Differentiating Fordyce Spots from Their Common Simulators Using Ultraviolet-Induced Fluorescence Dermatoscopy—Retrospective Study
Abstract
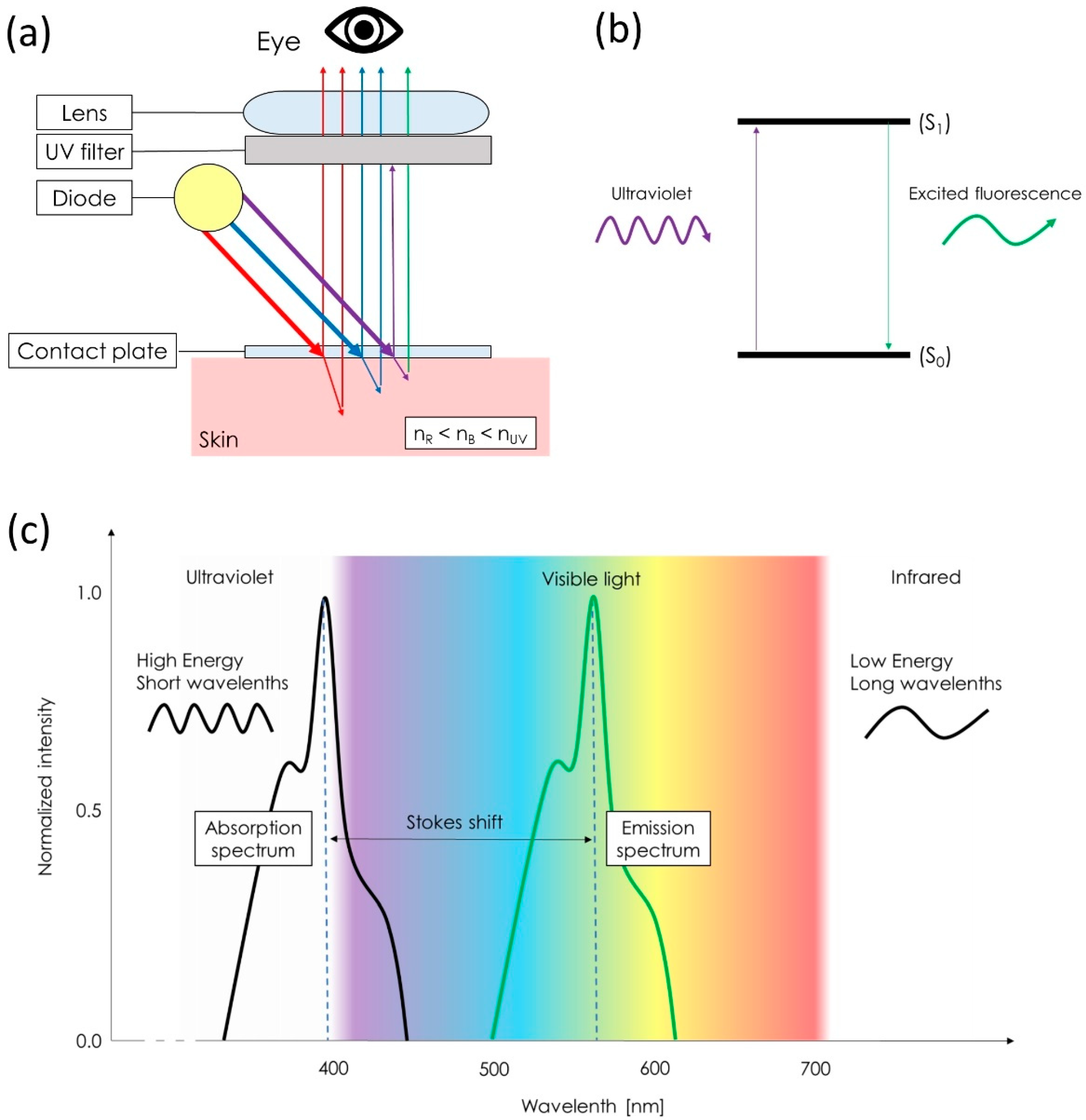
1. Introduction
2. Materials and Methods
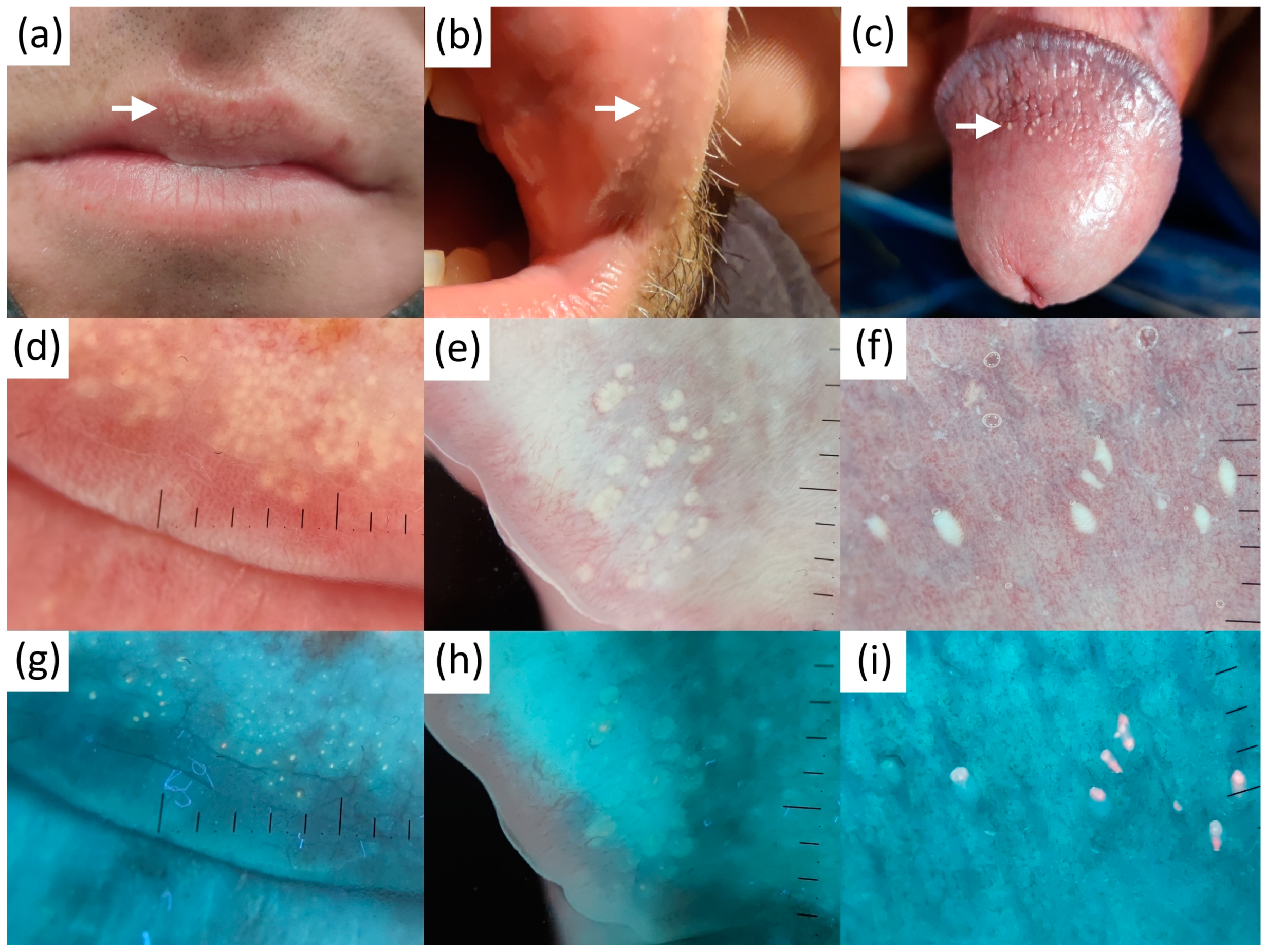
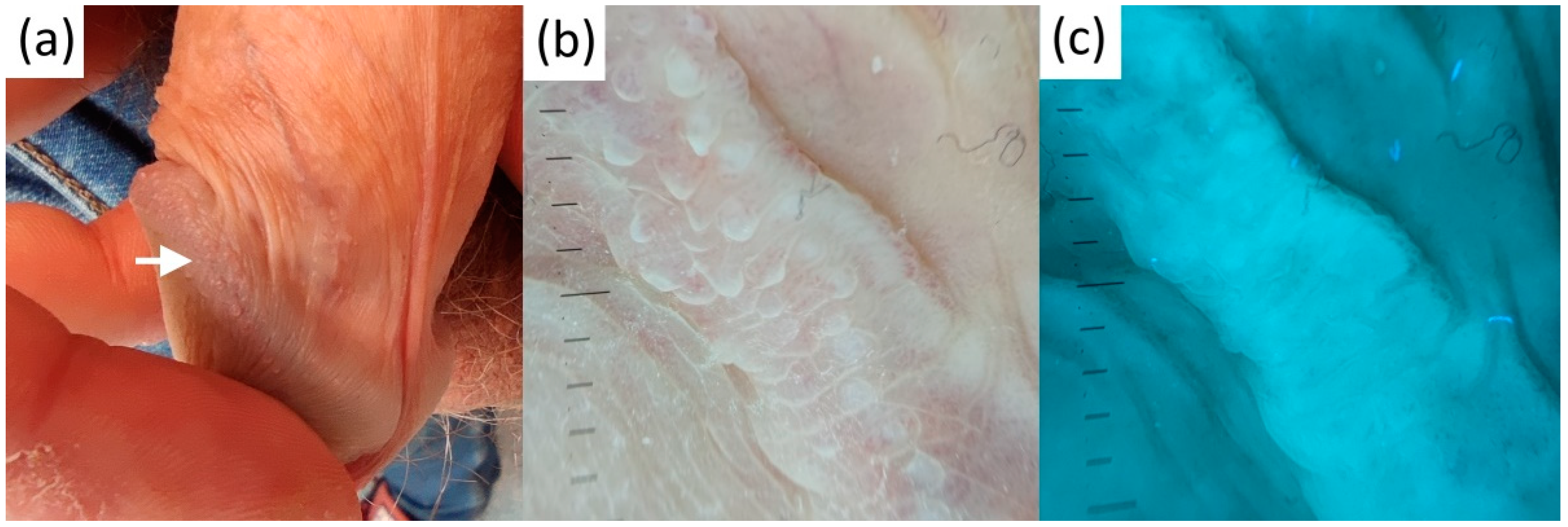
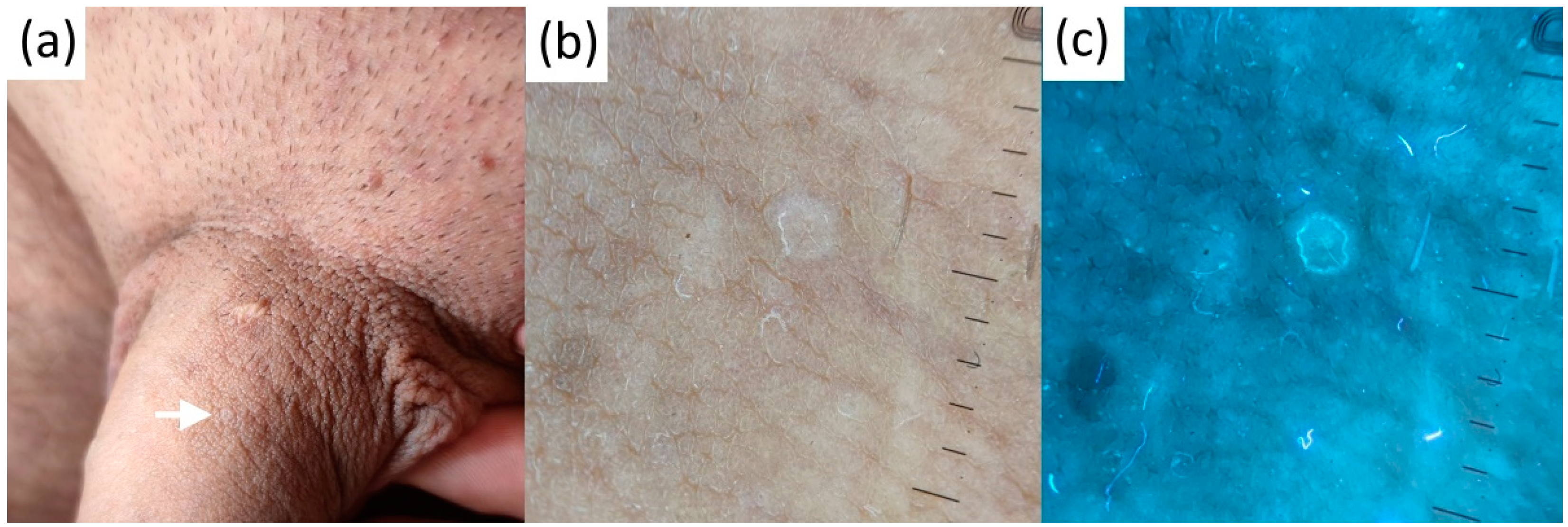
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carli, P.; de Giorgi, V.; Chiarugi, A.; Nardini, P.; Weinstock, M.A.; Crocetti, E.; Stante, M.; Giannotti, B. Addition of dermoscopy to conventional naked-eye examination in melanoma screening: A randomized study. J. Am. Acad. Dermatol. 2004, 50, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, M.E.; Macaskill, P.; Holt, P.E.; Menzies, S.W. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: A meta-analysis of studies performed in a clinical setting. Br. J. Dermatol. 2008, 159, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Kapsokalyvas, D.; Bruscino, N.; Alfieri, D.; de Giorgi, V.; Cannarozzo, G.; Cicchi, R.; Massi, D.; Pimpinelli, N.; Pavone, F.S. Spectral morphological analysis of skin lesions with a polarization multispectral dermoscope. Opt. Express 2013, 21, 4826–4840. [Google Scholar] [CrossRef] [PubMed]
- Suhai, B.; Horváth, G. How well does the Rayleigh model describe the E-vector distribution of skylight in clear and cloudy conditions? A full-sky polarimetric study. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2004, 21, 1669–1676. [Google Scholar] [CrossRef] [PubMed]
- Mojeski, J.A.; Almashali, M.; Jowdy, P.; Fitzgerald, M.E.; Brady, K.L.; Zeitouni, N.C.; Colegio, O.R.; Paragh, G. Ultraviolet imaging in dermatology. Photodiagnosis Photodyn. Ther. 2020, 30, 101743. [Google Scholar] [CrossRef]
- Tang, J.; Ran, Y. Polarized and ultraviolet dermoscopy for the diagnosis of dermatophytosis of vellus hair. IJDVL 2020, 86, 607. [Google Scholar]
- Szepetiuk, G.; Piérard-Franchimont, C.; Quatresooz, P.; Piérard, G.E. Physico-biological foundation of skin fluorescence--review. Pathol. Biol. 2012, 60, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Pietkiewicz, P.; Navarrete-Dechent, C. Scabies mite is bright green under UV dermatoscopy. Dermatol. Pract. Concept 2023, 13, e2023135. [Google Scholar] [CrossRef]
