Anatomical and Simulation Studies Based on Three-Dimensional-Computed Tomography Image Reconstruction of Femoral Offset
Abstract
1. Introduction
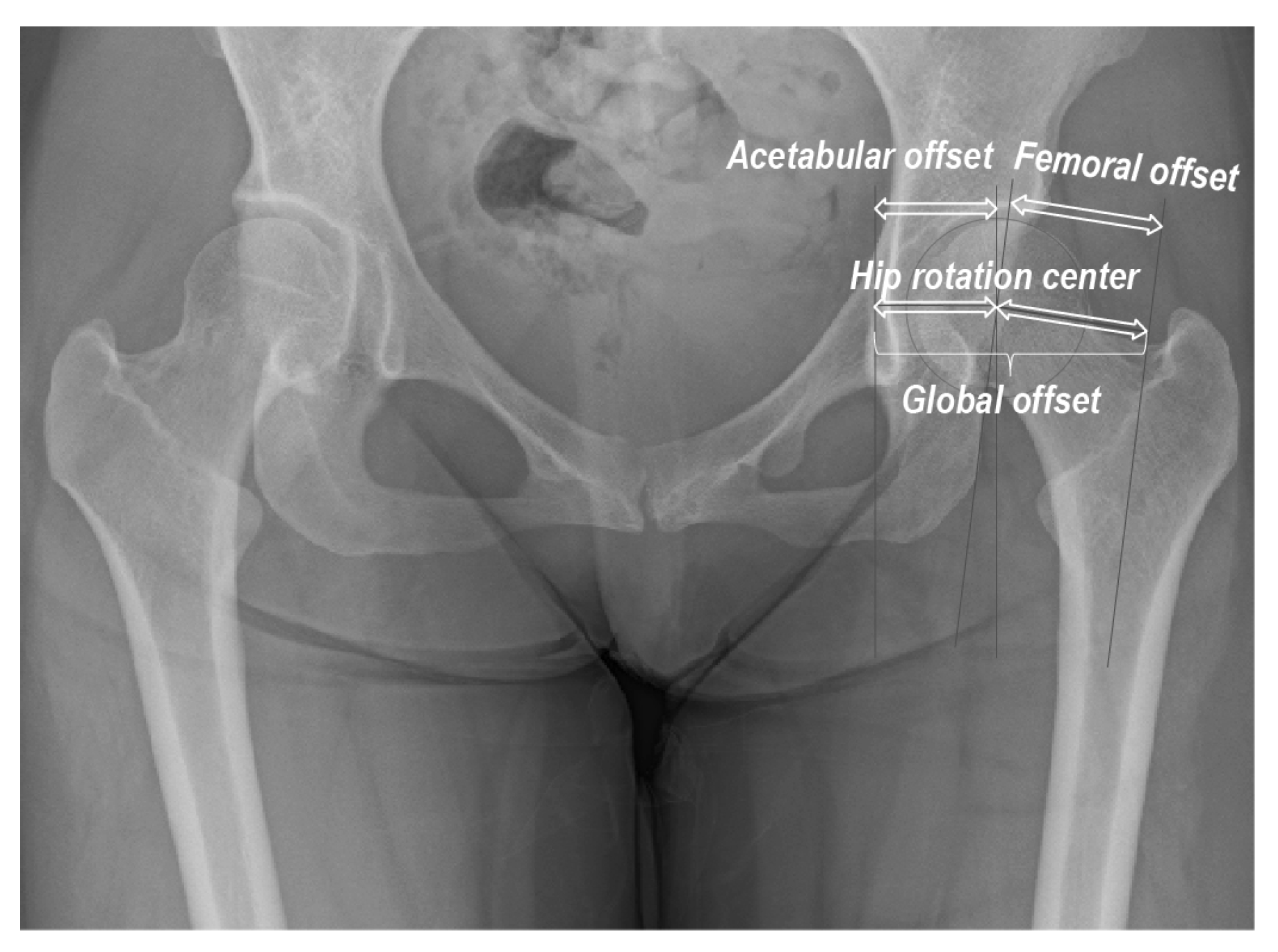
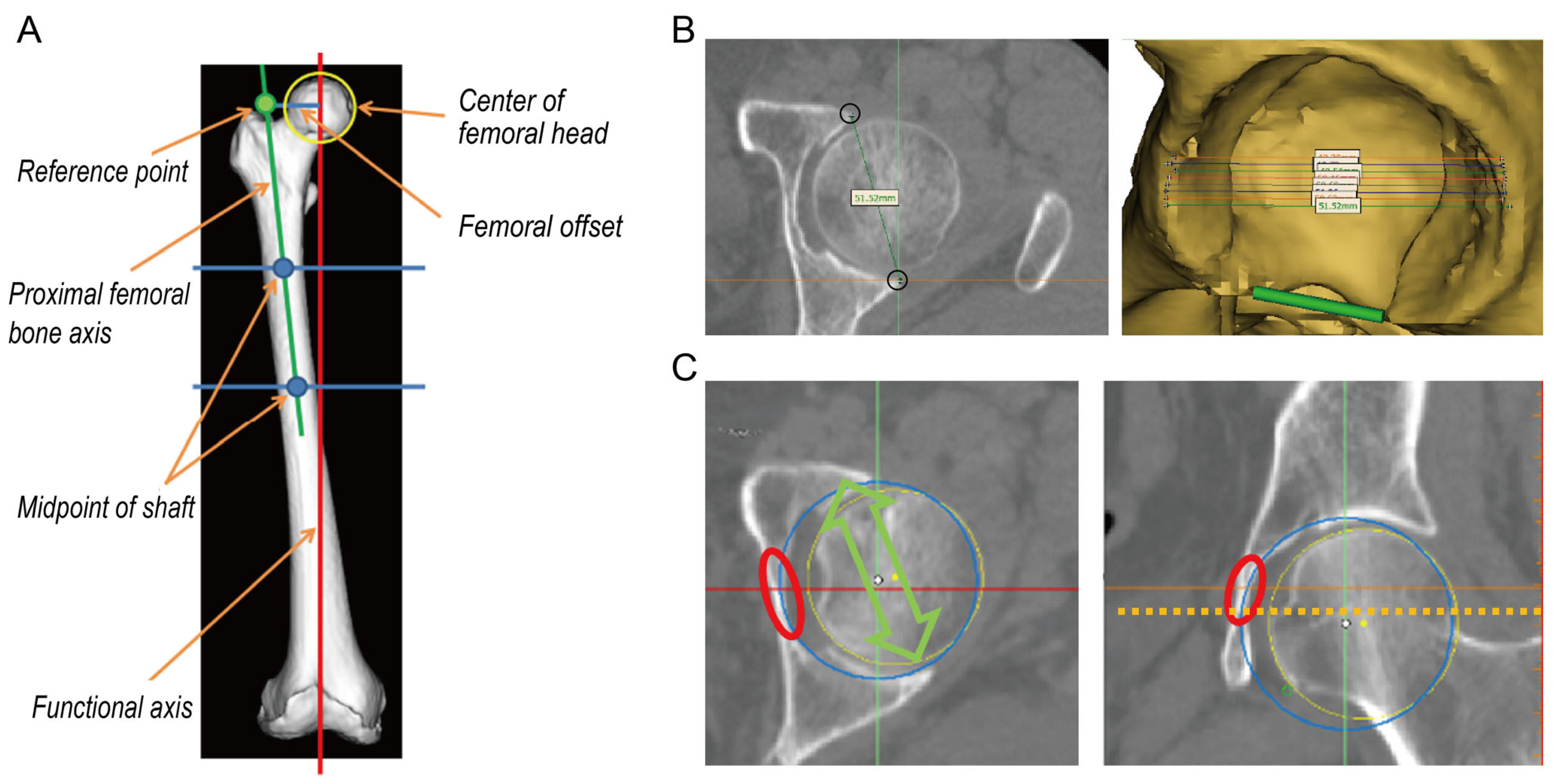
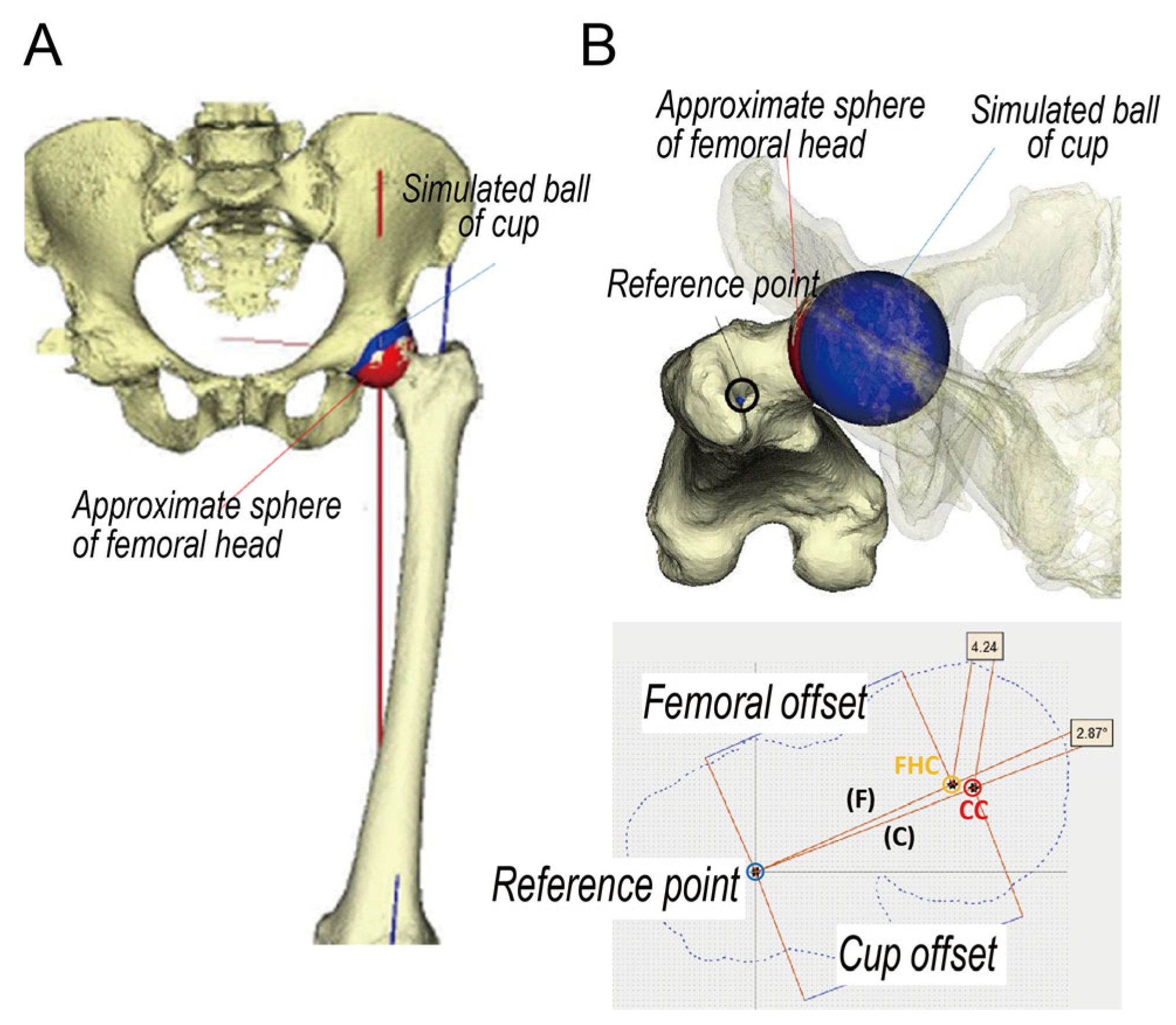
2. Materials and Methods
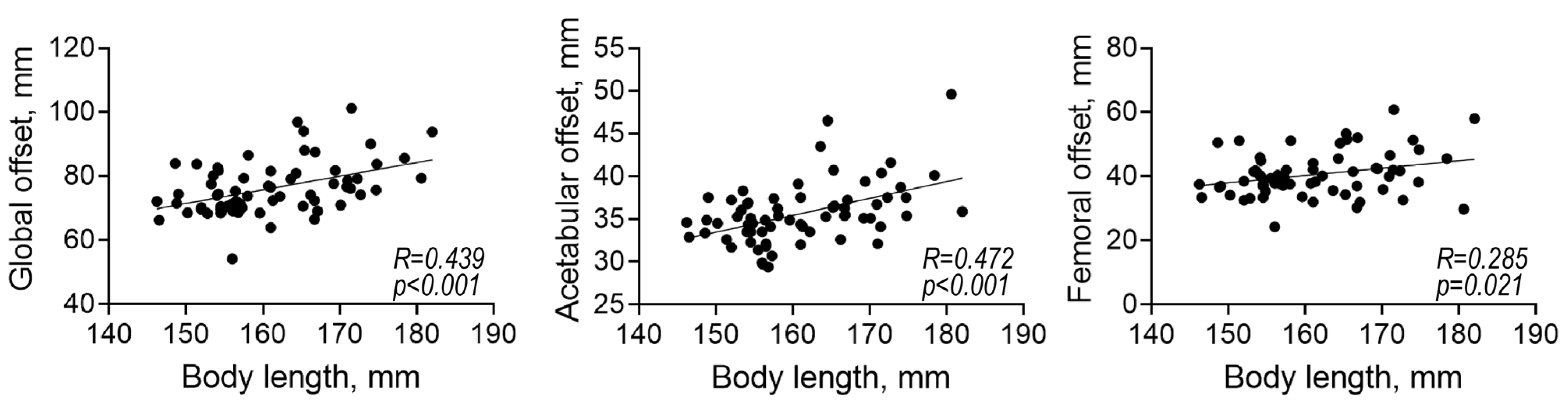
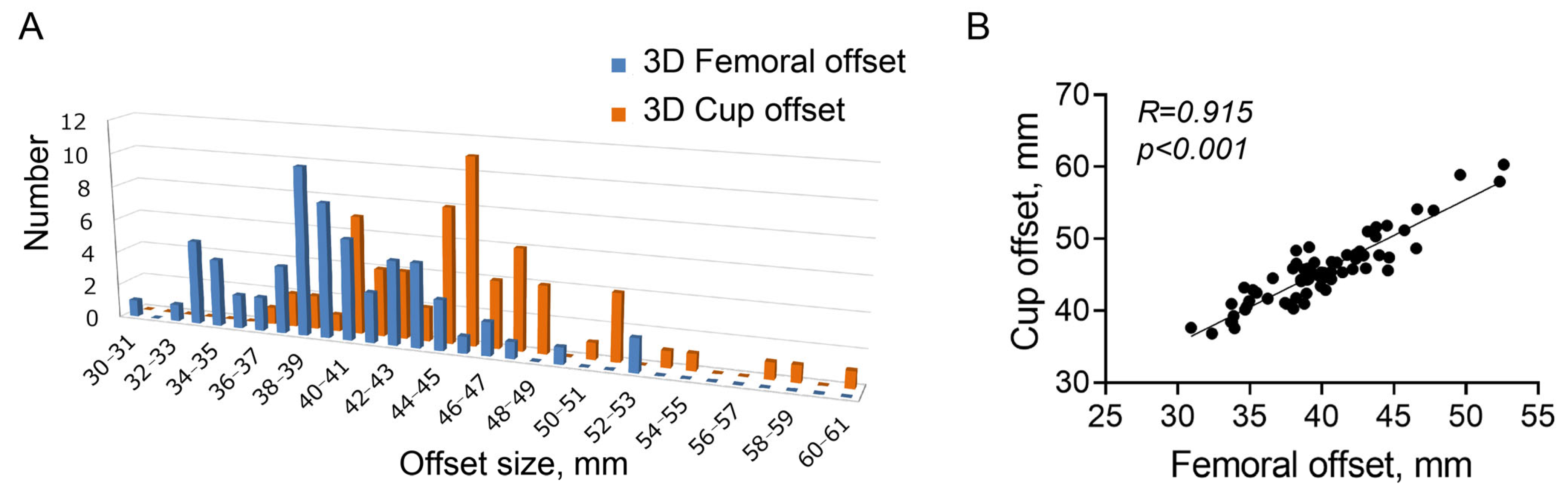
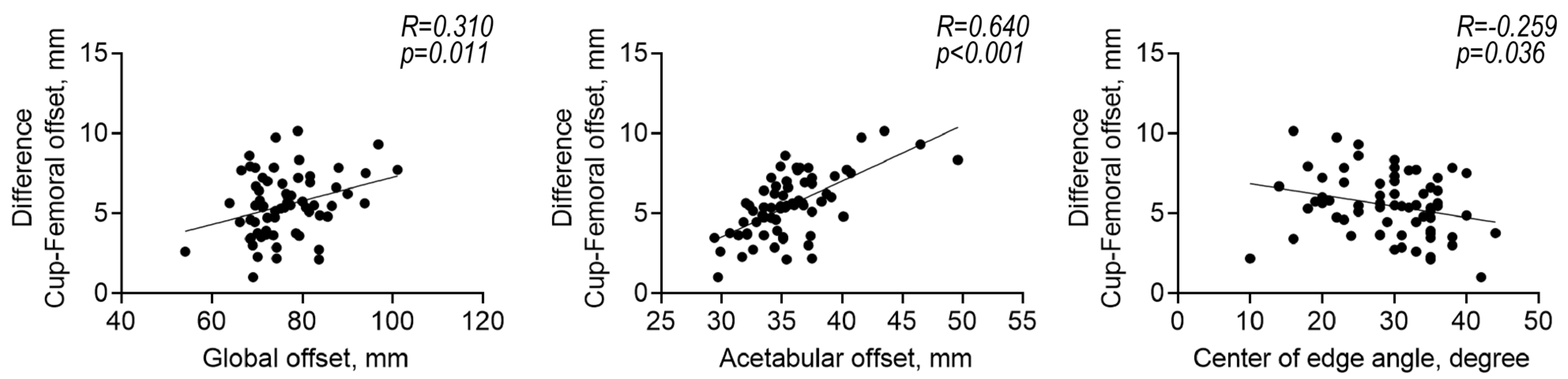
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Takao, M.; Nishii, T.; Sakai, T.; Sugano, N. Postoperative Limb-Offset Discrepancy Notably Affects Soft-Tissue Tension in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2016, 98, 1548–1554. [Google Scholar] [CrossRef]
- Komiyama, K.; Nakashima, Y.; Hirata, M.; Hara, D.; Kohno, Y.; Iwamoto, Y. Does High Hip Center Decrease Range of Motion in Total Hip Arthroplasty? A Computer Simulation Study. J. Arthroplast. 2016, 31, 2342–2347. [Google Scholar] [CrossRef]
- Sato, H.; Maezawa, K.; Gomi, M.; Kajihara, H.; Hayashi, A.; Maruyama, Y.; Nozawa, M.; Kaneko, K. Effect of Femoral Offset and Limb Length Discrepancy on Hip Joint Muscle Strength and Gait Trajectory after Total Hip Arthroplasty. Gait Posture 2020, 77, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Liebs, T.R.; Nasser, L.; Herzberg, W.; Rüther, W.; Hassenpflug, J. The Influence of Femoral Offset on Health-Related Quality of Life after Total Hip Replacement. Bone Jt. J. 2014, 96, 36–42. [Google Scholar] [CrossRef]
