Diagnostic Accuracy of Non-Contrast-Enhanced Time-Resolved MR Angiography to Assess Angioarchitectural Classification Features of Brain Arteriovenous Malformations
Abstract
:1. Introduction
2. Materials and Methods
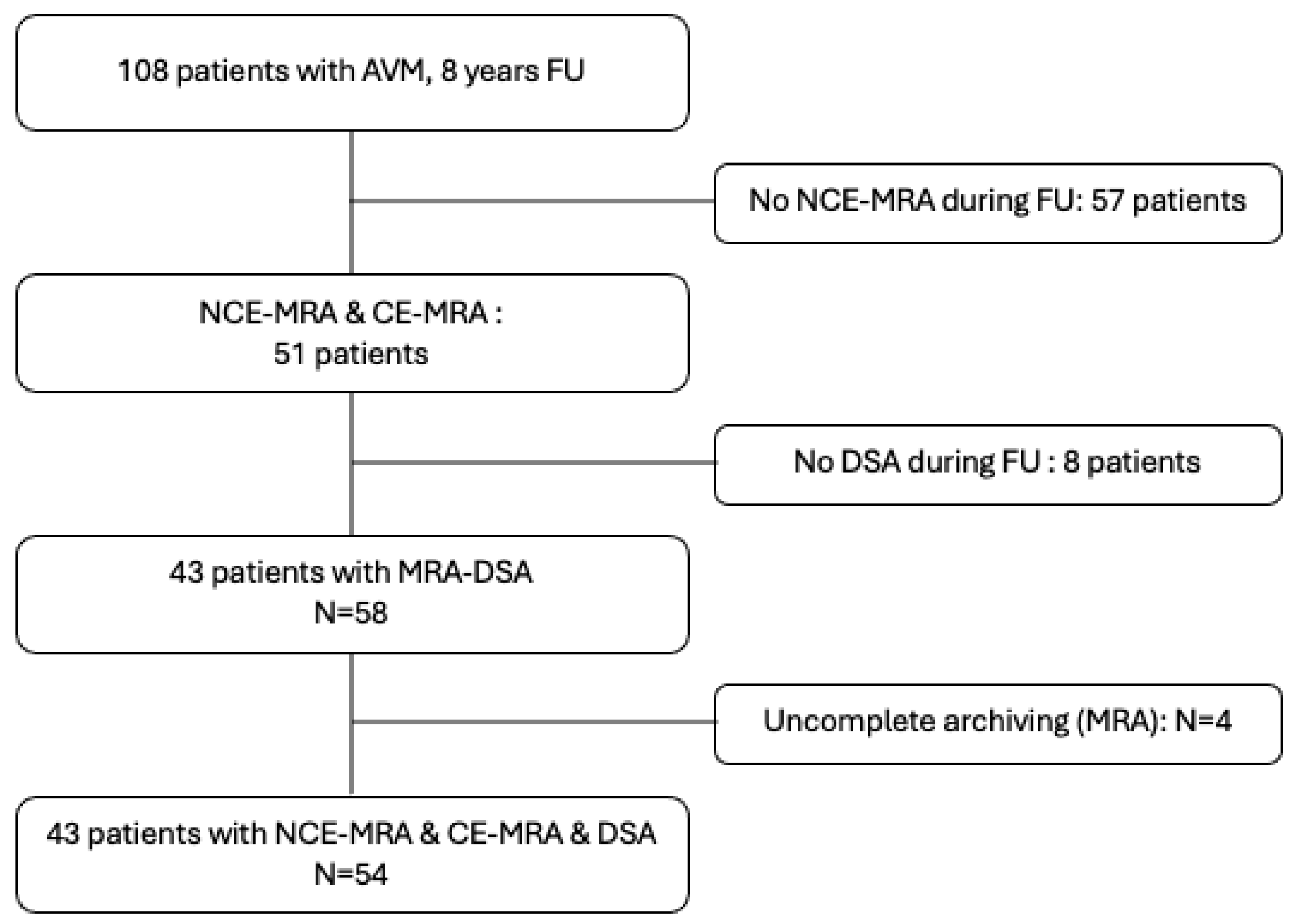
2.1. Recruitment
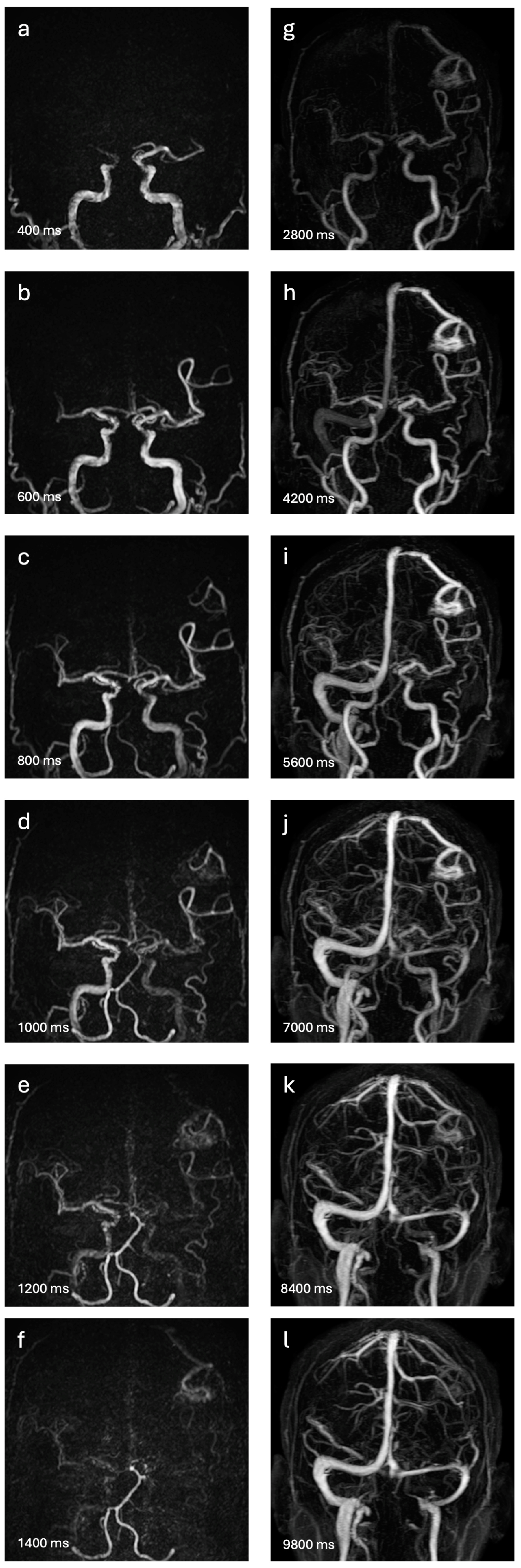
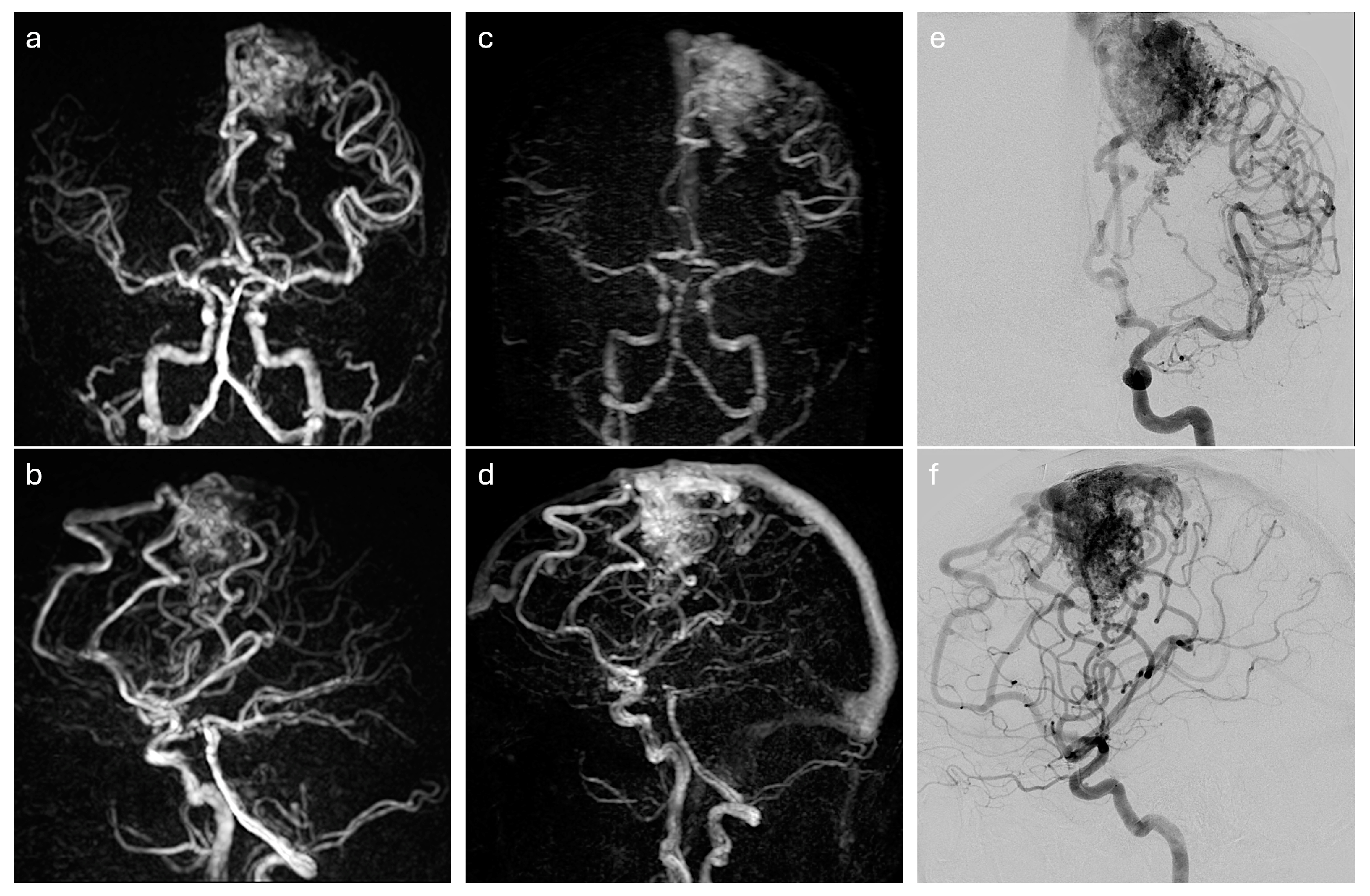
2.2. Four-Dimensional MRA Techniques
2.3. DSA Exploration
2.4. End Points
2.5. Interpretation
2.6. Data Analysis
3. Results
3.1. Population
3.2. Diagnostic Performance and Concordance of 4D-MRAs to Detect Shunts
3.3. Correlation and Concordance of Scaling between DSA and 4D-MRAs
3.4. Agreements of Readings 4D-MRAs Techniques
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mohr, J.P.; Overbey, J.R.; Hartmann, A.; Kummer, R.V.; Al-Shahi Salman, R.; Kim, H.; Van Der Worp, H.B.; Parides, M.K.; Stefani, M.A.; Houdart, E.; et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): Final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 2020, 19, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Leclerc, X.; Gauvrit, J.Y.; Trystram, D.; Reyns, N.; Pruvo, J.P.; Meder, J.F. Imagerie vasculaire non invasive et malformations artérioveineuses cérébrales. J. Neuroradiol. 2004, 31, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Yan, L.; Yao, Y.; Wang, S.; Yang, M.; Wang, B.; Zhuo, Y.; Ai, L.; Miao, X.; Zhao, J.; et al. Noncontrast dynamic MRA in intracranial arteriovenous malformation (AVM): Comparison with time of flight (TOF) and digital subtraction angiography (DSA). Magn. Reson. Imaging 2012, 30, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Iryo, Y.; Hirai, T.; Nakamura, M.; Kawano, T.; Kaku, Y.; Ohmori, Y.; Kai, Y.; Azuma, M.; Nishimura, S.; Shigematsu, Y.; et al. Evaluation of Intracranial Arteriovenous Malformations with Four-Dimensional Arterial-Spin Labeling–Based 3-T Magnetic Resonance Angiography. J. Comput. Assist. Tomogr. 