Weight-Bearing CT for Diseases around the Ankle Joint
Abstract
1. Introduction
2. Normal Anatomy
3. Diseases around the Ankle Joint
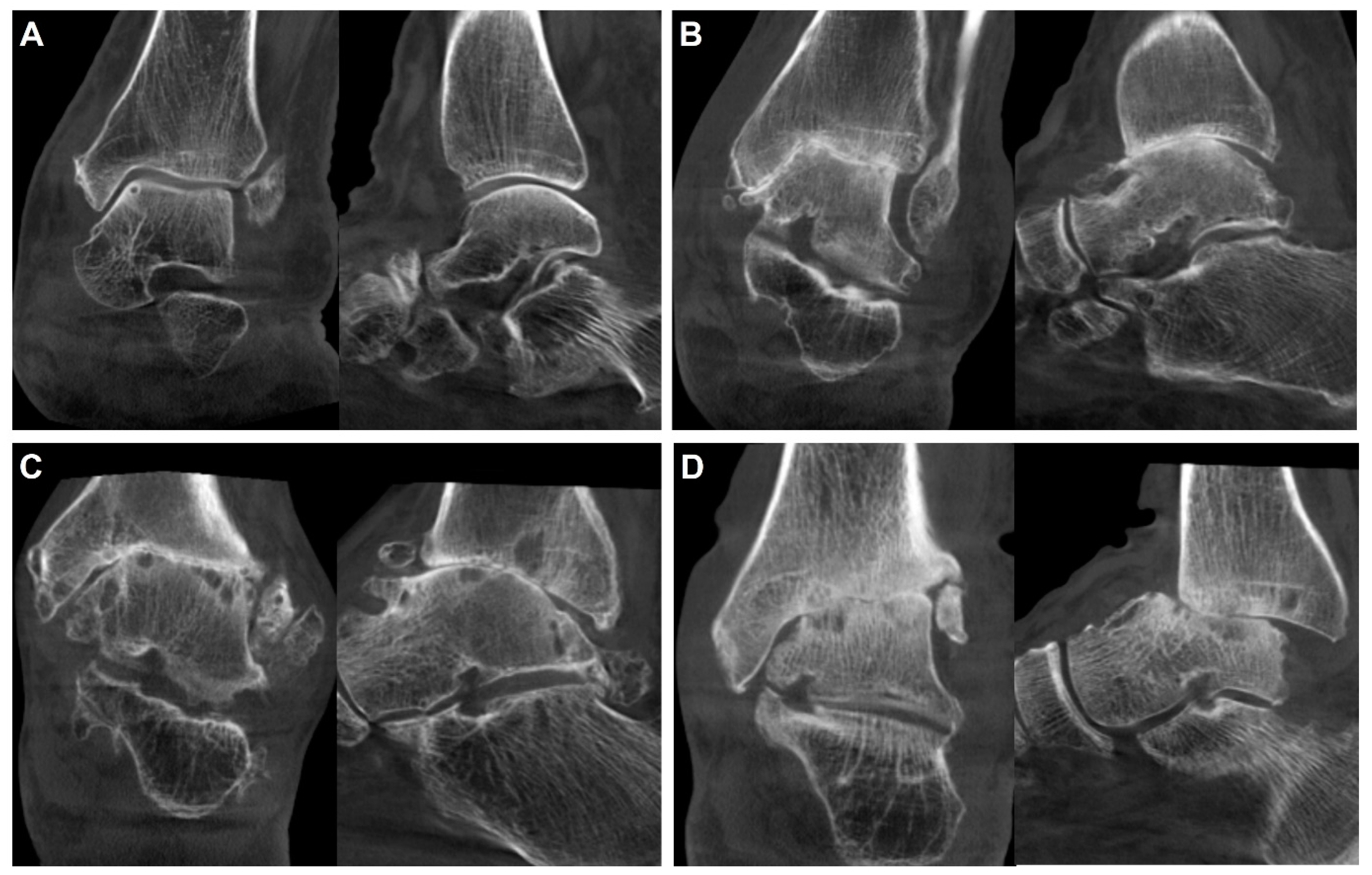
3.1. Ankle Osteoarthritis
3.1.1. Diagnosis
3.1.2. Classification
3.1.3. Treatment
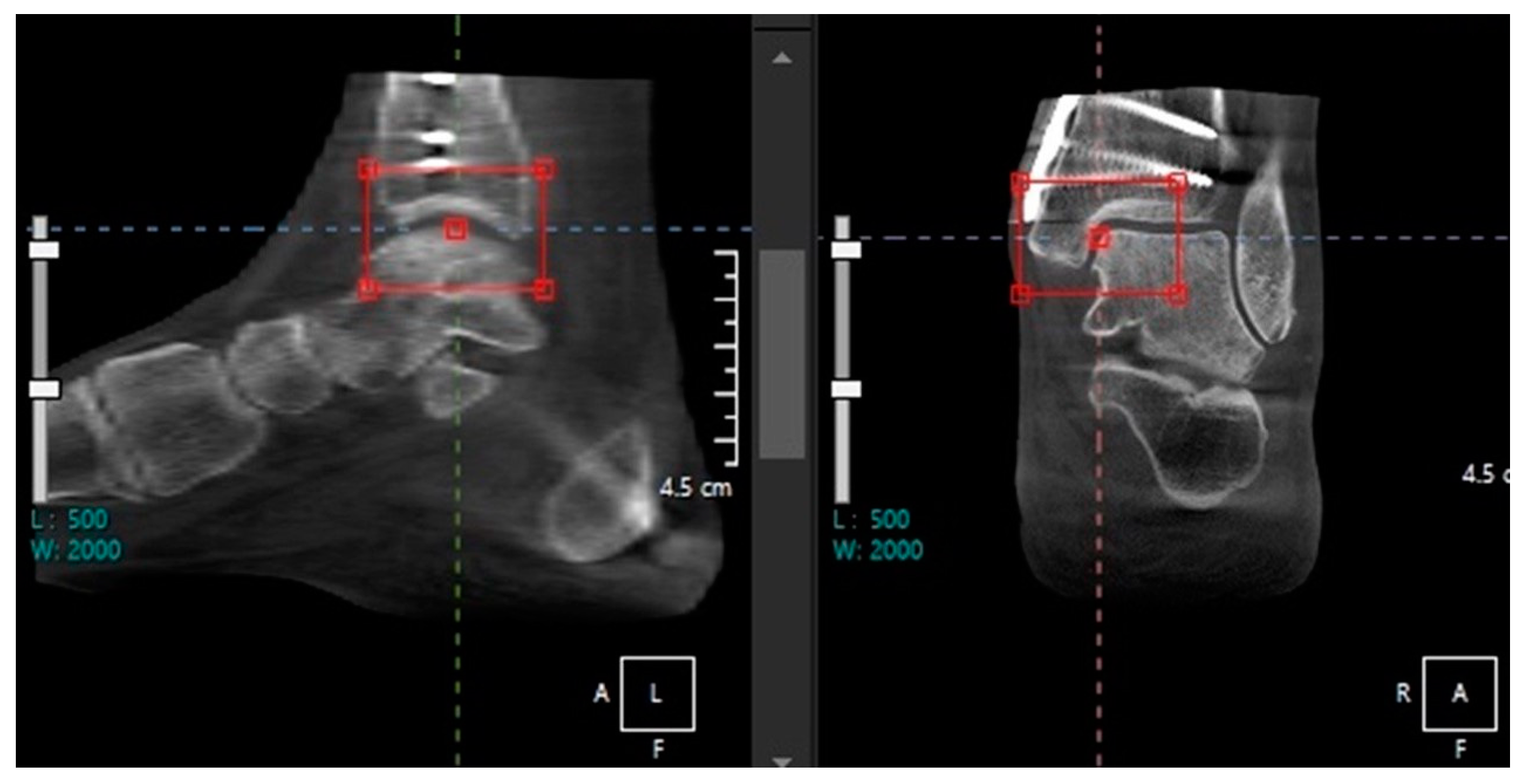
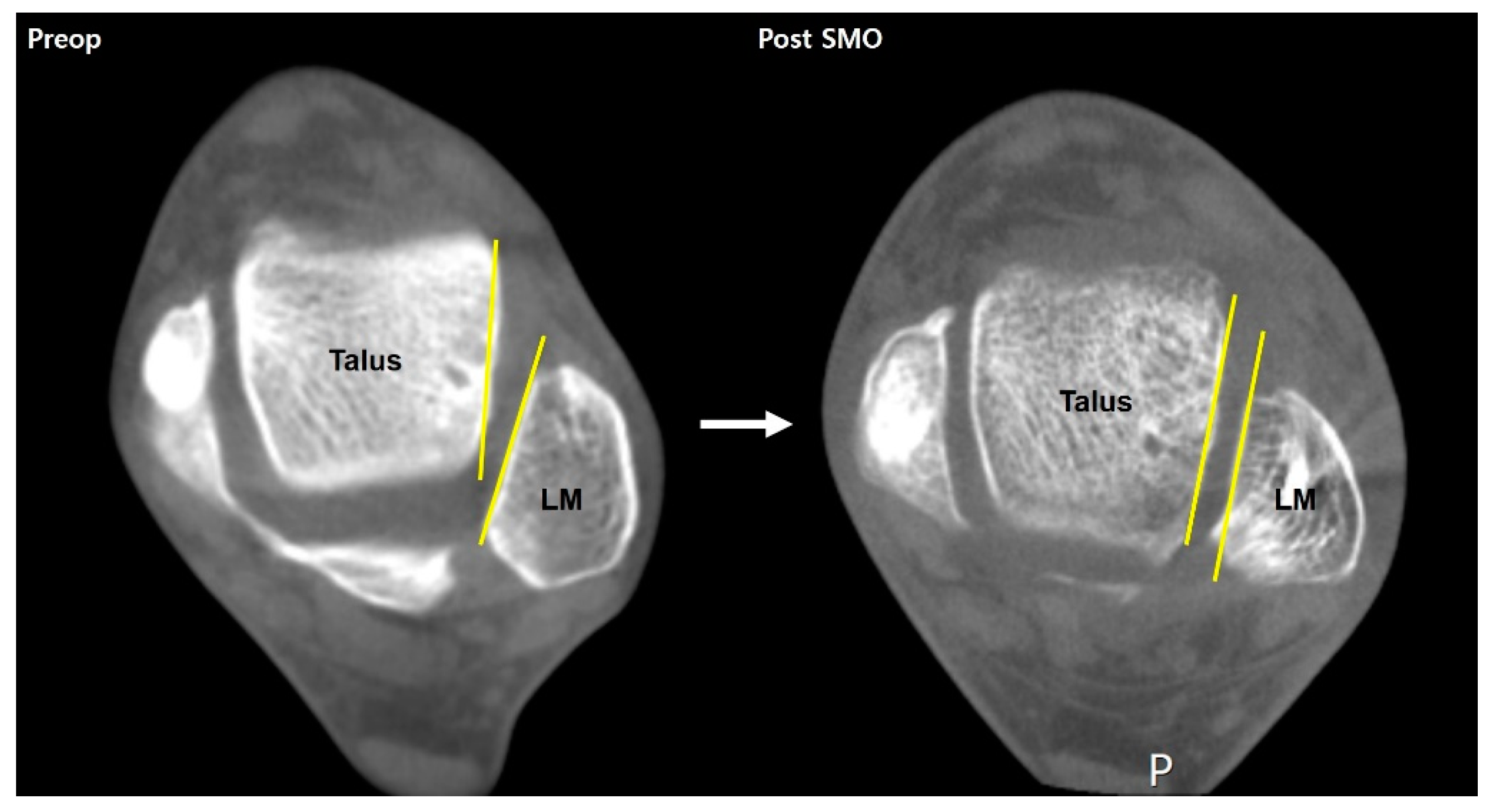
Deformity Correction Surgery
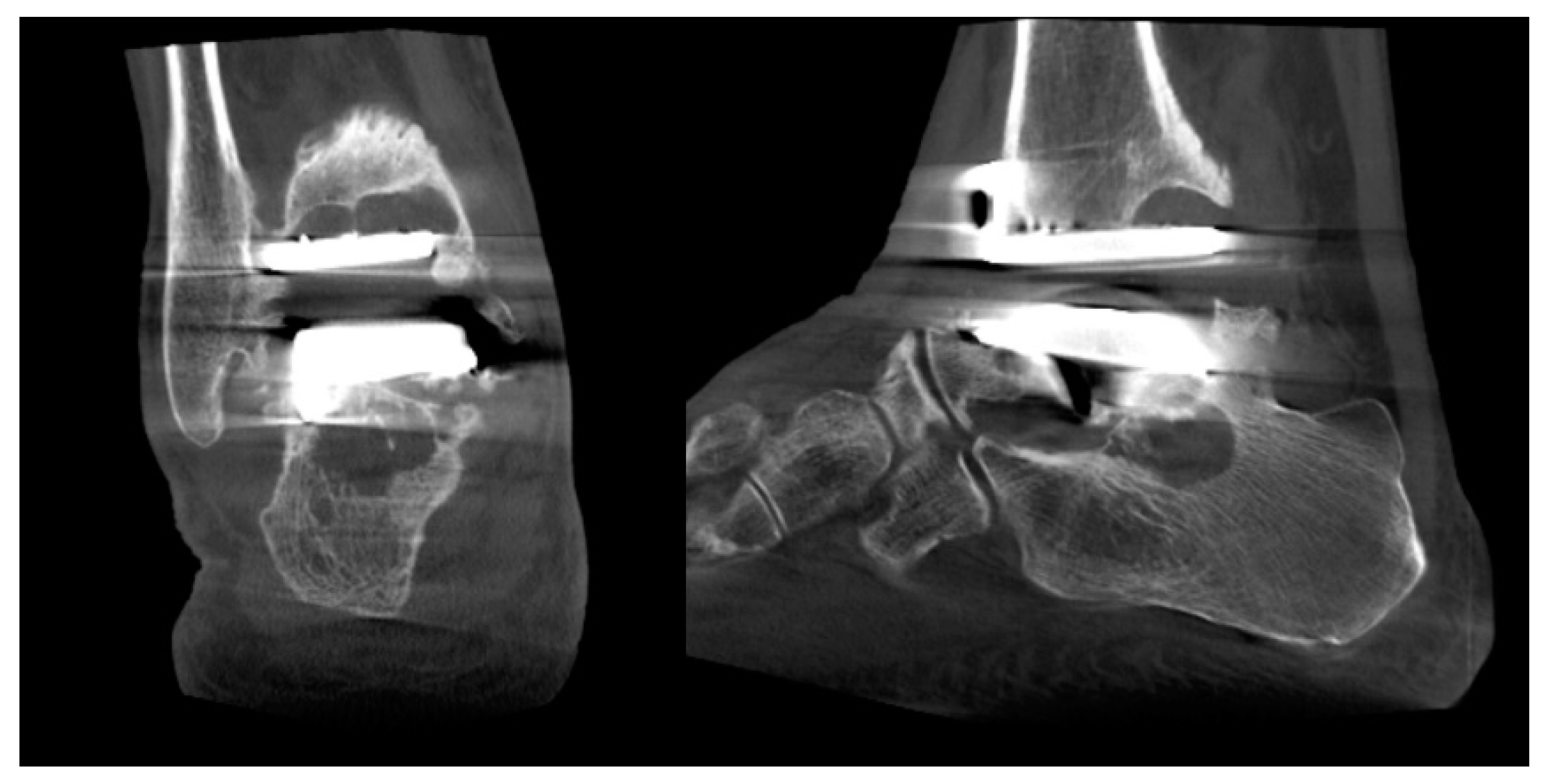
Ankle Replacement Surgery
3.2. Syndesmosis Injury
3.3. Osteochondral Lesion of Talus
3.4. Chronic Ankle Instability
3.5. Acute Ankle Sprain
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Barg, A.; Bailey, T.; Richter, M.; de Cesar Netto, C.; Lintz, F.; Burssens, A.; Phisitkul, P.; Hanrahan, C.J.; Saltzman, C.L. Weightbearing Computed Tomography of the Foot and Ankle: Emerging Technology Topical Review. Foot Ankle Int. 2018, 39, 376–386. [Google Scholar] [CrossRef]
- Lintz, F.; de Cesar Netto, C.; Barg, A.; Burssens, A.; Richter, M. Weight-bearing cone beam CT scans in the foot and ankle. EFORT Open Rev. 2018, 3, 278–286. [Google Scholar] [CrossRef]
- Kang, D.H.; Kang, C.; Hwang, D.S.; Song, J.H.; Song, S.H. The value of axial loading three dimensional (3D) CT as a substitute for full weightbearing (standing) 3D CT: Comparison of reproducibility according to degree of load. Foot Ankle Surg. 2019, 25, 215–220. [Google Scholar] [CrossRef]
- Song, J.H.; Kang, C.; Kim, T.G.; Lee, G.S.; Lee, J.K.; Ahn, K.J.; Kim, D.H.; Lee, S.W. Perioperative axial loading computed tomography findings in varus ankle osteoarthritis: Effect of supramalleolar osteotomy on abnormal internal rotation of the talus. Foot Ankle Surg. 2021, 27, 217–223. [Google Scholar] [CrossRef]
- Richter, M.; Lintz, F.; de Cesar Netto, C.; Barg, A.; Burssens, A. Results of more than 11,000 scans with weightbearing CT—Impact on costs, radiation exposure, and procedure time. Foot Ankle Surg. 2020, 26, 518–522. [Google Scholar] [CrossRef]
- Lepojärvi, S.; Niinimäki, J.; Pakarinen, H.; Koskela, L.; Leskelä, H.V. Rotational Dynamics of the Talus in a Normal Tibiotalar Joint as Shown by Weight-Bearing Computed Tomography. J. Bone Jt. Surg. Am. 2016, 98, 568–575. [Google Scholar] [CrossRef]
