Gender Differences in Epicardial Adipose Tissue and Plaque Composition by Coronary CT Angiography: Association with Cardiovascular Outcome
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Population
2.2. CCTA Acquisition
2.3. Analysis of CCTA Data, Plaque Parameters, and EAT Volume
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Quantification of EAT Volume and CCTA Plaque Parameters
3.3. Association of EAT Volume and Plaque Parameters with MACE
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
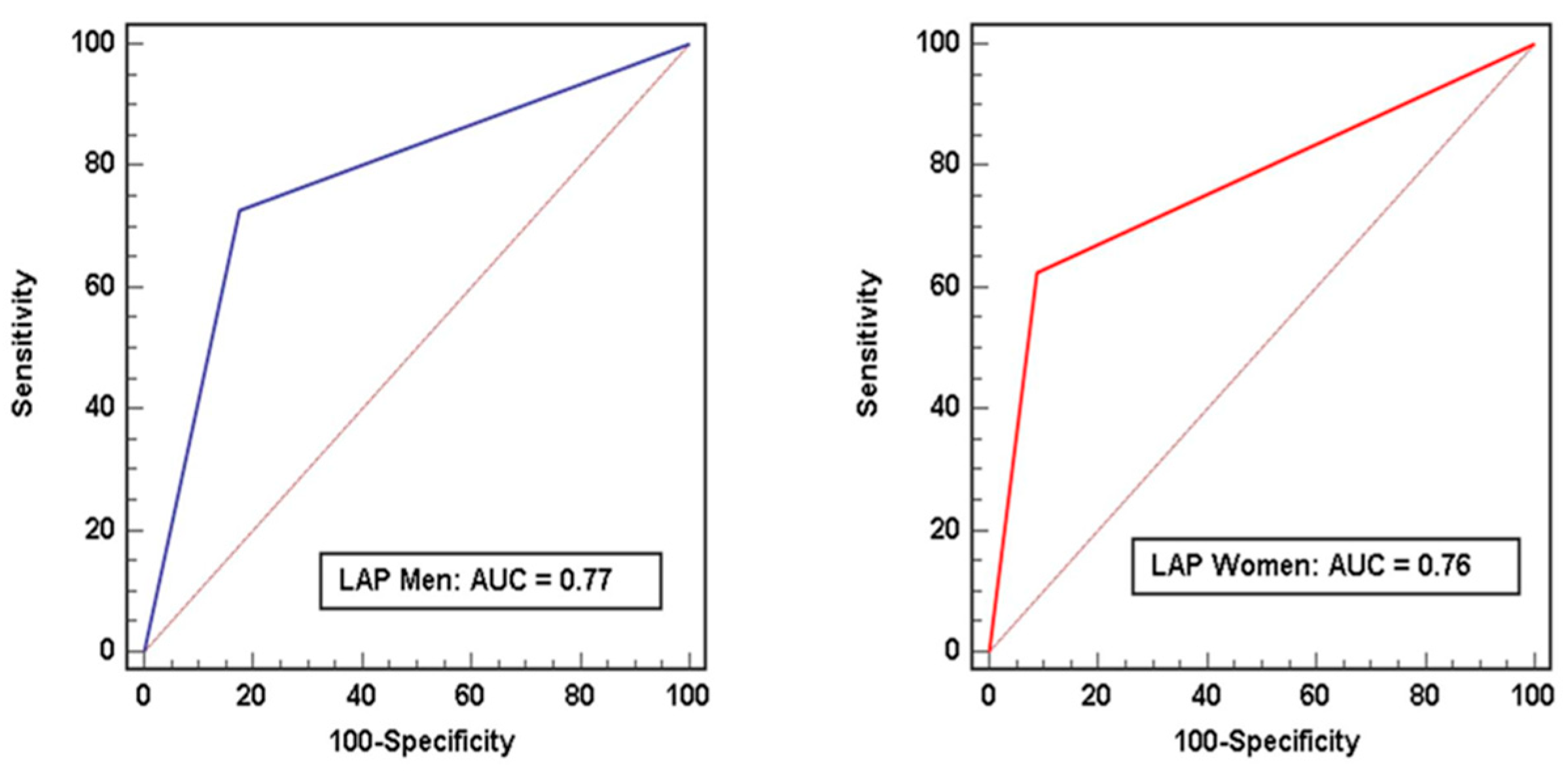
| AUC | Area under the curve |
| CAD | Coronary artery disease |
| CAD-RADS™ | Coronary artery disease reporting and data system |
| CCTA | Coronary CT angiography |
| EAT | Epicardial adipose tissue |
| HR | Hazard ratio |
| HU | Hounsfield unit |
| IQR | Interquartile range |
| MACE | Major adverse cardiovascular events |
| PCAT | Pericoronary adipose tissue |
| RI | Remodeling Index |
| ROC | Receiver-operating characteristics |
| ROI | Region of interest |
References
- Tesche, C.; Plank, F.; De Cecco, C.N.; Duguay, T.M.; Albrecht, M.H.; Varga-Szemes, A.; Bayer, R.R.N.; Yang, J.; Jacks, I.L.; Gramer, B.M.; et al. Prognostic implications of coronary CT angiography-derived quantitative markers for the prediction of major adverse cardiac events. J. Cardiovasc. Comput. Tomogr. 2016, 10, 458–465. [Google Scholar] [CrossRef]
- Thomsen, C.; Abdulla, J. Characteristics of high-risk coronary plaques identified by computed tomographic angiography and associated prognosis: A systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Brandt, V.; Emrich, T.; Schoepf, U.J.; Dargis, D.M.; Bayer, R.R.; De Cecco, C.N.; Tesche, C. Ischemia and outcome prediction by cardiac CT based machine learning. Int. J. Cardiovasc. Imaging 2020, 36, 2429–2439. [Google Scholar] [CrossRef] [PubMed]
- Investigators, S.-H.; Newby, D.E.; Adamson, P.D.; Berry, C.; Boon, N.A.; Dweck, M.R.; Flather, M.; Forbes, J.; Hunter, A.; Lewis, S.; et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N. Engl. J. Med. 2018, 379, 924–933. [Google Scholar] [CrossRef]
- Ferencik, M.; Mayrhofer, T.; Bittner, D.O.; Emami, H.; Puchner, S.B.; Lu, M.T.; Meyersohn, N.M.; Ivanov, A.V.; Adami, E.C.; Patel, M.R.; et al. Use of High-Risk Coronary Atherosclerotic Plaque Detection for Risk Stratification of Patients With Stable Chest Pain: A Secondary Analysis of the PROMISE Randomized Clinical Trial. JAMA Cardiol. 2018, 3, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Lakshmanan, S.; Rezvanizadeh, V.; Budoff, M.J. Comprehensive plaque assessment with serial coronary CT angiography: Translation to bedside. Int. J. Cardiovasc. Imaging 2020, 36, 2335–2346. [Google Scholar] [CrossRef]