2016, 40, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Fujima, N.; Osanai, T.; Shimizu, Y.; Yoshida, A.; Harada, T.; Nakayama, N.; Kudo, K.; Houkin, K.; Shirato, H. Utility of noncontrast-enhanced time-resolved four-dimensional MR angiography with a vessel-selective technique for intracranial arteriovenous malformations. Magn. Reson. Imaging 2016, 44, 834–845. [Google Scholar] [CrossRef] [PubMed]
- Heit, J.J.; Thakur, N.H.; Iv, M.; Fischbein, N.J.; Wintermark, M.; Dodd, R.L.; Steinberg, G.K.; Chang, S.D.; Kapadia, K.B.; Zaharchuk, G. Arterial-spin labeling MRI identifies residual cerebral arteriovenous malformation following stereotactic radiosurgery treatment. J. Neuroradiol. 2020, 47, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Villabona, A.; Pizzini, F.B.; Solbach, T.; Sokolska, M.; Ricciardi, G.; Lemonis, C.; DeVita, E.; Suzuki, Y.; Van Osch, M.J.P.; Foroni, R.I.; et al. Are Dynamic Arterial Spin-Labeling MRA and Time-Resolved Contrast-Enhanced MRA Suited for Confirmation of Obliteration following Gamma Knife Radiosurgery of Brain Arteriovenous Malformations? AJNR Am. J. Neuroradiol. 2021, 42, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Magro, E.; Gentric, J.-C.; Batista, A.L.; Kotowski, M.; Chaalala, C.; Roberge, D.; Weill, A.; Stapf, C.; Roy, D.; Bojanowski, M.W.; et al. The Treatment of Brain AVMs Study (TOBAS): An all-inclusive framework to integrate clinical care and research. J. Neurosurg. 2018, 128, 1823–1829. [Google Scholar] [CrossRef]
- Nakamura, M.; Yoneyama, M.; Tabuchi, T.; Takemura, A.; Obara, M.; Tatsuno, S.; Sawano, S. Vessel-selective, non-contrast enhanced, time-resolved MR angiography with vessel-selective arterial spin labeling technique (CINEMA–SELECT) in intracranial arteries. Radiol. Phys. Technol. 2013, 6, 327–334. [Google Scholar] [CrossRef]