- Al-Nasiri, M.; Navarrete-Dechent, C.; Korecka, C.; Salwowska, N.; Goldust, M.; Pietkiewicz, P. Ultraviolet reflectance dermatoscopy of trichobacteriosis axillaris reveals peripilar yellow-green luminescent concretions. Dermatol. Pract. Concept 2023, 13. Online ahead of print. [Google Scholar] [CrossRef]
- Fordyce, J.A. A peculiar affection of the mucous membrane of the lips and oral cavity. J. Cutan Dis. 1896, 14, 413–419. [Google Scholar] [CrossRef]
- Tsuji, T.; Yamauchi, R. Areolar sebaceous hyperplasia with a Fordyce’s spot-like lesion. J. Dermatol. 1994, 21, 524–526. [Google Scholar] [CrossRef] [PubMed]
- Belinchón, I.; Aguilar, A.; Tardío, J.; Gallego, M.A. Areolar sebaceous hyperplasia: A case report. Cutis 1996, 58, 63–64. [Google Scholar]
- Mansur, A.T.; Aydingoz, I.E. Unilateral buccal fordyce spots with ipsilateral facial paralysis: A sign of neuro-sebaceous connection? Acta Derm. Venereol. 2012, 92, 177–178. [Google Scholar] [CrossRef]
- Errichetti, E.; Piccirillo, A.; Viola, L.; Ricciuti, F.; Ricciuti, F. Areolar sebaceous hyperplasia associated with oral and genital Fordyce spots. J. Dermatol. 2013, 40, 670. [Google Scholar] [CrossRef]
- Lester, R.A.; Torgerson, R.R.; Sandhu, N.P. Rare presentation of sebaceous hyperplasia. BMJ Case Rep. 2014, 2014, bcr2014204025. [Google Scholar] [CrossRef] [PubMed]
- Montalvo, N.; Tapia, V.; Padilla, H.; Redrobán, L. Heterotopic sebaceous glands in the esophagus, a very rare histopathological diagnosis: A case report and review of the literature. Clin. Case Rep. 2016, 5, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Kansky, A.A.; Didanovic, V.; Dovsak, T.; Brzak, B.L.; Pelivan, I.; Terlevic, D. Epidemiology of oral mucosal lesions in Slovenia. Radiol. Oncol. 2018, 52, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Lam, J.M. A teenage boy with asymptomatic papules on his upper lip. Paediatr. Child Health 2018, 23, 499–500. [Google Scholar] [CrossRef]
- Thirunavukkarasu, B.; Nada, R.; Dawra, S.; Sinha, S.K. Ectopic sebaceous glands in oesophagus. BMJ Case Rep. 2019, 12, e232736. [Google Scholar] [CrossRef]
- Le, A.; Amin, M.; Cappell, M.S. Case Report of a Proposed, Novel, Endoscopic ‘Whitehead Pimple’ Sign of Ectopic Esophageal Sebaceous Glands Based on Their Mimicking the Dermatologic and Histopathologic Characteristics of Cutaneous Whitehead Pimples/Closed Comedones. Dig. Dis. Sci. 2019, 64, 2049–2053. [Google Scholar] [CrossRef]