- Weber, M.; Merle, C.; Nawabi, D.H.; Dendorfer, S.; Grifka, J.; Renkawitz, T. Inaccurate Offset Restoration in Total Hip Arthroplasty Results in Reduced Range of Motion. Sci. Rep. 2020, 10, 13208. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Naito, M.; Asayama, I.; Ishiko, T. Total Hip Arthroplasty: The Relationship Between Posterolateral Reconstruction, Abductor Muscle Strength, and Femoral Offset. J. Orthop. Surg. 2004, 12, 164–167. [Google Scholar] [CrossRef]
- Mahmood, S.S.; Mukka, S.S.; Crnalic, S.; Wretenberg, P.; Sayed-Noor, A.S. Association Between Changes in Global Femoral Offset After Total Hip Arthroplasty and Function, Quality of Life, and Abductor Muscle Strength. A Prospective Cohort Study of 222 Patients. Acta Orthop. 2016, 87, 36–41. [Google Scholar] [CrossRef]
- Rüdiger, H.A.; Guillemin, M.; Latypova, A.; Terrier, A. Effect of Changes of Femoral Offset on Abductor and Joint Reaction Forces in Total Hip Arthroplasty. Arch. Orthop. Trauma Surg. 2017, 137, 1579–1585. [Google Scholar] [CrossRef]
- Tanzer, M.; Graves, S.E.; Peng, A.; Shimmin, A.J. Is Cemented or Cementless Femoral Stem Fixation More Durable in Patients Older Than 75 Years of Age? A Comparison of the Best-performing Stems. Clin. Orthop. Relat. Res. 2018, 476, 1428–1437. [Google Scholar] [CrossRef]
