Solving STODS—Surgical Temporary Ocular Discomfort Syndrome
Abstract
:1. Introduction
2. The Importance of Preoperative Optimization
3. Key Elements to Preoperative Evaluation
4. Molecular Changes in Ocular Surface Abnormality and during Refractive Surgery
5. Methods for Preop Ocular Surface Optimization
6. Intraoperative Management
7. Postoperative Management of STODS
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Souza, S.; Annavajjhala, S.; Thakur, P.; Mullick, R.; Tejal, S.; Shetty, N. Study of Tear Film Optics and Its Impact on Quality of Vision. Indian J. Ophthalmol. 2020, 68, 2899. [Google Scholar] [CrossRef]
- FDA. Laser-Assisted In Situ Keratomileusis (LASIK) Lasers—Patient Labeling Recommendations Draft Guidance for Industry and Food and Drug Administration Staff; FDA: Silver Spring, MD, USA, 2022. [Google Scholar]
- Lee, B.H.; McLaren, J.W.; Erie, J.C.; Hodge, D.O.; Bourne, W.M. Reinnervation in the Cornea after LASIK. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3660–3664. [Google Scholar]
- Pflugfelder, S.C.; Stern, M.E. Biological Functions of Tear Film. Exp. Eye Res. 2020, 197, 108115. [Google Scholar] [CrossRef]
- Trattler, W.B.; Majmudar, P.A.; Donnenfeld, E.D.; McDonald, M.B.; Stonecipher, K.G.; Goldberg, D.F. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) Study: The Effect of Dry Eye. Clin. Ophthalmol. 2017, 11, 1423–1430. [Google Scholar] [CrossRef] [Green Version]
- Nibandhe, A.S.; Donthineni, P.R. Understanding and Optimizing Ocular Biometry for Cataract Surgery in Dry Eye Disease: A Review. Semin. Ophthalmol. 2022, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Goto, E.; Yagi, Y.; Matsumoto, Y.; Tsubota, K. Impaired Functional Visual Acuity of Dry Eye Patients. Am. J. Ophthalmol. 2002, 133, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Alio, J.L.; Plaza-Puche, A.B.; Férnandez-Buenaga, R.; Pikkel, J.; Maldonado, M. Multifocal Intraocular Lenses: An Overview. Surv. Ophthalmol. 2017, 62, 611–634. [Google Scholar] [CrossRef] [PubMed]
- Donnenfeld, E.D.; Solomon, R.; Roberts, C.W.; Wittpenn, J.R.; McDonald, M.B.; Perry, H.D. Cyclosporine 0.05% to Improve Visual Outcomes after Multifocal Intraocular Lens Implantation. J. Cataract Refract. Surg. 2010, 36, 1095–1100. [Google Scholar] [CrossRef]
- Woodward, M.A.; Randleman, B.J.; Stulting, D.R. Dissatisfaction after Multifocal Intraocular Lens Implantation. J. Cataract Refract. Surg. 2009, 35, 992–997. [Google Scholar] [CrossRef] [Green Version]
- Carones, F. Residual Astigmatism Threshold and Patient Satisfaction with Bifocal, Trifocal and Extended Range of Vision Intraocular Lenses (IOLs). Open J. Ophthalmol. 2017, 7, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Gupta, P.K.; Drinkwater, O.J.; VanDusen, K.W.; Brissette, A.R.; Starr, C.E. Prevalence of Ocular Surface Dysfunction in Patients Presenting for Cataract Surgery Evaluation. J. Cataract Refract. Surg. 2018, 44, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Chou, Y.; Hao, R.; Jiang, X.; Liu, Y.; Li, X. Evaluation of Ocular Surface Impairment in Meibomian Gland Dysfunction of Varying Severity Using a Comprehensive Grading Scale. Medicine 2019, 98, e16547. [Google Scholar] [CrossRef]
- Doughty, M.J. Fluorescein-Tear Breakup Time as an Assessment of Efficacy of Tear Replacement Therapy in Dry Eye Patients: A Systematic Review and Meta-Analysis. Ocul. Surf. 2014, 12, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Vidas Pauk, S. Noninvasive Tear Film Break-Up Time Assessment Using Handheld Lipid Layer Examination Instrument. ACC 2019, 58, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Kojima, T.; Dogru, M.; Kawashima, M.; Nakamura, S.; Tsubota, K. Advances in the Diagnosis and Treatment of Dry Eye. Prog. Retin. Eye Res. 2020, 78, 100842. [Google Scholar] [CrossRef] [PubMed]