- Schachner, L.A.; Hansen, R.C. Pediatric Dermatology; Elsevier Health Sciences: Philadelphia, PA, USA, 2011; p. 1808. [Google Scholar]
- Baeder, F.M.; Pelino, J.E.P.; de Almeida, E.R.; Duarte, D.A.; Santos, M.T.B.R. High-power diode laser use on Fordyce granule excision: A case report. J. Cosmet. Dermatol. 2010, 9, 321–324. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, J.H.; Kwon, N.H.; Yu, D.S.; Kim, G.M.; Park, C.J.; Lee, J.D.; Kim, S.Y. Clinicopathologic Manifestations of Patients with Fordyce’s Spots. Ann. Dermatol. 2012, 24, 103–106. [Google Scholar] [CrossRef]
- Elston, D.M.; Meffert, J. Photo quiz. What is your diagnosis? Fordyce Spots. Cutis 2001, 68, 24–49. [Google Scholar] [PubMed]
- Radhakrishnan, S.; Agarwal, D.C. Fordyce spots masquerading as penile warts. Med. J. Armed Forces India 2016, 72, 384–385. [Google Scholar] [CrossRef] [PubMed]
- Iwata, K.; Katsuda, Y. Somatic symptoms after sexual behavior with fear of four sexually transmitted diseases: A proposal of novel disorder. J. Family Med. Prim. Care 2016, 5, 706–708. [Google Scholar] [CrossRef]
- Flinck, A.; Paludan, A.; Matsson, L.; Holm, A.K.; Axelsson, I. Oral findings in a group of newborn Swedish children. Int. J. Paediatr. Dent. 1994, 4, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Arun Babu, T.; Vijayadevagaran, V.; Carounanidy, U. Congenital intraoral Fordyce spots. Arch Dis. Child. Fetal. Neonatal. Ed. 2016, 101, F252. [Google Scholar] [CrossRef]
- Ramachandran, S.; Kalra, S.; Shaw, S.C. Fordyce Spots in a Neonate. Indian Pediatr. 2022, 59, 91. [Google Scholar] [PubMed]
- Gaballah, K.Y.; Rahimi, I. Can presence of oral Fordyce’s granules serve as a marker for hyperlipidemia? Dent. Res. J. (Isfahan) 2014, 11, 553–558. [Google Scholar] [PubMed]
- De Felice, C.; Parrini, S.; Chitano, G.; Gentile, M.; Dipaola, L.; Latini, G. Fordyce granules and hereditary non-polyposis colorectal cancer syndrome. Gut 2005, 54, 1279–1282. [Google Scholar] [CrossRef]
