Abstract
A 17-year-old female presented to the emergency room with an arrow sticking out the right aspect of her neck. Her vital signs were stable with systolic blood pressure of 117 mmHg, without either tachycardia, dyspnea, or signs of active bleeding. She was fully conscious with intact sensory and motor function on all extremities. Computed Tomography (CT) showed that the tip of the arrowhead lodged at the transverse foramen of the third cervical vertebra. Digital subtraction angiography revealed that the arrowhead lies posterior to the right vertebral artery, narrowly missing it by about two millimeters. Emergency surgery was arranged in hybrid operating suite. An occlusion balloon catheter was introduced to right vertebral artery but not inflated prior to extracting the arrowhead. After extraction, oozing from the wound was noted. We then inflated the balloon while the neurosurgeon performed hemostasis with gauze compression and electrocoagulation probe. The right vertebral angiography after releasing of the balloon showed focal narrowing of the artery without contrast extravasation. The patient was discharged on the fifth hospital day, and no anticoagulant was prescribed due to lack of neurological deficit. Pre-surgical planning and partnership with the neurosurgeon lead to the optimal outcome for this case.

Figure 1.
Penetrating trauma with arrow at the right side of the patient’s neck (tail end of the arrow cut and removed).
Figure 1.
Penetrating trauma with arrow at the right side of the patient’s neck (tail end of the arrow cut and removed).

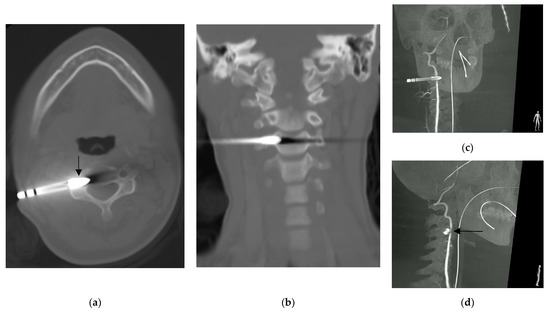
Figure 2.
Computed tomography showing: (a) the arrowhead (arrow) lodged at the transverse foramen of third cervical vertebra without violating the central canal, and; (b) the coronal reconstruction of the same scan showed that the arrowhead did not violate the neural foramen. Right vertebral artery angiography rotation view (c,d) showed narrowing of the right vertebral artery indented by the arrowhead (arrow) [1].
Figure 2.
Computed tomography showing: (a) the arrowhead (arrow) lodged at the transverse foramen of third cervical vertebra without violating the central canal, and; (b) the coronal reconstruction of the same scan showed that the arrowhead did not violate the neural foramen. Right vertebral artery angiography rotation view (c,d) showed narrowing of the right vertebral artery indented by the arrowhead (arrow) [1].
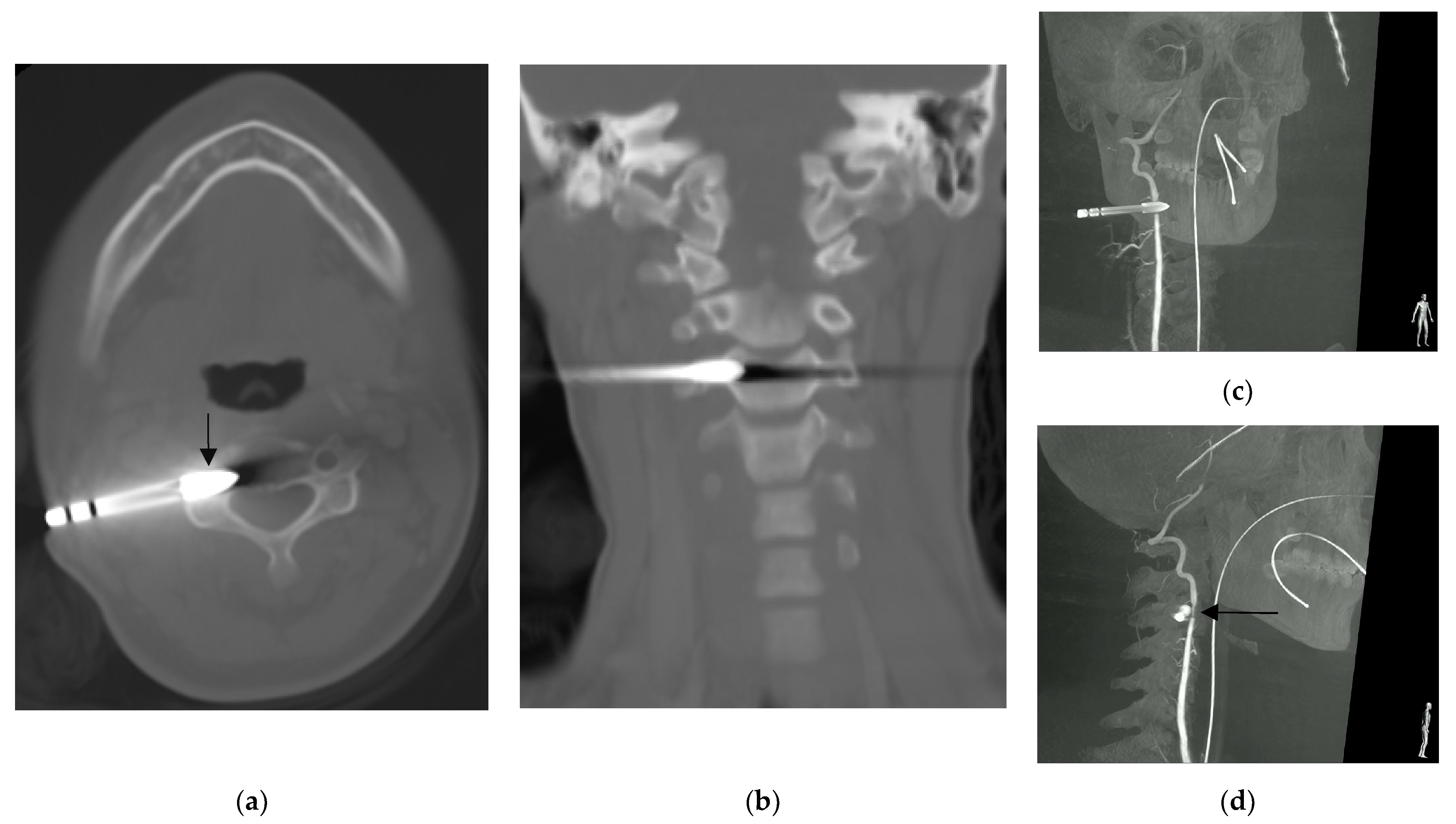
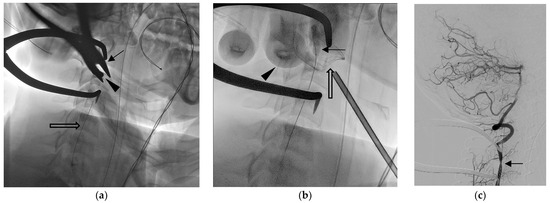
Figure 3.
Wound exploration was performed in hybrid operating suite [2]. Fluoroscope images showed the (a) surgical plier (arrow) grabbing the arrowhead (arrow), and the occlusion balloon catheter was deployed but not inflated (open arrow). After arrowhead extraction, oozing from the wound was noted. (b) The balloon was inflated (arrow) to decrease blood flow while the neurosurgeon applied direct compression (finger imaged, arrowhead) with gauze (open arrow) before performing a further hemostasis procedure. After that, the balloon was released. The following right vertebral angiography (c) shows focal narrowing of the artery lumen without extravasation. The patient reported no neurological deficit either when discharged or during their visit to the outpatient clinic 3 months later [3,4,5,6].
