Preoperative Hilar and Mediastinal Lymph Node Staging in Patients with Suspected or Diagnosed Lung Cancer: Accuracy of 18F-FDG-PET/CT:A Retrospective Cohort Study of 138 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Eligibility
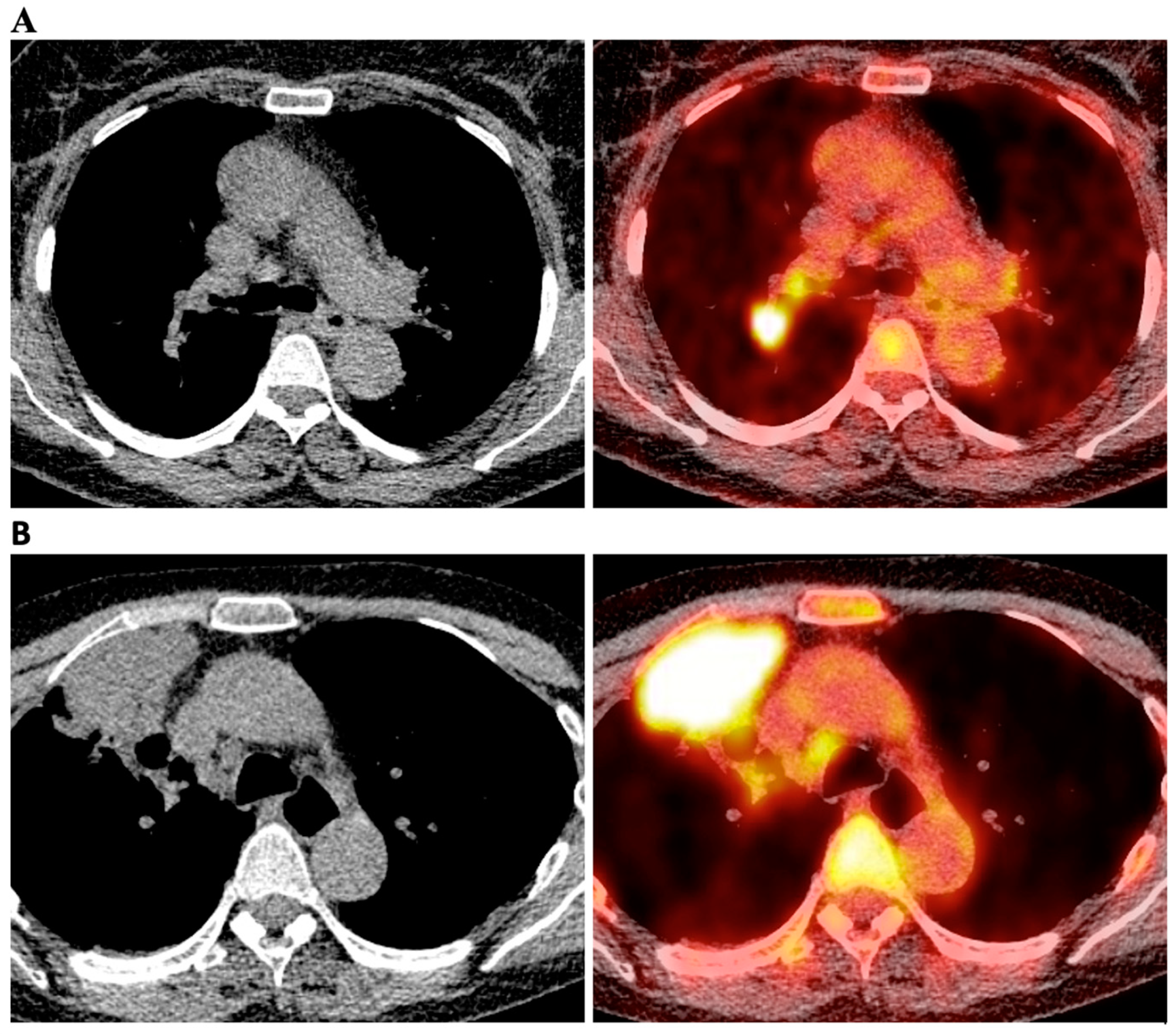
2.2. Integrated 18F-FDG PET/CT
2.3. Surgical Resection and Histopathology
2.4. Data Analysis
3. Results
3.1. Patient Characteristics
3.2. Evaluation of HMLN Status by Pathological Examination and Integrated 18F-FDG-PET/CT
3.3. Risk Factors Associated with False Negative Detection of HMLN Metastasis of 18F-FDG-PET/CT Staging
3.4. Risk Factors Associated with False Positive Detection of HMLN Metastasis of 18F-FDG-PET/CT Staging
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sheel, A.R.; McShane, J.; Poullis, M.P. Survival of patients with or without symptoms undergoing potentially curative resections for primary lung cancer. Ann. Thorac. Surg. 2013, 95, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Bayman, N.A.; Blackhall, F.; Jain, P.; Lee, L.; Thatcher, N.; Faivre-Finn, C. Management of unresectable stage III non-small-cell lung cancer with combined-modality therapy: A review of the current literature and recommendations for treatment. Clin. Lung Cancer 2008, 9, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Tieu, B.H.; Sanborn, R.E.; Thomas, C.R.J. Neoadjuvant therapy for resectable non-small cell lung cancer with mediastinal lymph node involvement. Thorac. Surg. Clin. 2008, 18, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Bilfinger, T.V. Surgical viewpoints for the definitive treatment of lung cancer. Respir. Care Clin. N. Am. 2003, 9, 141–162. [Google Scholar] [CrossRef]
- Verschakelen, J.A.; De Wever, W.; Bogaert, J. Role of computed tomography in lung cancer staging. Curr. Opin. Pulm. Med. 2004, 10, 248–255. [Google Scholar] [CrossRef]
- Birim, O.; Kappetein, A.P.; Stijnen, T.; Bogers, A.J. Meta-analysis of positron emission tomographic and computed tomographic imaging in detecting mediastinal lymph node metastases in nonsmall cell lung cancer. Ann. Thorac. Surg. 2005, 79, 375–382. [Google Scholar] [CrossRef]
- Webb, W.R.; Sarin, M.; Zerhouni, E.A.; Heelan, R.T.; Glazer, G.M.; Gatsonis, C. Interobserver variability in CT and MR staging of lung cancer. J. Comput. Assist. Tomogr. 1993, 17, 841–846. [Google Scholar] [CrossRef]
- Rohren, E.M.; Turkington, T.G.; Coleman, R.E. Clinical applications of PET in oncology. Radiology 2004, 231, 305–332. [Google Scholar] [CrossRef]