- Sato, T.; Minami, Y.; Asakura, K.; Katamine, M.; Kato, A.; Katsura, A.; Muramatsu, Y.; Kakizaki, R.; Nemoto, T.; Hashimoto, T.; et al. Age- and Gender-Related Differences in Coronary Lesion Plaque Composition on Optical Coherence Tomography. Circ. J. 2020, 84, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Sagris, M.; Antonopoulos, A.S.; Simantiris, S.; Oikonomou, E.; Siasos, G.; Tsioufis, K.; Tousoulis, D. Pericoronary fat attenuation index-a new imaging biomarker and its diagnostic and prognostic utility: A systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e526–e536. [Google Scholar] [CrossRef] [PubMed]
- Brandt, V.; Bekeredjian, R.; Schoepf, U.J.; Varga-Szemes, A.; Emrich, T.; Aquino, G.J.; Decker, J.; Bayer, R.R., 2nd; Ellis, L.; Ebersberger, U.; et al. Prognostic value of epicardial adipose tissue volume in combination with coronary plaque and flow assessment for the prediction of major adverse cardiac events. Eur. J. Radiol. 2022, 148, 110157. [Google Scholar] [CrossRef]
- Tesche, C.; Bauer, M.J.; Straube, F.; Rogowski, S.; Baumann, S.; Renker, M.; Fink, N.; Schoepf, U.J.; Hoffmann, E.; Ebersberger, U. Association of epicardial adipose tissue with coronary CT angiography plaque parameters on cardiovascular outcome in patients with and without diabetes mellitus. Atherosclerosis 2022, 363, 78–84. [Google Scholar] [CrossRef]
- Goeller, M.; Achenbach, S.; Duncker, H.; Dey, D.; Marwan, M. Imaging of the Pericoronary Adipose Tissue (PCAT) Using Cardiac Computed Tomography: Modern Clinical Implications. J. Thorac. Imaging 2021, 36, 149–161. [Google Scholar] [CrossRef]
- Bairey Merz, C.N.; Shaw, L.J.; Reis, S.E.; Bittner, V.; Kelsey, S.F.; Olson, M.; Johnson, B.D.; Pepine, C.J.; Mankad, S.; Sharaf, B.L.; et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part II: Gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J. Am. Coll. Cardiol. 2006, 47, S21–S29. [Google Scholar] [CrossRef]
- Plank, F.; Beyer, C.; Friedrich, G.; Wildauer, M.; Feuchtner, G. Sex differences in coronary artery plaque composition detected by coronary computed tomography: Quantitative and qualitative analysis. Neth. Heart J. 2019, 27, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.C.; Kwiecinski, J.; Doris, M.; McElhinney, P.; D’Souza, M.S.; Cadet, S.; Adamson, P.D.; Moss, A.J.; Alam, S.; Hunter, A.; et al. Sex-Specific Computed Tomography Coronary Plaque Characterization and Risk of Myocardial Infarction. JACC Cardiovasc. Imaging 2021, 14, 1804–1814. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Cury, R.C.; Abbara, S.; Achenbach, S.; Agatston, A.; Berman, D.S.; Budoff, M.J.; Dill, K.E.; Jacobs, J.E.; Maroules, C.D.; Rubin, G.D.; et al. CAD-RADS™ Coronary Artery Disease—Reporting and Data System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J. Cardiovasc. Comput. Tomogr. 2016, 10, 269–281. [Google Scholar] [CrossRef]
