Assessment of Fast-Track Pathway in Hip and Knee Replacement Surgery by Propensity Score Matching on Patient-Reported Outcomes
Abstract
:1. Introduction
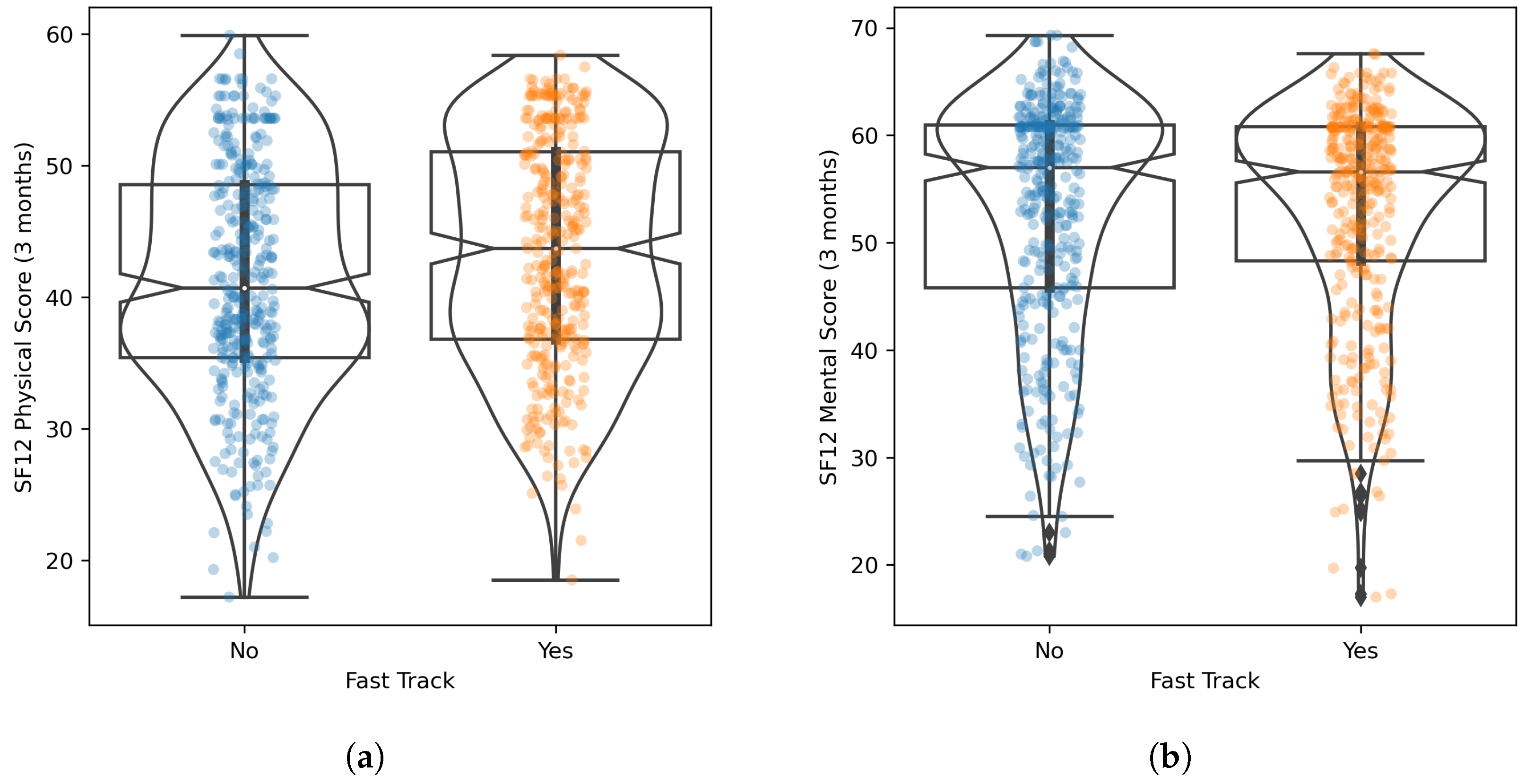
- (RQ1):
- Does the Fast Track pathway (including rehabilitation) have a positive impact on health status (as measured by the SF-12 Physical and Mental scores), compared with the Care-as-Usual one?
