How Frequently Benign Uterine Myomas Appear Suspicious for Sarcoma as Assessed by Transvaginal Ultrasound?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
- Premenopausal or postmenopausal women diagnosed as having at least one myoma.
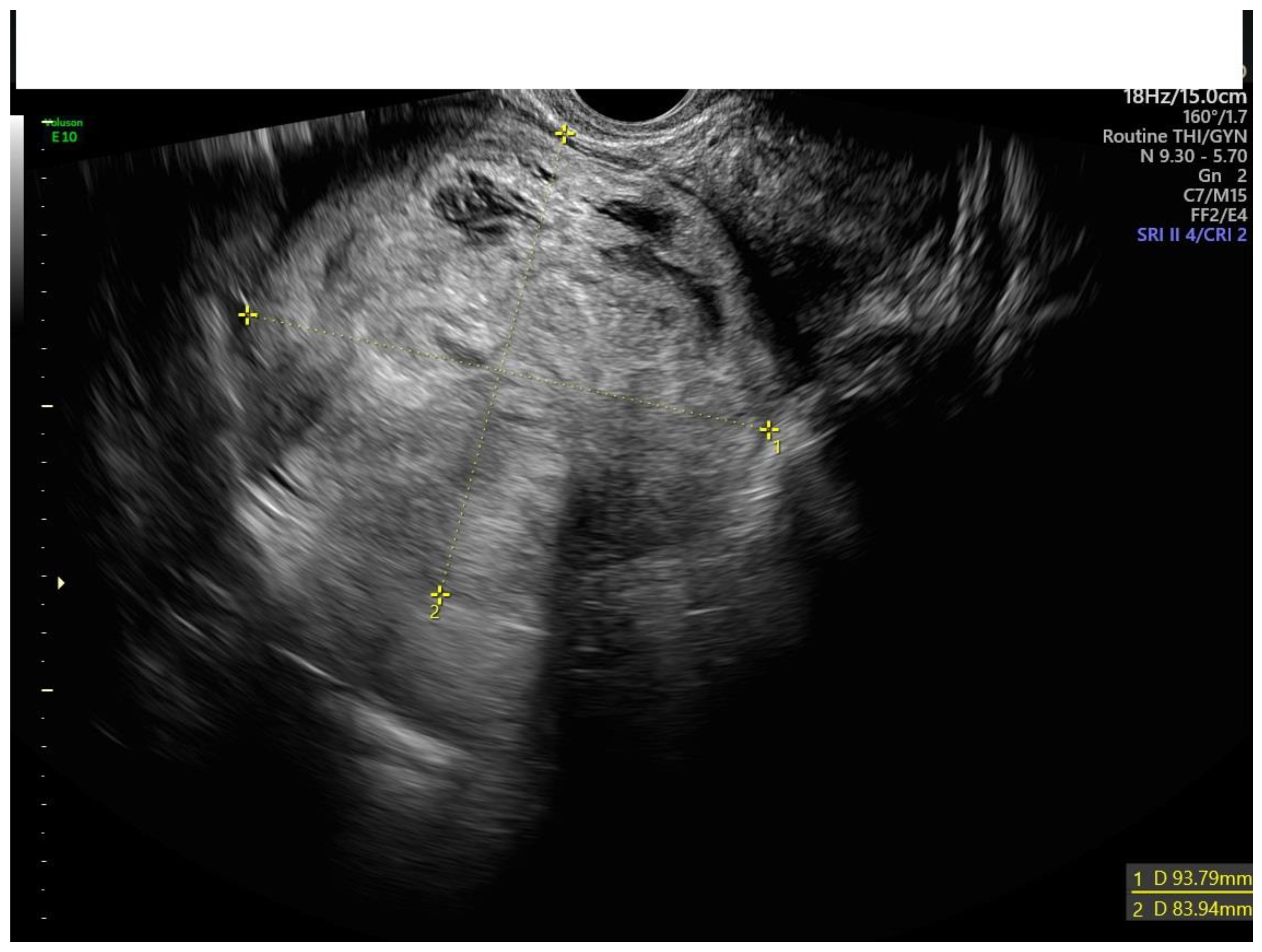
- Preoperative transvaginal or transrectal ultrasound.
- Surgical removal of myomas because of symptoms (bleeding, pain, discomfort), including hysterectomy (open or laparoscopic) and myomectomy (open, laparoscopic or hysteroscopic).