- Gwynne-Jones, D.P.; Gray, A.R. Cemented or Uncemented Acetabular Fixation in Combination with the Exeter Universal Cemented Stem. Bone Jt. J. 2020, 102, 414–422. [Google Scholar] [CrossRef]
- Halai, M.; Gupta, S.; Gilmour, A.; Bharadwaj, R.; Khan, A.; Holt, G. The Exeter Technique Can Lead to a Lower Incidence of Leg-Length Discrepancy After Total Hip Arthroplasty. Bone Jt. J. 2015, 97, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Dudda, M.; Kim, Y.J.; Zhang, Y.; Nevitt, M.C.; Xu, L.; Niu, J.; Goggins, J.; Doherty, M.; Felson, D.T. Morphologic Differences Between the Hips of Chinese Women and White Women: Could They Account for the Ethnic Difference in the Prevalence of Hip Osteoarthritis? Arthritis Rheum. 2011, 63, 2992–2999. [Google Scholar] [CrossRef]
- Yang, Z.; Jian, W.; Li, Z.H.; Jun, X.; Liang, Z.; Ge, Y.; Shi, Z.J. The Geometry of the Bone Structure Associated with Total Hip Arthroplasty. PLoS ONE 2014, 9, e91058. [Google Scholar] [CrossRef]
- Takamatsu, T.; Shishido, T.; Takahashi, Y.; Masaoka, T.; Tateiwa, T.; Kubo, K.; Endo, K.; Aoki, M.; Yamamoto, K. Radiographic Determination of Hip Rotation Center and Femoral Offset in Japanese Adults: A Preliminary Investigation Toward the Preoperative Implications in Total Hip Arthroplasty. Biomed. Res. Int. 2015, 2015, 610763. [Google Scholar] [CrossRef]
- Yin, Y.; Zhang, R.; Jin, L.; Li, S.; Hou, Z.; Zhang, Y. The Hip Morphology Changes with Ageing in Asian Population. Biomed. Res. Int. 2018, 2018, 1507979. [Google Scholar] [CrossRef]