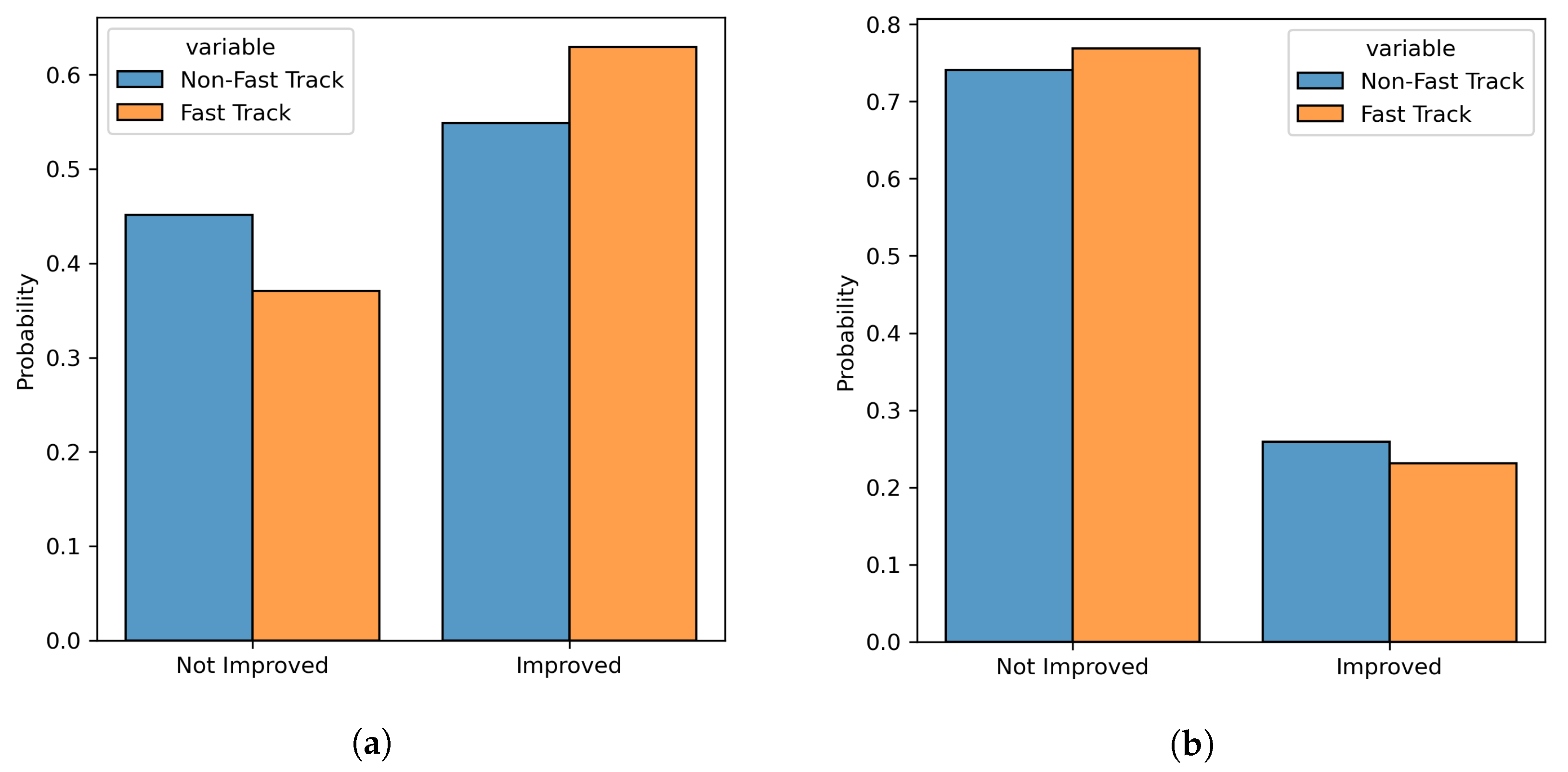
- (RQ2):
- Does the Fast Track pathway lead to a better improvement in health status (measured with respect to the pre-operative stage), compared with the Care-as-Usual one?
2. Methods
2.1. Study Design and Cohort Description
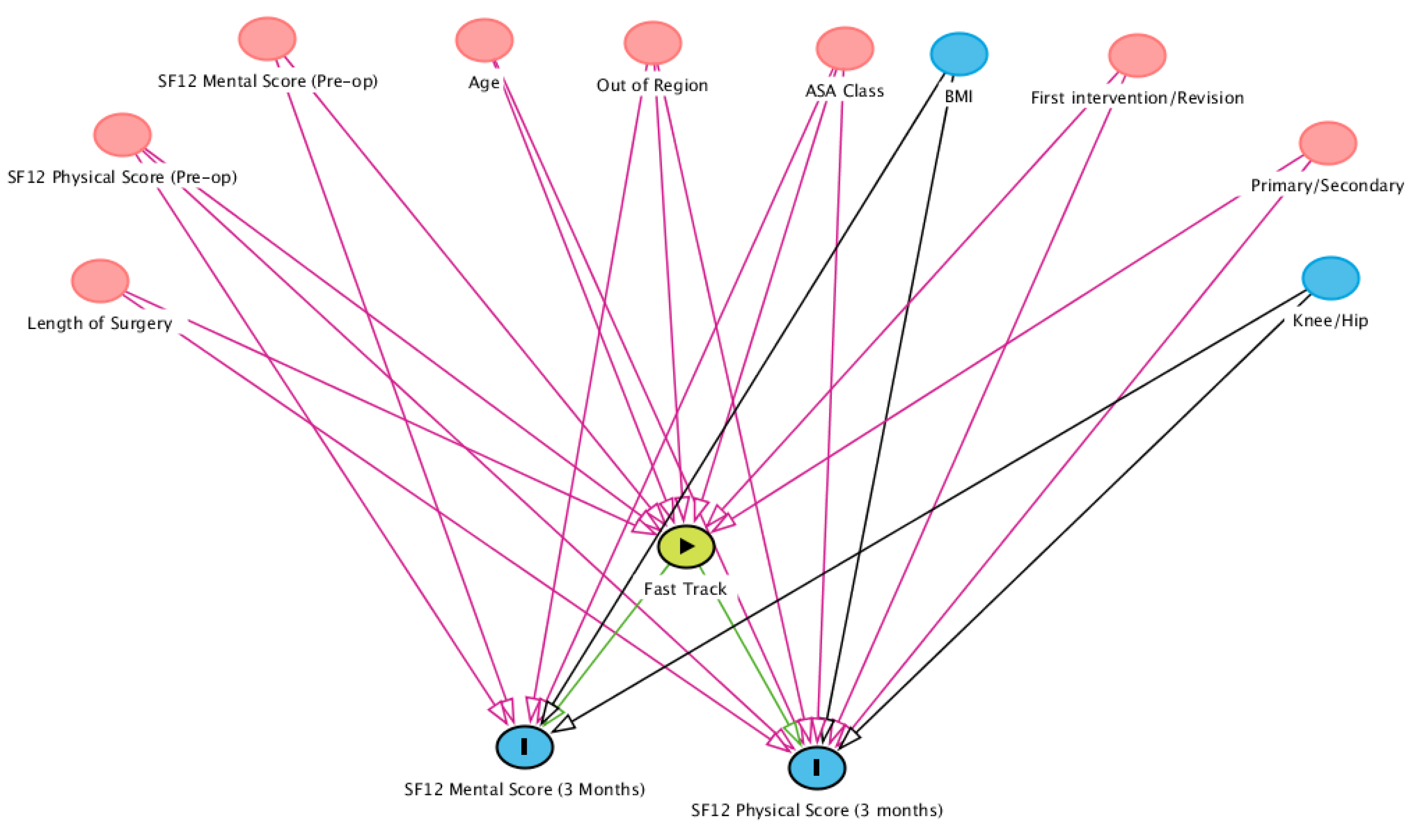
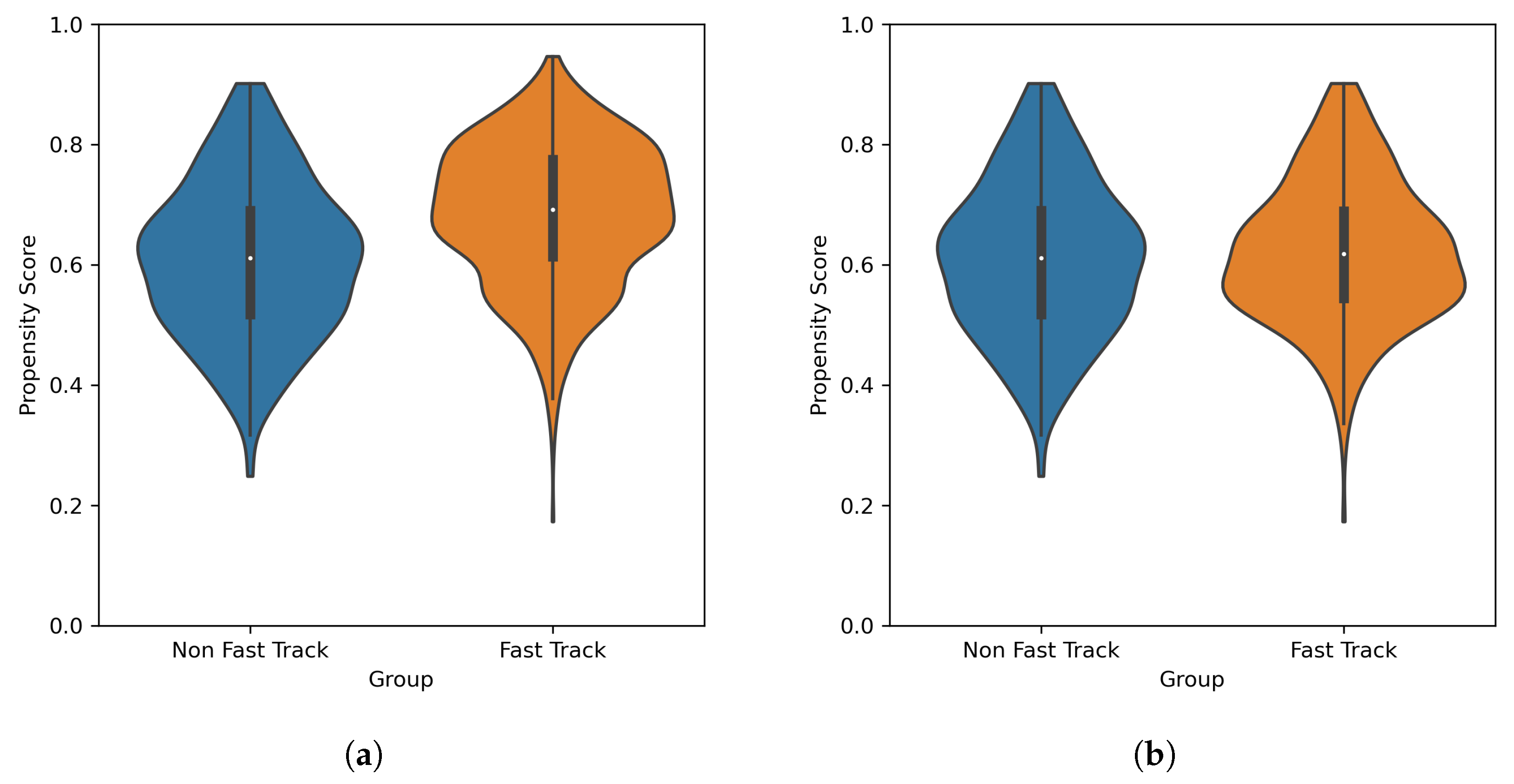
2.2. Statistical Methods: Propensity Score Matching
