Risk of Cardiovascular Events in Metabolically Healthy Overweight or Obese Adults: Role of LDL-Cholesterol in the Stratification of Risk
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants
2.2. Procedures
2.3. Classification of Participants by BMI and Metabolic Status
2.4. Statistics
3. Results
3.1. CV Risk Associated with BMI and Metabolic Status Combined in the Participants <70 Years
3.2. Models Including Variables with Missing Data
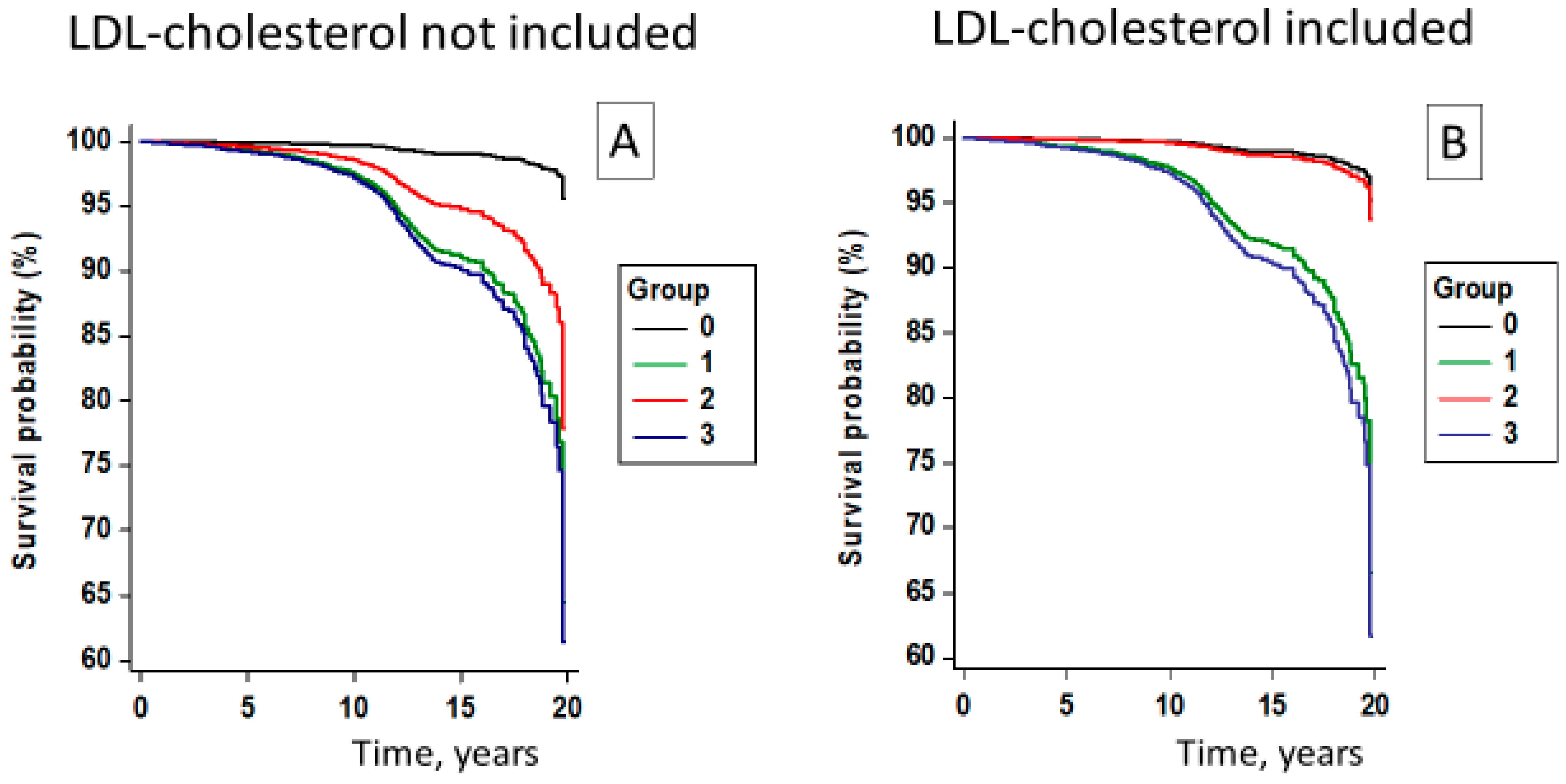
3.3. Metabolically Healthy Status including Normal LDL-Cholesterol Level
4. Discussion
4.1. Prevalence of MHO
4.2. Association of MHO with CV Risk
4.3. The Role of LDL-Cholesterol in the Association between OwOb Status and MACE
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eckel, N.; Meidtner, K.; Kalle-Uhlmann, T.; Stefan, N.; Schulze, M.B. Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016, 23, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.K.; Zinman, B.; Retnakaran, R. Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Ann. Intern. Med. 2013, 159, 758–769. [Google Scholar] [CrossRef]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef] [PubMed]
- Magkos, F. Metabolically healthy obesity: What’s in a name? Am. J. Clin. Nutr. 2019, 110, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Song, Y.; Chen, Y.; Hui, R.; Zhang, W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 168, 4761–4768. [Google Scholar] [CrossRef] [PubMed]
- Zheng, R.; Zhou, D.; Zhu, Y. The long-term prognosis of cardiovascular disease and all-cause mortality for metabolically healthy obesity: A systematic review and meta-analysis. J. Epidemiol. Community Health 2016, 70, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Zhang, L.; Zheng, R.; Zheng, Y. The prevalence, metabolic risk and effects of lifestyle intervention for metabolically healthy obesity: A systematic review and meta-analysis: A PRISMA-compliant article. Medicine 2017, 96, e8838. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; D’Cunha, N.; Tsiampalis, T.; Zec, M.; Sergi, D.; Travica, N.; Marx, W.; McKune, A.J.; Panagiotakos, D.B.; Naumovski, N. Metabolically Healthy Overweight and Obesity, Transition to Metabolically Unhealthy Status and Cognitive Function: Results from the Framingham Offspring Study. Nutrients 2023, 15, 1289. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; Saladini, F.; Mos, L.; Vriz, O.; Ermolao, A.; Battista, F.; Berton, G.; Canevari, M.; Rattazzi, M. Healthy overweight and obesity in the young: Prevalence and risk of major adverse cardiovascular events. Nutr. Metab. Cardiovasc. Dis. 2023; in press. [Google Scholar]
- Shin, M.J.; Hyun, Y.J.; Kim, O.Y.; Kim, J.Y.; Jang, Y.; Lee, J.H. Weight loss effect on inflammation and LDL oxidation in metabolically healthy but obese (MHO) individuals: Low inflammation and LDL oxidation in MHO women. Int. J. Obes. 2006, 30, 1529–1534. [Google Scholar] [CrossRef]
- Meigs, J.B.; Wilson, P.W.; Fox, C.S.; Vasan, R.S.; Nathan, D.M.; Sullivan, L.M.; D’agostino, R.B. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J. Clin. Endocrinol. Metab. 2006, 91, 2906–2912. [Google Scholar] [CrossRef]