- Definitive histologic diagnosis of benign uterine myoma.
- Incomplete ultrasound data.
- Definitive histologic diagnoses other than benign myoma (uterine sarcoma, smooth tumor of uterine muscle of uncertain malignant potential, or any other diagnosis).
2.3. Ultrasound Assessment
2.4. Reference Standard
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ryan, G.I.; Syrop, C.H.; Van Voorhis, B.J. Role, epidemiology, and natural history of benign uterine mass lesions. Clin. Obstet. Gynecol. 2005, 48, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, A.; Bernuit, D.; Gerlinger, C.; Schaefers, M.; Geppert, K. Prevalence, symptoms and management of uterine fibroids: An international internet-based survey of 21,746 women. BMC Women Health 2012, 12, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dueholm, M.; Hjorth, I.M. Structured imaging technique in the gynecologic office for the diagnosis of abnormal uterine bleeding. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 40, 23–43. [Google Scholar] [CrossRef] [PubMed]
- Van den Bosch, T.; Dueholm, M.; Leone, F.P.; Valentin, L.; Rasmussen, C.K.; Votino, A.; Van Schoubroeck, D.; Landolfo, C.; Installé, A.J.F.; Guerriero, S.; et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: A consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet. Gynecol. 2015, 46, 284–298. [Google Scholar] [CrossRef]
- FIGO Commitee on Gynecologic Oncology. FIGO staging for uterine Sarcomas. Int. J. Gyn. Obst 2009, 104, 179. [Google Scholar] [CrossRef]
- Desai, V.B.; Wright, J.D.; Gross, C.P.; Lin, H.; Boscoe, F.P.; Hutchison, L.M.; Schwartz, P.E.; Xu, X. Prevalence, characteristics, and risk factors of occult uterine cancer in presumed benign hysterectomy. Am. J. Obstet. Gynecol. 2019, 221, 39.e1–39.e14. [Google Scholar] [CrossRef]
- Valzacchi, R.G.M.; Rosas, P.; Uzal, M.; Gil, S.J.; Viglierchio, V.T. Incidence of Leiomyosarcoma at Surgery for Presumed Uterine Myomas in Different Age Groups. J. Minim. Invasive Gynecol. 2019, 27, 926–929. [Google Scholar] [CrossRef]
- D’Angelo, E.; Prat, J. Uterine sarcomas: A review. Gynecol. Oncol. 2010, 116, 131–139. [Google Scholar] [CrossRef]
- Ulrich, L.G. Benign leiomyoma or malignant sarcoma: The difficult differential diagnosis. Maturitas 2015, 80, 235–236. [Google Scholar] [CrossRef]
- Raine-Bennett, T.; Tucker, L.Y.; Zaritsky, E.; Littell, R.D.; Palen, T.; Neugebauer, R.; Axtell, A.; Schultze, P.M.; Kronbach, D.; Embry-Schubert, J.; et al. Occult Uterine Sarcoma and Leiomyosarcoma: Incidence of and Survival Associated with Morcellation. Obstet. Gynecol. 2016, 127, 29–39. [Google Scholar] [CrossRef]
- Halaska, M.J.; Haidopoulos, D.; Guyon, F.; Morice, P.; Zapardiel, I.; Kesic, V.; ESGO Council. European Society of Gynecological Oncology Statement on Fibroid and Uterine Morcellation. Int. J. Gynecol. Cancer. 2017, 27, 189–192. [Google Scholar] [CrossRef] [PubMed]
- ACOG Committee. Opinion No. 770 Summary: Uterine Morcellation for Presumed Leiomyomas. Obstet. Gynecol. 2019, 133, 604–605. [Google Scholar]
- Ludovisi, M.; Moro, F.; Pasciuto, T.; Di Noi, S.; Giunchi, S.; Savelli, L.; Pascual, M.A.; Sladkevicius, P.; Alcazar, J.L.; Franchi, D.; et al. Imaging in gynecological disease (15): Clinical and ultrasound characteristics of uterine sarcoma. Ultrasound Obstet. Gynecol. 2019, 54, 676–687. [Google Scholar] [CrossRef]
