Correlation between Thrombus Perviousness and Distal Embolization during Mechanical Thrombectomy in Acute Stroke
Abstract
:1. Introduction
2. Methods
2.1. Patient Imaging
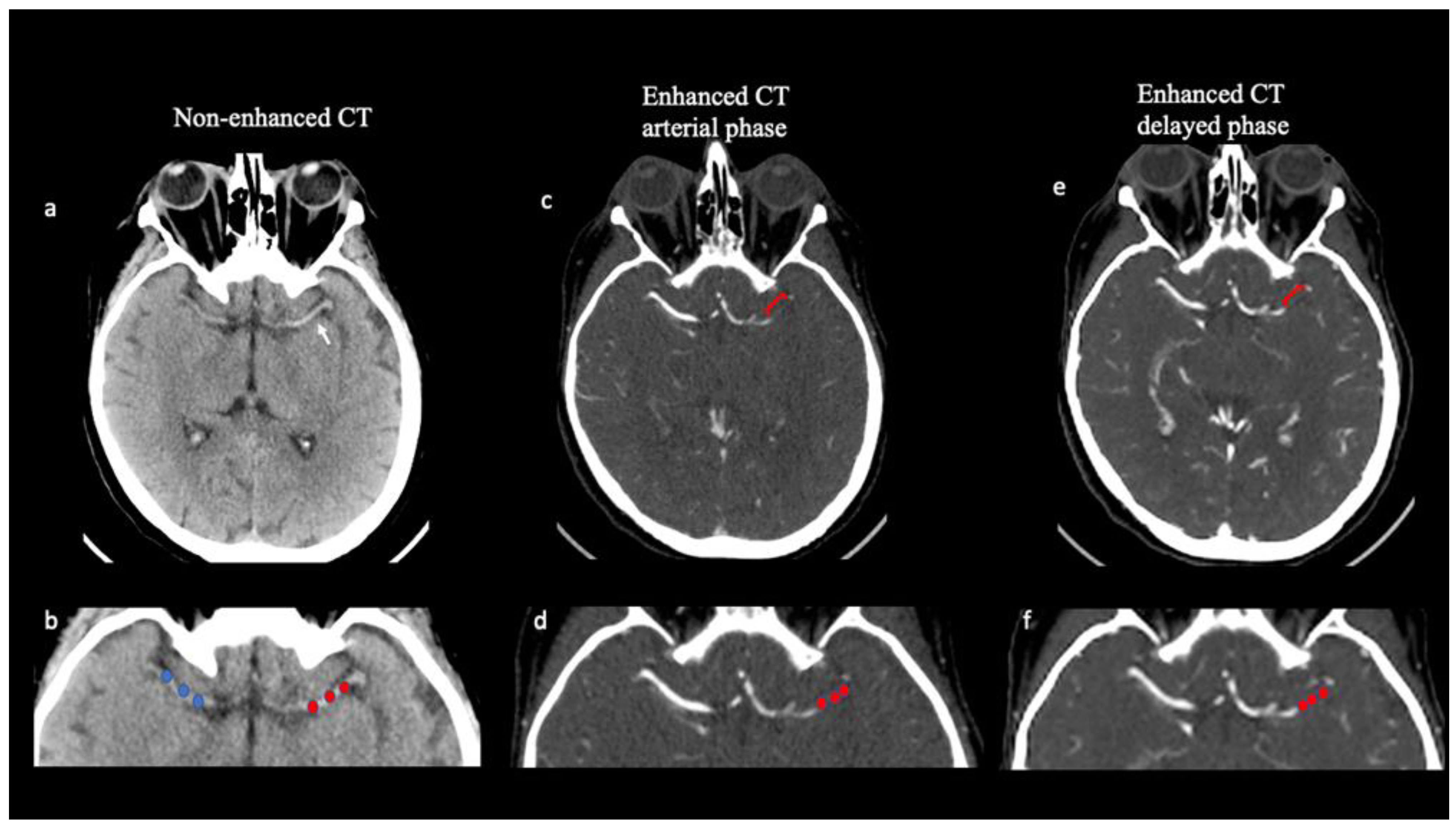
2.2. Image Analysis
Thrombus Attenuation and Length
2.3. Estimation of Perviousness
2.4. Histological Analysis of Clots
2.5. Statistical Analysis
3. Results
Predictors of Distal Embolization
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nogueira, R.G.; Liebeskind, D.S.; Sung, G.; Duckwiler, G.; Smith, W.S. Predictors of Good Clinical Outcomes, Mortality, and Successful Revascularization in Patients with Acute Ischemic Stroke Undergoing Thrombectomy. Stroke 2009, 40, 3777–3783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Pilato, F.; Silva, S.; Valente, I.; Distefano, M.; Broccolini, A.; Brunetti, V.; Caliandro, P.; Della Marca, G.; Di Iorio, R.; Frisullo, G.; et al. Predicting Factors of Functional Outcome in Patients with Acute Ischemic Stroke Admitted to Neuro-Intensive Care Unit. A Prospective Cohort Study. Brain Sci. 2020, 10, 911. [Google Scholar] [CrossRef] [PubMed]
- Di Maria, F.; Kyheng, M.; Consoli, A.; Desilles, J.-P.; Gory, B.; Richard, S.; Rodesch, G.; Labreuche, J.; Girot, J.-B.; Dargazanli, C.; et al. Identifying the predictors of first-pass effect and its influence on clinical outcome in the setting of endovascular thrombectomy for acute ischemic stroke: Results from a multicentric prospective registry. Int. J. Stroke 2020, 16, 20–28. [Google Scholar] [CrossRef]
- Santos, E.M.; Marquering, H.A.; Blanken, M.D.D.; Berkhemer, O.A.; Boers, A.M.; Yoo, A.J.; Beenen, L.F.; Treurniet, K.M.; Wismans, C.; van Noort, K.; et al. Thrombus Permeability Is Associated with Improved Functional Outcome and Recanalization in Patients with Ischemic Stroke. Stroke 2016, 47, 732–741. [Google Scholar] [CrossRef] [Green Version]
- Pilato, F.; Valente, I.; Calandrelli, R.; Alexandre, A.; Arena, V.; Dell’Aquila, M.; Broccolini, A.; Della Marca, G.; Morosetti, R.; Frisullo, G.; et al. Clot evaluation and distal embolization risk during mechanical thrombectomy in anterior circulation stroke. J. Neurol. Sci. 2021, 432, 120087. [Google Scholar] [CrossRef]
- He, G.; Deng, J.; Lu, H.; Wei, L.; Zhao, Y.; Zhu, Y.; Li, Y. Thrombus enhancement sign on CT angiography is associated with the first pass effect of stent retrievers. J. NeuroInterventional Surg. 2022, 15, 146–152. [Google Scholar] [CrossRef]
