Post-Traumatic Cilia Remaining Inert in the Posterior Chamber for 50 Years
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gopal, L.; Banker, A.S.; Sharma, T.; Parikh, S.; Bhende, P.S.; Chopra, S. Intraocular cilia associated with perforating injury. Indian J. Ophthalmol. 2000, 48, 33–36. [Google Scholar] [PubMed]
- Dettoraki, M.; Andreanos, K.; Davou, S.; Nomikarios, N.; Moschos, M.M.; Brouzas, D. Intravitreal cilium associated with retinal detachment 40 years following penetrating eye injury: A case report. BMC Ophthalmol. 2015, 15, 25. [Google Scholar] [CrossRef] [PubMed]
- Humayun, M.; de la Cruz, Z.; Maguire, A.; Dangel, M.E.; Stark, W.J.; Green, W.R. Intraocular cilia. Report of six cases of 6 weeks’ to 32 years’ duration. Arch. Ophthalmol. 1993, 111, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Galloway, G.D.; Ang, G.S.; Shenoy, R.; Beigi, B. Retained anterior chamber cilium causing endophthalmitis after phacoemulsification. Cataract. Refract. Surg. 2004, 30, 521–522. [Google Scholar] [CrossRef]
- Ramos, G.Z.; Goncalves, T.B.; Bordon, A.F. An unusual case of nine cilia embedded in the retina after a perforating ocular injury. Am. J. Ophthalmol. Case Rep. 2020, 17, 100587. [Google Scholar] [CrossRef] [PubMed]
- Yalniz-Akkaya, Z. Post-traumatic cilia remaining inert in the anterior chamber for 50 years: A case report. J. Med. Case Rep. 2011, 5, 527. [Google Scholar] [CrossRef] [PubMed]
- Hoh, H.B.; Menage, M.J.; Dean-Hart, C. Iris cyst after traumatic implantation of an eyelash into the anterior chamber. Br. J. Ophthalmol. 1993, 77, 741–742. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.; Oh, K.; Singerman, L.J. An eyelash in the vitreous cavity without apparent etiology. Ophthalmic. Surg. Lasers 1996, 2, 243–245. [Google Scholar] [CrossRef]
- Kertes, P.J.; Al-Ghamdi, A.A.; Brownstein, S.; Coupal, D.; Gilberg, S.; Britton, W.A., Jr. An intraocular cilium of uncertain origin. Can. J. Ophthalmol. 2004, 39, 279–281. [Google Scholar] [CrossRef]
