Endoscopic Biliary Drainage in Surgically Altered Anatomy
Abstract
:1. Introduction and Anatomical Considerations
- -
- Type I includes conditions in which the duodenum is in continuity with gastric remnant as in the case of sleeve gastrectomy and Billroth I;
- -
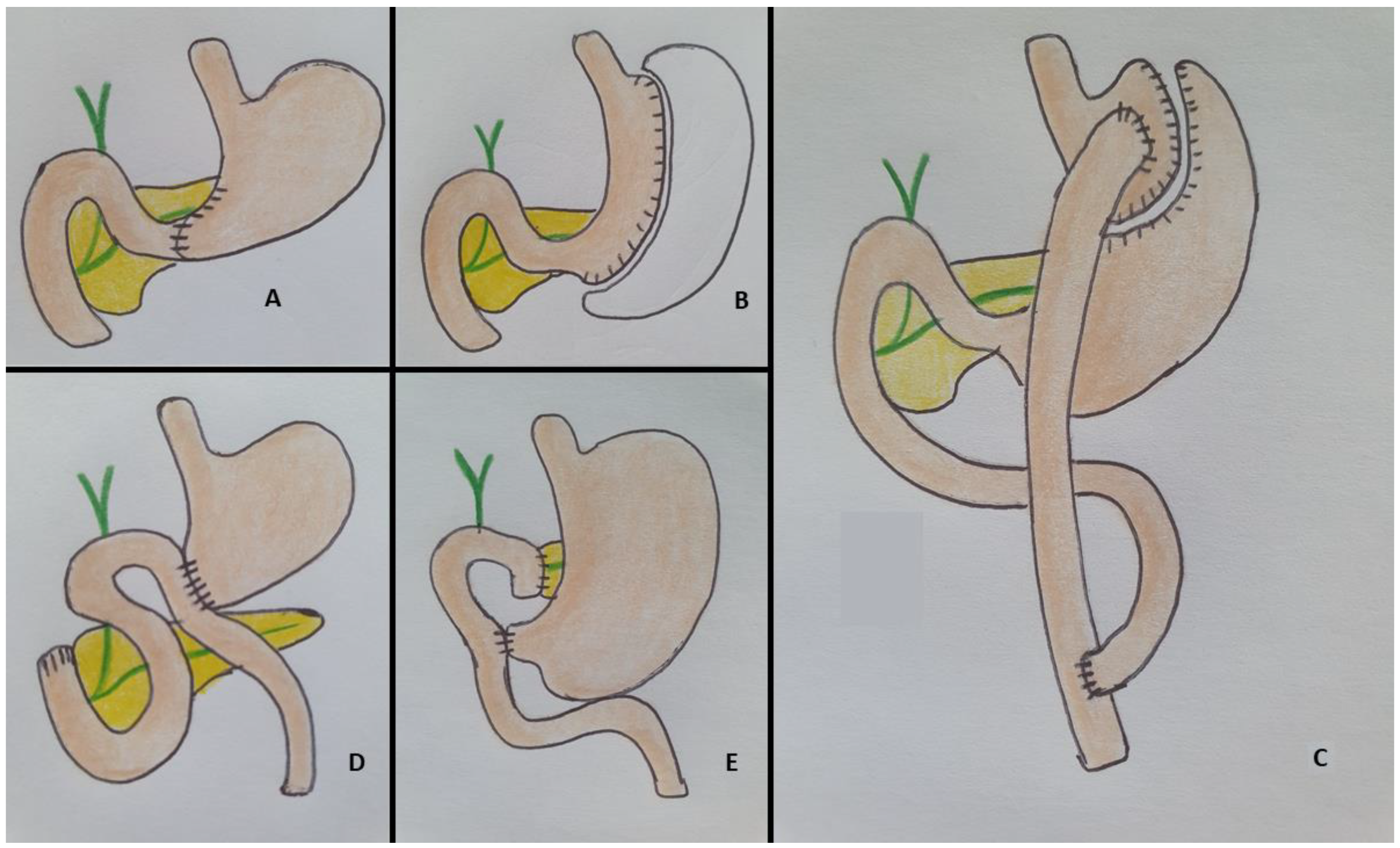
- Type II includes all the cases in which the stomach is absent (with an esophageal-jejunal anastomosis) or its remnant is not in continuity with the duodenum. This condition is present in Billroth II with gastrojejunostomy, Roux-en-Y gastric bypass (RYGB), Roux-en-Y hepatico-jejunostomy and Whipple’s procedure. Figure 1 summarizes the main surgical interventions and the anatomical alterations.