Figure 3.
Wound exploration was performed in hybrid operating suite [2]. Fluoroscope images showed the (a) surgical plier (arrow) grabbing the arrowhead (arrow), and the occlusion balloon catheter was deployed but not inflated (open arrow). After arrowhead extraction, oozing from the wound was noted. (b) The balloon was inflated (arrow) to decrease blood flow while the neurosurgeon applied direct compression (finger imaged, arrowhead) with gauze (open arrow) before performing a further hemostasis procedure. After that, the balloon was released. The following right vertebral angiography (c) shows focal narrowing of the artery lumen without extravasation. The patient reported no neurological deficit either when discharged or during their visit to the outpatient clinic 3 months later [3,4,5,6].
Author Contributions
Conceptualization, S.-C.W. and C.-H.L.; data curation, W.T.L.; writing—original draft preparation, S.-C.W.; writing—review and editing, C.-H.L.; supervision, C.-H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This retrospective study was approved by the Joint Institutional Review Board of Taipei Medical University (TMU–JIRB) (Approval No. N202211024; Approved date: 6 March 2023). The study was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Written informed consent was waived due to the retrospective nature of this work.
Data Availability Statement
All data are available within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- AlBayar, A.; Sullivan, P.Z.; Blue, R.; Leonard, J.; Kung, D.K.; Ozturk, A.K.; Chen, H.I.; Schuster, J.M. Risk of Vertebral Artery Injury and Stroke Following Blunt and Penetrating Cervical Spine Trauma: A Retrospective Review of 729 Patients. World Neurosurg. 2019, 130, e672–e679. [Google Scholar] [CrossRef] [PubMed]
- Van Waes, O.J.; Cheriex, K.C.A.L.; Navsaria, P.H.; van Riet, P.A.; Nicol, A.J.; Vermeulen, J. Management of Penetrating Neck Injuries. Br. J. Surg. 2012, 99, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.A.; Vargas, S.A.; Dublin, A.B. Endovascular Treatment of Traumatic Injuries of the Vertebral Artery. Am. J. Neuroradiol. 2008, 29, 1585–1589. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.W.; Kim, Y.S.; Yoon, E.J.; Kang, H.G. Chronic Headache Attributed to Vertebrobasilar Insufficiency. Diagnostics 2022, 12, 2038. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Kelly, M.P.; Min, W.-K.; Rahman, R.K.; Riew, K.D. Surgical Treatment of C3 and C4 Cervical Radiculopathies. Spine 2013, 38, 112. [Google Scholar] [CrossRef] [PubMed]
- Bakalarz, M.; Rożniecki, J.J.; Stasiołek, M. Clinical Characteristics of Patients with Vertebral Artery Hypoplasia. Int. J. Environ. Res. Public Health 2022, 19, 9317. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