- Willinek, W.A.; Hadizadeh, D.R.; Von Falkenhausen, M.; Urbach, H.; Hoogeveen, R.; Schild, H.H.; Gieseke, J. 4D time-resolved MR angiography with keyhole (4D-TRAK): More than 60 times accelerated MRA using a combination of CENTRA, keyhole, and SENSE at 3.0T. Magn. Reson. Imaging 2008, 27, 1455–1460. [Google Scholar] [CrossRef]
- Spetzler, R.F.; Martin, N.A. A proposed grading system for arteriovenous malformations. J. Neurosurg. 1986, 65, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Lopes, D.K.; Moftakhar, R.; Straus, D.; Munich, S.A.; Chaus, F.; Kaszuba, M.C. Arteriovenous malformation embocure score: AVMES. J. NeuroIntervent Surg. 2016, 8, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Dumont, T.; Kan, P.; Snyder, K.; Hopkins, L.; Siddiqui, A.; Levy, E. A proposed grading system for endovascular treatment of cerebral arteriovenous malformations: Buffalo score. Surg. Neurol. Int. 2015, 6, 3. [Google Scholar] [PubMed]
- Feghali, J.; Yang, W.; Xu, R.; Liew, J.; McDougall, C.G.; Caplan, J.M.; Tamargo, R.J.; Huang, J. R2 eD AVM Score: A Novel Predictive Tool for Arteriovenous Malformation Presentation with Hemorrhage. Stroke 2019, 50, 1703–1710. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Villabona, A.; Sokolska, M.; Solbach, T.; Grieve, J.; Rega, M.; Torrealdea, F.; Pizzini, F.B.; De Vita, E.; Suzuki, Y.; Van Osch, M.J.P.; et al. Planning of gamma knife radiosurgery (GKR) for brain arteriovenous malformations using triple magnetic resonance angiography (triple-MRA). Br. J. Neurosurg. 2022, 36, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Ozyurt, O.; Dincer, A.; Erdem Yildiz, M.; Peker, S.; Yilmaz, M.; Sengoz, M.; Ozturk, C. Integration of arterial spin labeling into stereotactic radiosurgery planning of cerebral arteriovenous malformations. Magn. Reson. Imaging 2017, 46, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Leclerc, X.; Guillaud, O.; Reyns, N.; Hodel, J.; Outteryck, O.; Bala, F.; Bricout, N.; Bretzner, M.; Ramdane, N.; Pruvo, J.-P.; et al. Follow-Up MRI for Small Brain AVMs Treated by Radiosurgery: Is Gadolinium Really Necessary? AJNR Am. J. Neuroradiol. 2020, 41, 437–445. [Google Scholar] [CrossRef]