- Pilato, F.; Verdolotti, T.; Calandrelli, R.; Valente, I.; Monelli, E.; Cottonaro, S.; Capone, F.; Motolese, F.; Iaccarino, G.; Rossi, S.S.; et al. Color-coded multiphase computed tomography angiography may predict outcome in anterior circulation acute ischemic stroke. J. Neurol. Sci. 2021, 430, 119989. [Google Scholar] [CrossRef]
- Berndt, M.; Friedrich, B.; Maegerlein, C.; Moench, S.; Hedderich, D.; Lehm, M.; Zimmer, C.; Straeter, A.; Poppert, H.; Wunderlich, S.; et al. Thrombus Permeability in Admission Computed Tomographic Imaging Indicates Stroke Pathogenesis Based on Thrombus Histology. Stroke 2018, 49, 2674–2682. [Google Scholar] [CrossRef]
- Benson, J.C.; Fitzgerald, S.; Kadirvel, R.; Johnson, C.; Dai, D.; Karen, D.; Kallmes, D.F.; Brinjikji, W. Clot permeability and histopathology: Is a clot’s perviousness on CT imaging correlated with its histologic composition? J. NeuroInterventional Surg. 2019, 12, 38–42. [Google Scholar] [CrossRef]
- Patel, T.; Fricano, S.; Waqas, M.; Tso, M.; Dmytriw, A.; Mokin, M.; Kolega, J.; Tomaszewski, J.; Levy, E.; Davies, J.; et al. Increased Perviousness on CT for Acute Ischemic Stroke is Associated with Fibrin/Platelet-Rich Clots. Am. J. Neuroradiol. 2020, 42, 57–64. [Google Scholar] [CrossRef]
- Verdolotti, T.; Pilato, F.; Cottonaro, S.; Monelli, E.; Giordano, C.; Guadalupi, P.; Benenati, M.; Ramaglia, A.; Costantini, A.M.; Alexandre, A.; et al. ColorViz, a New and Rapid Tool for Assessing Collateral Circulation during Stroke. Brain Sci. 2020, 10, 882. [Google Scholar] [CrossRef]
- Di Meglio, L.; Desilles, J.-P.; Ollivier, V.; Nomenjanahary, M.S.; Di Meglio, S.; Deschildre, C.; Loyau, S.; Olivot, J.-M.; Blanc, R.; Piotin, M.; et al. Acute ischemic stroke thrombi have an outer shell that impairs fibrinolysis. Neurology 2019, 93, e1686–e1698. [Google Scholar] [CrossRef]
- Jolugbo, P.; Ariëns, R.A. Thrombus Composition and Efficacy of Thrombolysis and Thrombectomy in Acute Ischemic Stroke. Stroke 2021, 52, 1131–1142. [Google Scholar] [CrossRef]
- Welsh, J.D.; Stalker, T.; Voronov, R.; Muthard, R.W.; Tomaiuolo, M.; Diamond, S.L.; Brass, L.F. A systems approach to hemostasis: 1. The interdependence of thrombus architecture and agonist movements in the gaps between platelets. Blood 2014, 124, 1808–1815. [Google Scholar] [CrossRef]
