Blood Count-Derived Inflammatory Markers Correlate with Lengthier Hospital Stay and Are Predictors of Pneumothorax Risk in Thoracic Trauma Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Inflammatory Biomarkers
- MLR = monocytes/lymphocytes
- NLR = neutrophils/lymphocytes
- PLR = platelets/lymphocytes
- SII = (neutrophils × platelets)/lymphocytes
- SIRI = (monocytes × platelets)/lymphocytes
- AISI = (neutrophils × monocytes × platelets)/lymphocytes
2.4. Study Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lundin, A.; Akram, S.K.; Berg, L.; Göransson, K.E.; Enocson, A. Thoracic injuries in trauma patients: Epidemiology and its influence on mortality. Scand. J. Trauma Resusc. Emerg. Med. 2022, 30, 69. [Google Scholar] [CrossRef]
- Bardenheuer, M.; Obertacke, U.; Waydhas, C.; Nast-Kolb, D. Epidemiologie des Schwerverletzten Eine prospektive Erfassung der präklinischen und klinischen Versorgung. Unfallchirurg 2000, 103, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Fokkema, A.T.; Johannesdottir, B.K.; Wendt, K.; Haaverstad, R.; Reininga, I.H.F.; Geisner, T. Comorbidities, injury severity and complications predict mortality in thoracic trauma. Eur. J. Trauma Emerg. Surg. 2022, online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Yimam, A.E.; Mustofa, S.Y.; Gebregzi, A.H.; Aytolign, H.A. Mortality rate and factors associated with death in traumatic chest injury patients: A retrospective study. Int. J. Surg. Open 2021, 37, 100420. [Google Scholar] [CrossRef]
- Peek, J.; Ochen, Y.; Saillant, N.; Groenwold, R.H.H.; Leenen, L.P.H.; Uribe-Leitz, T.; Houwert, R.M.; Heng, M. Traumatic rib fractures: A marker of severe injury. A nationwide study using the National Trauma Data Bank. Trauma Surg. Acute Care Open 2020, 5, e000441. [Google Scholar] [CrossRef] [PubMed]
- Huber, S.; Biberthaler, P.; Delhey, P.; Trentzsch, H.; Winter, H.; van Griensven, M.; Lefering, R.; Huber-Wagner, S. Predictors of poor outcomes after significant chest trauma in multiply injured patients: A retrospective analysis from the German Trauma Registry (Trauma Register DGU®). Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Binkowska, A.M.; Michalak, G.; Slotwinski, R. Review paper Current views on the mechanisms of immune responses to trauma and infection. Cent. Eur. J. Immunol. 2015, 2, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Soulaiman, S.E.; Dopa, D.; Raad, A.-B.T.; Hasan, W.; Ibrahim, N.; Hasan, A.-Y.; Sulaiman, H.A.; Darwich, M. Cohort retrospective study: The neutrophil to lymphocyte ratio as an independent predictor of outcomes at the presentation of the multi-trauma patient. Int. J. Emerg. Med. 2020, 13, 5. [Google Scholar] [CrossRef] [Green Version]