- Ishrat, S.; Nema, N.; Chandravanshi, S.C.L. Incidence and Pattern of Dry Eye after Cataract Surgery. Saudi J. Ophthalmol. 2019, 33, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Wellik, S.R. Glaucoma and Dry Eye Syndrome: Double Trouble. In Dry Eye Disease; Elsevier: Amsterdam, The Netherlands, 2023; pp. 147–152. [Google Scholar] [CrossRef]
- Han, K.E.; Yoon, S.C.; Ahn, J.M.; Nam, S.M.; Stulting, R.D.; Kim, E.K.; Seo, K.Y. Evaluation of Dry Eye and Meibomian Gland Dysfunction After Cataract Surgery. Am. J. Ophthalmol. 2014, 157, 1144–1150.e1. [Google Scholar] [CrossRef]
- Kato, K.; Miyake, K.; Hirano, K.; Kondo, M. Management of Postoperative Inflammation and Dry Eye After Cataract Surgery. Cornea 2019, 38, S25–S33. [Google Scholar] [CrossRef]
- Li, X.-M.; Hu, L.; Hu, J.; Wang, W. Investigation of Dry Eye Disease and Analysis of the Pathogenic Factors in Patients after Cataract Surgery. Cornea 2007, 26 (Suppl. S1), S16–S20. [Google Scholar] [CrossRef]
- Pflugfelder, S.C. Anti-Inflammatory Therapy of Dry Eye. Ocul. Surf. 2003, 1, 31–36. [Google Scholar] [CrossRef]
- Stern, M.E.; Gao, J.; Schwalb, T.A.; Ngo, M.; Tieu, D.D.; Chan, C.-C.; Reis, B.L.; Whitcup, S.M.; Thompson, D.; Smith, J.A. Conjunctival T-Cell Subpopulations in Sjögren’s and Non-Sjögren’s Patients with Dry Eye. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2609–2614. [Google Scholar]
- Solomon, A.; Dursun, D.; Liu, Z.; Xie, Y.; Macri, A.; Pflugfelder, S.C. Pro- and Anti-Inflammatory Forms of Interleukin-1 in the Tear Fluid and Conjunctiva of Patients with Dry-Eye Disease. Investig. Ophthalmol. Vis. Sci. 2001, 42, 2283–2292. [Google Scholar]
- Li, D.-Q.; Luo, L.; Chen, Z.; Kim, H.-S.; Song, X.J.; Pflugfelder, S.C. JNK and ERK MAP Kinases Mediate Induction of IL-1beta, TNF-Alpha and IL-8 Following Hyperosmolar Stress in Human Limbal Epithelial Cells. Exp. Eye Res. 2006, 82, 588–596. [Google Scholar] [CrossRef] [Green Version]
- Fu, R.; Klinngam, W.; Heur, M.; Edman, M.C.; Hamm-Alvarez, S.F. Tear Proteases and Protease Inhibitors: Potential Biomarkers and Disease Drivers in Ocular Surface Disease. Eye Contact Lens 2020, 46 (Suppl. S2), S70–S83. [Google Scholar] [CrossRef]
- Willis, K.A.; Postnikoff, C.K.; Freeman, A.; Rezonzew, G.; Nichols, K.; Gaggar, A.; Lal, C.V. The Closed Eye Harbours a Unique Microbiome in Dry Eye Disease. Sci. Rep. 2020, 10, 12035. [Google Scholar] [CrossRef]
- Lee, S.H.; Oh, D.H.; Jung, J.Y.; Kim, J.C.; Jeon, C.O. Comparative Ocular Microbial Communities in Humans with and without Blepharitis. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5585–5593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, X.; Deng, A.; Yang, J.; Bai, H.; Yang, Z.; Wu, J.; Lv, H.; Li, X.; Wen, T. Pathogens in the Meibomian Gland and Conjunctival Sac: Microbiome of Normal Subjects and Patients with Meibomian Gland Dysfunction. Infect. Drug Resist. 2018, 11, 1729–1740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, J.E.; Moore, J.E.; Jiru, X.; Moore, J.E.; Goodall, E.A.; Dooley, J.S.G.; Hayes, V.E.A.; Dartt, D.A.; Downes, C.S.; Moore, T.C.B. Ocular Pathogen or Commensal: A PCR-Based Study of Surface Bacterial Flora in Normal and Dry Eyes. Investig. Ophthalmol. Vis. Sci. 2007, 48, 5616–5623. [Google Scholar] [CrossRef] [PubMed]