- Ponti, G.; Meschieri, A.; Pollio, A.; Ruini, C.; Manfredini, M.; Longo, C.; Mandel, V.D.; Ciardo, S.; Tomasi, A.; Giannetti, L.; et al. Fordyce granules and hyperplastic mucosal sebaceous glands as distinctive stigmata in Muir-Torre syndrome patients: Characterization with reflectance confocal microscopy. J. Oral Pathol. Med. 2015, 44, 552–557. [Google Scholar] [CrossRef]
- Fernandez-Flores, A.; Rodríguez Peralto, J.L. Mismatch Repair Protein Expression in Fordyce Granules. Appl. Immunohistochem. Mol. Morphol. 2017, 25, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Chern, P.L.; Arpey, C.J. Fordyce spots of the lip responding to electrodesiccation and curettage. Dermatol. Surg. 2008, 34, 960–962. [Google Scholar] [PubMed]
- Pallua, N.; Stromps, J.P. Micro-punch technique for treatment of Fordyce spots: A surgical approach for an unpleasant condition of the male genital. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, e8–e11. [Google Scholar] [CrossRef] [PubMed]
- Plotner, A.N.; Brodell, R.T. Treatment of Fordyce spots with bichloracetic acid. Dermatol. Surg. 2008, 34, 397–399; discussion 399. [Google Scholar]
- Kim, Y.J.; Kang, H.Y.; Lee, E.S.; Kim, Y.C. Treatment of Fordyce spots with 5-aminolaevulinic acid-photodynamic therapy. Br. J. Dermatol. 2007, 156, 399–400. [Google Scholar] [CrossRef]
- Richey, D.F. Aminolevulinic acid photodynamic therapy for sebaceous gland hyperplasia. Dermatol. Clin. 2007, 25, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Gold, M.H.; Bradshaw, V.L.; Boring, M.M.; Bridges, T.M.; Biron, J.A.; Lewis, T.L. Treatment of sebaceous gland hyperplasia by photodynamic therapy with 5-aminolevulinic acid and a blue light source or intense pulsed light source. J. Drugs Dermatol. 2004, 3 (Suppl. S6), S6–S9. [Google Scholar]
- Ahn, G.R.; Park, S.J.; Lee, C.K.; Kim, B.J. A case of successful treatment of Fordyce spots with a single insulated microneedle radiofrequency device. Dermatol. Ther. 2019, 32, e13026. [Google Scholar] [CrossRef]
- Ryu, S.I.; Jeong, J.Y.; Kim, K.E.; Ryu, H.J. Fordyce Spots Treated by an Intralesional Insulated Microneedle Radiofrequency Device. Dermatol. Surg. 2021, 47, 1021–1022. [Google Scholar] [CrossRef]