1.1. Type I
- -
- Sleeve gastrectomy
- -
- Billroth I gastrectomy
1.2. Type II
- -
- Billroth II partial gastrectomy and gastrojejunostomy
- -
- Roux-en-Y gastric bypass
- -
- Pancreaticoduodenectomy (Whipple procedure)
2. Forward-View ERCP in SAAs
3. EUS-Guided Biliary Drainage Procedures
4. EUS-Guided Antegrade Intervention
5. EUS Hepaticogastrostomy
6. EDGE (EUS-Directed Transgastric ERCP) Procedure
7. EUS-Guided Biliary Intervention versus Enteroscopy-Assisted ERCP
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33, Erratum in CA Cancer J. Clin. 2021, 71, 359. [Google Scholar] [CrossRef] [PubMed]
- Buchwald, H.; Oien, D.M. Metabolic/bariatric surgery worldwide 2011. Obes. Surg. 2013, 23, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Elton, E.; Hanson, B.L.; Qaseem, T.; Howell, D.A. Diagnostic and therapeuticERCP using an enteroscope and a pediatric colonoscopeinlong-limb surgical bypass patients. Gastrointest. Endosc. 1998, 47, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Skinner, M.; Popa, D.; Neumann, H.; Wilcox, C.; Mönkemüller, K. ERCP with the overtube-assisted enteroscopy technique: A systematic review. Endoscopy 2014, 46, 560–572. [Google Scholar] [CrossRef] [PubMed]
- Mishra, T.; Lakshmi, K.K.; Peddi, K.K. Prevalence of Cholelithiasis and Choledocholithiasis in Morbidly Obese South Indian Patients and the Further Development of Biliary Calculus Disease After Sleeve Gastrectomy, Gastric Bypass and Mini Gastric Bypass. Obes. Surg. 2016, 26, 2411–2417. [Google Scholar] [CrossRef] [PubMed]
- Anveden, Å.; Peltonen, M.; Näslund, I.; Torgerson, J.; Carlsson, L.M.S. Long-term incidence of gallstone disease after bariatric surgery: Results from the nonrandomized controlled Swedish Obese Subjects study. Surg. Obes. Relat. Dis. 2020, 16, 1474–1482. [Google Scholar] [CrossRef] [PubMed]
- Nordby, T.; Hugenschmidt, H.; Fagerland, M.W.; Ikdahl, T.; Buanes, T.; Labori, K.J. Follow-up after curative surgery for pancreatic ductal adenocarcinoma: Asymptomatic recurrence is associated with improved survival. Eur. J. Surg. Oncol. 2013, 39, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, S.; Kale, A. Endoscopic ultrasound guided biliary drainage in surgically altered anatomy: A comprehensive review of various approaches. World J. Gastrointest. Endosc. 2023, 15, 122–132. [Google Scholar] [CrossRef]
- Nakai, Y.; Kogure, H.; Isayama, H.; Koike, K. Endoscopic Ultrasound-Guided Biliary Drainage for Benign Biliary Diseases. Clin. Endosc. 2019, 52, 212–219. [Google Scholar] [CrossRef]
- Jovani, M.; Ichkhanian, Y.; Vosoughi, K.; Khashab, M.A. EUS-guided biliary drainage for postsurgical anatomy. Endosc. Ultrasound 2019, 8, S57–S66. [Google Scholar]
- Katanuma, A.; Hayashi, T.; Kin, T.; Toyonaga, H.; Honta, S.; Chikugo, K.; Ueki, H.; Ishii, T.; Takahashi, K. Interventional endoscopic ultrasonography in patients with surgically altered anatomy: Techniques and literature review. Dig. Endosc. 2020, 32, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Li, J.S.; Zou, D.W.; Jin, Z.D.; Chen, J.; Shi, X.G.; Li, Z.S.; Liu, F. Endoscopic Retrograde Cholangiopancreatography in Billroth II Gastrectomy Patients: Outcomes and Potential Factors Affecting Technical Failure. Saudi J. Gastroenterol. 