- Bandeira, F.; Yusoff, N.Z.; Yam, G.H.-F.; Mehta, J.S. Corneal Re-Innervation Following Refractive Surgery Treatments. Neural. Regen. Res. 2019, 14, 557–565. [Google Scholar] [CrossRef]
- Pérez-Santonja, J.J.; Sakla, H.F.; Cardona, C.; Chipont, E.; Alió, J.L. Corneal Sensitivity after Photorefractive Keratectomy and Laser in Situ Keratomileusis for Low Myopia. Am. J. Ophthalmol. 1999, 127, 497–504. [Google Scholar] [CrossRef]
- Lee, H.K.; Lee, K.S.; Kim, H.C.; Lee, S.H.; Kim, E.K. Nerve Growth Factor Concentration and Implications in Photorefractive Keratectomy vs Laser in Situ Keratomileusis. Am. J. Ophthalmol. 2005, 139, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Nejima, R.; Miyata, K.; Tanabe, T.; Okamoto, F.; Hiraoka, T.; Kiuchi, T.; Oshika, T. Corneal Barrier Function, Tear Film Stability, and Corneal Sensation after Photorefractive Keratectomy and Laser in Situ Keratomileusis. Am. J. Ophthalmol. 2005, 139, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Darwish, T.; Brahma, A.; O’Donnell, C.; Efron, N. Subbasal Nerve Fiber Regeneration after LASIK and LASEK Assessed by Noncontact Esthesiometry and in Vivo Confocal Microscopy: Prospective Study. J. Cataract Refract Surg. 2007, 33, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Latvala, T.; Linna, T.; Tervo, T. Corneal Nerve Recovery after Photorefractive Keratectomy and Laser in Situ Keratomileusis. Int. Ophthalmol. Clin. 1996, 36, 21–27. [Google Scholar] [CrossRef]
- Feng, Y.; Yu, J.; Wang, D.; Li, J.; Huang, J.; Shi, J.; Ye, T.; Wang, Q.; Zhao, Y. The Effect of Hinge Location on Corneal Sensation and Dry Eye after LASIK: A Systematic Review and Meta-Analysis. Graefes. Arch. Clin. Exp. Ophthalmol. 2013, 251, 357–366. [Google Scholar] [CrossRef]
- Linna, T.U.; Vesaluoma, M.H.; Pérez-Santonja, J.J.; Petroll, W.M.; Alió, J.L.; Tervo, T.M. Effect of Myopic LASIK on Corneal Sensitivity and Morphology of Subbasal Nerves. Investig. Ophthalmol. Vis. Sci. 2000, 41, 393–397. [Google Scholar]
- Nettune, G.R.; Pflugfelder, S.C. Post-LASIK Tear Dysfunction and Dysesthesia. Ocul. Surf. 2010, 8, 135–145. [Google Scholar] [CrossRef] [Green Version]
- Calvillo, M.P.; McLaren, J.W.; Hodge, D.O.; Bourne, W.M. Corneal Reinnervation after LASIK: Prospective 3-Year Longitudinal Study. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3991–3996. [Google Scholar] [CrossRef]
- Patel, D.V.; McGhee, C.N.J. In Vivo Confocal Microscopy of Human Corneal Nerves in Health, in Ocular and Systemic Disease, and Following Corneal Surgery: A Review. Br. J. Ophthalmol. 2009, 93, 853–860. [Google Scholar] [CrossRef] [Green Version]
- Chao, C.; Stapleton, F.; Zhou, X.; Chen, S.; Zhou, S.; Golebiowski, B. Structural and Functional Changes in Corneal Innervation after Laser in Situ Keratomileusis and Their Relationship with Dry Eye. Graefes. Arch. Clin. Exp. Ophthalmol. 2015, 253, 2029–2039. [Google Scholar] [CrossRef]
- Erie, J.C.; McLaren, J.W.; Hodge, D.O.; Bourne, W.M. Recovery of Corneal Subbasal Nerve Density after PRK and LASIK. Am. J. Ophthalmol. 2005, 140, 1059–1064. [Google Scholar] [CrossRef]
- Sekundo, W.; Kunert, K.S.; Blum, M. Small Incision Corneal Refractive Surgery Using the Small Incision Lenticule Extraction (SMILE) Procedure for the Correction of Myopia and Myopic Astigmatism: Results of a 6 Month Prospective Study. Br. J. Ophthalmol. 2011, 95, 335–339. [Google Scholar] [CrossRef]