- Mutizwa, M.M.; Berk, D.R. Dichotomous long-term response to isotretinoin in two patients with fordyce spots. Pediatr. Dermatol. 2014, 31, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Handiani, F.; Sadati, M.S. Isotretinoin-induced regression of Fordyce spots in a patient with acne: The first report. G Ital. Dermatol. Venereol. 2015, 150, 343–344. [Google Scholar] [PubMed]
- Kim, S.K.; Do, J.E.; Kang, H.Y.; Lee, E.S.; Kim, Y.C. Combination of topical 5-aminolevulinic acid-photodynamic therapy with carbon dioxide laser for sebaceous hyperplasia. J. Am. Acad. Dermatol. 2007, 56, 523–524. [Google Scholar] [CrossRef] [PubMed]
- Jakhar, D.; Kaur, I. Mucoscopy of Fordyce’s Spots on Lips. Indian Dermatol. Online J. 2019, 10, 498–499. [Google Scholar] [CrossRef]
- Errichetti, E.; Zalaudek, I.; Kittler, H.; Apalla, Z.; Argenziano, G.; Bakos, R.; Blum, A.; Braun, R.P.; Ioannides, D.; Lacarrubba, F.; et al. Standardization of dermoscopic terminology and basic dermoscopic parameters to evaluate in general dermatology (non-neoplastic dermatoses): An expert consensus on behalf of the International Dermoscopy Society. Br. J. Dermatol. 2020, 182, 454–467. [Google Scholar] [CrossRef]
- Arrazola, P.; Mullani, N.A.; Abramovits, W. DermLite II: An innovative portable instrument for dermoscopy without the need of immersion fluids. Skinmed 2005, 4, 78–83. [Google Scholar] [PubMed]
- Thoreson, W.B.; Dacey, D.M. Diverse Cell Types, Circuits, and Mechanisms for Color Vision in the Vertebrate Retina. Physiol. Rev. 2019, 99, 1527–1573. [Google Scholar] [CrossRef] [PubMed]
- Hammond, B.R.; Renzi-Hammond, L. Individual variation in the transmission of UVB radiation in the young adult eye. PLoS ONE 2018, 13, e0199940. [Google Scholar] [CrossRef]
- Dyer, J.M.; Foy, V.M. Revealing The Unseen: A Review of Wood’s Lamp in Dermatology. J. Clin. Aesthet. Dermatol. 2022, 15, 25–30. [Google Scholar]
- Ruiz-Pino, M.; Foronda-García-Hidalgo, C.; Alarcón-Blanco, P.; Gutiérrez-Fernández, J. Male genitourinary infections by Corynebacterium glucuronolyticum. A review and clinical experience. Rev. Esp. Quimioter. 2019, 32, 479–484. [Google Scholar]
- Asawanonda, P.; Taylor, C.R. Wood’s light in dermatology. Int. J. Dermatol. 1999, 38, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Navarrete-Dechent, C.; Uribe, P.; Marghoob, A. Ink-enhanced dermoscopy is a useful tool to differentiate acquired solitary plaque porokeratosis from other scaly lesions. J. Am. Acad. Dermatol. 2019, 80, e137–e138. [Google Scholar] [CrossRef] [PubMed]