- Hamer, M.; Stamatakis, E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J. Clin. Endocrinol. Metab. 2012, 97, 2482–2488. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Tong, W.; Chen, J.; Zhang, Y.; Li, S. Metabolically healthy obesity and its associates in Mongolian Chinese adults. Metab. Syndr. Relat Disord. 2014, 12, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Oda, E. Low-density lipoprotein cholesterol is a predictor of metabolic syndrome in a Japanese health screening population. Intern. Med. 2013, 52, 2707–2713. [Google Scholar] [CrossRef] [PubMed]
- Dramé, M.; Godaert, L. The Obesity Paradox and Mortality in Older Adults: A Systematic Review. Nutrients 2023, 15, 1780. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, D.; Yoshida, T.; Watanabe, Y.; Yamada, Y.; Miyachi, M.; Kimura, M. Frailty modifies the association of body mass index with mortality among older adults: Kyoto-Kameoka study. Clin. Nutr. 2024, 43, 494–502. [Google Scholar] [CrossRef]
- Virdis, A.; Masi, S.; Casiglia, E.; Tikhonoff, V.; Cicero, A.F.; Ungar, A.; Rivasi, G.; Salvetti, M.; Barbagallo, C.M.; Bombelli, M.; et al. Identification of the uric acid thresholds predicting an increased total and cardiovascular mortality over 20 years. Hypertension 2020, 75, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P.; Parati, G.; Virdis, A.; Reboldi, G.; Masi, S.; Mengozzi, A.; from the Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension (SIIA). High heart rate amplifies the risk of cardiovascular mortality associated with elevated uric acid. Eur. J. Prev. Cardiol. 2021, 29, 1501–1509. [Google Scholar] [CrossRef] [PubMed]
- Schleicher, E.; Gerdes, C.; Petersmann, A.; Müller-Wieland, D.; Müller, U.A.; Freckmann, G.; Heinemann, L.; Nauck, M.; Landgraf, R. Definition, Classification and Diagnosis of Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2022, 130, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J. Hypertens. 2023, 41, 1874–2071. [Google Scholar]
- Lackner, K.J.; Peetz, D. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Burnham, K.P.; Anderson, D.R. Model Selection and Multimodel Inference: A Practical Information-Theoretic Approach. 2; Springer: New York, NY, USA, 2002. [Google Scholar]
- Rey-López, J.P.; de Rezende, L.F.; Pastor-Valero, M.; Tess, B.H. The prevalence of metabolically healthy obesity: A systematic review and critical evaluation of the definitions used. Obes. Rev. 2014, 15, 781–790. [Google Scholar] [CrossRef] [PubMed]
- van Vliet-Ostaptchouk, J.V.; Nuotio, M.L.; Slagter, S.N.; Doiron, D.; Fischer, K.; Foco, L.; Gaye, A.; Gögele, M.; Heier, M.; Hiekkalinna, T.; et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: A collaborative analysis of ten large cohort studies. BMC Endocr. Disord. 2014, 14, 9. [Google Scholar] [CrossRef] [PubMed]