- Toto, L.; Calienno, R.; Curcio, C.; Mattei, P.A.; Mastropasqua, A.; Lanzini, M.; Mastropasqua, L. Induced Inflammation and Apoptosis in Femtosecond Laser-Assisted Capsulotomies and Manual Capsulorhexes: An Immunohistochemical Study. J. Refract. Surg. 2015, 31, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Li, Y.; Wang, Z.; Jiang, Y.; Jin, Y. Comparison of corneal nerve regeneration and dry eye condition after conventional LASIK and femtosecond-assisted LASIK. Zhonghua Yan Ke Za Zhi 2015, 51, 188–192. [Google Scholar] [PubMed]
- Xia, L.-K.; Yu, J.; Chai, G.-R.; Wang, D.; Li, Y. Comparison of the Femtosecond Laser and Mechanical Microkeratome for Flap Cutting in LASIK. Int. J. Ophthalmol. 2015, 8, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.-C.; Chang, C.-K.; Ma, D.H.-K.; Lin, Y.-F.; Chen, K.-J.; Sun, M.-H.; Hsiao, C.-H.; Wu, P.-H. Dry Eye after LASIK with a Femtosecond Laser or a Mechanical Microkeratome. Optom. Vis. Sci. 2013, 90, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Chua, J.; Vania, M.; Cheung, C.M.G.; Ang, M.; Chee, S.P.; Yang, H.; Li, J.; Wong, T.T. Expression Profile of Inflammatory Cytokines in Aqueous from Glaucomatous Eyes. Mol. Vis. 2012, 18, 431–438. [Google Scholar]
- Karakus, S.; Mathews, P.M.; Agrawal, D.; Henrich, C.; Ramulu, P.Y.; Akpek, E.K. Impact of Dry Eye on Prolonged Reading. Optom. Vis. Sci. 2018, 95, 1105–1113. [Google Scholar] [CrossRef]
- Doughty, M.J.; Glavin, S. Efficacy of Different Dry Eye Treatments with Artificial Tears or Ocular Lubricants: A Systematic Review. Ophthalmic Physiol. Opt. 2009, 29, 573–583. [Google Scholar] [CrossRef]
- Lee, H.; Kim, M.; Park, S.Y.; Kim, E.K.; Seo, K.Y.; Kim, T. Mechanical Meibomian Gland Squeezing Combined with Eyelid Scrubs and Warm Compresses for the Treatment of Meibomian Gland Dysfunction. Clin. Exp. Optom. 2017, 100, 598–602. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Wang, H.; Liang, M.; Li, Z.; Li, Y.; Zhou, X.; Kuang, G. Hypochlorous Acid Can Be the Novel Option for the Meibomian Gland Dysfunction Dry Eye through Ultrasonic Atomization. Dis. Mrk. 2022, 2022, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Yeu, E.; Wirta, D.L.; Karpecki, P.; Baba, S.N.; Holdbrook, M.; Saturn I Study Group. Lotilaner Ophthalmic Solution, 0.25%, for the Treatment of Demodex Blepharitis: Results of a Prospective, Randomized, Vehicle-Controlled, Double-Masked, Pivotal Trial (Saturn-1). Cornea 2022, 1, 10–97. [Google Scholar] [CrossRef] [PubMed]
- Hura, A.S.; Epitropoulos, A.T.; Czyz, C.N.; Rosenberg, E.D. Visible Meibomian Gland Structure Increases After Vectored Thermal Pulsation Treatment in Dry Eye Disease Patients with Meibomian Gland Dysfunction. Clin. Ophthalmol. 2020, 14, 4287–4296. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.S.; DuBiner, H.B.; Epstein, R.J.; Ernest, P.H.; Greiner, J.V.; Hardten, D.R.; Holland, E.J.; Lemp, M.A.; McDonald, J.E.; Silbert, D.I.; et al. A New System, the LipiFlow, for the Treatment of Meibomian Gland Dysfunction. Cornea 2012, 31, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Badawi, D. TearCare® System Extension Study: Evaluation of the Safety, Effectiveness, and Durability through 12 Months of a Second TearCare® Treatment on Subjects with Dry Eye Disease. Clin. Ophthalmol. 2019, 13, 189–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vora, G.K.; Gupta, P.K. Intense Pulsed Light Therapy for the Treatment of Evaporative Dry Eye Disease. Curr. Opin. Ophthalmol. 2015, 26, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Hovanesian, J.A.; Nichols, K.K.; Jackson, M.; Katz, J.; Chan, A.; Glassberg, M.B.; Sloesen, B.; Korves, C.; Nguyen, C.; Syntosi, A. Real-World Experience with Lifitegrast Ophthalmic Solution (Xiidra®) in the US and Canada: Retrospective Study of Patient Characteristics, Treatment Patterns, and Clinical Effectiveness in 600 Patients with Dry Eye Disease. Clin. Ophthalmol. 2021, 15, 1041–1054. [Google Scholar] [CrossRef]