- Sahu, S.; Puri, L.R.; Singh, S.K. Intraocular eyelashes and iris cyst in anterior chamber following penetrating eye injury: A case report. Int. Med. Case Rep. J. 2017, 10, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Olorenshaw, G.M.; Brooks, A.M.; Grant, G.; Gillies, W.E. Tolerance of the eye for implanted cilia. Br. J. Ophthalmol. 1991, 75, 622–623. [Google Scholar] [CrossRef] [PubMed]
- Kargi, S.H.; Oz, O.; Erdinc, E.; Teke, M.Y.; Firat, E. Tolerated cilium in the anterior chamber. Ocul. Immunol. Inflamm. 2003, 11, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Higashide, T.; Sugiyama, K. Use of viscoelastic substance in ophthalmic surgery—Focus on sodium hyaluronate. Clin. Ophthalmol. 2008, 2, 21–30. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
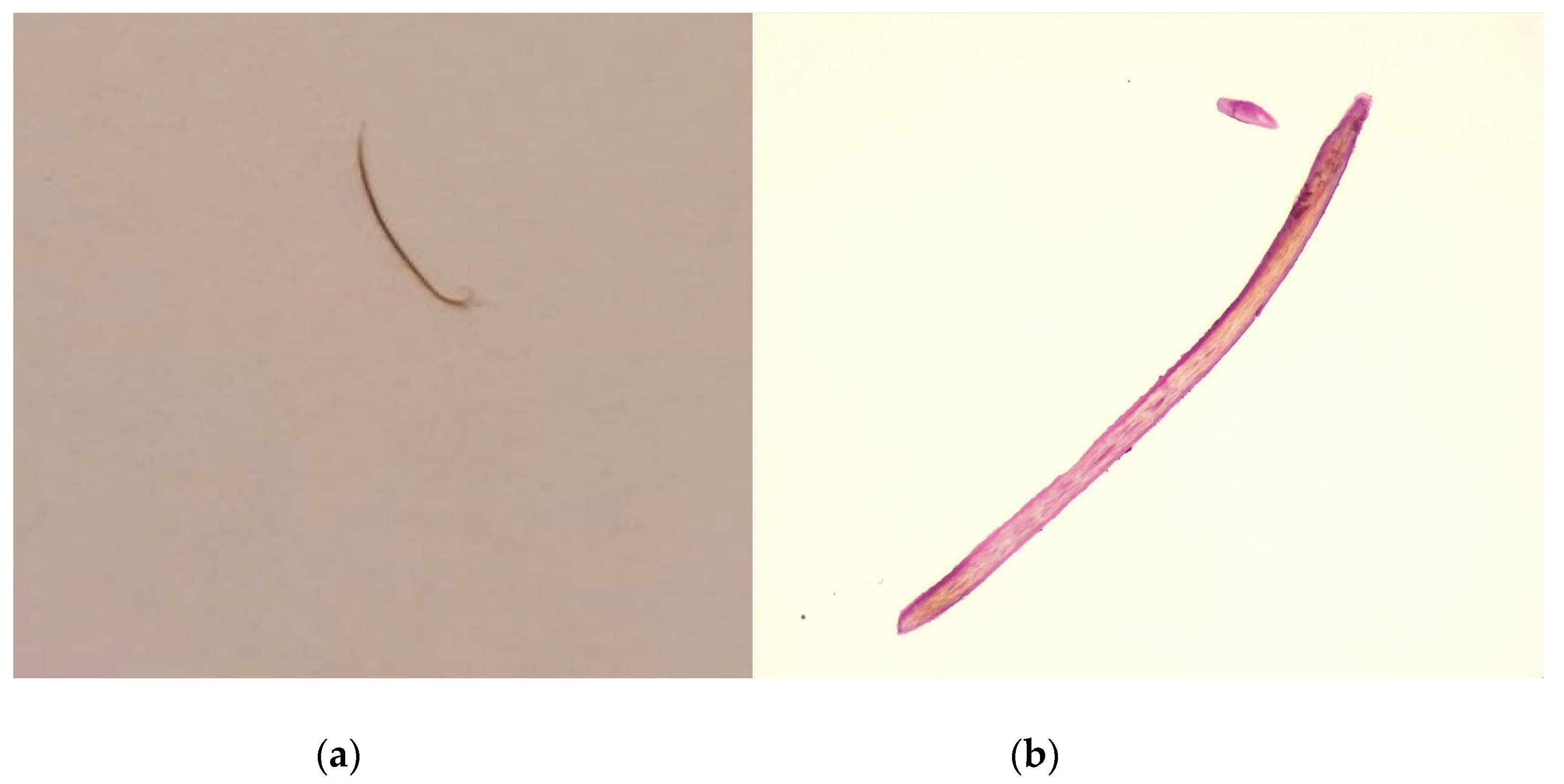
Teodoru, C.A.; Roman, M.D.; Hașegan, A.; Matei, C.; Mohor, C.; Munteanu, M.; Vică, M.L.; Matei, H.V.; Stanca, H.; Cerghedean-Florea, M.-E.; et al. Post-Traumatic Cilia Remaining Inert in the Posterior Chamber for 50 Years. Diagnostics 2023, 13, 1575. https://doi.org/10.3390/diagnostics13091575
Teodoru CA, Roman MD, Hașegan A, Matei C, Mohor C, Munteanu M, Vică ML, Matei HV, Stanca H, Cerghedean-Florea M-E, et al. Post-Traumatic Cilia Remaining Inert in the Posterior Chamber for 50 Years. Diagnostics. 2023; 13(9):1575. https://doi.org/10.3390/diagnostics13091575
Chicago/Turabian StyleTeodoru, Cosmin Adrian, Mihai Dan Roman, Adrian Hașegan, Claudiu Matei, Cosmin Mohor, Mihnea Munteanu, Mihaela Laura Vică, Horea Vladi Matei, Horia Stanca, Maria-Emilia Cerghedean-Florea, and et al. 2023. "Post-Traumatic Cilia Remaining Inert in the Posterior Chamber for 50 Years" Diagnostics 13, no. 9: 1575. https://doi.org/10.3390/diagnostics13091575
APA StyleTeodoru, C. A., Roman, M. D., Hașegan, A., Matei, C., Mohor, C., Munteanu, M., Vică, M. L., Matei, H. V., Stanca, H., Cerghedean-Florea, M.-E., & Dura, H. (2023). Post-Traumatic Cilia Remaining Inert in the Posterior Chamber for 50 Years. Diagnostics, 13(9), 1575. https://doi.org/10.3390/diagnostics13091575