- Hananouchi, T.; Sugano, N.; Nakamura, N.; Nishii, T.; Miki, H.; Yamamura, M.; Yoshikawa, H. Preoperative Templating of Femoral Components on Plain X-rays. Rotational Evaluation with Synthetic X-rays on ORTHODOC. Arch. Orthop. Trauma Surg. 2007, 127, 381–385. [Google Scholar] [CrossRef]
- Bjarnason, J.A.; Reikeras, O. Changes of Center of Rotation and Femoral Offset in Total Hip Arthroplasty. Ann. Transl. Med. 2015, 3, 355. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, G. Shelf Operation in Congenital Dysplasia of the Acetabulum and in Subluxation and Dislocation of the Hip. J. Bone Jt. Surg. Am. 1953, 35, 65–80. [Google Scholar] [CrossRef]
- Siebenrock, K.A.; Schoeniger, R.; Ganz, R. Anterior Femoro-Acetabular Impingement Due to Acetabular Retroversion. Treatment with Periacetabular Osteotomy. J. Bone Jt. Surg. Am. 2003, 85, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Flecher, X.; Ollivier, M.; Argenson, J.N. Lower Limb Length and Offset in Total Hip Arthroplasty. Orthop. Traumatol. Surg. Res. 2016, 102, S9–S20. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB Recommendation on Definitions of Joint Coordinate System of Various Joints for the Reporting of Human Joint Motion--Part I: Ankle, Hip, and Spine. International Society of Biomechanics. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Babisch, J.W.; Layher, F.; Amiot, L.P. The Rationale for Tilt-Adjusted Acetabular Cup Navigation. J. Bone Jt. Surg. Am. 2008, 90, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Majima, T.; Abe, S.; Nakamura, T.; Kanno, T.; Masuda, T.; Minami, A. Using the Transverse Acetabular Ligament as a Landmark for Acetabular Anteversion: An Intra-Operative Measurement. J. Orthop. Surg. 2013, 21, 189–194. [Google Scholar] [CrossRef]
- Evans, J.T.; Blom, A.W.; Timperley, A.J.; Dieppe, P.; Wilson, M.J.; Sayers, A.; Whitehouse, M.R. Factors Associated with Implant Survival Following Total Hip Replacement Surgery: A Registry Study of Data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man. PLoS Med. 2020, 17, e1003291. [Google Scholar] [CrossRef]
- Sariali, E.; Mouttet, A.; Pasquier, G.; Durante, E. Three-Dimensional Hip Anatomy in Osteoarthritis. Analysis of the Femoral Offset. J. Arthroplast. 2009, 24, 990–997. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral Offset: Anatomical Concept, Definition, Assessment, Implications for Preoperative Templating and Hip Arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef]
- Bonnin, M.P.; Archbold, P.H.; Basiglini, L.; Fessy, M.H.; Beverland, D.E. Do We Medialise the Hip Centre of Rotation in Total Hip Arthroplasty? Influence of Acetabular Offset and Surgical Technique. Hip Int. 2012, 22, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Buecking, B.; Boese, C.K.; Bergmeister, V.A.; Frink, M.; Ruchholtz, S.; Lechler, P. Functional Implications of Femoral Offset Following Hemiarthroplasty for Displaced Femoral Neck Fracture. Int. Orthop. 2016, 40, 1515–1521. [Google Scholar] [CrossRef]
