Diagnostic Accuracy of 128-Slice Single-Source CT for the Detection of Dislocated Bucket Handle Meniscal Tears in the Setting of an Acute Knee Trauma—Correlation with MRI and Arthroscopy
Abstract
:1. Introduction
2. Materials and Methods
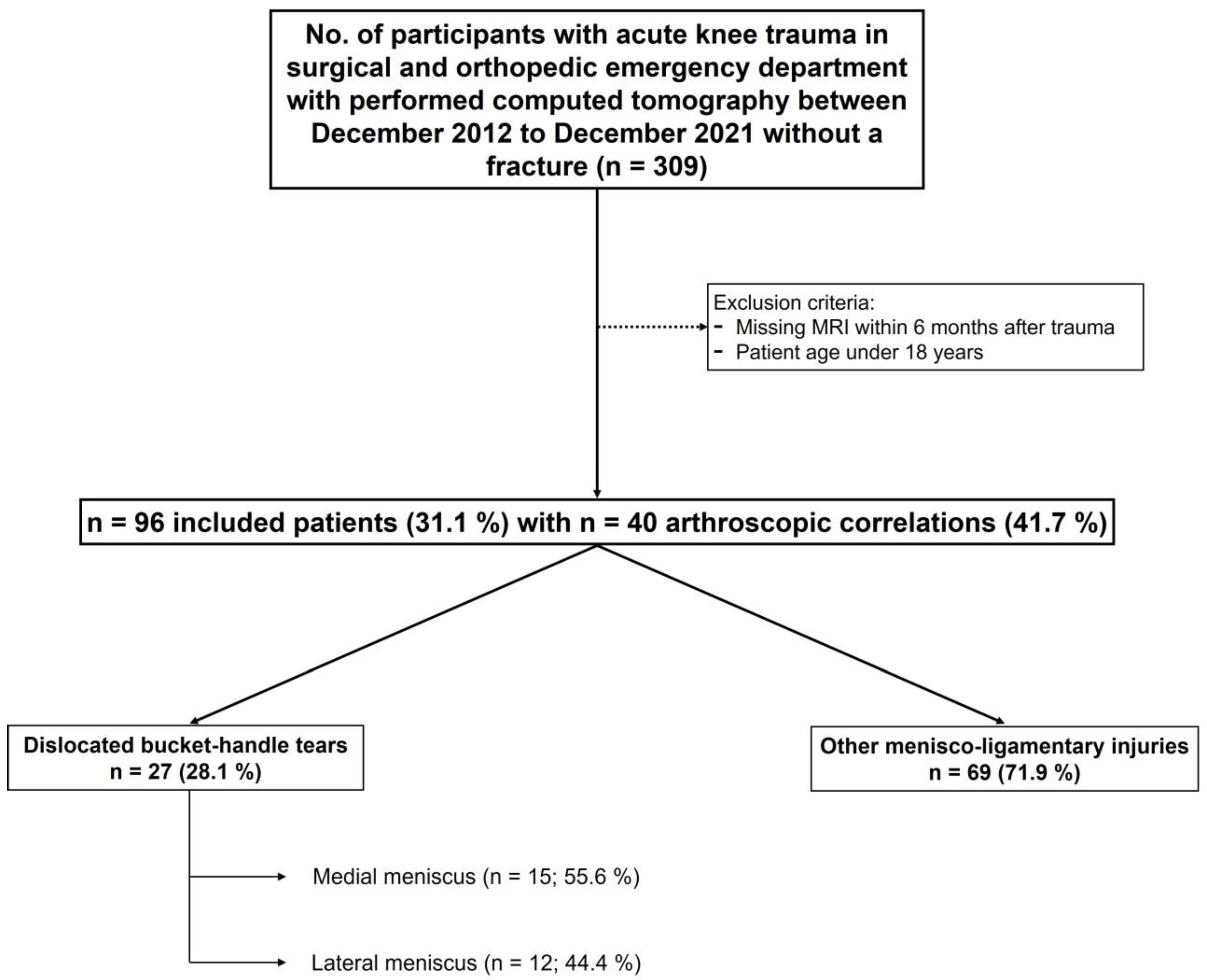
2.1. Study Population
2.2. Image Acquisition
2.3. Image Analysis
- Presence or absence (yes/no) of mentioned radiological signs of dislocated bucket handle meniscal tears (double delta sign, disproportional posterior horn sign, double PCL sign)
- Presence or absence (yes/no) of joint effusion
- Diagnostic confidence on a 5-point Likert scale [16]: 1 = “non-diagnostic imaging quality”, 2 = “slightly confident”, 3 = “fairly confident”, 4 = “confident”, and 5 = “very confident”.