- Tesche, C.; Caruso, D.; De Cecco, C.N.; Shuler, D.C.; Rames, J.D.; Albrecht, M.H.; Duguay, T.M.; Varga-Szemes, A.; Jochheim, D.; Baquet, M.; et al. Coronary Computed Tomography Angiography-Derived Plaque Quantification in Patients With Acute Coronary Syndrome. Am. J. Cardiol. 2017, 119, 712–718. [Google Scholar] [CrossRef]
- Xie, Z.; Zhu, J.; Li, W.; Liu, L.; Zhuo, K.; Yang, R.; Hu, F. Relationship of epicardial fat volume with coronary plaque characteristics, coronary artery calcification score, coronary stenosis, and CT-FFR for lesion-specific ischemia in patients with known or suspected coronary artery disease. Int. J. Cardiol. 2021, 332, 8–14. [Google Scholar] [CrossRef]
- Yu, W.; Zhang, F.; Liu, B.; Wang, J.; Shao, X.; Yang, M.F.; Yang, X.; Wu, Z.; Li, S.; Shi, Y.; et al. Incremental value of epicardial fat volume to coronary artery calcium score and traditional risk factors for predicting myocardial ischemia in patients with suspected coronary artery disease. J. Nucl. Cardiol. 2021, 29, 1583–1592. [Google Scholar] [CrossRef]
- Park, H.B.; Heo, R.; ó Hartaigh, B.; Cho, I.; Gransar, H.; Nakazato, R.; Leipsic, J.; Mancini, G.B.; Koo, B.K.; Otake, H.; et al. Atherosclerotic plaque characteristics by CT angiography identify coronary lesions that cause ischemia: A direct comparison to fractional flow reserve. JACC Cardiovasc. Imaging 2015, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Kihara, Y.; Kitagawa, T.; Ohashi, N.; Kunita, E.; Iwanaga, Y.; Kobuke, K.; Miyazaki, S.; Kawasaki, T.; Fujimoto, S.; et al. Coronary plaque characteristics in computed tomography and 2-year outcomes: The PREDICT study. J. Cardiovasc. Comput. Tomogr. 2018, 12, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Nasir, K.; Gopal, A.; Blankstein, R.; Ahmadi, N.; Pal, R.; Khosa, F.; Shaw, L.J.; Blumenthal, R.S.; Budoff, M.J. Noninvasive assessment of gender differences in coronary plaque composition with multidetector computed tomographic angiography. Am. J. Cardiol. 2010, 105, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Senoner, T.; Plank, F.; Beyer, C.; Langer, C.; Birkl, K.; Steinkohl, F.; Widmann, G.; Barbieri, F.; Adukauskaite, A.; Friedrich, G.; et al. Gender Differences in the Atherosclerosis Profile by Coronary CTA in Coronary Artery Calcium Score Zero Patients. J. Clin. Med. 2021, 10, 1220. [Google Scholar] [CrossRef] [PubMed]
- Conte, E.; Dwivedi, A.; Mushtaq, S.; Pontone, G.; Lin, F.Y.; Hollenberg, E.J.; Lee, S.E.; Bax, J.; Cademartiri, F.; Chinnaiyan, K.; et al. Age- and sex-related features of atherosclerosis from coronary computed tomography angiography in patients prior to acute coronary syndrome: Results from the ICONIC study. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 24–33. [Google Scholar] [CrossRef]