- Colin, F.; Horn Lang, T.; Zwicky, L.; Hintermann, B.; Knupp, M. Subtalar joint configuration on weightbearing CT scan. Foot Ankle Int. 2014, 35, 1057–1062. [Google Scholar] [CrossRef]
- Richter, M.; Lintz, F.; Zech, S.; Meissner, S.A. Combination of PedCAT Weightbearing CT with Pedography Assessment of the Relationship Between Anatomy-Based Foot Center and Force/Pressure-Based Center of Gravity. Foot Ankle Int. 2018, 39, 361–368. [Google Scholar] [CrossRef]
- Tazegul, T.E.; Anderson, D.D.; Barbachan Mansur, N.S.; Kajimura Chinelati, R.M.; Iehl, C.; VandeLune, C.; Ahrenholz, S.; Lalevee, M.; de Cesar Netto, C. An Objective Computational Method to Quantify Ankle Osteoarthritis from Low-Dose Weightbearing Computed Tomography. Foot Ankle Orthop. 2022, 7, 24730114221116805. [Google Scholar] [CrossRef]
- Kim, J.B.; Yi, Y.; Kim, J.Y.; Cho, J.H.; Kwon, M.S.; Choi, S.H.; Lee, W.C. Weight-bearing computed tomography findings in varus ankle osteoarthritis: Abnormal internal rotation of the talus in the axial plane. Skelet. Radiol. 2017, 46, 1071–1080. [Google Scholar] [CrossRef]
- Willey, M.C.; Compton, J.T.; Marsh, J.L.; Kleweno, C.P.; Agel, J.; Scott, E.J.; Bui, G.; Davison, J.; Anderson, D.D. Weight-Bearing CT Scan After Tibial Pilon Fracture Demonstrates Significant Early Joint-Space Narrowing. J. Bone Jt. Surg. Am. 2020, 102, 796–803. [Google Scholar] [CrossRef]
- Turmezei, T.D.; Malhotra, K.; MacKay, J.W.; Gee, A.H.; Treece, G.M.; Poole, K.E.S.; Welck, M.J. 3-D joint space mapping at the ankle from weight-bearing CT: Reproducibility, repeatability, and challenges for standardisation. Eur. Radiol. 2023, 33, 8333–8342. [Google Scholar] [CrossRef]
- Barg, A.; Amendola, R.L.; Henninger, H.B.; Kapron, A.L.; Saltzman, C.L.; Anderson, A.E. Influence of Ankle Position and Radiographic Projection Angle on Measurement of Supramalleolar Alignment on the Anteroposterior and Hindfoot Alignment Views. Foot Ankle Int. 2015, 36, 1352–1361. [Google Scholar] [CrossRef]
- Bernasconi, A.; Cooper, L.; Lyle, S.; Patel, S.; Cullen, N.; Singh, D.; Welck, M. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg. 2020, 26, 564–572. [Google Scholar] [CrossRef]