- Testa, A.C.; Di Legge, A.; Bonatti, M.; Manfredi, R.; Scambia, G. Imaging techniques for evaluation of uterine myomas. Best Pract. Res. Clin. Obstet. Gynaecol. 2016, 34, 37–53. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz, K.; Góra, T.; Guzik, P.; Harpula, M.; Chechliński, P.; Wolak, E.; Stryjkowska-Góra, A. Uterine Myomas and Sarcomas-Clinical and Ultrasound Characteristics and Differential Diagnosis Using Pulsed and Color Doppler Techniques. J. Ultrason. 2022, 22, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Chantasartrassamee, P.; Kongsawatvorakul, C.; Rermluk, N.; Charakorn, C.; Wattanayingcharoenchai, R.; Lertkhachonsuk, A.A. Preoperative clinical characteristics between uterine sarcoma and leiomyoma in patients with uterine mass, a case-control study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 270, 176–180. [Google Scholar] [CrossRef]
- Köhler, G.; Vollmer, M.; Nath, N.; Hessler, P.A.; Dennis, K.; Lehr, A.; Köller, M.; Riechmann, C.; Bralo, H.; Trojnarska, D.; et al. Benign uterine mass-discrimination from leiomyosarcoma by a preoperative risk score: A multicenter cohort study. Arch. Gynecol. Obstet. 2019, 300, 1719–1727. [Google Scholar] [CrossRef]
- Nagai, T.; Takai, Y.; Akahori, T.; Ishida, H.; Hanaoka, T.; Uotani, T.; Sato, S.; Matsunaga, S.; Baba, K.; Seki, H. Novel uterine sarcoma preoperative diagnosis score predicts the need for surgery in patients presenting with a uterine mass. Springerplus 2014, 3, 678. [Google Scholar] [CrossRef] [Green Version]
- Parker, W.H.; Fu, Y.S.; Berek, J.S. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet Gynecol. 1994, 83, 414–418. [Google Scholar]
- Armbrust, R.; Wernecke, K.D.; Sehouli, J.; David, M. The growth of uterine myomas in untreated women: Influence factors and ultrasound monitoring. Arch. Gynecol. Obstet. 2018, 297, 131–137. [Google Scholar] [CrossRef]
- Żak, K.; Zaremba, B.; Rajtak, A.; Kotarski, J.; Amant, F.; Bobiński, M. Preoperative Differentiation of Uterine Leiomyomas and Leiomyosarcomas: Current Possibilities and Future Directions. Cancers 2022, 14, 1966. [Google Scholar] [CrossRef] [PubMed]
- Dueholm, M.; Lundorf, E.; Hansen, E.S.; Ledertoug, S.; Olesen, F. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am. J. Obstet. Gynecol. 2002, 186, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.Y.; Kim, K.; Kim, Y.B.; No, J.H. Differential diagnosis between uterine sarcoma and leiomyoma using preoperative clinical characteristics. J. Obstet. Gynaecol. Res. 2016, 42, 313–318. [Google Scholar] [CrossRef]
- Oh, J.; Park, S.B.; Park, H.J.; Lee, E.S. Ultrasound Features of Uterine Sarcomas. Ultrasound Q. 2019, 35, 376–384. [Google Scholar] [CrossRef]
- Kurjak, A.; Kupesic, S.; Shalan, H.; Jukic, S.; Kosuta, D.; Ilijas, M. Uterine sarcoma: A report of 10 cases studied by transvaginal color and pulsed Doppler sonography. Gynecol. Oncol. 1995, 59, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Hata, T.; Maruyama, R.; Hirai, M. Uterine sarcoma: Can it be differentiated from uterine leiomyoma with Doppler ultrasonography? A preliminary report. Ultrasound Obstet. Gynecol. 1997, 9, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Hata, T.; Iida, K.; Miyazaki, K. Expression of thymidine phosphorylase in uterine sarcoma and uterine leiomyoma: Association with microvessel density and Doppler blood flow analysis. Ultrasound Obstet. Gynecol. 1997, 10, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Szabó, I.; Szánthó, A.; Csabay, L.; Csapó, Z.; Szirmai, K.; Papp, Z. Color Doppler ultrasonography in the differentiation of uterine sarcomas from uterine leiomyomas. Eur. J. Gynaecol. Oncol. 2002, 23, 29–34. [Google Scholar]
