Dynamic Computed Tomography Angiography as Imaging Method for Endoleak Classification after Endovascular Aneurysm Repair: A Case Series and Systematic Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
2.1. Imaging Protocol for Surveillance
2.2. Dose Length Product
2.3. Endoleak Classification
3. Systematic Review
3.1. Protocol and Eligibility Criteria
3.2. Search Strategy
3.3. Study Selection, Data Extraction, and Quality Assessment
3.4. Statistics
4. Results
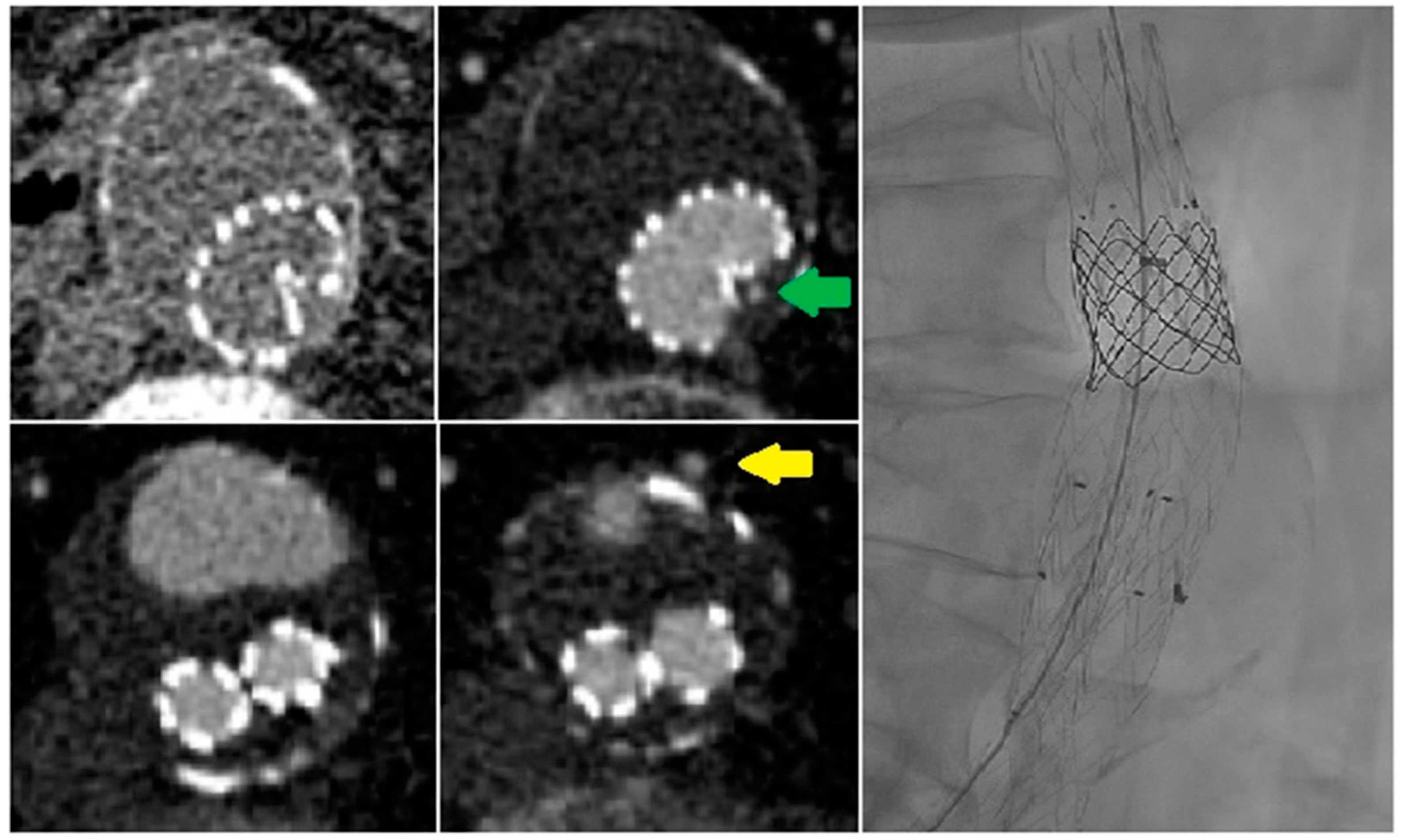
4.1. Time Attenuation Curves
4.2. Systematic Review
4.2.1. Acquisition Protocols
4.2.2. dCTA versus CE-DUS
4.2.3. dCTA versus sCTA
4.2.4. dCTA versus DSA
5. Discussion
5.1. Radiation Exposure
5.2. Timing of the Phases in the dCTA Protocol
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Charisis, N.; Bouris, V.; Conway, A.M.; Labropoulos, N. A Systematic Review and Pooled Meta-Analysis on the Incidence and Temporal Occurrence of Type II Endoleak Following an Abdominal Aortic Aneurysm Repair. Ann. Vasc. Surg. 2021, 75, 406–419. [Google Scholar] [CrossRef] [PubMed]
- Wanhainen, A.; Verzini, F.; van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Bashir, M.R.; Ferral, H.; Jacobs, C.; McCarthy, W.; Goldin, M. Endoleaks after endovascular abdominal aortic aneurysm repair: Management strategies according to CT findings. Am. J. Roentgenol. 2009, 192, W178–W186. [Google Scholar] [CrossRef] [PubMed]
- Mirza, T.A.; Karthikesalingam, A.; Jackson, D.; Walsh, S.R.; Holt, P.J.; Hayes, P.D.; Boyle, J. Duplex Ultrasound and Contrast-Enhanced Ultrasound Versus Computed Tomography for the Detection of Endoleak after EVAR: Systematic Review and Bivariate Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Sommer, W.H.; Becker, C.R.; Haack, M.; Rubin, G.D.; Weidenhagen, R.; Schwarz, F.; Nikolaou, K.; Reiser, M.F.; Johnson, T.R.; Clevert, D.A. Time-resolved CT angiography for the detection and classification of endoleaks. Radiology 2012, 263, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Tarulli, M.; Tan, K.T.; Lindsay, T.; Mahmood, D.N.; Santiago, S.; Jaberi, A.; Mafeld, S. Utility of 4D CT in endoleak characterization after advanced endovascular aortic repair. Vascular 2022, 2022, 170853812211053. [Google Scholar] [CrossRef] [PubMed]
- Hou, K.; Zhu, T.; Zhang, W.; Zeng, M.; Guo, D.; Fu, W.; Si, Y. Dynamic Volumetric Computed Tomography Angiography Is a Preferred Method for Unclassified Endoleaks by Conventional Computed Tomography Angiography After Endovascular Aortic Repair. J. Am. Heart Assoc. 2019, 8, e012011. [Google Scholar] [CrossRef] [PubMed]
- Apfaltrer, G.; Lavra, F.; Joseph Schoepf, U.; Scarabello, M.; Yamada, R.; van Assen, M.; Jacobs, B.E.; Bauer, M.J.; Greenberg, W.T.; Varga-Szemes, A.; et al. Quantitative analysis of dynamic computed tomography angiography for the detection of endoleaks after abdominal aorta aneurysm endovascular repair: A feasibility study. PLoS ONE 2021, 16, e0245134. [Google Scholar] [CrossRef] [PubMed]