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Diagnostic Performance of CT Regarding Dislocated Bucket Handle Meniscal Tears
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Logerstedt, D.S.; Scalzitti, D.A.; Bennell, K.L.; Hinman, R.S.; Silvers-Granelli, H.; Ebert, J.; Hambly, K.; Carey, J.L.; Snyder-Mackler, L.; Axe, M.J.; et al. Knee Pain and Mobility Impairments: Meniscal and Articular Cartilage Lesions Revision 2018. J. Orthop. Sports Phys. Ther. 2018, 48, A1–A50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, D.H.; de Smet, A.A.; Norris, M. Bucket-handle tears of the medial and lateral menisci of the knee: Value of MR imaging in detecting displaced fragments. AJR Am. J. Roentgenol. 1995, 165, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Ververidis, A.N.; Verettas, D.A.; Kazakos, K.J.; Tilkeridis, C.E.; Chatzipapas, C.N. Meniscal bucket handle tears: A retrospective study of arthroscopy and the relation to MRI. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 343–349. [Google Scholar] [CrossRef]
- Schuster, P.; Schlumberger, M. Handlungsalgorithmus: Kniegelenksdistorsion. Knie J. 2020, 2, 140–142. [Google Scholar] [CrossRef]
- Lefevre, N.; Naouri, J.F.; Herman, S.; Gerometta, A.; Klouche, S.; Bohu, Y. A Current Review of the Meniscus Imaging: Proposition of a Useful Tool for Its Radiologic Analysis. Radiol. Res. Pract. 2016, 2016, 8329296. [Google Scholar] [CrossRef] [Green Version]
- Booij, R.; Budde, R.P.J.; Dijkshoorn, M.L.; van Straten, M. Technological developments of X-ray computed tomography over half a century: User’s influence on protocol optimization. Eur. J. Radiol. 2020, 131, 109261. [Google Scholar] [CrossRef]
- Swamy, N.; Wadhwa, V.; Bajaj, G.; Chhabra, A.; Pandey, T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur. J. Radiol. 2018, 102, 115–124. [Google Scholar] [CrossRef]
- Bansal, S.; Floyd, E.R.; Kowalski, M.; Aikman, E.; Elrod, P.; Burkey, K.; Chahla, J.; LaPrade, R.F.; Maher, S.A.; Robinson, J.L.; et al. Meniscal repair: The current state and recent advances in augmentation. J. Orthop. Res. 2021, 39, 1368–1382. [Google Scholar] [CrossRef]
- Gardner, M.J.; Yacoubian, S.; Geller, D.; Suk, M.; Mintz, D.; Potter, H.; Helfet, D.L.; Lorich, D.G. The incidence of soft tissue injury in operative tibial plateau fractures: A magnetic resonance imaging analysis of 103 patients. J. Orthop. Trauma 2005, 19, 79–84. [Google Scholar] [CrossRef]
- Shiang, T.; Kotecha, H. CT diagnosis of bucket handle meniscus tear. Emerg. Radiol. 2020, 27, 451–453. [Google Scholar] [CrossRef]
- DeRamos, R.K. CT diagnosis of torn meniscus. Comput. Radiol. 1982, 6, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Manco, L.G.; Kavanaugh, J.H.; Fay, J.J.; Bilfield, B.S. Meniscus tears of the knee: Prospective evaluation with CT. Radiology 1986, 159, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Manco, L.G.; Berlow, M.E.; Czajka, J.; Alfred, R. Bucket-handle tears of the meniscus: Appearance at CT. Radiology 1988, 168, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Dorsay, T.A.; Helms, C.A. Bucket-handle meniscal tears of the knee: Sensitivity and specificity of MRI signs. Skelet. Radiol. 2003, 32, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Aydingöz, U.; Firat, A.K.; Atay, O.A.; Doral, M.N. MR imaging of meniscal bucket-handle tears: A review of signs and their relation to arthroscopic classification. Eur. Radiol. 2003, 13, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.; Kale, S.; Chandel, S.; Pal, D. Likert Scale: Explored and Explained. BJAST 2015, 7, 396–403. [Google Scholar] [CrossRef]
- Kundel, H.L.; Polansky, M. Measurement of observer agreement. Radiology 2003, 228, 303–308. [Google Scholar] [CrossRef]
- Khamis, M.E. Value of magnetic resonance imaging signs in diagnosis of bucket handle tear. Egypt. J. Radiol. Nucl. Med. 2016, 47, 1493–1500. [Google Scholar] [CrossRef] [Green Version]
