba, W.; Qi, M.; Robinson, J.L. Risk of fatal arrhythmic events in long QT syndrome patients after syncope. J. Am. Coll. Cardiol. 2010, 55, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Priori, S.G.; Schwartz, P.J.; Napolitano, C.; Bloise, R.; Ronchetti, E.; Grillo, M.; Vicentini, A.; Spazzolini, C.; Nastoli, J.; Bottelli, G.; et al. Risk stratification in the long-QT syndrome. N. Engl. J. Med. 2003, 348, 1866–1874. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.P.; Gallotti, R.G.; Shannon, K.M.; Bos, J.M.; Sadeghi, E.; Strasburger, J.F.; Wakai, R.T.; Horigome, H.; Clur, S.A.; Hill, A.C.; et al. Genotype Predicts Outcomes in Fetuses and Neonates with Severe Congenital Long QT Syndrome. JACC. Clin. Electrophysiol. 2020, 6, 1561–1570. [Google Scholar] [CrossRef] [PubMed]
- Aziz, P.F.; Tanel, R.E.; Zelster, I.J.; Pass, R.H.; Wieand, T.S.; Vetter, V.L.; Vogel, R.L.; Shah, M.J. Congenital long QT syndrome and 2:1 atrioventricular block: An optimistic outcome in the current era. Heart Rhythm 2010, 7, 781–785. [Google Scholar] [CrossRef]
- Biton, Y.; Rosero, S.; Moss, A.J.; Goldenberg, I.; Kutyifa, V.; McNitt, S.; Polonsky, B.; Baman, J.R.; Zareba, W. Primary prevention with the implantable cardioverter-defibrillator in high-risk long-QT syndrome patients. Europace 2019, 21, 339–346. [Google Scholar] [CrossRef]
- Delannoy, E.; Sacher, F.; Maury, P.; Mabo, P.; Mansourati, J.; Magnin, I.; Camous, J.P.; Tournant, G.; Rendu, E.; Kyndt, F.; et al. Cardiac characteristics and long-term outcome in Andersen-Tawil syndrome patients related to KCNJ2 mutation. Europace 2013, 15, 1805–1811. [Google Scholar] [CrossRef]
- Maffè, S.; Paffoni, P.; Bergamasco, L.; Dellavesa, P.; Zenone, F.; Baduena, L.; Franchetti Pardo, N.; Careri, G.; Facchini, E.; Sansone, V.; et al. Therapeutic management of ventricular arrhythmias in Andersen-Tawil syndrome. J. Electrocardiol. 2020, 58, 37–42. [Google Scholar] [CrossRef]
- Moreno-Manuel, A.I.; Gutiérrez, L.K.; Vera-Pedrosa, M.L.; Cruz, F.M.; Bermúdez-Jiménez, F.J.; Martínez-Carrascoso, I.; Sánchez-Pérez, P.; Macías, Á.; Jalife, J. Molecular stratification of arrhythmogenic mechanisms in the Andersen Tawil syndrome. Cardiovasc. Res. 2023, 119, 919–932. [Google Scholar] [CrossRef]
- Barrón-Díaz, D.R.; Totomoch-Serra, A.; Escobar-Cedillo, R.E.; García-Gutierrez, A.; Reyes-Quintero, Á.E.; Villegas Davirán, S.E.; Ibarra-Miramón, C.B.; Márquez, M.F. Andersen-Tawil Syndrome with High Risk of Sudden Cardiac Death in Four Mexican Patients. Cardiac and Extra-Cardiac Phenotypes. Rev. De Investig. Clin. Organo Hosp. Enfermedades Nutr. 2020, 73, 145–153. [Google Scholar] [CrossRef]
- Miyamoto, K.; Aiba, T.; Kimura, H.; Hayashi, H.; Ohno, S.; Yasuoka, C.; Tanioka, Y.; Tsuchiya, T.; Yoshida, Y.; Hayashi, H.; et al. Efficacy and safety of flecainide for ventricular arrhythmias in patients with Andersen-Tawil syndrome with KCNJ2 mutations. Heart Rhythm 2015, 12, 596–603. [Google Scholar] [CrossRef]
- Mazzanti, A.; Guz, D.; Trancuccio, A.; Pagan, E.; Kukavica, D.; Chargeishvili, T.; Olivetti, N.; Biernacka, E.K.; Sacilotto, L.; Sarquella-Brugada, G.; et al. Natural History and Risk Stratification in Andersen-Tawil Syndrome Type 1. J. Am. Coll. Cardiol. 2020, 75, 1772–1784. [Google Scholar] [CrossRef]
- Inoue, Y.Y.; Aiba, T.; Kawata, H.; Sakaguchi, T.; Mitsuma, W.; Morita, H.; Noda, T.; Takaki, H.; Toyohara, K.; Kanaya, Y.; et al. Different responses to exercise between Andersen-Tawil syndrome and catecholaminergic polymorphic ventricular tachycardia. Europace 2018, 20, 1675–1682. [Google Scholar] [CrossRef]