- Huber-Lang, M.; Lambris, J.D.; Ward, P.A. Innate immune responses to trauma. Nat. Immunol. 2018, 19, 327–341. [Google Scholar] [CrossRef]
- Brown, M.; Worrell, C.; Pariante, C.M. Inflammation and early life stress: An updated review of childhood trauma and inflammatory markers in adulthood. Pharmacol. Biochem. Behav. 2021, 211, 173291. [Google Scholar] [CrossRef]
- Favre, P.A.; de Molliens, L.; Petit, L.; Biais, M.; Carrié, C. May the neutrophil-to-lymphocyte ratio at admission predict the occurrence and the severity of ARDS after blunt chest trauma patients? A retrospective study. Am. J. Emerg. Med. 2020, 39, 137–142. [Google Scholar] [CrossRef]
- Kaller, R.; Arbănași, E.M.; Mureșan, A.V.; Voidăzan, S.; Arbănași, E.M.; Horváth, E.; Suciu, B.A.; Hosu, I.; Halmaciu, I.; Brinzaniuc, K.; et al. The Predictive Value of Systemic Inflammatory Markers, the Prognostic Nutritional Index, and Measured Vessels’ Diameters in Arteriovenous Fistula Maturation Failure. Life 2022, 12, 1447. [Google Scholar] [CrossRef]
- Arbănași, E.M.; Halmaciu, I.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Suciu, B.A.; Coșarcă, C.M.; Cojocaru, I.I.; Melinte, R.M.; Russu, E. Systemic Inflammatory Biomarkers and Chest CT Findings as Predictors of Acute Limb Ischemia Risk, Intensive Care Unit Admission, and Mortality in COVID-19 Patients. Diagnostics 2022, 12, 2379. [Google Scholar] [CrossRef] [PubMed]
- Halmaciu, I.; Arbănași, E.M.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Bacalbasa, N.; Suciu, B.A.; Cojocaru, I.I.; Runcan, A.I.; Grosu, F.; et al. Chest CT Severity Score and Systemic Inflammatory Biomarkers as Predictors of the Need for Invasive Mechanical Ventilation and of COVID-19 Patients’ Mortality. Diagnostics 2022, 12, 2089. [Google Scholar] [CrossRef] [PubMed]
- Mureșan, A.V.; Hălmaciu, I.; Arbănași, E.M.; Kaller, R.; Arbănași, E.M.; Budișcă, O.A.; Melinte, R.M.; Vunvulea, V.; Filep, R.C.; Mărginean, L.; et al. Prognostic Nutritional Index, Controlling Nutritional Status (CONUT) Score, and Inflammatory Biomarkers as Predictors of Deep Vein Thrombosis, Acute Pulmonary Embolism, and Mortality in COVID-19 Patients. Diagnostics 2022, 12, 2757. [Google Scholar] [CrossRef]
- Niculescu, R.; Russu, E.; Arbănași, E.M.; Kaller, R.; Arbănași, E.M.; Melinte, R.M.; Coșarcă, C.M.; Cocuz, I.G.; Sabău, A.H.; Tinca, A.C.; et al. Carotid Plaque Features and Inflammatory Biomarkers as Predictors of Restenosis and Mortality Following Carotid Endarterectomy. Int. J. Environ. Res. Public Health 2022, 19, 13934. [Google Scholar] [CrossRef]
- Arbănași, E.M.; Mureșan, A.V.; Arbănași, E.M.; Kaller, R.; Cojocaru, I.I.; Coșarcă, C.M.; Russu, E. The Neutrophil-to-Lymphocyte Ratio’s Predictive Utility in Acute Pulmonary Embolism: Systematic Review. J. Cardiovasc. Emergencies 2022, 8, 25–30. [Google Scholar] [CrossRef]