- Cerfolio, R.J.; Ojha, B.; Bryant, A.S.; Raghuveer, V.; Mountz, J.M.; Bartolucci, A.A. The accuracy of integrated PET-CT compared with dedicated PET alone for the staging of patients with nonsmall cell lung cancer. Ann. Thorac. Surg. 2004, 78, 1017–1023; discussion 1017–1023. [Google Scholar] [CrossRef]
- Mayor, S. NICE issues guidance for diagnosis and treatment of lung cancer. BMJ 2005, 330, 439. [Google Scholar] [CrossRef]
- Zhao, L.; He, Z.-Y.; Zhong, X.-N.; Cui, M.-L. (18)FDG-PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer: A meta-analysis. Surg. Oncol. 2012, 21, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.C.; Port, J.L.; Korst, R.J.; Liss, Y.; Meherally, D.N.; Altorki, N.K. Risk factors for occult mediastinal metastases in clinical stage I non-small cell lung cancer. Ann. Thorac. Surg. 2007, 84, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Al-Sarraf, N.; Aziz, R.; Gately, K.; Lucey, J.; Wilson, L.; McGovern, E.; Young, V. Pattern and predictors of occult mediastinal lymph node involvement in non-small cell lung cancer patients with negative mediastinal uptake on positron emission tomography. Eur. J. Cardio Thorac. Surg. 2008, 33, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Kaseda, K.; Watanabe, K.; Asakura, K.; Kazama, A.; Ozawa, Y. Identification of false-negative and false-positive diagnoses of lymph node metastases in non-small cell lung cancer patients staged by integrated (18F-)fluorodeoxyglucose-positron emission tomography/computed tomography: A retrospective cohort study. Thorac. Cancer 2016, 7, 473–480. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Zheng, Q.; Ma, Y.; Wang, Y.; Feng, Y.; Zhao, B.; Yang, Y. Implications of false negative and false positive diagnosis in lymph node staging of NSCLC by means of 18F-FDG PET/CT. PLoS ONE 2013, 8, e78552. [Google Scholar] [CrossRef] [PubMed]
- James, D.; Brierley, M.K.G.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; O’Sullivan, B., Mason, M., Asamura, H., Lee, A., Eycken, E.V., Denny, L., Amin, M.B., Gupta, S., Eds.; Wiley-Blackwell: New York, NY, USA, 2016; p. 272. [Google Scholar]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef] [Green Version]
- Asamura, H.; Chansky, K.; Crowley, J.; Goldstraw, P.; Rusch, V.W.; Vansteenkiste, J.F.; Watanabe, H.; Wu, Y.-L.; Zielinski, M.; Ball, D.; et al. The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2015, 10, 1675–1684. [Google Scholar] [CrossRef] [Green Version]