- Langheim, S.; Dreas, L.; Veschini, L.; Maisano, F.; Foglieni, C.; Ferrarello, S.; Sinagra, G.; Zingone, B.; Alfieri, O.; Ferrero, E.; et al. Increased expression and secretion of resistin in epicardial adipose tissue of patients with acute coronary syndrome. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H746–H753. [Google Scholar] [CrossRef]
- Towfighi, A.; Zheng, L.; Ovbiagele, B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch. Intern Med. 2009, 169, 1762–1766. [Google Scholar] [CrossRef]
- Daly, C.A.; Clemens, F.; Sendon, J.L.; Tavazzi, L.; Boersma, E.; Danchin, N.; Delahaye, F.; Gitt, A.; Julian, D.; Mulcahy, D.; et al. The clinical characteristics and investigations planned in patients with stable angina presenting to cardiologists in Europe: From the Euro Heart Survey of Stable Angina. Eur. Heart J. 2005, 26, 996–1010. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, D.; Hartaigh, B.; Gransar, H.; Lu, Y.; Rizvi, A.; Park, M.W.; Roudsari, H.M.; Stuijfzand, W.J.; Berman, D.S.; et al. Influence of symptom typicality for predicting MACE in patients without obstructive coronary artery disease: From the CONFIRM Registry (Coronary Computed Tomography Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry). Clin. Cardiol. 2018, 41, 586–593. [Google Scholar] [CrossRef]
- Nieman, K.; Hoffmann, U. Cardiac computed tomography in patients with acute chest pain. Eur. Heart J. 2015, 36, 906–914. [Google Scholar] [CrossRef]
- Kunce, J.T. Random Variables and Correlational Overkill. Educ. Psychol. Meas. 1975, 35, 529–534. [Google Scholar] [CrossRef]

| Parameter | Male (n = 220) | Female (n = 132) | p Value |
|---|---|---|---|
| Age (years) | 60.3 ± 10.1 | 66.4 ± 10.5 | 0.001 |
| Body-mass-index (kg/m2) | 27.8 ± 5.7 | 28.8 ± 4.9 | 0.002 |
| Hypertension n (%) | 120 (54%) | 74 (56%) | 0.74 |
| Dyslipidemia n (%) | 95 (43%) | 60 (45%) | 0.65 |
| Tobacco abuse n (%) | 65 (29%) | 31 (24%) | 0.23 |
| Diabetes mellitus n (%) | 41 (18%) | 21 (15%) | 0.89 |
| CAD family history n (%) | 61 (28%) | 34 (26%) | 0.71 |
| Framingham risk score | 10.4 (8.2, 13.6) | 10.2 (7.9, 13.1) | 0.65 |
| Medication at admission | |||
| Aspirin | 74 (33%) | 38 (29%) | 0.48 |
| Statins | 90 (41%) | 50 (38%) | 0.72 |
| Betablocker | 48 (22%) | 24 (18%) | 0.54 |
| ACE inhibitor | 41 (19%) | 22 (17%) | 0.49 |
| Diuretics | 44 (20%) | 21 (16%) | 0.67 |
| Clinical presentation at admission | |||
| No chest pain | 106 (48%) | 54 (41%) | 0.04 |
| Non-cardiac chest pain | 31 (14%) | 24 (18%) | |
| Typical chest pain | 38 (17%) | 14 (11%) | |
| Atypical chest pain | 64 (29%) | 41 (31%) | |
| Parameter | Male (n = 220) | Female (n = 132) | p Value |
|---|---|---|---|
| Agatston score | 17.5 (0.0, 142.1) | 2.8 (0.0, 58.9) | 0.005 |