- Berczeli, M.; Chinnadurai, P.; Legeza, P.; Peden, E.K.; Bavare, C.S.; Chang, S.M.; Lumsden, A.B. Dynamic, Time-Resolved CT Angiography After EVAR: A Quantitative Approach to Accurately Characterize Aortic Endoleak Type and Identify Inflow Vessels. J. Endovasc. Ther. 2022, 30, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Waldeck, S.; Overhoff, D.; Brockmann, M.A.; Becker, B.V. Detection of Endoleaks Following Thoracic and Abdominal Aortic Endovascular Aortic Repair—: A Comparison of Standard and Dynamic 4D-Computed Tomography Angiography. J. Endovasc. Ther. 2022, 152660282210953. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 105906. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. Quadas-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Rydberg, J.; Lalka, S.; Johnson, M.; Cikrit, D.; Dalsing, M.; Sawchuk, A.; Shafique, S. Characterization of endoleaks by dynamic computed tomographic angiography. Am. J. Surg. 2004, 188, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Lehmkuhl, L.; Andres, C.; Lücke, C.; Hoffmann, J.; Foldyna, B.; Grothoff, M.; Nitzsche, S.; Schmidt, A.; Ulrich, M.; Scheinert, D.; et al. Dynamic CT angiography after abdominal aortic endovascular aneurysm repair: Influence of enhancement patterns and optimal bolus timing on endoleak detection. Radiology 2013, 268, 890–899. [Google Scholar] [CrossRef] [PubMed]
- Sommer, W.H.; Clevert, D.A.; Bamberg, F.; Helck, A.; Albrecht, E.; Reiser, M.F.; Becker, C.R.; Nikolaou, K. Time-resolved Computed Tomography Imaging of the Aorta A Feasibility Study. J. Thorac. Imaging 2010, 25, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Koike, Y.; Ishida, K.; Hase, S.; Kobayashi, Y.; Nishimura, J.I.; Yamasaki, M.; Hosaka, N. Dynamic Volumetric CT Angiography for the Detection and Classification of Endoleaks: Application of Cine Imaging Using a 320-Row CT Scanner with 16-cm Detectors. J. Vasc. Interv. Radiol. 2014, 25, 1172–1180.e1. [Google Scholar] [CrossRef] [PubMed]




| Patient No. | Age (Years) | Sex | Initial Diameter (mm) | Diameter Increase (mm) | Time after Initial Operation (months) | Endoleak Classification on sCTA | Indication for dCTA | Endoleak Classification on dCTA |
|---|---|---|---|---|---|---|---|---|
| 1 | 78 | Male | 58 | +1 | 18 | 1× type II, 1× undefined | Undefined EL (type Ia or II) | 2× type II |
| 2 | 77 | Male | 56 | +20 | 39 | 1× undefined | Undefined EL (type Ia or II) | 1× type II |
| 3 | 88 | Male | 57 | +10 | 129 | None | AAA diameter increase without an endoleak | 1× type IIIb |
| 4 | 84 | Male | 59 | +10 | 54 | 1× undefined | Undefined EL (type Ia or II) | 1× type II |
| 5 | 83 | Female | 57 | +8 | 9 | 1× undefined | Undefined EL (type Ia or II) | 1× type IIIb |
| 6 | 87 | Male | 59 | +7 | 81 | 1× type II | AAA diameter increase with unclear origin of type II EL | 2× type II |