- Rami-Porta, R.; Bolejack, V.; Crowley, J.; Ball, D.; Kim, J.; Lyons, G.; Rice, T.; Suzuki, K.; Thomas, C.F.J.; Travis, W.D.; et al. The IASLC Lung Cancer Staging Project: Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2015, 10, 990–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eberhardt, W.E.; Mitchell, A.; Crowley, J.; Kondo, H.; Kim, Y.T.; Turrisi, A., 3rd; Goldstraw, P.; Rami-Porta, R. The IASLC Lung Cancer Staging Project: Proposals for the Revision of the M Descriptors in the Forthcoming Eighth Edition of the TNM Classification of Lung Cancer. J. Thorac. Oncol. 2015, 10, 1515–1522. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Caro, A.; Garcia-Reina, S.; Reguart, N.; Arguis, P.; Sanchez, M.; Gimferrer, J.M.; Marrades, R.; Lomeña, F. Incidence of occult mediastinal node involvement in cN0 non-small-cell lung cancer patients after negative uptake of positron emission tomography/computer tomography scan. Eur. J. Cardio Thorac. Surg. 2010, 37, 1168–1174. [Google Scholar] [CrossRef]
- Shimizu, K.; Yoshida, J.; Nagai, K.; Nishimura, M.; Ishii, G.; Morishita, Y.; Nishiwaki, Y. Visceral pleural invasion is an invasive and aggressive indicator of non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2005, 130, 160–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casiraghi, M.; Travaini, L.L.; Maisonneuve, P.; Tessitore, A.; Brambilla, D.; Agoglia, B.G.; Guarize, J.; Spaggiari, L. Lymph node involvement in T1 non-small-cell lung cancer: Could glucose uptake and maximal diameter be predictive criteria? Eur. J. Cardio Thorac. Surg. 2011, 39, e38–e43. [Google Scholar] [CrossRef] [PubMed]
- Shim, S.S.; Lee, K.S.; Kim, B.-T.; Chung, M.J.; Lee, E.J.; Han, J.; Choi, J.Y.; Kwon, O.J.; Shim, Y.M.; Kim, S. Non-small cell lung cancer: Prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology 2005, 236, 1011–1019. [Google Scholar] [CrossRef]
- Guberina, M.; Darwiche, K.; Hautzel, H.; Ploenes, T.; Pöttgen, C.; Guberina, N.; Herrmann, K.; Umutlu, L.; Wetter, A.; Theegarten, D.; et al. Impact of EBUS-TBNA in addition to [18F]FDG-PET/CT imaging on target volume definition for radiochemotherapy in stage III NSCLC. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2894–2903. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Distribution (n) |
|---|---|
| Sex | |
| Male/Female | 82/56 |
| Age | |
| Mean ± SD/Range | 64 ± 9.25/29 − 84 |
| Smoking status | |
| Smoker/former smoker/never smoker | 72/48/18 |