- Russu, E.; Mureșan, A.V.; Arbănași, E.M.; Kaller, R.; Hosu, I.; Voidăzan, S.; Arbănași, E.M.; Coșarcă, C.M. The Predictive Role of NLR and PLR in Outcome and Patency of Lower Limb Revascularization in Patients with Femoropopliteal Disease. J. Clin. Med. 2022, 11, 2620. [Google Scholar] [CrossRef]
- Melinte, R.M.; Arbănași, E.M.; Blesneac, A.; Zolog, D.N.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Melinte, I.M.; Niculescu, R.; Russu, E. Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty. Medicina 2022, 58, 1502. [Google Scholar] [CrossRef]
- Arbănași, E.M.; Mureșan, A.V.; Coșarcă, C.M.; Kaller, R.; Bud, T.I.; Hosu, I.; Voidăzan, S.T.; Arbănași, E.M.; Russu, E. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Impact on Predicting Outcomes in Patients with Acute Limb Ischemia. Life 2022, 12, 822. [Google Scholar] [CrossRef]
- Mureșan, A.V.; Russu, E.; Arbănași, E.M.; Kaller, R.; Hosu, I.; Arbănași, E.M.; Voidăzan, S.T. The Predictive Value of NLR, MLR, and PLR in the Outcome of End-Stage Kidney Disease Patients. Biomedicines 2022, 10, 1272. [Google Scholar] [CrossRef] [PubMed]
- Halmaciu, I.; Suciu, B.A.; Vunvulea, V.; Muresan, M.G.; Scarlat, F.C.; Molnar, C.; Bacalbasa, N.; Brinzaniuc, K.; Voidazan, S. The Importance of Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio in Predicting the Appearance of the Rectal Stenosis or Rectal Obstruction in Patients with Rectal Adenocarcinomas. Rev. Chim. 2020, 71, 239–247. [Google Scholar] [CrossRef]
- Howard, R.; Kanetsky, P.A.; Egan, K.M. Exploring the prognostic value of the neutrophil-to-lymphocyte ratio in cancer. Sci. Rep. 2019, 9, 19673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grassadonia, A.; Graziano, V.; Iezzi, L.; Vici, P.; Barba, M.; Pizzuti, L.; Cicero, G.; Krasniqi, E.; Mazzotta, M.; Marinelli, D.; et al. Prognostic Relevance of Neutrophil to Lymphocyte Ratio (NLR) in Luminal Breast Cancer: A Retrospective Analysis in the Neoadjuvant Setting. Cells 2021, 10, 1685. [Google Scholar] [CrossRef] [PubMed]
- Festa, E.; Ascione, T.; Bernasconi, A.; Di Gennaro, D.; Basso, M.A.; Guarino, A.; Balato, G. Diagnostic Performance of Neutrophil to Lymphocyte Ratio, Monocyte to Lymphocyte Ratio, Platelet to Lymphocyte Ratio, and Platelet to Mean Platelet Volume Ratio in Periprosthetic Hip and Knee Infections: A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 2033. [Google Scholar] [CrossRef]
- Zhao, G.; Chen, J.; Wang, J.; Wang, S.; Xia, J.; Wei, Y.; Wu, J.; Huang, G.; Chen, F.; Shi, J.; et al. Predictive values of the postoperative neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and lymphocyte-to-monocyte ratio for the diagnosis of early periprosthetic joint infections: A preliminary study. J. Orthop. Surg. Res. 2020, 15, 571. [Google Scholar] [CrossRef]