- Boeckh-Behrens, T.; Schubert, M.; Förschler, A.; Prothmann, S.; Kreiser, K.; Zimmer, C.; Riegger, J.; Bauer, J.; Neff, F.; Kehl, V.; et al. The Impact of Histological Clot Composition in Embolic Stroke. Clin. Neuroradiol. 2014, 26, 189–197. [Google Scholar] [CrossRef]
- Seker, F.; Pfaff, J.; Wolf, M.; Schönenberger, S.; Nagel, S.; Herweh, C.; Pham, M.; Bendszus, M.; Möhlenbruch, M.A. Impact of thrombus length on recanalization and clinical outcome following mechanical thrombectomy in acute ischemic stroke. J. NeuroInterventional Surg. 2016, 9, 937–939. [Google Scholar] [CrossRef]
- Berndt, M.; Mück, F.; Maegerlein, C.; Wunderlich, S.; Zimmer, C.; Wirth, S.; Mönch, S.; Kaesmacher, J.; Friedrich, B.; Boeckh-Behrens, T. Introduction of CTA-index as Simplified Measuring Method for Thrombus Perviousness. Clin. Neuroradiol. 2020, 31, 773–781. [Google Scholar] [CrossRef]
- Santos, E.M.; Dankbaar, J.W.; Treurniet, K.M.; Horsch, A.D.; Roos, Y.B.; Kappelle, L.J.; Niessen, W.J.; Majoie, C.B.; Velthuis, B.; Marquering, H.A.; et al. Permeable Thrombi Are Associated with Higher Intravenous Recombinant Tissue-Type Plasminogen Activator Treatment Success in Patients with Acute Ischemic Stroke. Stroke 2016, 47, 2058–2065. [Google Scholar] [CrossRef] [Green Version]
- Byun, J.-S.; Nicholson, P.; Hilditch, C.A.; Tsang, A.C.O.; Pereira, V.M.; Krings, T.; Fang, Y.; Brinjikji, W. Thrombus perviousness is not associated with first-pass revascularization using stent retrievers. Interv. Neuroradiol. 2019, 25, 285–290. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.T.; Lip, G.Y.H. Red vs White Thrombi: Treating the Right Clot Is Crucial. Arch. Intern. Med. 2003, 163, 2534–2535. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, A.M.; Pedicelli, A.; Valente, I.; Scarcia, L.; Giubbolini, F.; D’Argento, F.; Lozupone, E.; Distefano, M.; Pilato, F.; Colosimo, C. May endovascular thrombectomy without CT perfusion improve clinical outcome? Clin. Neurol. Neurosurg. 2020, 198, 106207. [Google Scholar] [CrossRef] [PubMed]
- Niesten, J.M.; Van Der Schaaf, I.C.; Van Dam, L.; Vink, A.; Vos, J.A.; Schonewille, W.J.; De Bruin, P.C.; Mali, W.P.T.M.; Velthuis, B.K. Histopathologic Composition of Cerebral Thrombi of Acute Stroke Patients Is Correlated with Stroke Subtype and Thrombus Attenuation. PLoS ONE 2014, 9, e88882. [Google Scholar] [CrossRef]
- Kirchhof, K.; Welzel, T.; Mecke, C.; Zoubaa, S.; Sartor, K. Differentiation of White, Mixed, and Red Thrombi: Value of CT in Estimation of the Prognosis of Thrombolysis—Phantom Study. Radiology 2003, 228, 126–130. [Google Scholar] [CrossRef]