- Ognard, J.; Magro, E.; Caroff, J.; Bodani, V.; Mosimann, P.J.; Gentric, J.-C. Endovascular Management of Brain Arteriovenous Malformations. Semin. Neurol. 2023, 43, 323–336. [Google Scholar] [CrossRef]
- Cong, F.; Zhuo, Y.; Yu, S.; Zhang, X.; Miao, X.; An, J.; Wang, S.; Cao, Y.; Zhang, Y.; Song, H.K.; et al. Noncontrast-enhanced time-resolved 4D dynamic intracranial MR angiography at 7T: A feasibility study. Magn. Reson. Imaging 2018, 48, 111–120. [Google Scholar] [CrossRef]
- Moon, J.I.; Baek, H.J.; Ryu, K.H.; Park, H. A novel non-contrast-enhanced MRA using silent scan for evaluation of brain arteriovenous malformation: A case report and review of literature. Medicine 2017, 96, e8616. [Google Scholar] [CrossRef] [PubMed]
- Arai, N.; Akiyama, T.; Fujiwara, K.; Koike, K.; Takahashi, S.; Horiguchi, T.; Jinzaki, M.; Yoshida, K. Silent MRA: Arterial spin labeling magnetic resonant angiography with ultra-short time echo assessing cerebral arteriovenous malformation. Neuroradiology 2020, 62, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhou, Z.; Qi, H.; Chen, H.; Chu, B.; Hatsukami, T.S.; Yuan, C.; Balu, N. A novel sequence for simultaneous measurement of whole-brain static and dynamic MRA, intracranial vessel wall image, and T1-weighted structural brain MRI. Magn. Reson. Med 2021, 85, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Togao, O.; Obara, M.; Helle, M.; Yamashita, K.; Kikuchi, K.; Momosaka, D.; Kikuchi, Y.; Nishimura, A.; Arimura, K.; Wada, T.; et al. Vessel-selective 4D-MR angiography using super-selective pseudo-continuous arterial spin labeling may be a useful tool for assessing brain AVM hemodynamics. Eur. Radiol. 2020, 30, 6452–6463. [Google Scholar] [CrossRef] [PubMed]