- Jo, S.; Jeong, T.; Lee, J.B.; Jin, Y.; Yoon, J.; Park, B. The prognostic value of platelet-to-lymphocyte ratio on in-hospital mortality in admitted adult traffic accident patients. PLoS ONE 2020, 15, e0233838. [Google Scholar] [CrossRef]
- Li, W.; Deng, W. Platelet-to-lymphocyte ratio predicts short-term mortality in patients with moderate to severe traumatic brain injury. Sci. Rep. 2022, 12, 13976. [Google Scholar] [CrossRef]
- Vunvulea, V.; Suciu, B.A.; Cocuz, I.G.; Bacalbașa, N.; Molnar, C.; Ghiga, D.V.; Hălmaciu, I. Importance of the neutrophil-to-lymphocyte ratio as a prognostic factor in patients with spleen trauma: A single center experience. Biomed. Rep. 2022, 17, 80. [Google Scholar] [CrossRef]
- Vunvulea, V.; Budișcă, O.A.; Arbănași, E.M.; Mureșan, A.V.; Arbănași, E.M.; Brînzaniuc, K.; Niculescu, R.; Cocuz, I.G.; Ivănescu, A.D.; Hălmaciu, I.; et al. The Predictive Role of Systemic Inflammatory Markers in the Development of Acute Kidney Failure and Mortality in Patients with Abdominal Trauma. J. Pers. Med. 2022, 12, 2045. [Google Scholar] [CrossRef]
- Cheng, H.-R.; Song, J.-Y.; Zhang, Y.-N.; Chen, Y.-B.; Lin, G.-Q.; Huang, G.-Q.; He, J.-C.; Wang, Z. High Monocyte-To-Lymphocyte Ratio Is Associated with Stroke-Associated Pneumonia. Front. Neurol. 2020, 11, 575809. [Google Scholar] [CrossRef]
- Kamiya, N.; Ishikawa, Y.; Kotani, K.; Hatakeyama, S.; Matsumura, M. Monocyte-to-Lymphocyte Ratio in the Diagnosis of Lymphoma in Adult Patients. Int. J. Gen. Med. 2022, 15, 4221–4226. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Qiao, W.; Liu, B.; Li, J.; Yuan, C.; Long, J.; Hu, C.; Zang, C.; Zheng, J.; Zhang, Y. The monocyte to lymphocyte ratio not only at baseline but also at relapse predicts poor outcomes in patients with hepatocellular carcinoma receiving locoregional therapy. BMC Gastroenterol. 2022, 22, 98. [Google Scholar] [CrossRef]
- Lin, K.-B.; Fan, F.-H.; Cai, M.-Q.; Yu, Y.; Fu, C.-L.; Ding, L.-Y.; Sun, Y.-D.; Sun, J.-W.; Shi, Y.-W.; Dong, Z.-F.; et al. Systemic immune inflammation index and system inflammation response index are potential biomarkers of atrial fibrillation among the patients presenting with ischemic stroke. Eur. J. Med. Res. 2022, 27, 106. [Google Scholar] [CrossRef]
- Zinellu, A.; Collu, C.; Nasser, M.; Paliogiannis, P.; Mellino, S.; Zinellu, E.; Traclet, J.; Ahmad, K.; Mangoni, A.A.; Carru, C.; et al. The Aggregate Index of Systemic Inflammation (AISI): A Novel Prognostic Biomarker in Idiopathic Pulmonary Fibrosis. J. Clin. Med. 2021, 10, 4134. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Hu, T.; Wang, J.; Xiao, R.; Liao, X.; Liu, M.; Sun, Z. Systemic immune-inflammation index as a potential biomarker of cardiovascular diseases: A systematic review and meta-analysis. Front. Cardiovasc. Med. 2022, 9, 933913. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Yang, J.; Wang, X.; Wang, X.; Chai, S. The Clinical Value of Systemic Inflammatory Response Index and Inflammatory Prognosis Index in Predicting 3-Month Outcome in Acute Ischemic Stroke Patients with Intravenous Thrombolysis. Int. J. Gen. Med. 2022, 15, 7907–7918. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.-C.; Jiang, W.; Chen, X.; Yang, L.; Wang, H.; Liu, Y.-H. Systemic immune-inflammation index independently predicts poor survival of older adults with hip fracture: A prospective cohort study. BMC Geriatr. 2021, 21, 155. [Google Scholar] [CrossRef]
- Feng, J.-F.; Chen, S.; Yang, X. Systemic immune-inflammation index (SII) is a useful prognostic indicator for patients with squamous cell carcinoma of the esophagus. Medicine 2017, 96, e5886. [Google Scholar] [CrossRef]
- Kim, M.; Moore, J.E. Chest Trauma: Current Recommendations for Rib Fractures, Pneumothorax, and Other Injuries. Curr. Anesthesiol. Rep. 2020, 10, 61–68. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, Z.; Yang, J.-X.; Gan, J.-X.; Xu, S.-W.; You, X.-D.; Jiang, G.-Y. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit. Care 2006, 10, R112. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Jindal, P. Principles of diagnosis and management of traumatic pneumothorax. J. Emergencies Trauma Shock 2008, 1, 34–41. [Google Scholar] [CrossRef]
- Lu, M.-S.; Huang, Y.-K.; Liu, Y.-H.; Liu, H.-P.; Kao, C.-L. Delayed pneumothorax complicating minor rib fracture after chest trauma. Am. J. Emerg. Med. 2008, 26, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Tran, J.; Haussner, W.; Shah, K. Traumatic Pneumothorax: A Review of Current Diagnostic Practices and Evolving Management. J. Emerg. Med. 2021, 61, 517–528. [Google Scholar] [CrossRef]
- Zanette, G.Z.; Waltrick, R.S.; Monte, M.B. Perfil epidemiológico do trauma torácico em um hospital referência da Foz do Rio Itajaí. Rev. Col. Bras. Cir. 2019, 46. [Google Scholar] [CrossRef] [PubMed]
- Ferro, T.N.; Goslar, P.W.; Romanovsky, A.A.; Petersen, S.R. Smoking in Trauma Patients: The Effects on the Incidence of Sepsis, Respiratory Failure, Organ Failure, and Mortality. J. Trauma Inj. Infect. Crit. Care 2010, 69, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Resnick, S.; Inaba, K.; Okoye, O.; Nosanov, L.; Grabo, D.; Benjamin, E.; Smith, J.; Demetriades, D. Impact of Smoking on Trauma Patients. Turk. J. Trauma Emerg. Surg. 2014, 20, 248–252. [Google Scholar] [CrossRef] [Green Version]
