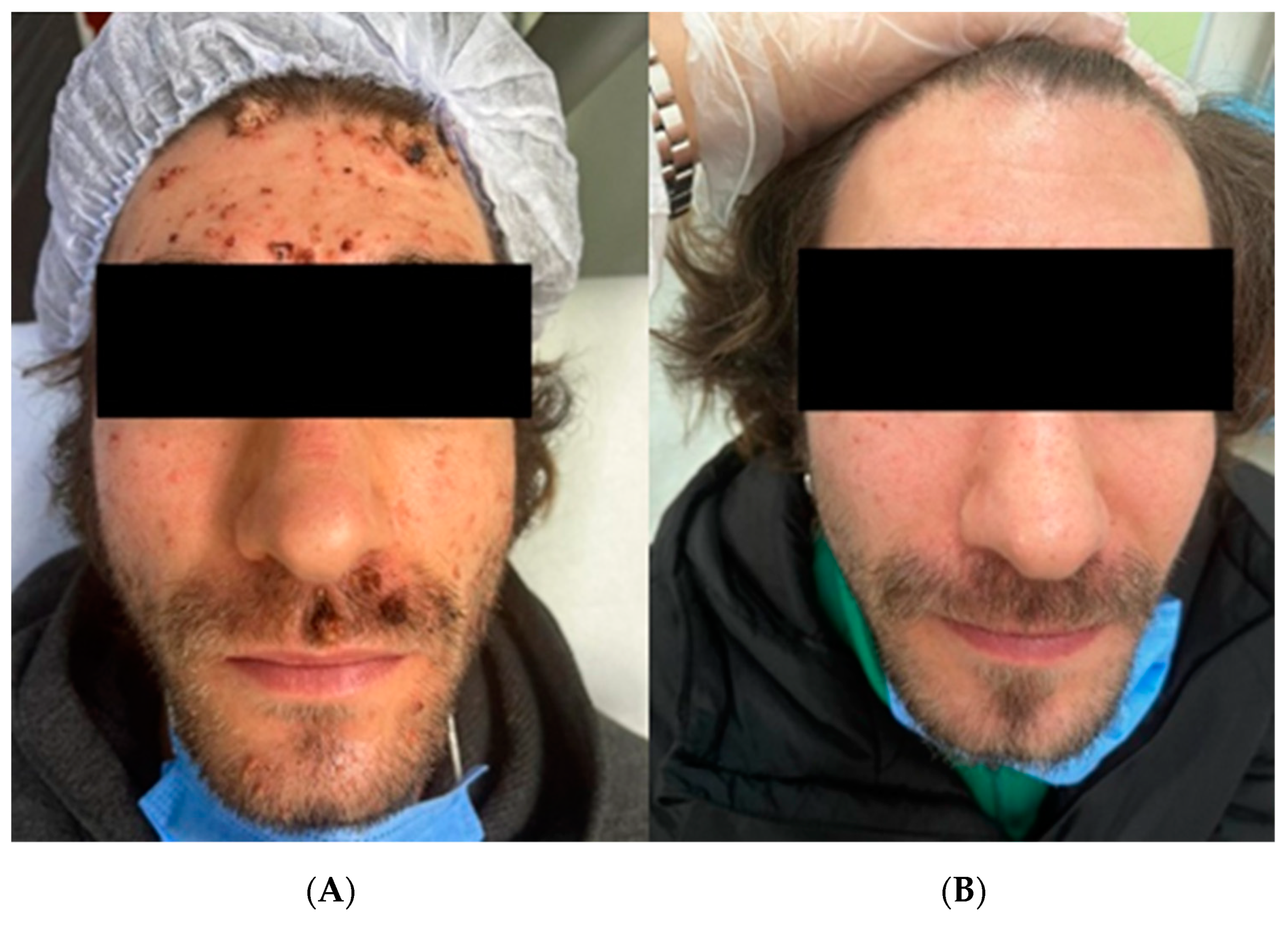
Photodynamic Therapy Used to Treat an HIV Patient with an Efflorescence of Viral Warts after HAART Therapy
Abstract
:Figures


Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cubie, H.A. Diseases associated with human papillomavirus infection. Virology 2013, 445, 21–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruggink, S.C.; Eekhof, J.A.H.; Egberts, P.F.; van Blijswijk, S.C.E.; Assendelft, W.J.J.; Gussekloo, J. Natural Course of Cutaneous Warts Among Primary Schoolchildren: A Prospective Cohort Study. Ann. Fam. Med. 2013, 11, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Lipke, M.M. An Armamentarium of Wart Treatments. Clin. Med. Res. 2006, 4, 273–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dall’Oglio, F.; D’Amico, V.; Nasca, M.R.; Micali, G. Treatment of cutaneous warts: An evidence-based review. Am. J. Clin. Dermatol. 2012, 13, 73–96. [Google Scholar] [CrossRef]
- Shen, S.; Feng, J.; Song, X.; Xiang, W. Efficacy of photodynamic therapy for warts induced by human papilloma virus infection: A systematic review and meta-analysis. Photodiagnosis Photodyn. Ther. 2022, 39, 102913. [Google Scholar] [CrossRef] [PubMed]
- Ozog, D.M.; Rkein, A.M.; Fabi, S.G.; Gold, M.H.; Goldman, M.P.; Lowe, N.J.; Martin, G.M.; Munavalli, G.S. Photodynamic Therapy: A Clinical Consensus Guide. Dermatol. Surg. 2016, 42, 804–827. [Google Scholar] [CrossRef] [PubMed]
- Manga, M.M.; Fowotade, A.; Yahaya, M. Human Papillomavirus (HPV) Infection in Males: A Need for More Awareness. In Current Perspectives in Human Papillomavirus; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef] [Green Version]
- Monfrecola, G.; Megna, M.; Rovati, C.; Arisi, M.; Rossi, M.; Calzavara-Pinton, I.; Fabbrocini, G.; Calzavara-Pinton, P. A Critical Reappraisal of Off-Label Use of Photodynamic Therapy for the Treatment of Non-Neoplastic Skin Conditions. Dermatology 2021, 237, 262–276. [Google Scholar] [CrossRef]
- Morton, C.A.; Szeimies, R.M.; Basset-Séguin, N.; Calzavara-Pinton, P.G.; Gilaberte, Y.; Hædersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 Part 2: Emerging indications—Field cancerization, photorejuvenation and inflammatory/infective dermatoses. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 17–29. [Google Scholar] [CrossRef]
- Ginat, D.T.; Schaefer, P.W. Highly Active Antiretroviral Therapy (HAART). In Neuroimaging Pharmacopoeia; Springer Nature Switzerland AG.: Cham, Switzerland, 2022; pp. 203–212. [Google Scholar] [CrossRef]