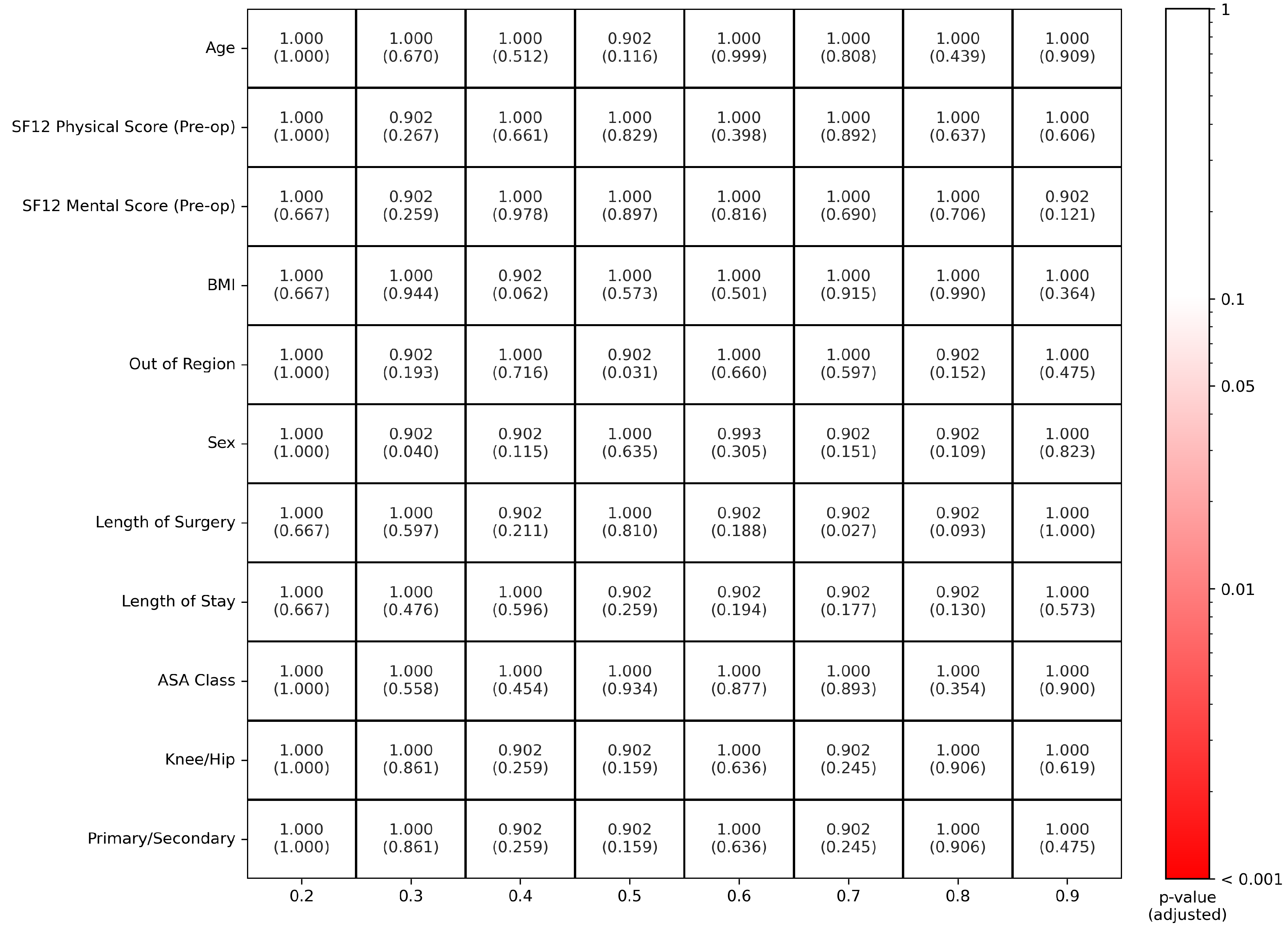
- In each decile of the distribution of propensity scores, the distribution of propensity scores for the Fast Track and Care-as-Usual populations should be the same;
- In each decile of the distribution of propensity scores, the distribution of each covariate in the Fast Track and Care-as-Usual populations should be the same;