- Zaar, O.; Polesie, S.; Navarrete-Dechent, C.; Errichetti, E.; Akay, B.N.; Jaimes, J.; Cabo, H.; Sabban, E.C.; Paoli, J. Dermoscopy of porokeratosis: Results from a multicentre study of the International Dermoscopy Society. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 2091–2096. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, B.B.; Shishak, M. An approach to venerophobia in males. Indian J. Sex Transm. Dis. AIDS 2017, 38, 103–106. [Google Scholar]
- Sonthalia, S.; Errichetti, E. Dermoscopy—Not just for diagnosis and not just for Dermatologists! Kathmandu Univ. Med. J. (KUMJ) 2017, 15, 1–2. [Google Scholar] [PubMed]
- Micali, G.; Lacarrubba, F. Augmented diagnostic capability using videodermatoscopy on selected infectious and non-infectious penile growths. Int. J. Dermatol. 2011, 50, 1501–1505. [Google Scholar] [CrossRef] [PubMed]



| No | Age | Sex | Ethnicity | Site | Clinical Presentation of Fordyce Spots | Context |
|---|---|---|---|---|---|---|
| 1 | 33 | M | Caucasian | Upper lip | Flat, poorly defined yellow-white papules grouped along the vermilion | STI suspect |
| 2 | 38 | M | Caucasian | Upper lip | Palpable, elevated well-defined yellowish papules grouped bilaterally in the vicinity of labial commissure of the mouth | Incidental finding |
| 3 | 33 | M | Caucasian | Upper lip | Slightly elevated, well-defined yellow-white papules grouped above the tubercle of the lip | STI suspect |
| 4 | 23 | M | Caucasian | Foreskin | Slightly elevated, well-defined yellow-white papules grouped bilaterally in the proximity of frenulum | STI suspect |
| 5 | 35 | M | Caucasian | Upper lip | Flat, poorly defined yellow-white papules grouped along the vermilion | Incidental finding |
| 6 | 28 | M | Caucasian | Foreskin | Slightly elevated, poorly defined scant yellow-white papules located bilaterally in the proximity of frenulum | Incidental finding |
| 7 | 30 | M | Caucasian | Foreskin | Slightly elevated, poorly defined scant yellow-white papules located bilaterally in the proximity of frenulum | Incidental finding |
| 8 | 43 | M | Caucasian | Upper lip | Flat, poorly defined yellow-white papules grouped unilaterally in the vicinity of left labial commissure of the mouth | Incidental finding |