| History of lung disease or diabetes | |
| Yes/no | 67/71 |
| Location of the tumor | |
| Central/non-central | 33/105 |
| Lobar distribution of the tumor | |
| RUL/RML/RLL/LUL/LLL | 40/8/30/41/19 |
| Histological type | |
| Adenocarcinoma/squamous cell carcinoma/other types/no malignancy | 69/48/14/7 |
| Pleural invasion | |
| Yes/No | 20/118 |
| Pathological T stage | |
| Tis/T1a/T1b/T1c/T2a/T2b/T3/T4 | 1/12/18/30/24/13/24/9 |
| Lymph node metastasis | |
| pN0/pN1/pN2 | 94/27/17 |
| Pathological stage | |
| 0/Ia1/Ia2/Ia3/Ib/IIa/IIb/IIIa/IIIb/IVa | 1/5/16/18/17/6/34/25/3/6 |
| Tumor size (cm) | |
| Median/Mean ± SD/Range | 2.8/3.164 ± 1.823/0.3 − 12.5 |
| SUVmax of primary tumor | |
| Median/Mean ± SD/Range | 8.1/9.623 ± 6.342/1.1 − 34.77 |
| pN0 | pN1 | pN2 | |
|---|---|---|---|
| cN0 (n = 83) | 65 | 13 | 5 |
| cN1 (n = 25) | 9 | 12 | 4 |
| cN2 (n = 17) | 9 | 1 | 7 |
| cN3 (n = 13) | 11 | 1 | 1 |
| Pathological Positive (N1 + N2) | Pathological Negative (N0) | |
|---|---|---|
| PET/CT (+) | 26 (TP) | 29 (FP) |
| PET/CT (−) | 18 (FN) | 65 (TN) |
| Variable | Status | Pathologically Positive | Pathologically Negative | p-Value |
|---|---|---|---|---|
| Age (years) | >65 | 10 | 33 | n.s. |
| ≤65 | 8 | 32 | ||
| Gender | Female | 7 | 26 | n.s. |
| Male | 11 | 39 | ||
| Smoking status | Never-smoker | 2 | 12 | n.s. |
| Ex-smoker | 7 | 21 | ||
| Current smoker | 9 | 32 | n.s. | |
| Concurrent lung disease | Absent | 14 | 45 | |
| Present | 4 | 20 | n.s. | |
| Concurrent diabetes | Absent | 15 | 53 | |
| Present | 3 | 12 | n.s. | |
| Tumor laterality | Right | 9 | 34 | |
| Left | 9 | 31 | n.s. | |
| Tumor location | Central | 4 | 11 | |
| Non-central | 14 | 54 | n.s. | |
| Other malignancy history | Absent | 8 | 35 | |
| Present | 10 | 30 | n.s. | |
| Tumor size | ≤3.0 cm | 6 | 44 | |
| >3.0 cm | 12 | 21 | 0.008 | |
| VPI | Absent | 12 | 58 | |
| Present | 6 | 7 | 0.020 | |
| SUVmax of primary tumor | <8.25 | 6 | 39 | |
| ≥8.25 | 12 | 23 | 0.026 | |
| Grade | well | 0 | 12 | |
| moderate/poor | 18 | 50 | 0.059 |
| Variable | Odds Ratio | Confidence Interval | p-Value |
|---|---|---|---|
| SUVmax of primary tumor (≥8.25) | 0.170 | 0.034–0.857 | 0.032 |
| VPI | 0.109 | 0.20–0.586 | 0.010 |
| Variable | Status | Pathologically Positive | Pathologically Negative | p-Value |
|---|---|---|---|---|
| Age (years) | >65 | 12 | 7 | 0.086 |
| ≤65 | 14 | 22 | ||
| Gender | Female | 12 | 11 | n.s. |
| Male | 14 | 18 | ||