2019, 25, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Nennstiel, S.; Freivogel, K.; Faber, A.; Schlag, C.; Haller, B.; Blöchinger, M.; Dollhopf, M.; Lewerenz, B.; Schepp, W.; Schirra, J.; et al. Endoscopic and Percutaneous Biliary Interventions in Patients with Altered Upper Gastrointestinal Anatomy—The Munich Multicenter Experience. Surg. Endosc. 2021, 35, 6853–6864. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Huang, Y.H.; Yao, W.; Chang, H.; Huang, X.B.; Zhang, Y.P.; Song, Z.Q. Adult Colonoscopy or Single-Balloon EnteroscopyAssisted ERCP in Long-Limb Surgical Bypass Patients. Clin. Res. Hepatol. Gastroenterol. 2014, 38, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Xu, B.; Li, Q.; Zhang, X.; Jiang, G.; Ge, X.; Nie, J.; Zhang, X.; Wu, P.; Ji, J.; et al. Endoscopic Retrograde Cholangiopancreatography in Patients with Surgically Altered Anatomy: One Single Center’s Experience. Medicine 2016, 95, e5743. [Google Scholar] [CrossRef]
- Gostout, C.J.; Bender, C.E. Colangiopancreatography, sphincterotomy, and common duct stone removal via roux-en-Y limb enteroscopy. Gastroenterology 1988, 95, 156–163. [Google Scholar] [CrossRef]
- Fugazza, A.; Anderloni, A.; Paduano, D.; Badalamenti, M.; Maselli, R.; Carrara, S.; Gabbiadini, R.; Colombo, M.; Spadaccini, M.; Cappello, A.; et al. Underwater cap-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: A pilot study. Endoscopy 2021, 53, 927–931. [Google Scholar] [CrossRef]
- Fujimoto, T.; Mori, Y.; Nakashima, Y.; Ohtsuka, T.; Nakamura, S.; Gotoh, Y.; Date, K.; Sadakari, Y.; Nakata, K.; Miyasaka, Y.; et al. Endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy: A retrospective study. Int. Surg. 2019, 103, 184–190. [Google Scholar] [CrossRef]
- Zouhairi, M.E.; Watson, J.B.; Desai, S.V.; Swartz, D.K.; Castillo-Roth, A.; Haque, M.; Jowell, P.S.; Branch, M.S.; Burbridge, R.A. Rotational assisted endoscopic retrograde cholangiopancreatography in patients with reconstructive gastrointestinal surgical anatomy. World J. Gastrointest. Endosc. 2015, 7, 278–282. [Google Scholar] [CrossRef]
- Iwashita, T.; Yasuda, I.; Mukai, T.; Iwata, K.; Doi, S.; Uemura, S.; Mabuchi, M.; Okuno, M.; Shimizu, M. Endoscopic ultrasound-guided antegrade biliary stenting for unresectable malignant biliary obstruction in patients with surgically altered anatomy: Single-center prospective pilot study. Dig. Endosc. 2017, 29, 362–368. [Google Scholar] [CrossRef]
- Iwashita, T.; Uemura, S.; Mita, N.; Iwasa, Y.; Ichikawa, H.; Mukai, T.; Yasuda, I.; Shimizu, M. Endoscopic ultrasound guided-antegrade biliary stenting vs percutaneous transhepatic biliary stenting for unresectable distal malignant biliary obstruction in patients with surgically altered anatomy. J. Hepatobiliary Pancreat. Sci. 2020, 27, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Minaga, K.; Takenaka, M.; Ogura, T.; Tamura, T.; Kuroda, T.; Kaku, T.; Uenoyama, Y.; Noguchi, C.; Nishikiori, H.; Imai, H.; et al. Endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction with surgically altered anatomy: A multicenter prospective registration study. Ther. Adv. Gastroenterol. 2020, 13, 1756284820930964. [Google Scholar] [CrossRef] [PubMed]