- Krähenbühl, N.; Tschuck, M.; Bolliger, L.; Hintermann, B.; Knupp, M. Orientation of the Subtalar Joint: Measurement and Reliability Using Weightbearing CT Scans. Foot Ankle Int. 2016, 37, 109–114. [Google Scholar] [CrossRef]
- Kang, H.W.; Kim, D.Y.; Park, G.Y.; Lee, D.O.; Lee, D.Y. Coronal plane Calcaneal-Talar Orientation in Varus Ankle Osteoarthritis. Foot Ankle Int. 2022, 43, 928–936. [Google Scholar] [CrossRef]
- TAKAKURA, Y. The Treatment for Osteoarthritis of Ankle Joint. Jpn. J. Rheum. Jt. Surg. 1986, 5, 347–352. [Google Scholar]
- Kim, J.B.; Park, C.H.; Ahn, J.Y.; Kim, J.; Lee, W.C. Characteristics of medial gutter arthritis on weightbearing CT and plain radiograph. Skelet. Radiol. 2021, 50, 1575–1583. [Google Scholar] [CrossRef] [PubMed]
- Holzer, N.; Salvo, D.; Marijnissen, A.C.; Vincken, K.L.; Ahmad, A.C.; Serra, E.; Hoffmeyer, P.; Stern, R.; Lübbeke, A.; Assal, M. Radiographic evaluation of posttraumatic osteoarthritis of the ankle: The Kellgren-Lawrence scale is reliable and correlates with clinical symptoms. Osteoarthr. Cartil. 2015, 23, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Krause, F.G.; Di Silvestro, M.; Penner, M.J.; Wing, K.J.; Glazebrook, M.A.; Daniels, T.R.; Lau, J.T.; Stothers, K.; Younger, A.S. Inter- and intraobserver reliability of the COFAS end-stage ankle arthritis classification system. Foot Ankle Int. 2010, 31, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; de Cesar Netto, C.; Lintz, F.; Barg, A.; Burssens, A.; Ellis, S. The Assessment of Ankle Osteoarthritis with Weight-Bearing Computed Tomography. Foot Ankle Clin. 2022, 27, 13–36. [Google Scholar] [CrossRef] [PubMed]
- Hintermann, B.; Knupp, M.; Barg, A. Supramalleolar Osteotomies for the Treatment of Ankle Arthritis. J. Am. Acad. Orthop. Surg. 2016, 24, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.J.; Azam, M.T.; Weiss, M.B.; Kennedy, J.G.; Walls, R.J. Supramalleolar osteotomy for the treatment of ankle osteoarthritis leads to favourable outcomes and low complication rates at mid-term follow-up: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 701–715. [Google Scholar] [CrossRef] [PubMed]