- Kunert, K.S.; Tisdale, A.S.; Stern, M.E.; Smith, J.A.; Gipson, I.K. Analysis of Topical Cyclosporine Treatment of Patients with Dry Eye Syndrome: Effect on Conjunctival Lymphocytes. Arch. Ophthalmol. 2000, 118, 1489–1496. [Google Scholar] [CrossRef]
- Stern, M.E.; Beuerman, R.W.; Fox, R.I.; Gao, J.; Mircheff, A.K.; Pflugfelder, S.C. The Pathology of Dry Eye: The Interaction between the Ocular Surface and Lacrimal Glands. Cornea 1998, 17, 584–589. [Google Scholar] [CrossRef]
- Cutolo, C.A.; Barabino, S.; Bonzano, C.; Traverso, C.E. The Use of Topical Corticosteroids for Treatment of Dry Eye Syndrome. Ocul. Immunol. Inflamm. 2019, 27, 266–275. [Google Scholar] [CrossRef]
- Yagci, A.; Gurdal, C. The Role and Treatment of Inflammation in Dry Eye Disease. Int. Ophthalmol. 2014, 34, 1291–1301. [Google Scholar] [CrossRef] [PubMed]
- Pan, Q.; Angelina, A.; Marrone, M.; Stark, W.J.; Akpek, E.K. Autologous Serum Eye Drops for Dry Eye. Cochrane Database Syst. Rev. 2017, 2, CD009327. [Google Scholar] [CrossRef] [PubMed]
- Murri, M.S.; Moshirfar, M.; Birdsong, O.C.; Ronquillo, Y.C.; Ding, Y.; Hoopes, P.C. Amniotic Membrane Extract and Eye Drops: A Review of Literature and Clinical Application. Clin. Ophthalmol. 2018, 12, 1105–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rennie, K.; Gruslin, A.; Hengstschläger, M.; Pei, D.; Cai, J.; Nikaido, T.; Bani-Yaghoub, M. Applications of Amniotic Membrane and Fluid in Stem Cell Biology and Regenerative Medicine. Stem Cells Int. 2012, 2012, 721538. [Google Scholar] [CrossRef]
- Bowen, C.M.; Ditmars, F.S.; Gupta, A.; Reems, J.-A.; Fagg, W.S. Cell-Free Amniotic Fluid and Regenerative Medicine: Current Applications and Future Opportunities. Biomedicines 2022, 10, 2960. [Google Scholar] [CrossRef]
- Yoo, S.-E.; Lee, D.-C.; Chang, M.-H. The Effect of Low-Dose Doxycycline Therapy in Chronic Meibomian Gland Dysfunction. Korean J. Ophthalmol. 2005, 19, 258–263. [Google Scholar] [CrossRef] [Green Version]
- Sheppard, J.D.; Singh, R.; McClellan, A.J.; Weikert, M.P.; Scoper, S.V.; Joly, T.J.; Whitley, W.O.; Kakkar, E.; Pflugfelder, S.C. Long-Term Supplementation With n-6 and n-3 PUFAs Improves Moderate-to-Severe Keratoconjunctivitis Sicca: A Randomized Double-Blind Clinical Trial. Cornea 2013, 32, 1297–1304. [Google Scholar] [CrossRef]
- Wirta, D.; Vollmer, P.; Paauw, J.; Chiu, K.-H.; Henry, E.; Striffler, K.; Nau, J.; ONSET-2 Study Group. Efficacy and Safety of OC-01 (Varenicline Solution) Nasal Spray on Signs and Symptoms of Dry Eye Disease: The ONSET-2 Phase 3 Randomized Trial. Ophthalmology 2022, 129, 379–387. [Google Scholar] [CrossRef]
- Messmer, E.M. Pathophysiology of Dry Eye Disease and Novel Therapeutic Targets. Exp. Eye Res. 2022, 217, 108944. [Google Scholar] [CrossRef]
- Koob, T.J.; Lim, J.J.; Zabek, N.; Massee, M. Cytokines in Single Layer Amnion Allografts Compared to Multilayer Amnion/Chorion Allografts for Wound Healing. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 1133–1140. [Google Scholar] [CrossRef]