- Magee, T.H.; Hinson, G.W. MRI of meniscal bucket-handle tears. Skelet. Radiol. 1998, 27, 495–499. [Google Scholar] [CrossRef]
- Mui, L.W.; Engelsohn, E.; Umans, H. Comparison of CT and MRI in patients with tibial plateau fracture: Can CT findings predict ligament tear or meniscal injury? Skelet. Radiol. 2007, 36, 145–151. [Google Scholar] [CrossRef]
- Chang, H.; Zheng, Z.; Shao, D.; Yu, Y.; Hou, Z.; Zhang, Y. Incidence and Radiological Predictors of Concomitant Meniscal and Cruciate Ligament Injuries in Operative Tibial Plateau Fractures: A Prospective Diagnostic Study. Sci. Rep. 2018, 8, 13317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helms, C.A.; Laorr, A.; Cannon, W.D. The absent bow tie sign in bucket-handle tears of the menisci in the knee. AJR Am. J. Roentgenol. 1998, 170, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Singson, R.D.; Feldman, F.; Staron, R.; Kiernan, H. MR imaging of displaced bucket-handle tear of the medial meniscus. AJR Am. J. Roentgenol. 1991, 156, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.L.; Morehouse, H.T.; Levy, I.M. Sagittal MR images of the knee: A low-signal band parallel to the posterior cruciate ligament caused by a displaced bucket-handle tear. AJR Am. J. Roentgenol. 1991, 156, 117–119. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.C.; Hsu, C.Y.; Shih, T.T.; Huang, K.M.; Li, Y.W. MR imaging of displaced meniscal tears of the knee. Importance of a “disproportional posterior horn sign”. Acta Radiol. 2001, 42, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Vande Berg, B.C.; Malghem, J.; Poilvache, P.; Maldague, B.; Lecouvet, F.E. Meniscal tears with fragments displaced in notch and recesses of knee: MR imaging with arthroscopic comparison. Radiology 2005, 234, 842–850. [Google Scholar] [CrossRef]
- Khil, E.K.; Choi, J.-A.; Hwang, E.; Sidek, S.; Choi, I. Paraspinal back muscles in asymptomatic volunteers: Quantitative and qualitative analysis using computed tomography (CT) and magnetic resonance imaging (MRI). BMC Musculoskelet. Disord. 2020, 21, 403. [Google Scholar] [CrossRef]
- Wang, F.-Z.; Sun, H.; Zhou, J.; Sun, L.-L.; Pan, S.-N. Reliability and Validity of Abdominal Skeletal Muscle Area Measurement Using Magnetic Resonance Imaging. Acad. Radiol. 2021, 28, 1692–1698. [Google Scholar] [CrossRef]
- Kim, J.-H.; van Rijn, R.M.; van Tulder, M.W.; Koes, B.W.; de Boer, M.R.; Ginai, A.Z.; Ostelo, R.W.G.J.; van der Windt, D.A.M.W.; Verhagen, A.P. Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; a systematic review. Chiropr. Man. Therap. 2018, 26, 37. [Google Scholar] [CrossRef] [Green Version]
- Naraghi, A.M.; White, L.M. Imaging of Athletic Injuries of Knee Ligaments and Menisci: Sports Imaging Series. Radiology 2016, 281, 23–40. [Google Scholar] [CrossRef] [Green Version]
- Fritz, B.; Yi, P.H.; Kijowski, R.; Fritz, J. Radiomics and Deep Learning for Disease Detection in Musculoskeletal Radiology: An Overview of Novel MRI- and CT-Based Approaches. Investig. Radiol. 2023, 58, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Bonaldi, L.; Pretto, A.; Pirri, C.; Uccheddu, F.; Fontanella, C.G.; Stecco, C. Deep Learning-Based Medical Images Segmentation of Musculoskeletal Anatomical Structures: A Survey of Bottlenecks and Strategies. Bioengineering 2023, 10, 137. [Google Scholar] [CrossRef] [PubMed]
- Norman, B.; Pedoia, V.; Majumdar, S. Use of 2D U-Net Convolutional Neural Networks for Automated Cartilage and Meniscus Segmentation of Knee MR Imaging Data to Determine Relaxometry and Morphometry. Radiology 2018, 288, 177–185. [Google Scholar] [CrossRef] [Green Version]
- Xue, Y.-P.; Jang, H.; Byra, M.; Cai, Z.-Y.; Wu, M.; Chang, E.Y.; Ma, Y.-J.; Du, J. Automated cartilage segmentation and quantification using 3D ultrashort echo time (UTE) cones MR imaging with deep convolutional neural networks. Eur. Radiol. 2021, 31, 7653–7663. [Google Scholar] [CrossRef] [PubMed]