- Murazaki, H.; Wada, T.; Togao, O.; Obara, M.; Helle, M.; Kobayashi, K.; Ishigami, K.; Kato, T. Improved temporal resolution and acceleration on 4D-MR angiography based on superselective pseudo-continuous arterial spin labeling combined with CENTRA-keyhole and view-sharing (4D-S-PACK) using an interpolation algorithm on the temporal axis and compressed sensing–sensitivity encoding (CS-SENSE). Magn. Reson. Imaging 2024, 109, 1–9. [Google Scholar] [PubMed]
- Kukuk, G.M.; Hadizadeh, D.R.; Boström, A.; Gieseke, J.; Bergener, J.; Nelles, M.; Mürtz, P.; Urbach, H.; Schild, H.H.; Willinek, W.A. Cerebral Arteriovenous Malformations at 3.0 T: Intraindividual Comparative Study of 4D-MRA in Combination with Selective Arterial Spin Labeling and Digital Subtraction Angiography. Investig. Radiol. 2010, 45, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Togao, O.; Obara, M.; Yamashita, K.; Kikuchi, K.; Wada, T.; Murazaki, H.; Arimura, K.; Nishimura, A.; Horie, N.; Van De Ven, K.; et al. Arterial Spin Labeling-Based MR Angiography for Cerebrovascular Diseases: Principles and Clinical Applications. Magn. Reson. Imaging 2023. early view. [Google Scholar] [CrossRef]
- Zhuo, Y.; Chang, J.; Chen, Y.; Wen, C.; Chen, F.; Li, W.; Gao, M.; Luo, W.; Wan, S.; Song, L.; et al. Value of contrast-enhanced MR angiography for the follow-up of treated brain arteriovenous malformations: Systematic review and meta-analysis. Eur. Radiol. 2023, 33, 7139–7148. [Google Scholar] [CrossRef]
- Illies, T.; Forkert, N.D.; Ries, T.; Regelsberger, J.; Fiehler, J. Classification of Cerebral Arteriovenous Malformations and Intranidal Flow Patterns by Color-Encoded 4D-Hybrid-MRA. AJNR Am. J. Neuroradiol. 2013, 34, 46–53. [Google Scholar] [CrossRef]