| 9 | 40 | M | Caucasian | Foreskin | Slightly elevated, poorly defined scant yellow-white papules located bilaterally in the proximity of frenulum | STI suspect |
| 10 | 29 | M | Caucasian | Glans | Slightly elevated, poorly defined scant yellow-white papules clustered on the left dorsal surface | Incidental finding |
| 11 | 31 | M | Caucasian | Glans | Elevated, well-defined yellow-white papules clustered on the mid-dorsal surface | STI suspect |
| 12 | 34 | F | Caucasian | Upper lip | Elevated, well-defined yellow-white papules grouped along the vermilion | Incidental finding |
| No | Age | Sex | Ethnicity | Site | Diagnosis/Clinical Presentation | Context |
|---|---|---|---|---|---|---|
| 1 | 47 | M | Caucasian | Glans | Genital lichen planus/slightly elevated whitepapules and annular lesions on the glans | STI suspect |
| 2 | 23 | M | Caucasian | Glans | Genital lichen planus/coalescing flat-top papules on the glans and foreskin | STI suspect |
| 3 | 9 | F | Caucasian | Pubis | Molluscum contagiosum/solitary umbilicatedpapule | Incidental finding |
| 4.1 | 6 | M | Caucasian | Neck | Molluscum contagiosum/multiple disseminated umbilicated papules | Incidental finding |
| 4.2 | 6 | M | Caucasian | Neck | Molluscum contagiosum/multiple disseminated umbilicated papules | Incidental finding |
| 4.3 | 6 | M | Caucasian | Scalp | Molluscum contagiosum/solitary umbilicatedpapule | Incidental finding |
| 5.1 | 41 | M | Caucasian | Pubis | Molluscum contagiosum/multiple disseminated and grouped umbilicated papules | STI suspect |
| 5.2 | 41 | M | Caucasian | Pubis | Molluscum contagiosum/multiple disseminated and grouped umbilicated papules | STI suspect |
| 5.3 | 41 | M | Caucasian | Pubis | Molluscum contagiosum/multiple disseminated and grouped umbilicated papules | STI suspect |
| 5.4 | 41 | M | Caucasian | Pubis | Molluscum contagiosum/multiple disseminated and grouped umbilicated papules | STI suspect |
| 6 | 28 | M | Caucasian | Glans | Penile pearly papules/multiple white papuleslocated on the corona of the penis | STI suspect |
| 7 | 43 | M | Caucasian | Glans | Penile pearly papules/multiple white papuleslocated on the corona of the penis | Incidental finding |