- Knupp, M.; Stufkens, S.A.; van Bergen, C.J.; Blankevoort, L.; Bolliger, L.; van Dijk, C.N.; Hintermann, B. Effect of supramalleolar varus and valgus deformities on the tibiotalar joint: A cadaveric study. Foot Ankle Int. 2011, 32, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Burssens, A.; Susdorf, R.; Krähenbühl, N.; Peterhans, U.; Ruiz, R.; Barg, A.; Hintermann, B. Supramalleolar Osteotomy for Ankle Varus Deformity Alters Subtalar Joint Alignment. Foot Ankle Int. 2022, 43, 1194–1203. [Google Scholar] [CrossRef]
- Faict, S.; Burssens, A.; Van Oevelen, A.; Maeckelbergh, L.; Mertens, P.; Buedts, K. Correction of ankle varus deformity using patient-specific dome-shaped osteotomy guides designed on weight-bearing CT: A pilot study. Arch. Orthop. Trauma Surg. 2023, 143, 791–799. [Google Scholar] [CrossRef]
- Lee, G.W.; Wang, S.H.; Lee, K.B. Comparison of Intermediate to Long-Term Outcomes of Total Ankle Arthroplasty in Ankles with Preoperative Varus, Valgus, and Neutral Alignment. J. Bone Jt. Surg. Am. 2018, 100, 835–842. [Google Scholar] [CrossRef]
- Pugely, A.J.; Lu, X.; Amendola, A.; Callaghan, J.J.; Martin, C.T.; Cram, P. Trends in the use of total ankle replacement and ankle arthrodesis in the United States Medicare population. Foot Ankle Int. 2014, 35, 207–215. [Google Scholar] [CrossRef]
- Yasutomi, M.; An, V.V.G.; Xu, J.; Wines, A.; Sivakumar, B.S.; Symes, M.J. Trends in the use of ankle arthrodesis and total ankle replacements in Australia over the past 20 years. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1997–2001. [Google Scholar] [CrossRef]
- Tapaninaho, K.; Ponkilainen, V.T.; Haapasalo, H.; Mattila, V.M.; Huttunen, T.T.; Repo, J.P. Incidence of ankle arthrodesis and total ankle replacement between 1997 and 2018: A nationwide registry study in Finland. Foot Ankle Surg. 2023, 29, 288–292. [Google Scholar] [CrossRef]
- Tucker, W.A.; Barnds, B.L.; Morris, B.L.; Tarakemeh, A.; Mullen, S.; Schroeppel, J.P.; Vopat, B.G. Nationwide Analysis of Total Ankle Replacement and Ankle Arthrodesis in Medicare Patients: Trends, Complications, and Cost. Foot Ankle Spec. 2022, 15, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.H.; Daniels, T.R. Ankle arthritis. J. Bone Jt. Surg. Am. 2003, 85, 923–936. [Google Scholar] [CrossRef] [PubMed]
- Cody, E.A.; Scott, D.J.; Easley, M.E. Total Ankle Arthroplasty: A Critical Analysis Review. JBJS Rev. 2018, 6, e8. [Google Scholar] [CrossRef] [PubMed]