- Baradaran-Rafii, A.; Asl, N.S.; Ebrahimi, M.; Jabbehdari, S.; Bamdad, S.; Roshandel, D.; Eslani, M.; Momeni, M. The Role of Amniotic Membrane Extract Eye Drop (AMEED) in in Vivo Cultivation of Limbal Stem Cells. Ocul. Surf. 2018, 16, 146–153. [Google Scholar] [CrossRef] [PubMed]
- John, T.; Tighe, S.; Sheha, H.; Hamrah, P.; Salem, Z.M.; Cheng, A.M.S.; Wang, M.X.; Rock, N.D. Corneal Nerve Regeneration after Self-Retained Cryopreserved Amniotic Membrane in Dry Eye Disease. J. Ophthalmol. 2017, 2017, 6404918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasper, J.C.; Winter, G.; Friess, W. Recent Advances and Further Challenges in Lyophilization. Eur. J. Pharm. Biopharm. 2013, 85, 162–169. [Google Scholar] [CrossRef] [PubMed]
- López-García, J.S.; García-Lozano, I.; Rivas, L.; Viso-Garrote, M.; Raposo, R.; Méndez, M.T. Lyophilized Autologous Serum Eyedrops: Experimental and Comparative Study. Am. J. Ophthalmol. 2020, 213, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Sabater-Cruz, N.; Martinez-Conesa, E.; Vilarrodona, A.; Casaroli-Marano, R.P. Lyophilized Amniotic Membrane Graft for Primary Pterygium Surgery: Preliminary Results. Cell Tissue Bank 2022, 23, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Swan, J. Use of Cryopreserved, Particulate Human Amniotic Membrane and Umbilical Cord (AM/UC) Tissue: A Case Series Study for Application in the Healing of Chronic Wounds. Surg. Technol. Int. 2014, 25, 73–78. [Google Scholar]
- Shimada, H.; Nakashizuka, H. Cataract Surgery by Intraoperative Surface Irrigation with 0.25% Povidone-Iodine. J. Clin. Med. 2021, 10, 3611. [Google Scholar] [CrossRef]
- Herrinton, L.J.; Shorstein, N.H.; Paschal, J.F.; Liu, L.; Contreras, R.; Winthrop, K.L.; Chang, W.J.; Melles, R.B.; Fong, D.S. Comparative Effectiveness of Antibiotic Prophylaxis in Cataract Surgery. Ophthalmology 2016, 123, 287–294. [Google Scholar] [CrossRef] [Green Version]
- Latz, C.; Asshauer, T.; Rathjen, C.; Mirshahi, A. Femtosecond-Laser Assisted Surgery of the Eye: Overview and Impact of the Low-Energy Concept. Micromachines 2021, 12, 122. [Google Scholar] [CrossRef]
- Mian, S.I.; Li, A.Y.; Dutta, S.; Musch, D.C.; Shtein, R.M. Dry Eyes and Corneal Sensation after Laser in Situ Keratomileusis with Femtosecond Laser Flap Creation Effect of Hinge Position, Hinge Angle, and Flap Thickness. J. Cataract Refract Surg. 2009, 35, 2092–2098. [Google Scholar] [CrossRef]
- Tai, Y.-C.; Sun, C.-C. Effects of Flap Diameter on Dry Eye Parameters and Corneal Sensation after Femtosecond Laser-Assisted LASIK. Taiwan J. Ophthalmol. 2019, 9, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Ibach, M.J.; Shafer, B.M.; Wallin, D.D.; Puls-Boever, K.R.; Thompson, V.M.; Berdahl, J.P. The Effectiveness and Safety of Dextenza 0.4 Mg for the Treatment of Postoperative Inflammation and Pain in Patients After Photorefractive Keratectomy: The RESTORE Trial. J. Refract. Surg. 2021, 37, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Lindholm, J.-M.; Taipale, C.; Ylinen, P.; Tuuminen, R. Perioperative Subconjunctival Triamcinolone Acetonide Injection for Prevention of Inflammation and Macular Oedema after Cataract Surgery. Acta Ophthalmol. 2020, 98, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Ramamoorthy, P.; Nichols, J.J. Compliance Factors Associated With Contact Lens-Related Dry Eye. Eye Contact Lens Sci. Clin. Pract. 2014, 40, 17–22. [Google Scholar] [CrossRef]
- Sullivan, D.A.; Liu, Y. System and Method for Treating Meibomian Gland Dysfunction. WO2019169172A1, 6 September 2019. Available online: https://patents.google.com/patent/WO2019169172A1/en (accessed on 20 November 2022).