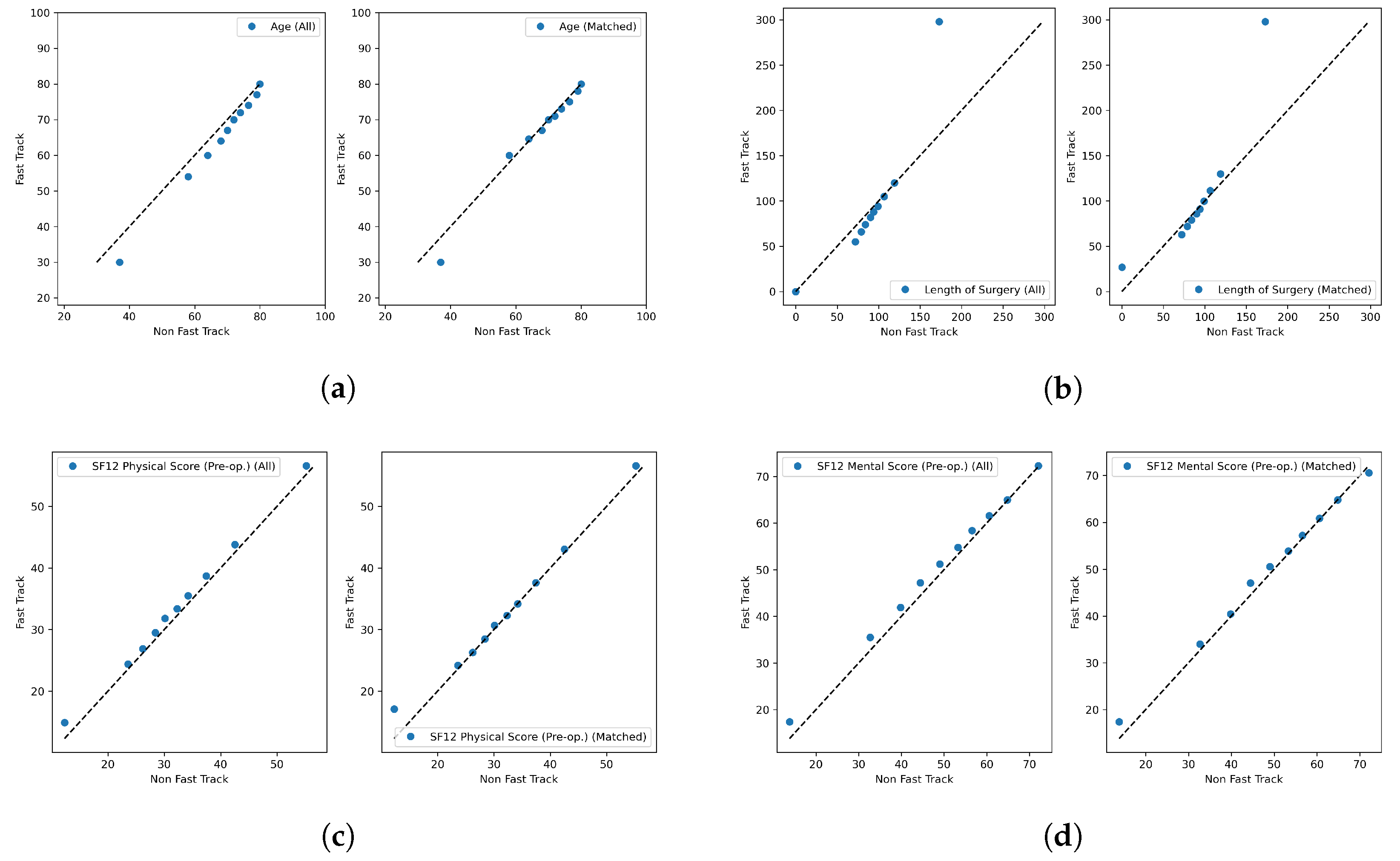
- Quantile–quantile plot qualitative analysis: for each of the corrected-for covariates, the post-match bi-variate distribution across Fast Track and Care-as-Usual patients should be closer to the diagional of the quantile–quantile plot than the same distribution for the pre-matched samples;
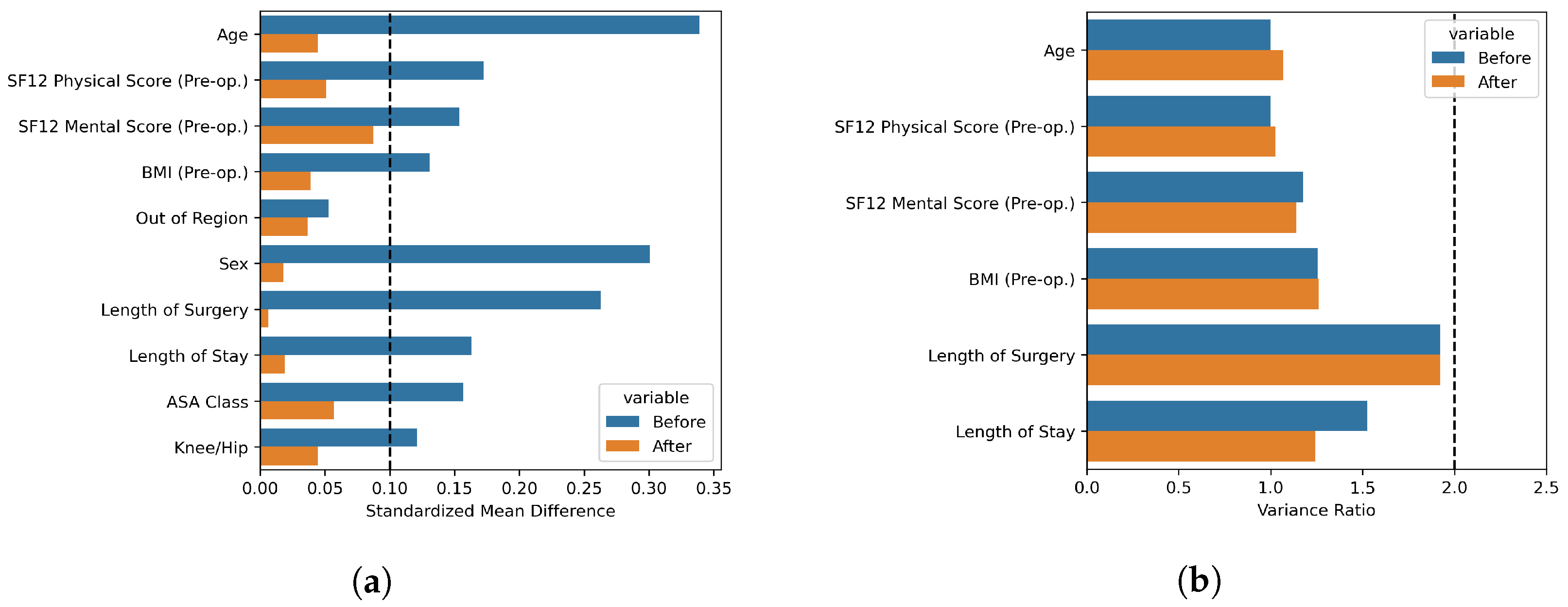
- Standardized mean differences (SMD) analysis: all corrected-for covariates should have a standardized mean difference smaller than 0.1 (which corresponds to a negligible effect size in the difference between the two populations [43])
- Variance ratio (VR) analysis: the ratio of the Fast Track and non-Fast Track sample variances should be smaller than 2.