| 8 | 31 | M | Caucasian | Glans | Penile pearly papules/multiple white papuleslocated on the corona of the penis | STI suspect |
| 9.1 | 45 | F | Caucasian | Popliteal fossa | Viral wart/solitary hyperkeratotic skin-colored papule | Incidental finding |
| 9.2 | 45 | F | Caucasian | Upper leg | Viral wart/solitary hyperkeratotic skin-colored papule | Incidental finding |
| 10 | 21 | M | Caucasian | Areola | Viral wart/solitary hyperkeratotic skin-colored papule | Incidental finding |
| 11 | 47 | M | Caucasian | Foreskin | Viral wart/solitary skin-colored papule | STI suspect |
| 12 | 35 | M | Caucasian | Penile shaft | Viral wart/multiple disseminated skin-colored papules | STI suspect |
| 13 | 44 | M | Caucasian | Pubis | Viral wart/multiple disseminated skin-colored papules | STI suspect |
| 14 | 32 | M | Caucasian | Penile shaft | Genital porokeratosis/disseminated scaly papules in the genital area | STI suspect |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pietkiewicz, P.; Navarrete-Dechent, C.; Goldust, M.; Korecka, K.; Todorovska, V.; Errichetti, E. Differentiating Fordyce Spots from Their Common Simulators Using Ultraviolet-Induced Fluorescence Dermatoscopy—Retrospective Study. Diagnostics 2023, 13, 985. https://doi.org/10.3390/diagnostics13050985
Pietkiewicz P, Navarrete-Dechent C, Goldust M, Korecka K, Todorovska V, Errichetti E. Differentiating Fordyce Spots from Their Common Simulators Using Ultraviolet-Induced Fluorescence Dermatoscopy—Retrospective Study. Diagnostics. 2023; 13(5):985. https://doi.org/10.3390/diagnostics13050985
Chicago/Turabian StylePietkiewicz, Paweł, Cristian Navarrete-Dechent, Mohamad Goldust, Katarzyna Korecka, Verce Todorovska, and Enzo Errichetti. 2023. "Differentiating Fordyce Spots from Their Common Simulators Using Ultraviolet-Induced Fluorescence Dermatoscopy—Retrospective Study" Diagnostics 13, no. 5: 985. https://doi.org/10.3390/diagnostics13050985
APA StylePietkiewicz, P., Navarrete-Dechent, C., Goldust, M., Korecka, K., Todorovska, V., & Errichetti, E. (2023). Differentiating Fordyce Spots from Their Common Simulators Using Ultraviolet-Induced Fluorescence Dermatoscopy—Retrospective Study. Diagnostics, 13(5), 985. https://doi.org/10.3390/diagnostics13050985