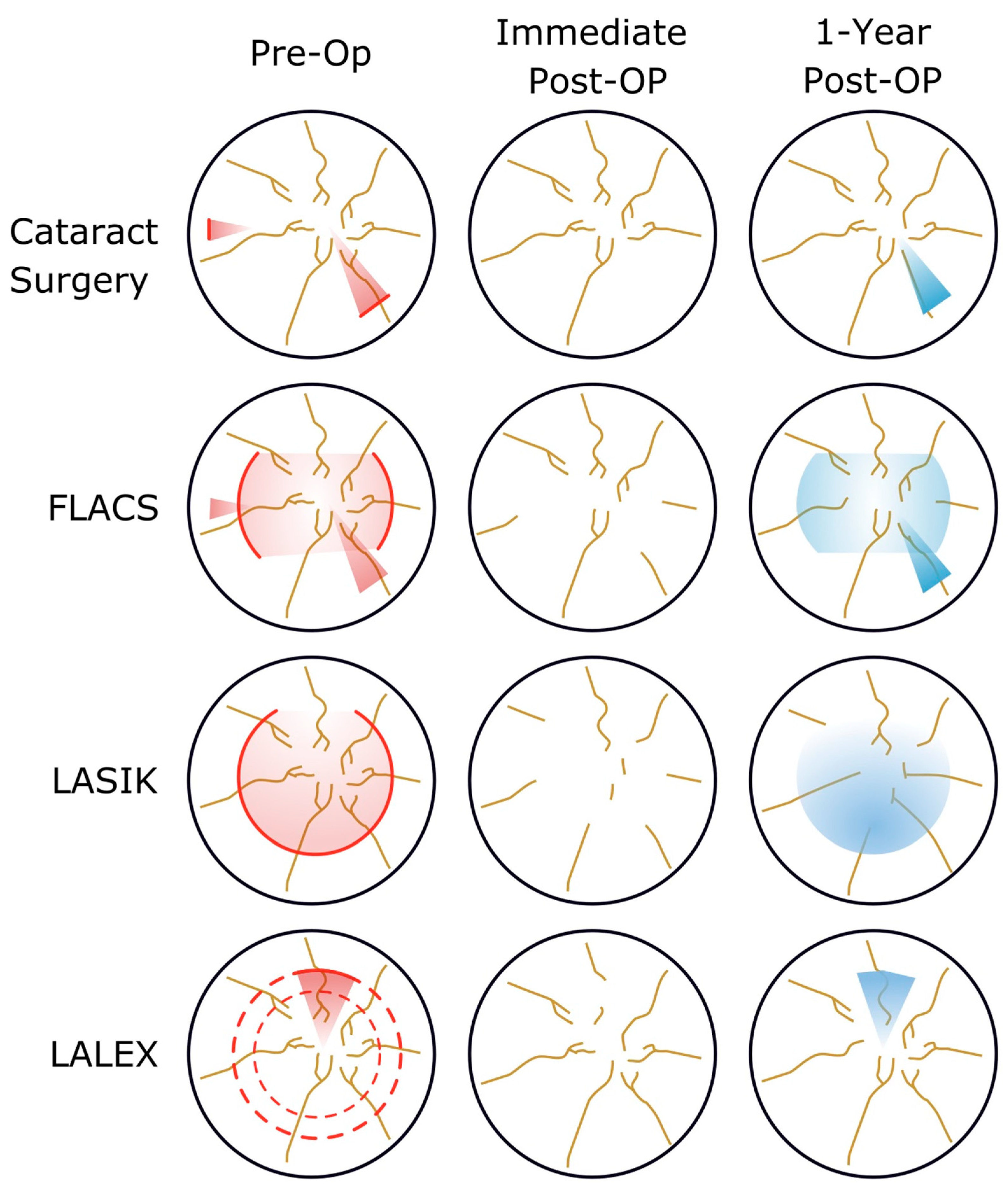







| Ocular Surgery | Mechanism | Potential Therapeutic Targets |
|---|---|---|
| Cataract Surgery Along Cataract Surgery + MIGS | Ocular Surface Inflammation; corneal nerve loss; microbiome disruption | TYRVAYA™—Spares surface CEQUA®, RESTASIS® HydroEye® Regener-Eyes® |
| PRK LASIK | Corneal nerve loss, worst with LASIK | NEOX FLO AMG TYRVAYA™—Spares surface CEQUA®, RESTASIS® |
| LALEX | Corneal nerve loss, least of all laser-based refractive surgeries | Regener-Eyes® TYRVAYA™—Spares surface CEQUA®, RESTASIS® |
| FLACS | Ocular Surface Inflammation, correlated with energy | TYRVAYA™—Spares surface CEQUA®, RESTASIS® HydroEye® Regener-Eyes® |
| Class | Mechanism | Examples | Duration | Special Uses/Comments |
|---|---|---|---|---|
| Lifestyle Changes | Preventing tear desiccation | Fan placement, avoiding prolonged reading | Indefinitely | This should become a permanent lifestyle change for all patients |
| Increasing Tear Films | Tear replacement; inflammatory marker dilution | REFRESH TEARS® (Abbvie, Chicago, IL, USA) | QID, 2–4 months pre-op | Frequent use of unpreserved tears can worsen symptoms |
| Punctal Occlusion | DuraPlug | 2–4 months pre-op | Avoid using with some anti-inflammatories, diluting them in the tear film reduces effect | |
| Hypchlorous Acid Scrubs Lotilaner Ophthalmic Solution | Meibomian exfoliation, mechanical debridement | Avenova®, OCuSOFT | 2–4 months pre-op | For predominantly blepharitis or Demodex symptoms |
| Warming | Heat-based meibomian expression | Warm Compresses IPL | BID 2 months pre-op | Careful applying heat and debridement to inflamed tissue |
| Heat-based meibomian expression | LipiFlow®, TearCare® | 2 months pre-op | More regulated and gentle on eyelids | |
| Pro-Biotics | Tear film support | HydroEye® | 2 months pre-op | Surface sparing, easy to continue post-op |