- SooHoo, N.F.; Zingmond, D.S.; Ko, C.Y. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J. Bone Jt. Surg. Am. 2007, 89, 2143–2149. [Google Scholar] [CrossRef]
- Goldberg, A.J.; Chowdhury, K.; Bordea, E.; Hauptmannova, I.; Blackstone, J.; Brooking, D.; Deane, E.L.; Bendall, S.; Bing, A.; Blundell, C.; et al. Total Ankle Replacement Versus Arthrodesis for End-Stage Ankle Osteoarthritis: A Randomized Controlled Trial. Ann. Intern. Med. 2022, 175, 1648–1657. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Merchan, E.C.; Moracia-Ochagavia, I. Results of Total Ankle Arthroplasty Versus Ankle Arthrodesis. Foot Ankle Clin. 2024, 29, 27–52. [Google Scholar] [CrossRef]
- Thompson, M.J.; Consul, D.; Umbel, B.D.; Berlet, G.C. Accuracy of Weightbearing CT Scans for Patient-Specific Instrumentation in Total Ankle Arthroplasty. Foot Ankle Orthop. 2021, 6, 24730114211061493. [Google Scholar] [CrossRef] [PubMed]
- Zeitlin, J.; Henry, J.; Ellis, S. Preoperative Guidance with Weight-Bearing Computed Tomography and Patient-Specific Instrumentation in Foot and Ankle Surgery. HSS J. 2021, 17, 326–332. [Google Scholar] [CrossRef] [PubMed]
- de Cesar Netto, C.; Day, J.; Godoy-Santos, A.L.; Roney, A.; Barbachan Mansur, N.S.; Lintz, F.; Ellis, S.J.; Demetracopoulos, C.A. The use of three-dimensional biometric Foot and Ankle Offset to predict additional realignment procedures in total ankle replacement. Foot Ankle Surg. 2022, 28, 1029–1034. [Google Scholar] [CrossRef]
- Vale, C.; Almeida, J.F.; Pereira, B.; Andrade, R.; Espregueira-Mendes, J.; Gomes, T.M.; Oliva, X.M. Complications after total ankle arthroplasty- A systematic review. Foot Ankle Surg. 2023, 29, 32–38. [Google Scholar] [CrossRef]
- Glazebrook, M.A.; Arsenault, K.; Dunbar, M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009, 30, 945–949. [Google Scholar] [CrossRef] [PubMed]
- Lawton, C.D.; Prescott, A.; Butler, B.A.; Awender, J.F.; Selley, R.S.; Dekker Ii, R.G.; Balderama, E.S.; Kadakia, A.R. Modern total ankle arthroplasty versus ankle arthrodesis: A systematic review and meta-analysis. Orthop. Rev. 2020, 12, 8279. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; Mast, J.; Bernasconi, A.; Mehdi, N.; de Cesar Netto, C.; Fernando, C.; Buedts, K. 3D, Weightbearing Topographical Study of Periprosthetic Cysts and Alignment in Total Ankle Replacement. Foot Ankle Int. 2020, 41, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chun, D.I.; Kim, J.; Kim, Y.S.; Cho, J.H.; Won, S.H.; Park, S.Y.; Yi, Y. Relationship between fracture morphology of lateral malleolus and syndesmotic stability after supination-external rotation type ankle fractures. Injury 2019, 50, 1382–1387. [Google Scholar] [CrossRef]
- Dikos, G.D.; Heisler, J.; Choplin, R.H.; Weber, T.G. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J. Orthop. Trauma 2012, 26, 433–438. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.H.; Kwon, H.W.; Lee, M.; Kim, D.; Choi, Y.J.; Park, K.R.; Lee, S.; Cho, J. Normal Distal Tibiofibular Syndesmosis Assessment Using Postmortem Computed Tomography (PMCT). Diagnostics 2023, 14, 36. [Google Scholar] [CrossRef]
- Li, J.; Fang, M.; Van Oevelen, A.; Peiffer, M.; Audenaert, E.; Burssens, A. Diagnostic applications and benefits of weightbearing CT in the foot and ankle: A systematic review of clinical studies. Foot Ankle Surg. 2024, 30, 7–20. [Google Scholar] [CrossRef]
- Hagemeijer, N.C.; Chang, S.H.; Abdelaziz, M.E.; Casey, J.C.; Waryasz, G.R.; Guss, D.; DiGiovanni, C.W. Range of Normal and Abnormal Syndesmotic Measurements Using Weightbearing CT. Foot Ankle Int. 2019, 40, 1430–1437. [Google Scholar] [CrossRef]
- Krähenbühl, N.; Bailey, T.L.; Weinberg, M.W.; Davidson, N.P.; Hintermann, B.; Presson, A.P.; Allen, C.M.; Henninger, H.B.; Saltzman, C.L.; Barg, A. Is load application necessary when using computed tomography scans to diagnose syndesmotic injuries? A cadaver study. Foot Ankle Surg. 2020, 26, 198–204. [Google Scholar] [CrossRef]
- Krähenbühl, N.; Bailey, T.L.; Weinberg, M.W.; Davidson, N.P.; Hintermann, B.; Presson, A.P.; Allen, C.M.; Henninger, H.B.; Saltzman, C.L.; Barg, A. Impact of Torque on Assessment of Syndesmotic Injuries Using Weightbearing Computed Tomography Scans. Foot Ankle Int. 2019, 40, 710–719. [Google Scholar] [CrossRef]
- Shamrock, A.; Den Hartog, T.J.; Dowley, K.; Day, J.; Barbachan Mansur, N.S.; Carvalho, K.A.M.; de Cesar Netto, C.; O’Malley, M. Normal Values for Distal Tibiofibular Syndesmotic Space with and without Subject-Driven External Rotation Stress. Foot Ankle Int. 2024, 45, 80–85. [Google Scholar] [CrossRef]