- Chazot, A.; Barrat, J.-A.; Gaha, M.; Jomaah, R.; Ognard, J.; Ben Salem, D. Brain MRIs make up the bulk of the gadolinium footprint in medical imaging. J. Neuroradiol. 2020, 47, 259–265. [Google Scholar] [CrossRef]
- Pinter, N.K.; Klein, J.P.; Mechtler, L.L. Potential Safety Issues Related to the Use of Gadolinium-based Contrast Agents. Contin. Lifelong Learn. Neurol. 2016, 22, 1678–1684. [Google Scholar] [CrossRef]
- Tedeschi, E.; Caranci, F.; Giordano, F.; Angelini, V.; Cocozza, S.; Brunetti, A. Gadolinium retention in the body: What we know and what we can do. Radiol. Med. 2017, 122, 589–600. [Google Scholar] [CrossRef]
- Pasquini, L.; Napolitano, A.; Visconti, E.; Longo, D.; Romano, A.; Tomà, P.; Espagnet, M.C.R. Gadolinium-Based Contrast Agent-Related Toxicities. CNS Drugs 2018, 32, 229–240. [Google Scholar] [CrossRef]
- Guo, B.J.; Yang, Z.L.; Zhang, L.J. Gadolinium Deposition in Brain: Current Scientific Evidence and Future Perspectives. Front. Mol. Neurosci. 2018, 11, 335. [Google Scholar] [CrossRef] [PubMed]
- Blomqvist, L.; Nordberg, G.F.; Nurchi, V.M.; Aaseth, J.O. Gadolinium in Medical Imaging—Usefulness, Toxic Reactions and Possible Countermeasures—A Review. Biomolecules 2022, 12, 742. [Google Scholar] [CrossRef]
- Iyad, N.; Ahmad, M.S.; Alkhatib, S.G.; Hjouj, M. Gadolinium contrast agents- challenges and opportunities of a multidisciplinary approach: Literature review. Eur. J. Radiol. Open 2023, 11, 100503. [Google Scholar] [CrossRef] [PubMed]
- Fraum, T.J.; Ludwig, D.R.; Bashir, M.R.; Fowler, K.J. Gadolinium-based contrast agents: A comprehensive risk assessment. Magn. Reson. Imaging 2017, 46, 338–353. [Google Scholar] [CrossRef]
- Alghamdi, S.A. Gadolinium-Based Contrast Agents in Pregnant Women: A Literature Review of MRI Safety. Cureus 2023. Available online: https://www.cureus.com/articles/153609-gadolinium-based-contrast-agents-in-pregnant-women-a-literature-review-of-mri-safety (accessed on 3 March 2023).