| Anti-inflammatories | Corticosteroid | Prednisolone Acetate | BID 2 months pre-op | Monitor for pressure response |
| LFA-1 | Xiidra® | BID 2 months pre-op | Paired with Prednisolone Acetate BID | |
| Calcineurin inhibition | CEQUA®, RESTASIS®, | BID 2 months pre-op | Paired with Prednisolone Acetate QDAY | |
| Verenicline | TYRVAYA™ | BID 1 month pre-op | Nasal spray; spares ocular surface; easy to continue post-op | |
| IPL | OptiLight | 4 section pre-op | Can repeated post-op | |
| MMP Inhibition | Doxycycline | ORACEA®, Periostat® | 1–2 weeks pre-op | Minimal antibacterial properties so microbiome preservation |
| Advanced Tear Substitutes | Autologous Serum Tears | Serum Tears | 2 months pre-op | Theoretically contain more patient-specific bio-compatible materials |
| Amnionic-Based Therapies | Amnionic Fluid-Based Tears | Regener-Eyes® | QID 2 months pre-op | Can be used under drug depot system (Hyper-CL™) |
| Cryopreserved or Lyophilized Amnionic Membrane Grafts | AMG | Pre- or Post-Op | Can be placed under contact lens; consider for post-laser STODS | |
| Amnionic and Placental derived | NEOX FLO | Pre- or Post-Op | Can be placed under contact lens; consider for post-laser STODS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirabayashi, M.T.; Barnett, B.P. Solving STODS—Surgical Temporary Ocular Discomfort Syndrome. Diagnostics 2023, 13, 837. https://doi.org/10.3390/diagnostics13050837
Hirabayashi MT, Barnett BP. Solving STODS—Surgical Temporary Ocular Discomfort Syndrome. Diagnostics. 2023; 13(5):837. https://doi.org/10.3390/diagnostics13050837
Chicago/Turabian StyleHirabayashi, Matthew T., and Brad P. Barnett. 2023. "Solving STODS—Surgical Temporary Ocular Discomfort Syndrome" Diagnostics 13, no. 5: 837. https://doi.org/10.3390/diagnostics13050837
APA StyleHirabayashi, M. T., & Barnett, B. P. (2023). Solving STODS—Surgical Temporary Ocular Discomfort Syndrome. Diagnostics, 13(5), 837. https://doi.org/10.3390/diagnostics13050837