- Aviram, R.; Ochshorn, Y.; Markovitch, O.; Fishman, A.; Cohen, I.; Altaras, M.M.M.; Tepper, T. Uterine sarcomas versus leiomyomas: Gray-scale and Doppler sonographic findings. J. Clin. Ultrasound. 2005, 33, 10–13. [Google Scholar] [CrossRef]
- Exacoustos, C.; Romanini, M.E.; Amadio, A.; Amoroso, C.; Szabolcs, B.; Zupi, E.; Arduini, D. Can gray-scale and color Doppler sonography differentiate between uterine leiomyosarcoma and leiomyoma? J. Clin. Ultrasound. 2007, 35, 449–457. [Google Scholar] [CrossRef]
- Russo, C.; Camilli, S.; Martire, F.G.; Di Giovanni, A.; Lazzeri, L.; Malzoni, M.; Zupi, E.; Exacoustos, C. Ultrasound features of highly vascularized uterine myomas (uterine smooth muscle tumors) and correlation with histopathology. Ultrasound Obstet. Gynecol. 2022, 60, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Dubreuil, J.; Tordo, J.; Rubello, D.; Giammarile, F.; Skanjeti, A. Diffusion-weighted MRI and 18F-FDG-PET/CT imaging: Competition or synergy as diagnostic methods to manage sarcoma of the uterus? A systematic review of the literature. Nucl. Med. Commun. 2017, 38, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Aoki, M.; Miyagawa, C.; Murakami, K.; Takaya, H.; Kotani, Y.; Nakai, H.; Matsumura, N. Differential Diagnosis of Uterine Leiomyoma and Uterine Sarcoma using Magnetic Resonance Images: A Literature Review. Healthcare 2019, 7, 158. [Google Scholar] [CrossRef] [PubMed]


| Ultrasound Feature | Frequency in Uterine Sarcomas |
|---|---|
| Irregular contour | 52.8% |
| No visible myometrium | 24.6% |
| Not uniform cchogenicity | 77.4% |
| Irregular cystic areas | 44.6% |
| Intralesional color score 3–4 | 67.9% |
| Ultrasound Suspicious Features | N (%) |
|---|---|
| None | 478 (59.0) |
| One | 203 (25.0) |
| Two | 89 (11.0) |
| Three | 24 (3.0) |
| Four | 15 (1.9) |
| Five | 1 (0.1) |
| Suspicious | Center A | Center B | Center C | Center D | Center E | Center F |
|---|---|---|---|---|---|---|
| No | 233 (95.1%) | 189 (95.0%) | 107 (96.4%) | 125 (97.7%) | 37 (94.9%) | 79 (89.8%) |
| Yes | 12 (4.9%) | 10 (5.0%) | 4 (3.6%) | 3 (2.3%) | 2 (5.1%) | 9 (10.2%) |
| Total | 245 | 199 | 111 | 128 | 39 | 88 |
| Suspicious Examiner’s Impression | ||
|---|---|---|
| Number of Suspicious Ultrasound Features * | No | Yes |
| None | 478 (100.0%) | 0 |
| One | 198 (97.5%) | 5 (2.5%) |
| Two | 76 (85.4%) | 13 (14.6%) |
| Three | 15 (64.0%) | 9 (36.0%) |
| Four | 3 (20.0%) | 12 (80.0%) |
| Five | 0 | 1 (100.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabezas, N.; López-Picazo, A.; Diaz, P.; Valero, B.; Rodriguez, M.J.; Redondo, A.; Díaz-de la Noval, B.; Pascual, M.A.; Ajossa, S.; Guerriero, S.; et al. How Frequently Benign Uterine Myomas Appear Suspicious for Sarcoma as Assessed by Transvaginal Ultrasound? Diagnostics 2023, 13, 501. https://doi.org/10.3390/diagnostics13030501
Cabezas N, López-Picazo A, Diaz P, Valero B, Rodriguez MJ, Redondo A, Díaz-de la Noval B, Pascual MA, Ajossa S, Guerriero S, et al. How Frequently Benign Uterine Myomas Appear Suspicious for Sarcoma as Assessed by Transvaginal Ultrasound? Diagnostics. 2023; 13(3):501. https://doi.org/10.3390/diagnostics13030501
Chicago/Turabian StyleCabezas, Nieves, Ana López-Picazo, Patricia Diaz, Beatriz Valero, María José Rodriguez, Ana Redondo, Begoña Díaz-de la Noval, Maria Angela Pascual, Silvia Ajossa, Stefano Guerriero, and et al. 2023. "How Frequently Benign Uterine Myomas Appear Suspicious for Sarcoma as Assessed by Transvaginal Ultrasound?" Diagnostics 13, no. 3: 501. https://doi.org/10.3390/diagnostics13030501