- Mohr, J.P.; Koennecke, H.-C.; Hartmann, A. Management of brain arteriovenous malformations: Still a long and winding road ahead. Neurology 2020, 95, 899–900. [Google Scholar] [CrossRef] [PubMed]
- Raymond, J.; Gentric, J.-C.; Magro, E.; Nico, L.; Bacchus, E.; Klink, R.; Cognard, C.; Januel, A.-C.; Sabatier, J.-F.; Iancu, D.; et al. Endovascular treatment of brain arteriovenous malformations: Clinical outcomes of patients included in the registry of a pragmatic randomized trial. J. Neurosurg. 2022, 138, 1393–1402. [Google Scholar] [CrossRef]
- Darsaut, T.E.; Magro, E.; Bojanowski, M.W.; Chaalala, C.; Nico, L.; Bacchus, E.; Klink, R.; Iancu, D.; Weill, A.; Roy, D.; et al. Surgical treatment of brain arteriovenous malformations: Clinical outcomes of patients included in the registry of a pragmatic randomized trial. J. Neurosurg. 2022, 138, 891–899. [Google Scholar] [CrossRef]
- Lawton, M.T.; Rutledge, W.C.; Kim, H.; Stapf, C.; Whitehead, K.J.; Li, D.Y.; Krings, T.; terBrugge, K.; Kondziolka, D.; Morgan, M.K.; et al. Brain arteriovenous malformations. Nat. Rev. Dis. Primers 2015, 1, 15008. [Google Scholar] [CrossRef]
- Norris, J.S.; Valiante, T.A.; Wallace, M.C.; Willinsky, R.A.; Montanera, W.J.; terBrugge, K.G.; Tymianski, M. A simple relationship between radiological arteriovenous malformation hemodynamics and clinical presentation: A prospective, blinded analysis of 31 cases. J. Neurosurg. 1999, 90, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Nico, E.; Hossa, J.; McGuire, L.S.; Alaraj, A. Rupture-Risk Stratifying Patients with Cerebral Arteriovenous Malformations Using Quantitative Hemodynamic Flow Measurements. World Neurosurg. 2023, 179, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shi, D.; Chen, C.; Li, Y.; Wang, M.; Han, X.; Jin, L.; Bi, X. Noncontrast-enhanced four-dimensional MR angiography for the evaluation of cerebral arteriovenous malformation: A preliminary trial. Magn. Reson. Imaging 2011, 34, 1199–1205. [Google Scholar] [CrossRef] [PubMed]
- Malikova, H.; Koubska, E.; Vojtech, Z.; Weichet, J.; Syrucek, M.; Sroubek, J.; Rulseh, A.; Liscak, R. Late morphological changes after radiosurgery of brain arteriovenous malformations: An MRI study. Acta Neurochir. 2016, 158, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Soize, S.; Bouquigny, F.; Kadziolka, K.; Portefaix, C.; Pierot, L. Value of 4D MR Angiography at 3T Compared with DSA for the Follow-Up of Treated Brain Arteriovenous Malformation. AJNR Am. J. Neuroradiol. 2014, 35, 1903–1909. [Google Scholar] [CrossRef] [PubMed]
- Günther, M.; Bock, M.; Schad, L.R. Arterial spin labeling in combination with a look-locker sampling strategy: Inflow turbo-sampling EPI-FAIR (ITS-FAIR). Magn. Reson. Med. 2001, 46, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Jagadeesan, B.; Tariq, F.; Nada, A.; Bhatti, I.A.; Masood, K.; Siddiq, F. Principles Behind 4D Time-Resolved MRA/Dynamic MRA in Neurovascular Imaging. Semin. Roentgenol. 2024, 59, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Lahlouh, M.; Blanc, R.; Piotin, M.; Szewczyk, J.; Passat, N.; Chenoune, Y. Cerebral AVM segmentation from 3D rotational angiography images by convolutional neural networks. Neurosci. Inform. 2023, 3, 100138. [Google Scholar] [CrossRef]