- Wildman, R.P.; Muntner, P.; Reynolds, K.; McGinn, A.P.; Rajpathak, S.; Wylie-Rosett, J.; Sowers, M.R. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: Prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch. Intern. Med. 2008, 168, 1617–1624. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.Y.; Wang, M.Y.; Lin, Y.S.; Lin, C.-J.; Lo, K.; Chang, I.-J.; Cheng, T.-Y.; Tsai, S.-Y.; Chen, H.-H.; Lin, C.-Y.; et al. The Association between Metabolically Healthy Obesity, Cardiovascular Disease, and All-Cause Mortality Risk in Asia: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 1320. [Google Scholar] [CrossRef]
- Savastano, S.; Barbato, A.; Di Somma, C.; Guida, B.; Pizza, G.; Barrea, L. Beyond waist circumference in an adult male population of Southern Italy: Is there any role for subscapular skinfold thickness in the relationship between insulin-like growth factor-I system and metabolic parameters? J. Endocrinol. Investig. 2012, 35, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Tellez-Plaza, M.; Briongos-Figuero, L.; Pichler, G.; Dominguez-Lucas, A.; Simal-Blanco, F.; Mena-Martin, F.J.; Bellido-Casado, J.; Arzua-Mouronte, D.; Chaves, F.J.; Redon, J.; et al. Cohort profile: The Hortega Study for the evaluation of non-traditional risk factors of cardiometabolic and other chronic diseases in a general population from Spain. BMJ Open 2019, 9, e024073. [Google Scholar] [CrossRef] [PubMed]
- Visaria, A.; Setoguchi, S. Body mass index and all-cause mortality in a 21st century U.S. population: A National Health Interview Survey analysis. PLoS ONE 2023, 18, e0287218. [Google Scholar] [CrossRef] [PubMed]
- Caleyachetty, R.; Thomas, G.N.; Toulis, K.A.; Mohammed, N.; Gokhale, K.M.; Balachandran, K.; Nirantharakumar, K. Metabolically Healthy Obese and Incident Cardiovascular Disease Events Among 3.5 Million Men and Women. J. Am. Coll. Cardiol. 2017, 70, 1429–1437. [Google Scholar] [CrossRef]
- Hilvo, M.; Dhar, I.; Lääperi, M.; Lysne, V.; Sulo, G.; Tell, G.S.; Jousilahti, P.; Nygård, O.K.; Brenner, H.; Schöttker, B.; et al. Primary cardiovascular risk prediction by LDL-cholesterol in Caucasian middle-aged and older adults: A joint analysis of three cohorts. Eur. J. Prev. Cardiol. 2022, 29, e128–e137. [Google Scholar] [CrossRef]
- Ference, B.A.; Ginsberg, H.N.; Graham, I.; Ray, K.K.; Packard, C.J.; Bruckert, E.; Hegele, R.A.; Krauss, R.M.; Raal, F.J.; Schunkert, H.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2017, 38, 2459–2472. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Grandi, E.; D’Addato, S.; Borghi, C. Interaction between low-density lipoprotein-cholesterolaemia, serum uric level and incident hypertension: Data from the Brisighella Heart Study. J. Hypertens. 2019, 37, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Mongraw-Chaffin, M.; Foster, M.C.; Anderson, C.A.M.; Burke, G.L.; Haq, N.; Kalyani, R.R.; Ouyang, P.; Sibley, C.T.; Tracy, R.; Woodward, M.; et al. Metabolically Healthy Obesity, Transition to Metabolic Syndrome, and Cardiovascular Risk. J. Am. Coll. Cardiol. 2018, 71, 1857–1865. [Google Scholar] [CrossRef] [PubMed]