- Bhimani, R.; Ashkani-Esfahani, S.; Lubberts, B.; Guss, D.; Hagemeijer, N.C.; Waryasz, G.; DiGiovanni, C.W. Utility of Volumetric Measurement via Weight-Bearing Computed Tomography Scan to Diagnose Syndesmotic Instability. Foot Ankle Int. 2020, 41, 859–865. [Google Scholar] [CrossRef]
- Walley, K.C.; Gonzalez, T.A.; Callahan, R.; Fairfull, A.; Roush, E.; Saloky, K.L.; Juliano, P.J.; Lewis, G.S.; Aynardi, M.C. The Role of 3D Reconstruction True-Volume Analysis in Osteochondral Lesions of the Talus: A Case Series. Foot Ankle Int. 2018, 39, 1113–1119. [Google Scholar] [CrossRef]
- Yasui, Y.; Hannon, C.P.; Fraser, E.J.; Ackermann, J.; Boakye, L.; Ross, K.A.; Duke, G.L.; Shimozono, Y.; Kennedy, J.G. Lesion Size Measured on MRI Does Not Accurately Reflect Arthroscopic Measurement in Talar Osteochondral Lesions. Orthop. J. Sports Med. 2019, 7, 2325967118825261. [Google Scholar] [CrossRef]
- Siegler, S.; Konow, T.; Belvedere, C.; Ensini, A.; Kulkarni, R.; Leardini, A. Analysis of surface-to-surface distance mapping during three-dimensional motion at the ankle and subtalar joints. J. Biomech. 2018, 76, 204–211. [Google Scholar] [CrossRef]
- Dibbern, K.N.; Li, S.; Vivtcharenko, V.; Auch, E.; Lintz, F.; Ellis, S.J.; Femino, J.E.; de Cesar Netto, C. Three-Dimensional Distance and Coverage Maps in the Assessment of Peritalar Subluxation in Progressive Collapsing Foot Deformity. Foot Ankle Int. 2021, 42, 757–767. [Google Scholar] [CrossRef]
- Efrima, B.; Dahmen, J.; Barbero, A.; Benady, A.; Maccario, C.; Indino, C.; Kerkhoffs, G.; Usuelli, F.G. Enhancing precision in osteochondral lesions of the talus measurements and improving agreement in surgical decision-making using weight-bearing computed tomography and distance mapping. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1871–1879. [Google Scholar] [CrossRef]
- Van Bergeyk, A.B.; Younger, A.; Carson, B. CT analysis of hindfoot alignment in chronic lateral ankle instability. Foot Ankle Int. 2002, 23, 37–42. [Google Scholar] [CrossRef]