- Vivekanandam, V.; Männikkö, R.; Skorupinska, I.; Germain, L.; Gray, B.; Wedderburn, S.; Kozyra, D.; Sud, R.; James, N.; Holmes, S.; et al. Andersen-Tawil syndrome: Deep phenotyping reveals significant cardiac and neuromuscular morbidity. Brain A J. Neurol. 2022, 145, 2108–2120. [Google Scholar] [CrossRef]
- Krych, M.; Biernacka, E.K.; Ponińska, J.; Kukla, P.; Filipecki, A.; Gajda, R.; Hasdemir, C.; Antzelevitch, C.; Kosiec, A.; Szperl, M.; et al. Andersen-Tawil syndrome: Clinical presentation and predictors of symptomatic arrhythmias—Possible role of polymorphisms K897T in KCNH2 and H558R in SCN5A gene. J. Cardiol. 2017, 70, 504–510. [Google Scholar] [CrossRef]
- Horigome, H.; Ishikawa, Y.; Kokubun, N.; Yoshinaga, M.; Sumitomo, N.; Lin, L.; Kato, Y.; Tanabe-Kameda, Y.; Ohno, S.; Nagashima, M.; et al. Multivariate analysis of TU wave complex on electrocardiogram in Andersen-Tawil syndrome with KCNJ2 mutations. Ann. Noninvasive Electrocardiol. 2020, 25, e12721. [Google Scholar] [CrossRef]
- Dewi, I.P.; Dharmadjati, B.B. Short QT syndrome: The current evidences of diagnosis and management. J. Arrhythmia 2020, 36, 962–966. [Google Scholar] [CrossRef]
- Guerrier, K.; Kwiatkowski, D.; Czosek, R.J.; Spar, D.S.; Anderson, J.B.; Knilans, T.K. Short QT Interval Prevalence and Clinical Outcomes in a Pediatric Population. Circ. Arrhythmia Electrophysiol. 2015, 8, 1460–1464. [Google Scholar] [CrossRef]
- Gollob, M.H.; Redpath, C.J.; Roberts, J.D. The short QT syndrome: Proposed diagnostic criteria. J. Am. Coll. Cardiol. 2011, 57, 802–812. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Horie, M.; Ozawa, J.; Sumitomo, N.; Ohno, S.; Hoshino, K.; Ehara, E.; Takahashi, K.; Maeda, Y.; Yoshinaga, M.; et al. Novel electrocardiographic criteria for short QT syndrome in children and adolescents. Europace 2021, 23, 2029–2038. [Google Scholar] [CrossRef] [PubMed]
- Bjerregaard, P. Diagnosis and management of short QT syndrome. Heart Rhythm 2018, 15, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, O.; Sarquella-Brugada, G.; Cesar, S.; Arbelo, E.; Brugada, J.; Brugada, R. Recent Advances in Short QT Syndrome. Front. Cardiovasc. Med. 2018, 5, 149. [Google Scholar] [CrossRef] [PubMed]
- El-Battrawy, I.; Besler, J.; Liebe, V.; Schimpf, R.; Tülümen, E.; Rudic, B.; Lang, S.; Wolpert, C.; Zhou, X.; Akin, I.; et al. Long-Term Follow-Up of Patients with Short QT Syndrome: Clinical Profile and Outcome. J. Am. Heart Assoc. 2018, 7, e010073. [Google Scholar] [CrossRef] [PubMed]
- Giustetto, C.; Schimpf, R.; Mazzanti, A.; Scrocco, C.; Maury, P.; Anttonen, O.; Probst, V.; Blanc, J.J.; Sbragia, P.; Dalmasso, P.; et al. Long-term follow-up of patients with short QT syndrome. J. Am. Coll. Cardiol. 2011, 58, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Villafañe, J.; Atallah, J.; Gollob, M.H.; Maury, P.; Wolpert, C.; Gebauer, R.; Watanabe, H.; Horie, M.; Anttonen, O.; Kannankeril, P.; et al. Long-term follow-up of a pediatric cohort with short QT syndrome. J. Am. Coll. Cardiol. 2013, 61, 1183–1191. [Google Scholar] [CrossRef]
- El-Battrawy, I.; Besler, J.; Ansari, U.; Liebe, V.; Schimpf, R.; Tülümen, E.; Rudic, B.; Lang, S.; Odening, K.; Cyganek, L.; et al. Long-term follow-up of implantable cardioverter-defibrillators in Short QT syndrome. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2019, 108, 1140–1146. [Google Scholar] [CrossRef]