| 7 | 74 | Male | 74 | +8 | 85 | 1× type II | AAA diameter increase without an endoleak | 2× type II |
| 8 | 84 | Male | 59 | +1 | 62 | 1× undefined | Undefined EL (type Ib or II) | 3× type II |
| 9 | 67 | Male | 38 | +8 | 34 | 1× type II | AAA diameter increase with unclear origin of type II EL | 1× type II |
| 10 | 78 | Male | 57 | None | 15 | 1× undefined | Undefined EL (type Ia, II or III) | 1× type II |
| 11 | 66 | Male | 53 | +3 | 3 | 1× undefined | Undefined EL (type II or III) | 1× type II |
| 12 | 89 | Female | 54 | +12 | 93 | None | AAA diameter increase without an endoleak | None |
| 13 | 73 | Male | 62 | +8 | 25 | 1× undefined | Undefined EL (type II or III) | 1× type II |
| 14 | 83 | Male | 56 | +6 | 35 | 1× undefined | Undefined EL (type Ia or II) | 1× type II |
| 15 | 73 | Female | 54 | None | 8 | 1× undefined | Undefined EL (type Ia or II) | 1× type Ia |
| 16 | 66 | Male | 49 | +2 | 74 | 1× undefined | Undefined EL (type II or III) | 1× type IIIb |
| Patient No. | Endoleak | Branch | Peak Stent (HU) | Peak Endoleak | Peak Endoleak/ Stent (%) | Time Peak Stent (s) | Time Peak Endoleak (s) |
|---|---|---|---|---|---|---|---|
| 1 | 2× type II | AMI | 348.8 | 332.4 | 95.3 | 20.6 | 28.9 |
| L1 | 348.8 | 333.6 | 95.6 | 20.6 | 28.6 | ||
| 2 | 1× type II | L1 | 370.9 | 304.1 | 82 | 28.5 | 33.3 |
| 3 | 1× type IIIb | 459.9 | 425.8 | 92.6 | 25.6 | 28.9 | |
| 4 | 1× type II | L1 | 401.2 | 252.1 | 62.8 | 23.6 | 33.4 |
| 5 | 1× type IIIc | NA | NA | NA | NA | NA | |
| 6 | 2× type II | AII | 607.4 | 268.3 | 44.2 | 33.4 | MAX * |
| L1 | 607.4 | 323.6 | 53.3 | 33.4 | MAX * | ||
| 7 | 2× type II | L1 | 538.9 | 186.6 | 34.6 | 28.6 | MAX * |
| L2 | 538.9 | 171 | 31.7 | 28.6 | MAX * | ||
| 8 | 3× type II | AMI | 496.1 | 350 | 70.6 | MAX * | MAX * |
| L1 | 496.1 | 341.7 | 68.9 | MAX * | MAX * | ||
| L2 | 496.1 | 138.8 | 28 | MAX * | MAX * | ||
| 9 | 1× type II | L1 | 549.9 | 232.6 | 42.3 | 23.5 | 33.5 |
| 10 | 1× type II | NA | NA | NA | NA | NA | NA |
| 11 | 1× type II | NA | NA | NA | NA | NA | NA |
| 12 | None | NA | NA | NA | NA | NA | |
| 13 | 1× type II | L1 | 473.1 | 413 | 87.3 | 24.2 | 30.5 |
| 14 | 1× type II | L1 | 306.1 | 78.1 | 25.5 | 30.8 | 38.5 |
| 15 | 1× type Ia | 466 | 408.6 | 87.7 | 18.8 | 23.7 | |
| 16 | 1× type IIIb | 473.1 | 413.4 | 87.4 | 28.4 | 33.5 |
| Author | Year | No. | Type of Study | dCTA vs. | CT Scanner Type | Scan Duration (s) | No. of Phases | Contrast (mL) | Test Bolus | Tube Voltage (kVp) | Tube Current-Time Product (mAs) | Range (cm) | DLP * (mGy*cm) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sommer et al. [5] | 2012 | 54 | Prospective | CE-DUS | 128-section Somatom Definition AS+ (Siemens) | 30–60 | 12 | 60 | No | 80 | 120 | 27 | 952 ± 42 |
| Hou et al. [7] | 2019 | 12 | Prospective | DSA | 320-row detector (Aquilion One, Toshiba) | 24–32 | 12–16 | 55–74 | Yes | 80 | 120 | 16 | 505–566 |