- Bilgic, A.B.; Gocmen, R.; Arsava, E.M.; Topcuoglu, M.A. The Effect of Clot Volume and Permeability on Response to Intravenous Tissue Plasminogen Activator in Acute Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 104541. [Google Scholar] [CrossRef]
| Variables | No Distal Embolization (n = 55) | Distal Embolization (n = 45) | Total (100) | p-Value |
|---|---|---|---|---|
| Age (years) | 74.18 (71.30–77.07) | 70.97 (67.29–74.66) | 72.74 (70.43–75.04) | 0.17 |
| Female n (%) | 25 (45.45%) | 28 (62.22%) | 53 (53.00%) | 0.09 |
| Diabetes n (%) | 15 (27.27%) | 13 (28.89%) | 28 (28.00%) | 0.86 |
| AF n (%) | 17 (30.91%) | 12 (26.67%) | 29 (29.00%) | 0.64 |
| Smoking n (%) | 9 (16.36%) | 8 (17.78%) | 17 (17.00%) | 0.85 |
| Hypertension n (%) | 43 (78.18%) | 28 (62.22%) | 741 (71.00%) | 0.08 |
| Systolic Pressure (mmHg) | 141.62 (130.42–152.81) | 136.07 (126.96–145.18) | 138.69 (131.57–145.81) | 0.44 |
| Diastolic Pressure (mmHg) | 81.38 (75.81–86.96) | 78.14 (72.40–83.88) | 79.67 (75.67–83.67) | 0.42 |
| Mean Pressure (mmHg) | 105.02 (96.80–113.24) | 98.12 (91.75–104.50) | 100.79 (95.71–105.87) | 0.19 |
| Wake-up-Stroke n (%) | 7 (12.73%) | 3 (6.67%) | 10 (10.00%) | 0.31 |
| rt-PA n (%) | 26 (47.27%) | 23 (51.11%) | 49 (49.00%) | 0.70 |
| Onset-to-Needle (min) | 154.17 (121.48–186.85) | 168.14 (120.26–216.01) | 160.85 (132.55–189.15) | 0.62 |
| Cardioembolic stroke n (%) | 30 (60.00%) | 23 (62.16%) | 53 (53%) | 0.84 |
| Thrombus Length at CTA (mm) | 13.22 (11.44–15.00) | 16.05 (13.01–19.08) | 14.57 (12.83–16.31) | 0.11 |
| Hyperdensity at CT n (%) | 30 (54.55%) | 31 (68.89%) | 61 (61.00%) | 0.14 |
| Occlusion site ad DSA | 0.45 | |||
| ICA | 13 (24.07%) | 16 (34.78%) | 29 (29.00%) | |
| M1 | 32 (59.26%) | 24 (52.17%) | 56 (56.00%) | |
| ICA+M1 | 5 (9.26%) | 5 (10.87%) | 10 (10.00% | |
| M2 | 4 (7.41%) | 1 (2.17%) | 5 (5.00%) | |
| HCT (%) | 39.54 (38.06–41.02) | 39.95 (38.55–41.34) | 39.72 (38.70–40.75) | 0.70 |
| n. of Passages | 1.96 (1.58–2.35) | 2.09 (1.72–2.46) | 2.02 (1.75–2.29) | 0.65 |
| Technique n (%) | 0.20 | |||
| Combined | 25 (45.45%) | 27 (60.00%) | 52 (52.00%) | |
| Stent-retriever | 1 (1.82%) | 2 (4.44%) | 3 (3.00%) | |
| Contact Aspiration | 29 (52.73%) | 16 (35.56%) | 45 (45.00%) | |
| HU pre-CE | 53.04 (50.84–55.24) | 54.71 (52.34–57.09) | 53.86 (52.24–55.48) | 0.31 |