- Antzelevitch, C.; Yan, G.X.; Ackerman, M.J.; Borggrefe, M.; Corrado, D.; Guo, J.; Gussak, I.; Hasdemir, C.; Horie, M.; Huikuri, H.; et al. J-Wave syndromes expert consensus conference report: Emerging concepts and gaps in knowledge. Europace 2017, 19, 665–694. [Google Scholar] [CrossRef]
- Sebastian, S.A.; Panthangi, V.; Sethi, Y.; Padda, I.; Khan, U.; Affas, Z.R.; Mareddy, C.; Dolack, L.; Johal, G. Precision Medicine and Cardiac Channelopathies: Human iPSCs Take the Lead. Curr. Probl. Cardiol. 2023, 48, 101990. [Google Scholar] [CrossRef]
- Martínez-Barrios, E.; Cesar, S.; Cruzalegui, J.; Hernandez, C.; Arbelo, E.; Fiol, V.; Brugada, J.; Brugada, R.; Campuzano, O.; Sarquella-Brugada, G. Clinical Genetics of Inherited Arrhythmogenic Disease in the Pediatric Population. Biomedicines 2022, 10, 106. [Google Scholar] [CrossRef] [PubMed]
- Dalos, D.; Fiedler, L.; Radojevic, J.; Sponder, M.; Dichtl, W.; Schukro, C. Prevalence of early repolarization syndrome and long-term clinical outcome in patients with the diagnosis of idiopathic ventricular fibrillation. Heart Vessel. 2019, 34, 625–631. [Google Scholar] [CrossRef] [PubMed]
| Category | Condition | Percent (%) |
|---|---|---|
| Cardiomyopathies | Hypertrophic cardiomyopathy | 36 |
| Dilative cardiomyopathy | 3 | |
| Arrhythmogenic RV cardiomyopathy | 3 | |
| Coronary anomalies | Abnormal origin of LCA from the right sinus Abnormal origin of RCA from the left sinus Others | 24 |
| Primary arrhythmias | Long QT syndrome | <1 |
| Brugada syndrome | ||
| Catecholaminergic polymorphic ventricular tachycardia | ||
| Andersen–Tawil syndrome | ||
| Short QT syndrome | ||
| Wolff–Parkinson–White syndrome | ||
| Congenital complete heart block | ||
| Others | Increased cardiac mass | 10 |
| Marfan syndrome | 6 | |
| Congenital heart disease | 5 | |
| Myocarditis | 3 | |
| Ischemic heart disease | 2 | |
| Commotio cordis | <1 |
| Protein | Gene | Disease |
|---|---|---|
| Na channels | SCN5A | Long QT3 (GOF) |
| Brugada syndrome (LOF) | ||
| K channels | KCNQ1 | Long QT1 (LOF) Short QT2 (GOF) |
| KCNH2 | Long QT2 (LOF) Short QT1 (GOF) | |
| KCNJ2 | Andersen–Tawil syndrome (LOF) Short QT3 (GOF) | |
| DPP6/Kv4.x | Idiopathic familial ventricular fibrillation (GOF) | |
| Ca channels | CACNA1C | Brugada syndrome (LOF) |
| Timothy syndrome (GOF) | ||
| RYR2 | Catecholaminergic polymorphic VT (GOF) Calcium release deficiency syndrome (LOF) Exon 3 deletion syndrome | |
| Regulatory proteins | CASQ2 | Catecholaminergic polymorphic VT (LOF) |
| CALM | Long QTS (GOF) Catecholaminergic polymorphic VT (LOF) Idiopathic ventricular fibrillation |
| Condition | Prevalence | Affected Populations | Diagnostic Criteria | Risk Factors | Management and Therapy | Prognosis and Follow-Up |
|---|---|---|---|---|---|---|
| Brugada Syndrome | ~1–5 per 10,000 | Predominantly males, SE Asian descent | Type 1 Brugada ECG pattern, genetic testing (SCN5A mutation) | Fever, drugs, alcohol, electrolyte imbalances | Avoidance of triggers, drug therapy (quinidine), ICD implantation | High risk of SCD without treatment; regular follow-up and family screening recommended |
| CPVT | 1:10,000 | Mostly children and adolescents | Stress test, genetic testing (RYR2, CASQ2, TRDN mutations) | Physical or emotional stress | Beta-blockers, ICD in severe cases, flecainide, lifestyle modification | High risk of SCD, especially if untreated; regular exercise testing and genetic counseling |