- Farris, S.G.; Zvolensky, M.J.; Beckham, J.C.; Vujanovic, A.A.; Schmidt, N.B. Trauma exposure and cigarette smoking: The impact of negative affect and affect-regulatory smoking motives. J. Addict. Dis. 2014, 33, 354–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grigorian, A.; Lekawa, M.; Dolich, M.; Schubl, S.D.; Doben, A.R.; Kuza, C.M.; Barrios, C.; Nahmias, J. Smoking is associated with an improved short-term outcome in patients with rib fractures. Eur. J. Trauma Emerg. Surg. 2019, 46, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Modarresi, M.; Gillon, B.; Mojarrab, J.N.; Aguilar, R.; Hunter, Z.D.; Schade, M.S.; Sanabria, J.; Klug, R.; Adkins, S.; Sanabria, J.R. The Effects of Obesity on Outcomes in Trauma Injury: Overview of the Current Literature. Marshall J. Med. 2017, 3, 40. [Google Scholar] [CrossRef]
- Liu, T.; Chen, J.-J.; Bai, X.-J.; Zheng, G.-S.; Gao, W. The effect of obesity on outcomes in trauma patients: A meta-analysis. Injury 2013, 44, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Cromwell, P.M.; Reynolds, I.S.; Heneghan, H.M.; Glasgow, S.M. Obesity and outcomes in trauma—A systematic review and meta-analysis. Injury 2022, 54, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Zickler, W.P.; Sharpe, J.P.; Lewis, R.H.; Zambetti, B.R.; Jones, M.D.; Zickler, M.K.; Zickler, C.L.; Magnotti, L.J. In for a Penny, in for a Pound: Obesity weighs heavily on both cost and outcome in trauma. Am. J. Surg. 2022, 224, 590–594. [Google Scholar] [CrossRef]
- Hsieh, T.-M.; Chuang, P.-C.; Liu, C.-T.; Wu, B.-Y.; Liu, Y.-W.; Hsieh, C.-H. Protective Role of Obesity on Trauma Impact: A Retrospective Analysis of Patients with Surgical Blunt Bowel Mesenteric Injury Due to Road Traffic Accidents. Risk Manag. Health Policy 2022, 15, 1533–1543. [Google Scholar] [CrossRef] [PubMed]
- Dvorak, J.E.; Lester, E.L.W.; Maluso, P.J.; Tatebe, L.; Schlanser, V.; Kaminsky, M.; Messer, T.; Dennis, A.J.; Starr, F.; Bokhari, F. The Obesity Paradox in the Trauma Patient: Normal May not Be Better. World J. Surg. 2020, 44, 1817–1823. [Google Scholar] [CrossRef]
- Dilektasli, E.; Inaba, K.; Haltmeier, T.; Wong, M.D.; Clark, D.; Benjamin, E.R.; Lam, L.; Demetriades, D. The prognostic value of neutrophil-to-lymphocyte ratio on mortality in critically ill trauma patients. J. Trauma Acute Care Surg. 2016, 81, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Younan, D.; Richman, J.; Zaky, A.; Pittet, J.-F. An Increasing Neutrophil-to-Lymphocyte Ratio Trajectory Predicts Organ Failure in Critically-Ill Male Trauma Patients. An Exploratory Study. Healthcare 2019, 7, 42. [Google Scholar] [CrossRef] [Green Version]
- Rau, C.-S.; Wu, S.-C.; Tsai, C.-H.; Chou, S.-E.; Su, W.-T.; Hsu, S.-Y.; Hsieh, C.-H. Association of White Blood Cell Subtypes and Derived Ratios with a Mortality Outcome in Adult Patients with Polytrauma. Healthcare 2022, 10, 1384. [Google Scholar] [CrossRef]