- Anderloni, A.; Fugazza, A.; Spadaccini, M.; Colombo, M.; Capogreco, A.; Carrara, S.; Maselli, R.; Ferrara, E.C.; Galtieri, P.A.; Pellegatta, G.; et al. Feasibility and safety of a new dedicated biliary stent for EUS-guided hepaticogastrostomy: The FIT study (with video). Endosc. Ultrasound 2023, 12, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, S.W.; Jang, H.J.; Park, D.H.; Kim, J.H.; Jung, J.H.; Koh, D.H.; Lee, J. Successful Intubation Using a Cap-Assisted Colonoscope for Endoscopic Retrograde Cholangiopancreatography in Patients Undergoing Roux-en-Y Reconstruction. J. Clin. Med. 2023, 12, 1353. [Google Scholar] [CrossRef] [PubMed]
- Yamada, A.; Kogure, H.; Nakai, Y.; Takahara, N.; Mizuno, S.; Tada, M.; Koike, K. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: A propensity-matched analysis. Dig. Endosc. 2019, 31, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Kogure, H.; Sato, T.; Nakai, Y.; Ishigaki, K.; Hakuta, R.; Saito, K.; Takahara, N.; Hamada, T.; Mizuno, S.; Yamada, A.; et al. Endoscopic management of pancreatic diseases in patients with surgically altered anatomy: Clinical outcomes of combination of double-balloon endoscopy- and endoscopic ultrasound-guided interventions. Dig. Endosc. 2021, 33, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, Y.; Matsumoto, K.; Kato, H.; Tsutsumi, K.; Tomoda, T.; Matsumi, A.; Miyamoto, K.; Yamazaki, T.; Saragai, Y.; Fujii, Y.; et al. Treatment outcomes, including risk factors of stone recurrence, for hepatolithiasis using balloon-assisted endoscopy in patients with hepaticojejunostomy (with video). Surg. Endosc. 2021, 35, 1895–1902. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.F.; Modayil, R.; Gurram, K.C.; Brathwaite, C.E.M.; Friedel, D.; Stavropoulos, S.N. Spiral enteroscopy-assisted ERCP in bariatric-length Roux-en-Y anatomy: A large single-center series and review of the literature (with video). Gastrointest. Endosc. 2018, 87, 1241–1247. [Google Scholar] [CrossRef]
- Vila, J.J.; Fernández-Urién, I.; Carrascosa, J. EUS and ERCP: A rationale categorization of a productive partnership. Endosc. Ultrasound 2021, 10, 25–32. [Google Scholar] [CrossRef]
- Spadaccini, M.; Binda, C.; Fugazza, A.; Repici, A.; Tarantino, I.; Fabbri, C.; Cugia, L.; Anderloni, A.; On Behalf of The Interventional Endoscopy Ultra Sound I-Eus Group. Informed Consent for Endoscopic Biliary Drainage: Time for a New Paradigm. Medicina 2022, 58, 331. [Google Scholar] [CrossRef]
- Binda, C.; Spadaccini, M.; Cugia, L.; Anderloni, A. EUS and ERCP partnership. Endosc. Ultrasound 2022, 11, 426–427. [Google Scholar] [CrossRef]
- Tanisaka, Y.; Mizuide, M.; Fujita, A.; Jinushi, R.; Shiomi, R.; Shin, T.; Hirata, D.; Terada, R.; Tashima, T.; Mashimo, Y.; et al. Endoscopic ultrasound-guided biliary drainage in patients with surgically altered anatomy: A systematic review and Meta-analysis. Scand. J. Gastroenterol. 2023, 58, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Ogura, T.; Kitano, M.; Takenaka, M.; Okuda, A.; Minaga, K.; Yamao, K.; Yamashita, Y.; Hatamaru, K.; Noguchi, C.; Gotoh, Y.; et al. Multicenter prospective evaluation study of endoscopic ultrasound-guided hepaticogastrostomy combined with antegrade stenting (with video). Dig. Endosc. 2018, 30, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Fugazza, A.; Colombo, M.; Spadaccini, M.; Vespa, E.; Gabbiadini, R.; Capogreco, A.; Repici, A.; Anderloni, A. Relief of jaundice in malignant biliary obstruction: When should we consider endoscopic ultrasonography-guided hepaticogastrostomy as an option? Hepatobiliary Pancreat. Dis. Int. 2022, 21, 234–240. [Google Scholar] [CrossRef]