| Smoking status | Never-smoker | 2 | 2 | n.s. |
| Ex-smoker | 9 | 11 | ||
| Current smoker | 15 | 16 | n.s. | |
| Concurrent lung disease | Absent | 16 | 15 | |
| Present | 10 | 14 | n.s. | |
| Concurrent diabetes | Absent | 24 | 27 | |
| Present | 2 | 2 | n.s. | |
| Tumor laterality | Right | 16 | 18 | |
| Left | 10 | 11 | n.s. | |
| Tumor location | Central | 10 | 8 | |
| Non-central | 16 | 21 | n.s. | |
| Other malignancy history | Absent | 17 | 20 | |
| Present | 9 | 9 | n.s. | |
| Tumor size | ≤3.0 cm | 15 | 14 | |
| >3.0 cm | 11 | 14 | n.s. | |
| VPI | Absent | 23 | 25 | |
| Present | 3 | 4 | n.s. | |
| SUVmax of primary tumor | <8.25 | 10 | 13 | |
| ≥8.25 | 15 | 16 | n.s. | |
| Grade | well | 2 | 8 | |
| moderate/poor | 24 | 19 | 0.076 | |
| SUVmax of LN | ≥4.7 | 12 | 5 | |
| <4.7 | 12 | 22 | 0.017 |
| Variable | Odds Ratio | Confidence Interval | p-Value |
|---|---|---|---|
| SUVmax of LN (<4.7) | 0.061 | 0.007–0.531 | 0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Damirov, F.; Büsing, K.; Yavuz, G.; Hatz, R.; Manapov, F.; Michels, J.; Hohenberger, P.; Roessner, E. Preoperative Hilar and Mediastinal Lymph Node Staging in Patients with Suspected or Diagnosed Lung Cancer: Accuracy of 18F-FDG-PET/CT:A Retrospective Cohort Study of 138 Patients. Diagnostics 2023, 13, 403. https://doi.org/10.3390/diagnostics13030403
Damirov F, Büsing K, Yavuz G, Hatz R, Manapov F, Michels J, Hohenberger P, Roessner E. Preoperative Hilar and Mediastinal Lymph Node Staging in Patients with Suspected or Diagnosed Lung Cancer: Accuracy of 18F-FDG-PET/CT:A Retrospective Cohort Study of 138 Patients. Diagnostics. 2023; 13(3):403. https://doi.org/10.3390/diagnostics13030403
Chicago/Turabian StyleDamirov, Fuad, Karen Büsing, Gökce Yavuz, Rudolf Hatz, Farkhad Manapov, Julia Michels, Peter Hohenberger, and Eric Roessner. 2023. "Preoperative Hilar and Mediastinal Lymph Node Staging in Patients with Suspected or Diagnosed Lung Cancer: Accuracy of 18F-FDG-PET/CT:A Retrospective Cohort Study of 138 Patients" Diagnostics 13, no. 3: 403. https://doi.org/10.3390/diagnostics13030403
APA StyleDamirov, F., Büsing, K., Yavuz, G., Hatz, R., Manapov, F., Michels, J., Hohenberger, P., & Roessner, E. (2023). Preoperative Hilar and Mediastinal Lymph Node Staging in Patients with Suspected or Diagnosed Lung Cancer: Accuracy of 18F-FDG-PET/CT:A Retrospective Cohort Study of 138 Patients. Diagnostics, 13(3), 403. https://doi.org/10.3390/diagnostics13030403