| Variables | All Patients n = 611 | Pneumothorax n = 155 (25.37%) | No Pneumothorax n = 456 (74.63%) | p Value |
|---|---|---|---|---|
| Age mean ± SD (min–max) | 47.48 ± 18.66 (18–98) | 51.68 ± 19.39 (19–93) | 46.12 ± 18.23 (18–98) | 0.002 |
| Male | 448 (73.32%) | 114 (73.54%) | 334 (73.24%) | 0.94 |
| Female | 163 (26.67%) | 41 (25.15%) | 122 (26.75%) | |
| Comorbidities and risk factors | ||||
| Arterial hypertension, No. (%) | 160 (10.8%) | 40 (25.81%) | 120 (26.32%) | 0.828 |
| Ischemic heart disease, No. (%) | 82 (13.42%) | 24 (15.48%) | 58 (12.72%) | 0.269 |
| Atrial fibrillation, No. (%) | 33 (5.4%) | 8 (5.16%) | 25 (5.48%) | 0.984 |
| Myocardial infarction, No. (%) | 20 (3.27%) | 6 (3.87%) | 14 (3.07%) | 0.262 |
| Diabetes mellitus, No. (%) | 66 (10.8%) | 12 (7,74%) | 54 (11.84%) | 0.122 |
| Chronic obstructive pulmonary disease, No. (%) | 55 (9%) | 23 (14.84%) | 32 (7.02%) | 0.066 |
| Peripheral arterial disease, No. (%) | 45 (7.36%) | 12 (7.74%) | 33 (7.24%) | 0.712 |
| Chronic kidney disease, No. (%) | 27 (4.42%) | 9 (5.81%) | 18 (3.95%) | 0.271 |
| Tobacco, No. (%) | 34 (5.56%) | 15 (9.68%) | 19 (4.17%) | 0.019 |
| Obesity, No. (%) | 224 (36.66%) | 44 (28.39%) | 180 (39.47%) | 0.038 |
| Type of trauma | ||||
| Blunt | 539 (88.22%) | 90 (58.06%) | 449 (98.4%) | <0.001 |
| Penetrating | 72 (11.78) | 65 (41.93%) | 7 (1.6%) | |
| Laboratory data | ||||
| Hemoglobin g/dL mean ± SD | 12.54 ± 2.32 | 12.82 ± 2.01 | 12.45 ± 2.41 | 0.91 |
| Hematocrit % mean ± SD | 37.5 ± 7.15 | 38.29 ± 5.61 | 37.24 ± 7.56 | 0.12 |
| Glucose mg/dL mean ± SD | 132.46 ± 54.17 | 136.51 ± 47.49 | 131.15 ± 56.14 | 0.29 |
| Sodium mean ± SD | 137.31 ± 16.12 | 139.91 ± 12.71 | 136.48 ± 17 | 0.024 |
| Potassium mean ± SD | 4.38 ± 1.116 | 4.3 ± 0.88 | 4.4 ± 1.24 | 0.34 |
| Neutrophils ×103/μL mean ± SD | 9.75 ± 5.07 | 13.13 ± 5.64 | 8.65 ± 4.35 | <0.0001 |
| Lymphocytes ×103/μL mean ± SD | 1.94 ± 1.02 | 1.52 ± 0.93 | 2.08 ± 1.01 | <0.0001 |
| Monocyte ×103/μL mean ± SD | 0.96 ± 0.86 | 1.18 ± 0.86 | 0.89 ± 0.84 | <0.0001 |
| Plt ×103/μL mean ± SD | 248.53 ± 90.46 | 265.39 ± 110.07 | 243.10 ± 82.57 | 0.009 |
| MLR, mean ± SD | 0.64 ± 0.63 | 0.96 ± 0.66 | 0.53 ± 0.59 | <0.0001 |
| NLR, mean ± SD | 6.76 ± 6.4 | 12.12 ± 9.23 | 5.04 ± 3.83 | <0.0001 |
| PLR, mean ± SD | 163.45 ± 113.55 | 229.41 ± 155.68 | 142.18 ± 86.14 | <0.0001 |
| SII, mean ± SD | 1636.60 ± 1554.68 | 3040.74 ± 2251.73 | 1183.75 ± 853.06 | <0.0001 |
| SIRI, mean ± SD | 6.89 ± 8.14 | 13.25 ± 10.4 | 4.83 ± 5.97 | <0.0001 |
| AISI, mean ± SD | 1739.16 ± 2372.9 | 3421.47 ± 3097.28 | 1196.59 ± 1777.91 | <0.0001 |
| Outcomes | ||||
| Length of hospital stay, mean ± SD | 6.73 ± 4.14 | 7.62 ± 4.26 | 6.45 ± 4.06 | 0.003 |