| Obstructive CAD | 82 (37%) | 33 (25%) | 0.019 |
| EAT volume (cm3/m2) | 50.8 (44.6, 56.8) | 47.7 (43.2, 53.2) | 0.004 |
| Total plaque volume (mm3) | 119.4 (64.2, 182.3) | 100.2 (67.7, 137.3) | 0.016 |
| Calcified plaque volume (mm3) | 26.7 (4.3, 67.0) | 26.1 (5.3, 65.3) | 0.76 |
| Non-calcified plaque volume (mm3) | 90.2 (45.4, 138.2) | 79.7 (43.0, 117.1) | 0.02 |
| Low-attenuation plaque | 51 (23%) | 16 (12%) | 0.011 |
| Spotty calcification | 55 (24%) | 24 (18%) | 0.21 |
| Positive remodeling | 65 (29%) | 26 (19%) | 0.043 |
| Napkin-ring sign | 36 (16%) | 11 (8%) | 0.033 |
| ≥2 high-risk plaque features | 54 (24%) | 17 (13%) | 0.007 |
| 1 vessel CAD | 39 (18%) | 11 (8%) | 0.01 |
| 2 vessel CAD | 24 (11%) | 5 (4%) | |
| 3 vessel CAD | 11 (5%) | 2 (2%) |
| Male | |||
|---|---|---|---|
| Parameter | MACE (n = 22) | No MACE (n = 198) | p Value |
| Agatston score | 690 (181, 2112) | 11 (1.0, 97.3) | <0.001 |
| Obstructive CAD | 19 (86%) | 63 (32%) | <0.001 |
| EAT volume (cm3/m2) | 57.8 (53.2, 64.4) | 50.3 (44.6, 55.8) | 0.002 |
| Total plaque volume (mm3) | 129.4 (94.2, 153.5) | 112.0 (58.8, 184.9) | 0.034 |
| Calcified plaque volume (mm3) | 11.4 (3.5, 54.1) | 29.4 (3.2, 67.0) | 0.57 |
| Non-calcified plaque volume (mm3) | 115.8 (94.9, 156.3) | 89.6 (44.8, 136.7) | 0.037 |
| Low-attenuation plaque | 16 (72%) | 35 (17%) | <0.001 |
| Spotty calcification | 13 (59%) | 40 (20%) | <0.001 |
| Positive remodeling | 13 (59%) | 52 (26%) | 0.015 |
| Napkin-ring sign | 11 (50%) | 25 (13%) | <0.001 |
| ≥2 high-risk plaque features | 15 (68%) | 40 (20%) | <0.001 |
| Female | |||
| Parameter | MACE (n = 8) | No MACE (n = 124) | p Value |
| Agatston score | 12.1 (59.9, 389.5) | 1.2 (0.0, 48.0) | 0.003 |
| Obstructive CAD | 6 (75%) | 27 (22%) | 0.82 |
| EAT volume (cm3/m2) | 53.0 (45.3, 59.8) | 47.6 (42.5, 53.1) | 0.018 |
| Total plaque volume (mm3) | 147.3 (112.1, 171.6) | 98.8 (63.9, 132.8) | 0.018 |
| Calcified plaque volume (mm3) | 10.7 (5.3, 51.6) | 30.7 (5.3, 65.3) | 0.74 |
| Non-calcified plaque volume (mm3) | 119.9 (82.9, 141.3) | 77.3 (42.6, 115.9) | 0.041 |
| Low-attenuation plaque | 5 (63%) | 11 (9%) | <0.001 |
| Spotty calcification | 5 (63%) | 19 (15%) | 0.008 |
| Positive remodeling | 5 (63%) | 21 (17%) | 0.002 |
| Napkin-ring sign | 3 (38%) | 8 (6%) | 0.002 |
| ≥2 high-risk plaque features | 6 (75%) | 11 (9%) | <0.001 |
| Parameter | Univariable Analysis Hazard Ratio 95% CI p Value | Multivariable Analysis Hazard Ratio 95% CI p Value | ||||
|---|---|---|---|---|---|---|
| Male | ||||||
| Agatston score | 1.001 | 1.007–1.002 | 0.001 | 1.0008 | 1.0002–1.0014 | 0.014 |
| Obstructive CAD | 13.67 | 3.91–47.93 | 0.001 | - | - | - |
| EAT volume | 1.09 | 1.04–1.15 | 0.007 | 1.067 | 1.001–1.14 | 0.049 |