- Cho, J.H.; Park, S.W.; Kim, E.J.; Park, C.H.; Park, D.H.; Lee, K.J.; Lee, S.S. Long-term outcomes and predictors of adverse events of EUS-guided hepatico-gastrostomy for malignant biliary obstruction: Multicenter, retrospective study. Surg. Endosc. 2022, 36, 8950–8958. [Google Scholar] [CrossRef]
- Kedia, P.; Sharaiha, R.Z.; Kumta, N.A.; Kahaleh, M. Internal EUSdirected transgastric ERCP (EDGE): Game over. Gastroenterology 2014, 147, 566–568. [Google Scholar] [CrossRef]
- Kedia, P.; Kumta, N.A.; Widmer, J.; Sundararajan, S.; Cerefice, M.; Gaidhane, M.; Sharaiha, R.; Kahaleh, M. Endoscopic ultrasounddirected transgastric ERCP (EDGE) for Roux-en-Y anatomy: A novel technique. Endoscopy 2015, 47, 159–163. [Google Scholar]
- Auriemma, F.; Fugazza, A.; Colombo, M.; Spadaccini, M.; Repici, A.; Anderloni, A. Safety issues in endoscopy ultrasound-guided interventions using lumen apposing metal stents. Minerva Gastroenterol. 2022, 68, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Ngamruengphong, S.; Nieto, J.; Kunda, R.; Kumbhari, V.; Chen, Y.I.; Bukhari, M.; El Zein, M.H.; Bueno, R.P.; Hajiyeva, G.; Ismail, A.; et al. Endoscopic ultrasound-guided creation of a transgastric fistula for the management of hepatobiliary disease in patients with roux-en-Y gastric bypass. Endoscopy 2017, 49, 549–552. [Google Scholar] [CrossRef]
- Tyberg, A.; Nieto, J.; Salgado, S.; Weaver, K.; Kedia, P.; Sharaiha, R.Z.; Gaidhane, M.; Kahaleh, M. Endoscopic ultrasound (EUS)-directed transgastric endoscopic retrograde cholangiopancreatography or EUS: Mid-term analysis of an emerging procedure. Clin. Endosc. 2017, 50, 185–190. [Google Scholar] [CrossRef]
- Bukhari, M.; Kowalski, T.; Nieto, J.; Kunda, R.; Ahuja, N.K.; Irani, S.; Shah, A.; Loren, D.; Brewer, O.; Sanaei, O.; et al. An international, multicenter, comparative trial of EUS-guided gastrogastrostomyassisted ERCP versus enteroscopy-assisted ERCP in patients with roux-en-Y gastric bypass anatomy. Gastrointest. Endosc. 2018, 88, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Khashab, M.A.; El Zein, M.H.; Sharzehi, K.; Marson, F.P.; Haluszka, O.; Small, A.J.; Nakai, Y.; Park, D.H.; Kunda, R.; Teoh, A.Y.; et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: An international comparative study. Endosc. Int. Open 2016, 4, E1322–E1327. [Google Scholar] [CrossRef] [PubMed]


| Authors | BD Procedure | SAA | Indication | Pts | Technical Success | Clinical Success | AEs |
|---|---|---|---|---|---|---|---|
| Simon Nennstiel [13] | Duodenoscope 168 (20.2%) Pediatric colonoscope 285 (34.3%) SBE 144 (17.3%) DBE 78 (9.4%) Colonoscope 103 (12.4%) Gastroscope 50 (6%) | RY 186 (44%) B II 105 (24.8%) Whipple 120 (28.4%) | Malignant 203 (49.4%) Benign 187 (45.5%) | 441 | Duodenoscope -B II 62 (88.1%) -Whipple 11 (57.9%) -RY 58 (75.3%) -Pediatric Colonoscope -B II 49 (66.2%) -Whipple 71 (64%) -Roux-en-Y 37 (37%) -SBE -BII - -Whipple 15 (56.6%) -RY 78 (69.6%) DBE -B II- -Whipple 9 (64.3%) -RY 29 (48.3%) Colonoscope -B II 8 (50%) -Whipple 18 (50%) -RY 28 (54.9%) Gastroscope -B II 33 (16.2%) -Whipple 7 (3.2%) -RY 10 (2.4%) | - | Total 4 (8%) -B II 4 (12.1%) |