| HU post-CE 1 | 57.25 (54.96–59.54) | 58.70 (56.31–61.09) | 57.96 (56.31–59.61) | 0.39 |
| HU post-CE 2 | 61.95 (59.54–64.36) | 62.56 (60.03–65.09) | 62.25 (60.51–63.98) | 0.73 |
| Perviousness pre-post 1 | 4.24 (3.89–4.58) | 3.71 (3.33–4.10) | 3.98 (3.72–4.25) | 0.05 |
| Perviousness pre-post 2 | 12.49 (10.01–14.98) | 12.32 (9.76–14.87) | 12.41 (10.64–14.18) | 0.92 |
| Fragment Dimension (mm) | 12.00 (9.40–14.60) | 11.72 (9.63–13.81) | 11.37 (10.03–12.72) | 0.87 |
| Mastocytes n (%) | 1 (16.67%) | 5 (50.00%) | 6 (37.50%) | 0.18 |
| Stratification n (%) | 27 (64.29%) | 22 (51.16%) | 49 (57.65%) | 0.22 |
| Chrystals n (%) | 2 (4.76%) | 2 (4.65%) | 4 (4.71%) | 0.98 |
| Heritrocitic Core n (%) | 26 (61.90%) | 22 (51.16%) | 48 (56.47%) | 0.32 |
| Distal Embolization | Coef. | p-Value | 95% Conf | Interval |
|---|---|---|---|---|
| rt-PA | 1.07 | 0.89 | 0.41 | 2.8 |
| Thrombus Length at CTA | 1.04 | 0.21 | 0.98 | 1.11 |
| Technique: (ref. Combined) | 1 | |||
| Contact Aspiration | 0.39 | 0.05 | 0.15 | 1.02 |
| Perviousness pre-post 1 | 0.66 | 0.04 | 0.44 | 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pilato, F.; Valente, I.; Alexandre, A.M.; Calandrelli, R.; Scarcia, L.; D’Argento, F.; Lozupone, E.; Arena, V.; Pedicelli, A. Correlation between Thrombus Perviousness and Distal Embolization during Mechanical Thrombectomy in Acute Stroke. Diagnostics 2023, 13, 431. https://doi.org/10.3390/diagnostics13030431
Pilato F, Valente I, Alexandre AM, Calandrelli R, Scarcia L, D’Argento F, Lozupone E, Arena V, Pedicelli A. Correlation between Thrombus Perviousness and Distal Embolization during Mechanical Thrombectomy in Acute Stroke. Diagnostics. 2023; 13(3):431. https://doi.org/10.3390/diagnostics13030431
Chicago/Turabian StylePilato, Fabio, Iacopo Valente, Andrea M. Alexandre, Rosalinda Calandrelli, Luca Scarcia, Francesco D’Argento, Emilio Lozupone, Vincenzo Arena, and Alessandro Pedicelli. 2023. "Correlation between Thrombus Perviousness and Distal Embolization during Mechanical Thrombectomy in Acute Stroke" Diagnostics 13, no. 3: 431. https://doi.org/10.3390/diagnostics13030431
APA StylePilato, F., Valente, I., Alexandre, A. M., Calandrelli, R., Scarcia, L., D’Argento, F., Lozupone, E., Arena, V., & Pedicelli, A. (2023). Correlation between Thrombus Perviousness and Distal Embolization during Mechanical Thrombectomy in Acute Stroke. Diagnostics, 13(3), 431. https://doi.org/10.3390/diagnostics13030431