| Total plaque volume | 1.00 | 0.99–1.006 | 0.69 | - | - | - |
| Calcified plaque volume | 0.99 | 0.98–1.005 | 0.53 | - | - | - |
| Non-calcified plaque volume | 1.004 | 0.99–1.01 | 0.15 | - | - | - |
| Low-attenuation plaque | 12.49 | 4.56–34.19 | 0.001 | 3.82 | 1.02–14.34 | 0.036 |
| Spotty calcification | 5.74 | 2.29–14.37 | 0.002 | - | - | - |
| Positive remodeling | 4.08 | 1.65–10.11 | 0.002 | - | - | - |
| Napkin-ring sign | 6.96 | 2.73–17.73 | 0.001 | - | - | - |
| ≥2 high-risk features | 8.52 | 3.26–22.28 | 0.001 | - | - | - |
| Female | ||||||
| Agatston score | 1.001 | 0.99–1.002 | 0.26 | - | - | - |
| Obstructive CAD | 10.7 | 2.05–56.4 | 0.004 | - | - | - |
| EAT volume | 1.08 | 0.99–1.18 | 0.06 | - | - | - |
| Total plaque volume | 1.01 | 1.001–1.02 | 0.04 | - | - | - |
| Calcified plaque volume | 1.007 | 0.99–1.01 | 0.12 | - | - | - |
| Non-calcified plaque volume | 1.02 | 0.99–1.03 | 0.08 | - | - | - |
| Low-attenuation plaque | 17.12 | 3.59–81.4 | 0.004 | 2.42 | 1.06–11.75 | 0.041 |
| Spotty calcification | 9.21 | 2.03–41.78 | 0.004 | - | - | - |
| Positive remodeling | 8.17 | 1.81–36.86 | 0.006 | - | - | - |
| Napkin-ring sign | 8.70 | 1.75–43.12 | 0.008 | - | - | - |
| ≥2 high-risk features | 30.81 | 5.54–171.42 | 0.001 | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ebersberger, U.; Bauer, M.J.; Straube, F.; Fink, N.; Schoepf, U.J.; Varga-Szemes, A.; Emrich, T.; Griffith, J.; Hoffmann, E.; Tesche, C. Gender Differences in Epicardial Adipose Tissue and Plaque Composition by Coronary CT Angiography: Association with Cardiovascular Outcome. Diagnostics 2023, 13, 624. https://doi.org/10.3390/diagnostics13040624
Ebersberger U, Bauer MJ, Straube F, Fink N, Schoepf UJ, Varga-Szemes A, Emrich T, Griffith J, Hoffmann E, Tesche C. Gender Differences in Epicardial Adipose Tissue and Plaque Composition by Coronary CT Angiography: Association with Cardiovascular Outcome. Diagnostics. 2023; 13(4):624. https://doi.org/10.3390/diagnostics13040624
Chicago/Turabian StyleEbersberger, Ullrich, Maximilian J. Bauer, Florian Straube, Nicola Fink, U. Joseph Schoepf, Akos Varga-Szemes, Tilman Emrich, Joseph Griffith, Ellen Hoffmann, and Christian Tesche. 2023. "Gender Differences in Epicardial Adipose Tissue and Plaque Composition by Coronary CT Angiography: Association with Cardiovascular Outcome" Diagnostics 13, no. 4: 624. https://doi.org/10.3390/diagnostics13040624
APA StyleEbersberger, U., Bauer, M. J., Straube, F., Fink, N., Schoepf, U. J., Varga-Szemes, A., Emrich, T., Griffith, J., Hoffmann, E., & Tesche, C. (2023). Gender Differences in Epicardial Adipose Tissue and Plaque Composition by Coronary CT Angiography: Association with Cardiovascular Outcome. Diagnostics, 13(4), 624. https://doi.org/10.3390/diagnostics13040624