- Chapman, R.M.; Van Citters, D.W.; Chapman, D.; Dalury, D.F. Higher Offset Cross-Linked Polyethylene Acetabular Liners: Is Wear A Significant Clinical Concern? Hip Int. 2019, 29, 652–659. [Google Scholar] [CrossRef]
- Meermans, G.; Doorn, J.V.; Kats, J.J. Restoration of the Centre of Rotation in Primary Total Hip Arthroplasty: The Influence of Acetabular Floor Depth and Reaming Technique. Bone Jt. J. 2016, 98, 1597–1603. [Google Scholar] [CrossRef] [PubMed]

| Men | Women | p-Value | |
|---|---|---|---|
| Number | 28 | 38 | |
| Age (year) | 52.5 (15.5) | 58.0 (15.7) | 0.159 |
| Body length (cm) | 169.4 (5.6) | 154.9 (4.0) | <0.001 |
| Body mass index (kg/m2) | 23.5 (3.2) | 23.6 (4.5) | 0.902 |
| Center of edge angle, (°) | 31.9 (5.3) | 28.1 (6.8) | 0.015 |
| Global offset (mm) | 80.9 (8.8) | 72.6 (5.9) | <0.001 |
| Acetabular offset (mm) | 37.7 (4.0) | 34.2 (2.4) | <0.001 |
| Femoral offset (mm) | 43.2 (8.3) | 38.4 (5.0) | 0.005 |
| Men | Women | p-Value | |
|---|---|---|---|
| Number | 28 | 38 | |
| Femoral offset, mm | 42.1 (4.8) | 38.4 (3.6) | <0.001 |
| Cup offset, mm | 48.4 (5.1) | 43.3 (3.4) | <0.001 |
| Cup-femoral offset, mm | 6.3 (1.9) | 4.9 (1.8) | 0.002 |