- Lintz, F.; Bernasconi, A.; Baschet, L.; Fernando, C.; Mehdi, N.; de Cesar Netto, C. Relationship Between Chronic Lateral Ankle Instability and Hindfoot Varus Using Weight-Bearing Cone Beam Computed Tomography. Foot Ankle Int. 2019, 40, 1175–1181. [Google Scholar] [CrossRef]
- Lintz, F.; Bernasconi, A.; Ferkel, E.I. Can Weight-Bearing Computed Tomography Be a Game-Changer in the Assessment of Ankle Sprain and Ankle Instability? Foot Ankle Clin. 2023, 28, 283–295. [Google Scholar] [CrossRef]
- Fuller, R.M.; Kim, J.; An, T.W.; Rajan, L.; Cororaton, A.D.; Kumar, P.; Deland, J.T.; Ellis, S.J. Assessment of Flatfoot Deformity Using Digitally Reconstructed Radiographs: Reliability and Comparison to Conventional Radiographs. Foot Ankle Int. 2022, 43, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Jacques, T.; Morel, V.; Dartus, J.; Badr, S.; Demondion, X.; Cotten, A. Impact of introducing extremity cone-beam CT in an emergency radiology department: A population-based study. Orthop. Traumatol. Surg. Res. 2021, 107, 102834. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Schilke, R.; Duerr, F.; Zech, S.; Andreas Meissner, S.; Naef, I. Automatic software-based 3D-angular measurement for Weight-Bearing CT (WBCT) provides different angles than measurement by hand. Foot Ankle Surg. 2022, 28, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Zech, S.; Naef, I.; Duerr, F.; Schilke, R. Automatic software-based 3D-angular measurement for weight-bearing CT (WBCT) is valid. Foot Ankle Surg. 2024, 30, 417–422. [Google Scholar] [CrossRef] [PubMed]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Kim, J.; Kim, S.; Yi, Y. Weight-Bearing CT for Diseases around the Ankle Joint. Diagnostics 2024, 14, 1641. https://doi.org/10.3390/diagnostics14151641
Kim J, Kim J, Kim S, Yi Y. Weight-Bearing CT for Diseases around the Ankle Joint. Diagnostics. 2024; 14(15):1641. https://doi.org/10.3390/diagnostics14151641
Chicago/Turabian StyleKim, Jahyung, Jaeyoung Kim, Saintpee Kim, and Young Yi. 2024. "Weight-Bearing CT for Diseases around the Ankle Joint" Diagnostics 14, no. 15: 1641. https://doi.org/10.3390/diagnostics14151641
APA StyleKim, J., Kim, J., Kim, S., & Yi, Y. (2024). Weight-Bearing CT for Diseases around the Ankle Joint. Diagnostics, 14(15), 1641. https://doi.org/10.3390/diagnostics14151641