2.3. Statistical Methods: Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petersen, P.B.; Kehlet, H.; Jørgensen, C.C. Improvement in fast-track hip and knee arthroplasty: A prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci. Rep. 2020, 10, 21233. [Google Scholar] [CrossRef] [PubMed]
- Drosos, G.I.; Kougioumtzis, I.E.; Tottas, S.; Ververidis, A.; Chatzipapas, C.; Tripsianis, G.; Tilkeridis, K. The results of a stepwise implementation of a fast-track program in total hip and knee replacement patients. J. Orthop. 2020, 21, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Romano, L.U.; Rigoni, M.; Torri, E.; Nella, M.; Morandi, M.; Casetti, P.; Nollo, G. A propensity score-matched analysis to assess the outcomes in pre-and post-fast-track hip and knee elective prosthesis patients. J. Clin. Med. 2021, 10, 741. [Google Scholar] [CrossRef]
- Rocchi, M.; Stagni, C.; Govoni, M.; Mazzotta, A.; Vivarelli, L.; Orlandi Magli, A.; Perrone, M.; Benedetti, M.G.; Dallari, D. Comparison of a fast track protocol and standard care after hip arthroplasty in the reduction of the length of stay and the early weight-bearing resumption: Study protocol for a randomized controlled trial. Trials 2021, 22, 1–13. [Google Scholar] [CrossRef]
- Elmoghazy, A.D.; Lindner, N.; Tingart, M.; Salem, K.H. Conventional versus fast track rehabilitation after total hip replacement: A randomized controlled trial. J. Orthop. Trauma Rehabil. 2022, 29, 22104917221076501. [Google Scholar] [CrossRef]
- Riemer, B.; MacIntyre, K.; Nortje, M.; Dower, B.; Grobler, G.; Springfield, M. Rapid mobilisation following total hip and knee arthroplasty. SA Orthop. J. 2017, 16, 58–61. [Google Scholar] [CrossRef] [Green Version]
- Berg, U.; Berg, M.; Rolfson, O.; Erichsen-Andersson, A. Fast-track program of elective joint replacement in hip and knee—patients’ experiences of the clinical pathway and care process. J. Orthop. Surg. Res. 2019, 14, 1–8. [Google Scholar] [CrossRef]
- Hansen, T.B. Fast track in hip arthroplasty. EFORT Open Rev. 2017, 2, 179. [Google Scholar] [CrossRef]
- Ansari, D.; Gianotti, L.; Schröder, J.; Andersson, R. Fast-track surgery: Procedure-specific aspects and future direction. Langenbeck’s Arch. Surg. 2013, 398, 29–37. [Google Scholar] [CrossRef]
- de Carvalho Almeida, R.F.; Serra, H.O.; de Oliveira, L.P. Fast-track versus conventional surgery in relation to time of hospital discharge following total hip arthroplasty: A single-center prospective study. J. Orthop. Surg. Res. 2021, 16, 1–7. [Google Scholar] [CrossRef]
- Kehlet, H. Fast-track hip and knee arthroplasty. Lancet 2013, 381, 1600–1602. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Kehlet, H. Fast-track hip and knee arthroplasty–have we reached the goal? Acta Orthop. 2019, 90, 3–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhong, M.; Liu, D.; Tang, H.; Zheng, Y.; Bai, Y.; Liang, Q.; Yang, X. Impacts of the perioperative fast track surgery concept on the physical and psychological rehabilitation of total hip arthroplasty: A prospective cohort study of 348 patients. Medicine 2021, 100, e26869. [Google Scholar] [CrossRef]
- Jørgensen, P.B.; Bogh, S.B.; Kierkegaard, S.; Sørensen, H.; Odgaard, A.; Søballe, K.; Mechlenburg, I. The efficacy of early initiated, supervised, progressive resistance training compared to unsupervised, home-based exercise after unicompartmental knee arthroplasty: A single-blinded randomized controlled trial. Clin. Rehabil. 2017, 31, 61–70. [Google Scholar] [CrossRef]
- De Berardinis, L.; Senarighi, M.; Ciccullo, C.; Forte, F.; Spezia, M.; Gigante, A.P. Fast-track surgery and telerehabilitation protocol in unicompartmental knee arthroplasty leads to superior outcomes when compared with the standard protocol: A propensity-matched pilot study. Knee Surg. Relat. Res. 2022, 34, 44. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 1997, 78, 606–617. [Google Scholar] [CrossRef]
- Hu, Q.; He, T.; Sun, Y.; Wang, F.; Wu, J. Effect of fast-track surgery on inflammatory response and immune function in patients with laparoscopic distal gastrectomy. Eur. Surg. 2019, 51, 254–260. [Google Scholar] [CrossRef]
- Feng, F.; Ji, G.; Li, J.P.; Li, X.H.; Shi, H.; Zhao, Z.W.; Wu, G.S.; Liu, X.N.; Zhao, Q.C. Fast-track surgery could improve postoperative recovery in radical total gastrectomy patients. World J. Gastroenterol. WJG 2013, 19, 3642. [Google Scholar] [CrossRef] [PubMed]
- Ni, C.; Yang, Y.; Chang, Y.; Cai, H.; Xu, B.; Yang, F.; Lau, W.; Wang, Z.; Zhou, W. Fast-track surgery improves postoperative recovery in patients undergoing partial hepatectomy for primary liver cancer: A prospective randomized controlled trial. Eur. J. Surg. Oncol. (EJSO) 2013, 39, 542–547. [Google Scholar] [CrossRef]