| Fei Wang [15] | -Gastroscope -Duodenoscope -Standard colonoscope -Long-type colonoscope DBE SBE | BII 52 (53%) Subtotal or Total Gastrectomy with RY 20 (21%) Pancreatoduodenectomy or RY hepaticojejunostomy reconstruction 25 (25.8%) | Malignant 33 (34.02%) Benign 60 (61.85%) | 97 | B II—gastroscope 11/13 84.6% Duodenoscope 5/8 (62.5%) Standard colonoscope 29/31 (93.5%) Subtotal or total gastrectomy with RY anastomosis Standard colonoscope 2/4 (50%) Long colonoscope 7/10 (70%) DBE (5/6) 83.3% Pancreatoduodenectomy or RY Hepatico-jejunostomy reconstruction Standard colonoscope 3/6 (50%) Long colonoscope 88.9% (8/9) DBE 8/10 (80%) | - | Total (10/97) 10.3% 3 Pancreatitis 4 Hyperamylasemia 1 Cholangitis 1 Bleeding 1 Cardiopulmonary accident |
| Fugazza [17] | Pediatric colonoscope | Distal gastrectomy and RY 3/6 (50%) Whipple (Pylorus preserving) 2/6 (33.3%) Gastrojejunal Bypass 1/6 (16.7%) | Benign 6/6 | 6 | 100% | 100% | 0 |
| Takaaki Fujimoto [18] | DBE Gastroscope | Gastrectomy and RY 38 (37.2%); BII 24 (23.5%); Pancretoduodenoctomy followed by BII 23 (22.5%); Pancretoduodenoctomy or RY hepaticojejunostomy 17 (16.6%) | Benign 100% | 102 | 88% (144/164) | \ | 11/180 (6%) 2 Perforation 7 Cholangitis 2 Hyperamylasemia |
| Zouhairi [19] | RA-ERCP | 33 RY (91.7%) 2 B II (5.5%) 1 Hepaticojejunostomy (2.93%) | Bengin 100% | 36 | 29/32 (89.7%) | \ | 10/42 (23.8%) 3 Nausea and abdominal pain 7 Pancreatitis |
| Iwashita [20] | EUS-AI | 14 Gastrectomy with RY 1 Gastrectomy with BII 1 Hepatectomy with biliary reconstruction 4 Gastric bypass | Malignant 100% | 20 | 19/20 95% | 19/20 95% | 4/20 (20%) 3 Mild pancreatitis 1 Mild fever |
| Iwashita [21] | EUS AI PTBD | Gastrectomy with RY 49 (76.6%) Gastrectomy with BII 8 (11.8%) Gastric bypass 7 (10.3%) | Malignant 100% | 64 | EUS AI 34/35 (97.1%) PTBD (28/29) 96.6% | EUS AI 34/35 (97.1%) PTBD (27/29) 93.1% | EUS AI 4/34 (11.4%) PTBD 8/29 (27.6%) |
| Minaga [22] | EUS AI EUS HGS Combination technique | Gastrectomy with RY 19/40 (47.5%) Gastrectomy with BII 6/40 (15%) Pancreaticoduodenectomy 11/40/27.5%) Hepaticojejunostomy with RY 4/40 (10%) | Malignant 100% | 40 | EUS HGS 24 60% EUS AI 2 5% Combination technique 14 35% | 38 [95,(83.1–99.4)] | Early AEs 6 (15%)
|
| Anderloni [23] | EUS HGS | 4 RY | Malignant 100% | 22 | 100% | 20/22 (91%) | 3/22 (13.6) Hepatic abscess |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spadaccini, M.; Giacchetto, C.M.; Fiacca, M.; Colombo, M.; Andreozzi, M.; Carrara, S.; Maselli, R.; Saccà, F.; De Marco, A.; Franchellucci, G.; et al. Endoscopic Biliary Drainage in Surgically Altered Anatomy. Diagnostics 2023, 13, 3623. https://doi.org/10.3390/diagnostics13243623
Spadaccini M, Giacchetto CM, Fiacca M, Colombo M, Andreozzi M, Carrara S, Maselli R, Saccà F, De Marco A, Franchellucci G, et al. Endoscopic Biliary Drainage in Surgically Altered Anatomy. Diagnostics. 2023; 13(24):3623. https://doi.org/10.3390/diagnostics13243623
Chicago/Turabian StyleSpadaccini, Marco, Carmelo Marco Giacchetto, Matteo Fiacca, Matteo Colombo, Marta Andreozzi, Silvia Carrara, Roberta Maselli, Fabio Saccà, Alessandro De Marco, Gianluca Franchellucci, and et al. 2023. "Endoscopic Biliary Drainage in Surgically Altered Anatomy" Diagnostics 13, no. 24: 3623. https://doi.org/10.3390/diagnostics13243623
APA StyleSpadaccini, M., Giacchetto, C. M., Fiacca, M., Colombo, M., Andreozzi, M., Carrara, S., Maselli, R., Saccà, F., De Marco, A., Franchellucci, G., Khalaf, K., Koleth, G., Hassan, C., Anderloni, A., Repici, A., & Fugazza, A. (2023). Endoscopic Biliary Drainage in Surgically Altered Anatomy. Diagnostics, 13(24), 3623. https://doi.org/10.3390/diagnostics13243623