- Hemke, R.; Buckless, C.G.; Tsao, A.; Wang, B.; Torriani, M. Deep learning for automated segmentation of pelvic muscles, fat, and bone from CT studies for body composition assessment. Skelet. Radiol. 2020, 49, 387–395. [Google Scholar] [CrossRef]
- Kamiya, N. Deep Learning Technique for Musculoskeletal Analysis. Adv. Exp. Med. Biol. 2020, 1213, 165–176. [Google Scholar] [CrossRef]
- Nishii, T.; Kobayashi, T.; Tanaka, H.; Kotoku, A.; Ohta, Y.; Morita, Y.; Umehara, K.; Ota, J.; Horinouchi, H.; Ishida, T.; et al. Deep Learning-based Post Hoc CT Denoising for Myocardial Delayed Enhancement. Radiology 2022, 305, 82–91. [Google Scholar] [CrossRef]
- Rao, N.; Patel, Y.; Opsha, O.; Chen, Q.; Owen, J.; Eisemon, E.; Fogel, J.; Beltran, J. Use of the V-sign in the diagnosis of bucket-handle meniscal tear of the knee. Skelet. Radiol. 2012, 41, 293–297. [Google Scholar] [CrossRef]
- Zanetti, M.; Pfirrmann, C.W.A.; Schmid, M.R.; Romero, J.; Seifert, B.; Hodler, J. Patients with suspected meniscal tears: Prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am. J. Roentgenol. 2003, 181, 635–641. [Google Scholar] [CrossRef]
- de Smet, A.A.; Norris, M.A.; Yandow, D.R.; Quintana, F.A.; Graf, B.K.; Keene, J.S. MR diagnosis of meniscal tears of the knee: Importance of high signal in the meniscus that extends to the surface. AJR Am. J. Roentgenol. 1993, 161, 101–107. [Google Scholar] [CrossRef] [Green Version]
- Stoller, D.W.; Martin, C.; Crues, J.V.; Kaplan, L.; Mink, J.H. Meniscal tears: Pathologic correlation with MR imaging. Radiology 1987, 163, 731–735. [Google Scholar] [CrossRef] [PubMed]



| Diagnostic Performance in CT | |||||
|---|---|---|---|---|---|
| Parameters | CT Images with Bone Kernel Reconstructions (n = 96) | CT Images with Soft-Tissue Kernel Reconstructions (n = 45) | |||
| Reader 1 | Reader 2 | Reader 1 | Reader 2 | ||
| Diagnostic confidence 5-point Likert scale | 1 (n) | 8 | 5 | 0 | 0 |
| 2 (n) | 36 | 32 | 4 | 2 | |
| 3 (n) | 19 | 23 | 11 | 12 | |
| 4 (n) | 27 | 31 | 21 | 24 | |
| 5 (n) | 6 | 5 | 9 | 7 | |
| Sensitivity % | 88.9 | 92.6 | 94.7 | 94.7 | |
| Specificity % | 100 | 98.6 | 100 | 100 | |
| Accuracy % | 96.9 | 96.9 | 97.8 | 97.8 | |
| PPV % | 100 | 96.2 | 100 | 100 | |
| NPV % | 95.8 | 97.1 | 96.3 | 96.3 | |
| False positive (n) | 0 | 1 | 0 | 0 | |
| False negative (n) | 3 | 2 | 1 | 1 | |
| True positive (n) | 24 | 25 | 18 | 18 | |
| True negative (n) | 69 | 68 | 26 | 26 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gohla, G.; Kraus, M.S.; Peyker, I.; Springer, F.; Keller, G. Diagnostic Accuracy of 128-Slice Single-Source CT for the Detection of Dislocated Bucket Handle Meniscal Tears in the Setting of an Acute Knee Trauma—Correlation with MRI and Arthroscopy. Diagnostics 2023, 13, 1295. https://doi.org/10.3390/diagnostics13071295
Gohla G, Kraus MS, Peyker I, Springer F, Keller G. Diagnostic Accuracy of 128-Slice Single-Source CT for the Detection of Dislocated Bucket Handle Meniscal Tears in the Setting of an Acute Knee Trauma—Correlation with MRI and Arthroscopy. Diagnostics. 2023; 13(7):1295. https://doi.org/10.3390/diagnostics13071295
Chicago/Turabian StyleGohla, Georg, Mareen Sarah Kraus, Isabell Peyker, Fabian Springer, and Gabriel Keller. 2023. "Diagnostic Accuracy of 128-Slice Single-Source CT for the Detection of Dislocated Bucket Handle Meniscal Tears in the Setting of an Acute Knee Trauma—Correlation with MRI and Arthroscopy" Diagnostics 13, no. 7: 1295. https://doi.org/10.3390/diagnostics13071295
APA StyleGohla, G., Kraus, M. S., Peyker, I., Springer, F., & Keller, G. (2023). Diagnostic Accuracy of 128-Slice Single-Source CT for the Detection of Dislocated Bucket Handle Meniscal Tears in the Setting of an Acute Knee Trauma—Correlation with MRI and Arthroscopy. Diagnostics, 13(7), 1295. https://doi.org/10.3390/diagnostics13071295