- Christelis, N.; Wallace, S.; Sage, C.E.; Babitu, U.; Liew, S.; Dugal, J.; Nyulasi, I.; Mutalima, N.; Tran, T.; Myles, P.S. An enhanced recovery after surgery program for hip and knee arthroplasty. Med. J. Aust. 2015, 202, 363–368. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.K.; Malviya, A.; Muller, S.D.; Carluke, I.; Partington, P.F.; Emmerson, K.P.; Reed, M.R. Reduced short-term complications and mortality following enhanced recovery primary hip and knee arthroplasty: Results from 6,000 consecutive procedures. Acta Orthop. 2014, 85, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Auyong, D.B.; Allen, C.J.; Pahang, J.A.; Clabeaux, J.J.; MacDonald, K.M.; Hanson, N.A. Reduced length of hospitalization in primary total knee arthroplasty patients using an updated enhanced recovery after orthopedic surgery (ERAS) pathway. J. Arthroplast. 2015, 30, 1705–1709. [Google Scholar] [CrossRef]
- Malviya, A.; Martin, K.; Harper, I.; Muller, S.D.; Emmerson, K.P.; Partington, P.F.; Reed, M.R. Enhanced recovery program for hip and knee replacement reduces death rate: A study of 4,500 consecutive primary hip and knee replacements. Acta Orthop. 2011, 82, 577–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castorina, S.; Guglielmino, C.; Castrogiovanni, P.; Szychlinska, M.A.; Ioppolo, F.; Massimino, P.; Leonardi, P.; Maci, C.; Iannuzzi, M.; Di Giunta, A.; et al. Clinical evidence of traditional vs fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. Muscles, Ligaments Tendons J. 2017, 7, 504. [Google Scholar] [CrossRef] [PubMed]
- Wilches, C.; Sulbaran, J.; Fernandez, J.; Gisbert, J.; Bausili, J.; Pelfort, X. Fast-track recovery technique applied to primary total hip and knee replacement surgery. Analysis of costs and complications. Rev. Espa Nola De Cirugía Ortopédica Y Traumatol. 2017, 61, 111–116. [Google Scholar] [CrossRef]
- Maempel, J.; Clement, N.; Ballantyne, J.; Dunstan, E. Enhanced recovery programmes after total hip arthroplasty can result in reduced length of hospital stay without compromising functional outcome. Bone Jt. J. 2016, 98, 475–482. [Google Scholar] [CrossRef]
- Bouman, A.I.; Hemmen, B.; Evers, S.M.; van de Meent, H.; Ambergen, T.; Vos, P.E.; Brink, P.R.; Seelen, H.A. Effects of an integrated ‘fast Track’ Rehabilitation Service for Multi-Trauma Patients: A non-randomized clinical trial in the Netherlands. PLoS ONE 2017, 12, e0170047. [Google Scholar] [CrossRef] [Green Version]
- Hoorntje, A.; Koenraadt, K.L.; Boevé, M.G.; van Geenen, R.C. Outpatient unicompartmental knee arthroplasty: Who is afraid of outpatient surgery? Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 759–766. [Google Scholar] [CrossRef] [Green Version]
- den Hertog, A.; Gliesche, K.; Timm, J.; Mühlbauer, B.; Zebrowski, S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: A randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch. Orthop. Trauma Surg. 2012, 132, 1153–1163. [Google Scholar] [CrossRef] [Green Version]
- Baumhauer, J.F.; Bozic, K.J. Value-based healthcare: Patient-reported outcomes in clinical decision making. Clin. Orthop. Relat. Res. 2016, 474, 1375–1378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damman, O.C.; Jani, A.; de Jong, B.A.; Becker, A.; Metz, M.J.; de Bruijne, M.C.; Timmermans, D.R.; Cornel, M.C.; Ubbink, D.T.; van der Steen, M.; et al. The use of PROMs and shared decision-making in medical encounters with patients: An opportunity to deliver value-based health care to patients. J. Eval. Clin. Pract. 2020, 26, 524–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Squitieri, L.; Bozic, K.J.; Pusic, A.L. The role of patient-reported outcome measures in value-based payment reform. Value Health 2017, 20, 834–836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heymans, M.J.; Kort, N.P.; Snoeker, B.A.; Schotanus, M.G. Impact of enhanced recovery pathways on safety and efficacy of hip and knee arthroplasty: A systematic review and meta-analysis. World J. Orthop. 2022, 13, 307. [Google Scholar] [CrossRef]
- Lovecchio, F.; Alvi, H.; Sahota, S.; Beal, M.; Manning, D. Is outpatient arthroplasty as safe as fast-track inpatient arthroplasty? A propensity score matched analysis. J. Arthroplast. 2016, 31, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [Green Version]
- Waal, J.M.V.D.; Terwee, C.B.; Windt, D.A.V.D.; Bouter, L.M.; Dekker, J. The impact of non-traumatic hip and knee disorders on health-related quality of life as measured with the SF-36 or SF-12. A systematic review. Qual. Life Res. 2005, 14, 1141–1155. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–55. [Google Scholar] [CrossRef]