| IVF | 1.2% of shockable out-of-hospital cardiac arrest survivors | Young, healthy patients | Exclusion of other causes, extensive diagnostic work-up | History of syncope, VF with adrenergic tone | ICD implantation, possibly pharmacological challenges | High recurrence of ventricular arrhythmias; long-term monitoring required |
| Long QT Syndrome | 1:2000 to 1:2500 | Affects all age groups, higher incidence in children and adolescents | Prolonged QT interval on ECG, LQTS diagnostic score, genetic testing | Syncopal episodes, SCD in family history, specific triggers like exercise or stress | Beta-blockers, ICD for secondary prevention, lifestyle modification | High risk of recurrent events; genotype-specific therapy and follow-up |
| Andersen–Tawil Syndrome (ATS) | ~1 per 1,000,000 | No specific population targeted | Genetic testing (KCNJ2 mutation for ATS1), ECG findings (prominent U waves, wide T–U junction, prolonged Q–U interval) | History of syncope, sustained VT, amiodarone administration | ICD implantation post-arrest or with sustained VT, flecainide, beta-blockers, acetazolamide, ILR for unexplained syncope | High risk of life-threatening arrhythmias; 7.9% 5-year cumulative probability of SCD; regular monitoring with Holter, ECG exercise tests, and possibly ILR |
| Short QT Syndrome (SQTS) | ~0.05% in pediatric population | Pediatric population, individuals with a family history of SQTS | QTc < 320 ms or QTc < 360 ms with risk factors, genetic mutations, early repolarization | No uniform triggers identified; history of arrhythmic syncope or cardiac arrest | ICD implantation for secondary prevention, quinidine, isoprenaline infusion, ILR for unexplained syncope | High risk of recurrent arrhythmic events; risk stratification with modified Gollob score; regular follow-up necessary |
| Early Repolarization Syndrome (ERS) | 0.5/100,000, more frequent in young males and athletes | Adults, more common in males and athletes | J-point elevation ≥ 1 mm in two adjacent inferior and/or lateral leads, QRS notching or slurring, genetic testing | ERP in relatives, history of arrhythmic syncope, unexplained SD in family history | ICD implantation, quinidine, catheter ablation of PVC, ILR | Considered a benign finding but with potential for life-threatening arrhythmias in the presence of ERP and cardiac arrest; case-by-case management |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pupaza, A.; Cinteza, E.; Vasile, C.M.; Nicolescu, A.; Vatasescu, R. Assessment of Sudden Cardiac Death Risk in Pediatric Primary Electrical Disorders: A Comprehensive Overview. Diagnostics 2023, 13, 3551. https://doi.org/10.3390/diagnostics13233551
Pupaza A, Cinteza E, Vasile CM, Nicolescu A, Vatasescu R. Assessment of Sudden Cardiac Death Risk in Pediatric Primary Electrical Disorders: A Comprehensive Overview. Diagnostics. 2023; 13(23):3551. https://doi.org/10.3390/diagnostics13233551
Chicago/Turabian StylePupaza, Adelina, Eliza Cinteza, Corina Maria Vasile, Alin Nicolescu, and Radu Vatasescu. 2023. "Assessment of Sudden Cardiac Death Risk in Pediatric Primary Electrical Disorders: A Comprehensive Overview" Diagnostics 13, no. 23: 3551. https://doi.org/10.3390/diagnostics13233551
APA StylePupaza, A., Cinteza, E., Vasile, C. M., Nicolescu, A., & Vatasescu, R. (2023). Assessment of Sudden Cardiac Death Risk in Pediatric Primary Electrical Disorders: A Comprehensive Overview. Diagnostics, 13(23), 3551. https://doi.org/10.3390/diagnostics13233551