- Fingeret, M.; Marques-Vidal, P.; Vollenweider, P. Incidence of type 2 diabetes, hypertension, and dyslipidemia in metabolically healthy obese and non-obese. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Panagiotakos, D.B.; Yannakoulia, M.; Georgousopoulou, E.; Critselis, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C.; The ATTICA Study Investigators. Transition from metabolically benign to metabolically unhealthy obesity and 10-year cardiovascular disease incidence: The ATTICA cohort study. Metabolism 2019, 93, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Chen, K.; Wang, A.P.; Gao, J.; Zhao, K.; Wang, H.; Dou, J.; Lv, Z.; Wang, B.; Yan, W.; et al. Cardiovascular disease outcomes in metabolically healthy obesity in communities of Beijing cohort study. Int. J. Clin. Pract. 2019, 73, e13279. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, D.; Perucha, E. Cholesterol metabolism: A new molecular switch to control inflammation. Clin. Sci. 2021, 135, 1389–1408. [Google Scholar] [CrossRef] [PubMed]
- Tall, A.R.; Yvan-Charvet, L. Cholesterol, inflammation and innate immunity. Nat. Rev. Immunol. 2015, 15, 104–116. [Google Scholar] [CrossRef]
- Sesso, H.D.; Buring, J.E.; Rifai, N.; Blake, G.J.; Gaziano, J.M.; Ridker, P.M. C-reactive protein and the risk of developing hypertension. JAMA 2003, 290, 2945–2951. [Google Scholar] [CrossRef]
- Solak, Y.; Afsar, B.; Vaziri, N.D.; Aslan, G.; Yalcin, C.E.; Covic, A.; Kanbay, M. Hypertension as an autoimmune and inflammatory disease. Hypertens. Res. 2016, 39, 567–573. [Google Scholar] [CrossRef]

| BMI < 25 kg/m2 | BMI ≥ 25 kg/m2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Metab− N = 983 | Metab+ N = 3604 | Metab− N = 438 | Metab+ N = 6560 | ||||||
| Variable | Mean | SD | Mean | SD | Mean | SD | Mean | SD | p-Value |
| Age, years | 40.9 | 11.7 | 51.5 | 12.1 | 46.9 | 12.1 | 54.1 | 10.9 | <0.001 |
| BMI, kg/m2 | 21.7 | 2.0 | 22.7 | 1.7 | 27.9 | 3.0 | 29.1 | 3.5 | <0.001 |
| Office SBP, mmHg | 114.6 | 8.8 | 139.2 | 21.7 | 117.1 | 8.2 | 141.8 | 21.0 | <0.001 |
| Office DBP, mmHg | 71.9 | 6.7 | 84.7 | 12.6 | 74.1 | 6.2 | 86.0 | 12.3 | <0.001 |
| Heart rate, bpm | 68.6 | 10.8 | 72.4 | 12.5 | 67.7 | 10.4 | 72.4 | 12.2 | <0.001 |
| Glucose, mg/dL | 82.5 | 7.2 | 92.1 | 16.4 | 85.2 | 7.4 | 98.2 | 22.2 | <0.001 |
| Triglycerides, mg/dL | 73.9 | 27.3 | 106.8 | 60.6 | 83.9 | 30.4 | 135.9 | 79.3 | <0.001 |
| Uric acid, mg/dL | 4.2 | 1.0 | 4.5 | 1.3 | 4.7 | 1.3 | 5.1 | 1.3 | <0.001 |
| Total cholesterol, mg/dL | 200.8 | 37.7 | 209.4 | 39.6 | 208.4 | 37.5 | 215.9 | 38.8 | <0.001 |
| HDL-cholesterol, mg/dL | 63.4 | 13.4 | 55.6 | 15.1 | 59.1 | 12.4 | 50.1 | 13.1 | <0.001 |
| LDL-cholesterol, mg/dL | 122.7 | 34.9 | 132.4 | 35.5 | 132.4 | 34.5 | 138.5 | 35.8 | <0.001 |
| Sex, males, % | 42.2 | ---- | 49.3 | ---- | 47.0 | ---- | 49.0 | ---- | 0.001 |
| Smoker or ex-smoker, % | 33.9 | ---- | 36.8 | ---- | 34.9 | ---- | 37.3 | ---- | 0.17 |
| Anti-HT treatment, % | 8.8 | ---- | 28.1 | ---- | 17.6 | ---- | 37.8 | ---- | <0.001 |
| Alcohol, yes (N = 10,047), % | 35.6 | ---- | 53.9 | ---- | 44.7 | ---- | 59.2 | ---- | <0.001 |
| Sedentary, (N = 8124), % | 50.9 | ---- | 58.6 | ---- | 50.3 | ---- | 61.6 | ---- | <0.001 |