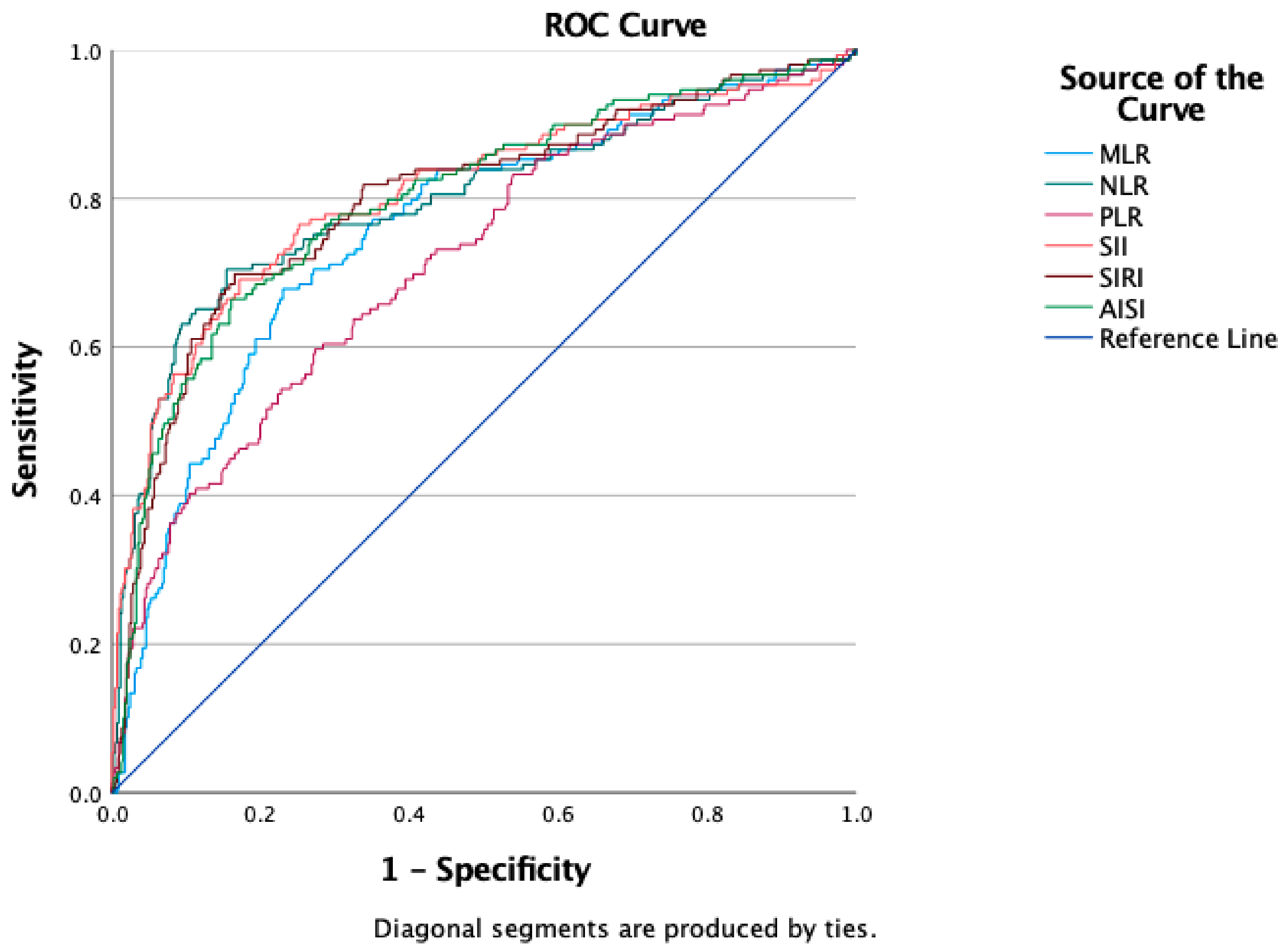
| Variables | Cut-Off | AUC | Std. Error | 95% CI | Sensitivity | Specificity | p Value |
|---|---|---|---|---|---|---|---|
| Pneumothorax | |||||||
| NLR | 6 | 0.798 | 0.024 | 0.751–0.845 | 76.5% | 71% | <0.0001 |
| MLR | 0.62 | 0.758 | 0.023 | 0.712–0.804 | 70.5% | 72.9% | <0.0001 |
| PLR | 165.71 | 0.714 | 0.025 | 0.665–0.763 | 60.4% | 71.6% | <0.0001 |
| SII | 1632.86 | 0.807 | 0.023 | 0.761–0.852 | 77.2% | 73.4% | <0.0001 |
| SIRI | 6.17 | 0.799 | 0.023 | 0.754–0.843 | 71.8% | 76.2% | <0.0001 |
| AISI | 1479.7 | 0.799 | 0.023 | 0.754–0.843 | 71.1% | 75.8% | <0.0001 |
| Pneumothorax | |||
|---|---|---|---|
| OR | 95% CI | p Value | |
| Age | 1.01 | 1.006–1.02 | 0.002 |
| COPD | 2.93 | 1.15–7.50 | 0.02 |
| Obesity | 0.65 | 0.44–0.97 | 0.03 |
| Tobacco | 2.29 | 1.12–4.66 | 0.01 |
| High NLR | 6.03 | 3.94–9.21 | <0.001 |
| High MLR | 5.97 | 3.97–8.97 | <0.001 |
| High PLR | 3.51 | 2.39–5.17 | <0.001 |
| High SII | 8.78 | 5.68–13.59 | <0.001 |
| High SIRI | 8.55 | 5.43–13.47 | <0.001 |
| High AISI | 7.73 | 5.06–11.85 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vunvulea, V.; Melinte, R.M.; Brinzaniuc, K.; Suciu, B.A.; Ivănescu, A.D.; Hălmaciu, I.; Incze-Bartha, Z.; Pastorello, Y.; Trâmbițaș, C.; Mărginean, L.; et al. Blood Count-Derived Inflammatory Markers Correlate with Lengthier Hospital Stay and Are Predictors of Pneumothorax Risk in Thoracic Trauma Patients. Diagnostics 2023, 13, 954. https://doi.org/10.3390/diagnostics13050954
Vunvulea V, Melinte RM, Brinzaniuc K, Suciu BA, Ivănescu AD, Hălmaciu I, Incze-Bartha Z, Pastorello Y, Trâmbițaș C, Mărginean L, et al. Blood Count-Derived Inflammatory Markers Correlate with Lengthier Hospital Stay and Are Predictors of Pneumothorax Risk in Thoracic Trauma Patients. Diagnostics. 2023; 13(5):954. https://doi.org/10.3390/diagnostics13050954
Chicago/Turabian StyleVunvulea, Vlad, Răzvan Marian Melinte, Klara Brinzaniuc, Bogdan Andrei Suciu, Adrian Dumitru Ivănescu, Ioana Hălmaciu, Zsuzsanna Incze-Bartha, Ylenia Pastorello, Cristian Trâmbițaș, Lucian Mărginean, and et al. 2023. "Blood Count-Derived Inflammatory Markers Correlate with Lengthier Hospital Stay and Are Predictors of Pneumothorax Risk in Thoracic Trauma Patients" Diagnostics 13, no. 5: 954. https://doi.org/10.3390/diagnostics13050954
APA StyleVunvulea, V., Melinte, R. M., Brinzaniuc, K., Suciu, B. A., Ivănescu, A. D., Hălmaciu, I., Incze-Bartha, Z., Pastorello, Y., Trâmbițaș, C., Mărginean, L., Kaller, R., Kassas, A., & Hogea, T. (2023). Blood Count-Derived Inflammatory Markers Correlate with Lengthier Hospital Stay and Are Predictors of Pneumothorax Risk in Thoracic Trauma Patients. Diagnostics, 13(5), 954. https://doi.org/10.3390/diagnostics13050954