| Distance cup-head center, mm | 8.1 (3.0) | 7.2 (2.3) | 0.146 |
| Angle cup-head center, ° | 6.2 (4.3) | 7.1 (3.4) | 0.335 |
| Femoral anteversion, ° | 13.2 (9.6) | 21.2 (9.9) | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu, T.; Takahashi, D.; Ishizu, H.; Yokota, S.; Hasebe, Y.; Uetsuki, K.; Iwasaki, N. Anatomical and Simulation Studies Based on Three-Dimensional-Computed Tomography Image Reconstruction of Femoral Offset. Diagnostics 2023, 13, 1434. https://doi.org/10.3390/diagnostics13081434
Shimizu T, Takahashi D, Ishizu H, Yokota S, Hasebe Y, Uetsuki K, Iwasaki N. Anatomical and Simulation Studies Based on Three-Dimensional-Computed Tomography Image Reconstruction of Femoral Offset. Diagnostics. 2023; 13(8):1434. https://doi.org/10.3390/diagnostics13081434
Chicago/Turabian StyleShimizu, Tomohiro, Daisuke Takahashi, Hotaka Ishizu, Shunichi Yokota, Yoshihiro Hasebe, Keita Uetsuki, and Norimasa Iwasaki. 2023. "Anatomical and Simulation Studies Based on Three-Dimensional-Computed Tomography Image Reconstruction of Femoral Offset" Diagnostics 13, no. 8: 1434. https://doi.org/10.3390/diagnostics13081434
APA StyleShimizu, T., Takahashi, D., Ishizu, H., Yokota, S., Hasebe, Y., Uetsuki, K., & Iwasaki, N. (2023). Anatomical and Simulation Studies Based on Three-Dimensional-Computed Tomography Image Reconstruction of Femoral Offset. Diagnostics, 13(8), 1434. https://doi.org/10.3390/diagnostics13081434