| High waist circ, (N = 8113), % | 2.4 | ---- | 7.5 | ---- | 32.2 | ---- | 44.0 | ---- | <0.001 |
| MACE, % | 0.5 | ---- | 5.7 | ---- | 2.7 | ---- | 7.4 | ---- | <0.001 |
| Group | Estimate | Standard Error | Wald Chi2 | p-Value | Hazard Ratio | 95% Confidence Limit |
|---|---|---|---|---|---|---|
| BMI < 25.0 Metab+ | 1.93 | 0.45 | 18.12 | <0.0001 | 6.92 | 2.84 to 16.86 |
| BMI = 25.0–29.9 Metab− | 1.22 | 0.56 | 4.75 | 0.029 | 3.38 | 1.13 to 10.11 |
| BMI = 25.0–29.9 Metab+ | 1.95 | 0.45 | 18.57 | <0.0001 | 7.06 | 2.90 to 17.18 |
| BMI ≥ 30 Metab− | 1.85 | 0.73 | 6.38 | 0.011 | 6.34 | 1.51 to 26.56 |
| BMI ≥ 30 Metab+ | 2.20 | 0.46 | 23.13 | <0.0001 | 9.00 | 3.67 to 22.04 |
| Group | Wald Chi2 | p-Value | Hazard Ratio | 95% Confidence Limit |
|---|---|---|---|---|
| BMI < 25 and metabolically unhealthy | ||||
| Without including LDL-CT | 18.14 | <0.0001 | 6.91 | 2.40 to 16.83 |
| Including LDL-CT | 7.17 | 0.007 | 4.77 | 1.52 to14.95 |
| BMI ≥ 25 and metabolically healthy | ||||
| Without including LDL-CT | 6.68 | 0.011 | 3.85 | 1.35 to 10.96 |
| Including LDL-CT | 0.07 | 0.79 | 0.73 | 0.08 to 7.04 |
| BMI ≥ 25 and metabolically unhealthy | ||||
| Without including LDL-CT | 19.01 | <0.0001 | 7.19 | 2.96 to 17.45 |
| Including LDL-CT | 8.11 | 0.004 | 5.25 | 1.58 to 16.44 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palatini, P.; Virdis, A.; Masi, S.; Mengozzi, A.; Casiglia, E.; Tikhonoff, V.; Cicero, A.F.G.; Ungar, A.; Parati, G.; Rivasi, G.; et al. Risk of Cardiovascular Events in Metabolically Healthy Overweight or Obese Adults: Role of LDL-Cholesterol in the Stratification of Risk. Diagnostics 2024, 14, 1314. https://doi.org/10.3390/diagnostics14131314
Palatini P, Virdis A, Masi S, Mengozzi A, Casiglia E, Tikhonoff V, Cicero AFG, Ungar A, Parati G, Rivasi G, et al. Risk of Cardiovascular Events in Metabolically Healthy Overweight or Obese Adults: Role of LDL-Cholesterol in the Stratification of Risk. Diagnostics. 2024; 14(13):1314. https://doi.org/10.3390/diagnostics14131314
Chicago/Turabian StylePalatini, Paolo, Agostino Virdis, Stefano Masi, Alessandro Mengozzi, Edoardo Casiglia, Valerie Tikhonoff, Arrigo F. G. Cicero, Andrea Ungar, Gianfranco Parati, Giulia Rivasi, and et al. 2024. "Risk of Cardiovascular Events in Metabolically Healthy Overweight or Obese Adults: Role of LDL-Cholesterol in the Stratification of Risk" Diagnostics 14, no. 13: 1314. https://doi.org/10.3390/diagnostics14131314
APA StylePalatini, P., Virdis, A., Masi, S., Mengozzi, A., Casiglia, E., Tikhonoff, V., Cicero, A. F. G., Ungar, A., Parati, G., Rivasi, G., Salvetti, M., Barbagallo, C. M., Bombelli, M., Dell’Oro, R., Bruno, B., Lippa, L., D’Elia, L., Masulli, M., Verdecchia, P., ... Borghi, C., on behalf of the Working Group on Uric Acid and Cardiovascular Risk of the Italian Society of Hypertension (SIIA). (2024). Risk of Cardiovascular Events in Metabolically Healthy Overweight or Obese Adults: Role of LDL-Cholesterol in the Stratification of Risk. Diagnostics, 14(13), 1314. https://doi.org/10.3390/diagnostics14131314