- Kane, L.T.; Fang, T.; Galetta, M.S.; Goyal, D.K.; Nicholson, K.J.; Kepler, C.K.; Vaccaro, A.R.; Schroeder, G.D. Propensity score matching: A statistical method. Clin. Spine Surg. 2020, 33, 120–122. [Google Scholar] [CrossRef]
- Benedetto, U.; Head, S.J.; Angelini, G.D.; Blackstone, E.H. Statistical primer: Propensity score matching and its alternatives. Eur. J. Cardio-Thorac. Surg. 2018, 53, 1112–1117. [Google Scholar] [CrossRef] [Green Version]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [Green Version]
- Rosenbaum, P.R. Optimal matching for observational studies. J. Am. Stat. Assoc. 1989, 84, 1024–1032. [Google Scholar] [CrossRef]
- Zhang, Z.; Kim, H.J.; Lonjon, G.; Zhu, Y.; written on behalf of AME Big-Data Clinical Trial Collaborative Group. Balance diagnostics after propensity score matching. Ann. Transl. Med. 2019, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 26. [Google Scholar] [CrossRef]
- Milella, F.; Famiglini, L.; Banfi, G.; Cabitza, F. Application of Machine Learning to Improve Appropriateness of Treatment in an Orthopaedic Setting of Personalized Medicine. J. Pers. Med. 2022, 12, 1706. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.A.; Leucht, S. How to obtain NNT from Cohen’s d: Comparison of two methods. PLoS ONE 2011, 6, e19070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huo, T.; Guo, Y.; Shenkman, E.; Muller, K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: A report from the wellness incentive and navigation (WIN) study. Health Qual. Life Outcomes 2018, 16, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Wijnen, B.F.; Hemmen, B.; Bouman, A.I.; van de Meent, H.; Ambergen, T.; Brink, P.R.; Seelen, H.A.; Evers, S.M. Cost-effectiveness of an integrated ’fast track’ rehabilitation service for multi-trauma patients: A non-randomized clinical trial in the Netherlands. PLoS ONE 2019, 14, e0213980. [Google Scholar] [CrossRef] [Green Version]
- Malec, J.F.; Ketchum, J.M. A standard method for determining the minimal clinically important difference for rehabilitation measures. Arch. Phys. Med. Rehabil. 2020, 101, 1090–1094. [Google Scholar] [CrossRef] [PubMed]
- Tille, E.; Beyer, F.; Auerbach, K.; Tinius, M.; Lützner, J. Better short-term function after unicompartmental compared to total knee arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 1–9. [Google Scholar] [CrossRef]
| Feature | Mean | Std. Dev. | Missing Rate |
|---|---|---|---|
| Age (years) | 68.72 | 10.96 | 0.00 |
| SF12 Physical Score (Pre-op) | 32.10 | 7.70 | 0.00 |
| SF12 Mental Score (Pre-op) | 49.69 | 12.54 | 0.00 |
| BMI | 27.39 | 4.73 | 0.01 |
| SF12 Physical Score (3 months) | 42.07 | 9.32 | 0.00 |
| SF12 Mental Score (3 months) | 52.56 | 10.71 | 0.00 |
| Length of Surgery (minutes) | 93.98 | 34.48 | 0.02 |
| Length of Stay (days) | 4.01 | 1.95 | 0.02 |
| Feature | Categories | Missing Rate | |
| Fast Track | Yes (66%), No (34%) | 0.00 | |
| Out of Region | Yes (18%), No (82%) | 0.00 | |
| Sex | Male (59%), Female (41%) | 0.00 | |
| ASA Class | 1 (11%), 2 (82%), 3 (7%) | 0.00 | |
| Knee/Hip | Knee (55%), Hip (45%) | 0.00 | |
| Primary/Secondary | Primary (84%), Secondary (16%) | 0.00 | |
| First intervention/Revision | First intervention (91%), Revision (9%) | 0.00 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campagner, A.; Milella, F.; Guida, S.; Bernareggi, S.; Banfi, G.; Cabitza, F. Assessment of Fast-Track Pathway in Hip and Knee Replacement Surgery by Propensity Score Matching on Patient-Reported Outcomes. Diagnostics 2023, 13, 1189. https://doi.org/10.3390/diagnostics13061189
Campagner A, Milella F, Guida S, Bernareggi S, Banfi G, Cabitza F. Assessment of Fast-Track Pathway in Hip and Knee Replacement Surgery by Propensity Score Matching on Patient-Reported Outcomes. Diagnostics. 2023; 13(6):1189. https://doi.org/10.3390/diagnostics13061189
Chicago/Turabian StyleCampagner, Andrea, Frida Milella, Stefania Guida, Susan Bernareggi, Giuseppe Banfi, and Federico Cabitza. 2023. "Assessment of Fast-Track Pathway in Hip and Knee Replacement Surgery by Propensity Score Matching on Patient-Reported Outcomes" Diagnostics 13, no. 6: 1189. https://doi.org/10.3390/diagnostics13061189
APA StyleCampagner, A., Milella, F., Guida, S., Bernareggi, S., Banfi, G., & Cabitza, F. (2023). Assessment of Fast-Track Pathway in Hip and Knee Replacement Surgery by Propensity Score Matching on Patient-Reported Outcomes. Diagnostics, 13(6), 1189. https://doi.org/10.3390/diagnostics13061189