| Apfaltrer et al. [8] | 2020 | 19 | Retrospective | sCTA | Third-generation, dual-source (Siemens) | NA | 12 | 50 | No | 70 | 200 | NA | 1064–1065 |
| Berczeli et al. [9] | 2022 | 24 | Retrospective | DSA | Third-generation, dual-source (Siemens) | 39 | 10–12 | 70–90 | Yes | 84–110 | 150 | NA | 1038 ± 533 |
| Tarulli et al. [6] | 2022 | 13 | Retrospective | sCTA | 320-row detector (Aquilion One, Toshiba) | 120 | 10–40 | 70–160 | Yes | 100 | 175 ** | 16 | 4724 (1108–11,069) |
| Waldeck et al. [10] | 2022 | 69 | Retrospective | sCTA | 320-row detector (Aquilion One, Toshiba) | 14 | 10 | 60–70 | Yes | 90 | adaptive | 36 | 856 ± 55 |
| Current series | 2022 | 16 | Retrospective | sCTA and DSA | Second-generation, dual-source (Siemens) | 41.2 | 16 | 100 | No | 80 | 151 ± 3.5 | 28.4 | 1524 ± 139 |
| Study | Risk of Bias | Applicability Concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Patient Selection | Index Test | |
| Sommer et al. [5] |  |  |  |  |  |  |  |
| Hou et al. [7] |  |  |  |  |  |  |  |
| Apfaltrer et al. [8] |  |  |  |  |  |  |  |
| Berczeli et al. [9] |  |  |  |  |  |  |  |
| Tarulli et al. [6] |  |  |  |  |  |  |  |
| Waldeck et al. [10] |  |  |  |  |  |  |  |
 Low Risk Low Risk  High Risk High Risk | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boer, G.J.; van Engen, L.A.H.; van Dam, L.; van de Luijtgaarden, K.M.; Bokkers, R.P.H.; de Vries, J.-P.P.M.; Fioole, B. Dynamic Computed Tomography Angiography as Imaging Method for Endoleak Classification after Endovascular Aneurysm Repair: A Case Series and Systematic Review of the Literature. Diagnostics 2023, 13, 829. https://doi.org/10.3390/diagnostics13050829
Boer GJ, van Engen LAH, van Dam L, van de Luijtgaarden KM, Bokkers RPH, de Vries J-PPM, Fioole B. Dynamic Computed Tomography Angiography as Imaging Method for Endoleak Classification after Endovascular Aneurysm Repair: A Case Series and Systematic Review of the Literature. Diagnostics. 2023; 13(5):829. https://doi.org/10.3390/diagnostics13050829
Chicago/Turabian StyleBoer, Gert Jan, Ludo A. H. van Engen, Lievay van Dam, Koen M. van de Luijtgaarden, Reinoud P. H. Bokkers, Jean-Paul P. M. de Vries, and Bram Fioole. 2023. "Dynamic Computed Tomography Angiography as Imaging Method for Endoleak Classification after Endovascular Aneurysm Repair: A Case Series and Systematic Review of the Literature" Diagnostics 13, no. 5: 829. https://doi.org/10.3390/diagnostics13050829
APA StyleBoer, G. J., van Engen, L. A. H., van Dam, L., van de Luijtgaarden, K. M., Bokkers, R. P. H., de Vries, J.-P. P. M., & Fioole, B. (2023). Dynamic Computed Tomography Angiography as Imaging Method for Endoleak Classification after Endovascular Aneurysm Repair: A Case Series and Systematic Review of the Literature. Diagnostics, 13(5), 829. https://doi.org/10.3390/diagnostics13050829