- Wang, H.; Xiong, L.; Xia, Y.; Wang, X. 5-aminolaevulinic acid-based photodynamic therapy induces both necrosis and apoptosis of keratinocytes in plantar warts. J. Cosmet. Laser Ther. 2020, 22, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Alcántara-González, J.; Calzado-Villarreal, L.; Sánchez-Largo, M.E.; Andreu-Barasoain, M.; Salado, M.R.-D. Recalcitrant viral warts treated with photodynamic therapy methyl aminolevulinate and red light (630 nm): A case series of 51 patients. Lasers Med. Sci. 2020, 35, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Ohtsuki, A.; Hasegawa, T.; Hirasawa, Y.; Tsuchihashi, H.; Ikeda, S. Photodynamic therapy using light-emitting diodes for the treatment of viral warts. J. Dermatol. 2009, 36, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Foresto, E.; Gilardi, P.; Ibarra, L.E.; Cogno, I.S. Light-activated green drugs: How we can use them in photodynamic therapy and mass-produce them with biotechnological tools. Phytomedicine Plus 2021, 1, 100044. [Google Scholar] [CrossRef]
- Romero, M.P.; Jibaja, I.; Bucheli, J.; Inada, N.; Bagnato, V. Clinical study of anogenital condyloma acuminata treatment with photodynamic therapy including immunocompromised conditions. Photodiagnosis Photodyn. Ther. 2022, 37, 102735. [Google Scholar] [CrossRef] [PubMed]
- Caucanas, M.; Gillard, P.; Vanhooteghem, O. Efficiency of Photodynamic Therapy in the Treatment of Diffuse Facial Viral Warts in an Immunosuppressed Patient: Towards a Gold Standard? Case Rep Derm. 2010, 2, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Parietti, M.; Trunfio, M.; Delmonte, S.; Conti, L.; Trentalange, A.; Bonora, S.; Calcagno, A.; Ribero, S. Efflorescence of acquired epidermodysplasia verruciformis due to immune reconstitution inflammatory syndrome-like mechanisms following anti-HPV vaccination in a HIV-positive patient. Int. J. STD AIDS 2022, 33, 94–96. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ambrogio, F.; Meduri, A.R.; Infante, G.; Poli, M.A.; Romita, P.; Bonamonte, D.; Filotico, R.; Ingravallo, G.; Cazzato, G.; Laface, C.; et al. Photodynamic Therapy Used to Treat an HIV Patient with an Efflorescence of Viral Warts after HAART Therapy. Diagnostics 2023, 13, 1098. https://doi.org/10.3390/diagnostics13061098
Ambrogio F, Meduri AR, Infante G, Poli MA, Romita P, Bonamonte D, Filotico R, Ingravallo G, Cazzato G, Laface C, et al. Photodynamic Therapy Used to Treat an HIV Patient with an Efflorescence of Viral Warts after HAART Therapy. Diagnostics. 2023; 13(6):1098. https://doi.org/10.3390/diagnostics13061098
Chicago/Turabian StyleAmbrogio, Francesca, Alexandre Raphael Meduri, Giovanni Infante, Melita Anna Poli, Paolo Romita, Domenico Bonamonte, Raffaele Filotico, Giuseppe Ingravallo, Gerardo Cazzato, Carmelo Laface, and et al. 2023. "Photodynamic Therapy Used to Treat an HIV Patient with an Efflorescence of Viral Warts after HAART Therapy" Diagnostics 13, no. 6: 1098. https://doi.org/10.3390/diagnostics13061098
APA StyleAmbrogio, F., Meduri, A. R., Infante, G., Poli, M. A., Romita, P., Bonamonte, D., Filotico, R., Ingravallo, G., Cazzato, G., Laface, C., De Marco, A., & Foti, C. (2023). Photodynamic Therapy Used to Treat an HIV Patient with an Efflorescence of Viral Warts after HAART Therapy. Diagnostics, 13(6), 1098. https://doi.org/10.3390/diagnostics13061098