- Zhang, H.; Su, Y.; Liang, S.; Lv, X. Transarterial AVM embolization using Tsinghua grading system: Patient selection and complete obliteration. Neurosci. Inform. 2024, 4, 100160. [Google Scholar] [CrossRef]
- Hsu, C.C.-T.; Fomin, I.; Wray, B.; Brideaux, A.; Lyons, D.; Jaya Kumar, M.; Watkins, T.; Haacke, E.M.; Krings, T. Susceptibility weighted imaging for qualitative grading of persistent arteriovenous shunting in deep-seated arteriovenous malformations after stereotactic radiation surgery. Neuroradiol. J. 2023, 36, 414–420. [Google Scholar] [CrossRef]
- Raman, A.; Uprety, M.; Calero, M.J.; Villanueva, M.R.B.; Joshaghani, N.; Villa, N.; Badla, O.; Goit, R.; Saddik, S.E.; Dawood, S.N.; et al. A Systematic Review Comparing Digital Subtraction Angiogram with Magnetic Resonance Angiogram Studies in Demonstrating the Angioarchitecture of Cerebral Arteriovenous Malformations. Cureus 2022. Available online: https://www.cureus.com/articles/97064-a-systematic-review-comparing-digital-subtraction-angiogram-with-magnetic-resonance-angiogram-studies-in-demonstrating-the-angioarchitecture-of-cerebral-arteriovenous-malformations (accessed on 9 June 2022).
| Description | Med. or Freq. | [IQR] or % |
|---|---|---|
| Demographics (over n = 43) | ||
| Age, years | 55 | [34–61] |
| Sex, male | 27 | 62.80% |
| Hemorrhagic presentation | 37 | 68.52% |
| Treated (overall n = 54) | 22 | 40.74% |
| Embolization | 8 | 36.36% |
| Embolization then radiosurgery | 6 | 27.27% |
| Embolization then surgery | 5 | 22.73% |
| Radiosurgery | 3 | 13.64% |
| bAVM location (over n = 43) | ||
| Supratentorial | 38 | 88.30% |
| Infratentorial | 5 | 11.63% |
| bAVM visualisation (DSA consensus) | 40 | 74.07% |
| Shunt (over non-treated n = 32) | 29 | 90.62% |
| Residual shunt (over treated n = 22) | 11 | 50.00% |
| bAVM Grading (DSA consensus, overall) | ||
| SM | 1 | [1–3] |
| AVMES | 3 | [3–6] |
| Buffalo | 2 | [2–3] |
| R2DAVM | 4 | [4–5] |
| Time intervals (overall) | ||
| Delay between DSA and 4D MRA, months | 4 | [1–18] |
| Shunt Detection | CE-4D-MRA | NCE-4D-MRA |
|---|---|---|
| Visualisation (%) | 63.58 | 56.79 |
| Kappa (interobs.) | 0.73 | 0.82 |
| Kappa (vs. DSA) | 0.59 | 0.58 |
| Sensitivity | 80.83 | 75.00 |
| Specificity | 85.71 | 95.24 |
| PPV | 84.17 | 97.82 |
| NPV | 61.10 | 57.14 |
| AUC * | 83.27 | 85.11 |
| CE-4D-MRA (vs. DSA) | NCE-4D-MRA (vs. DSA) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Med./Freq. | IQR/% | p-Value | Corr. Coef. | Kappa | Med./Freq. | IQR/% | p-Value | Corr. Coef. | Kappa |
| Grading scales | ||||||||||
| SM | 2 | [1–4] | 1.000 | 0.76 | 0.58 | 3 | [1–4] | <0.001 * | 0.78 | 0.66 |
| AVMES | 4 | [3–7] | 0.007 * | 0.80 | 0.57 | 4 | [3–6] | 0.014 * | 0.73 | 0.49 |
| Buffalo | 2 | [2–4] | 0.714 | 0.79 | 0.65 | 3 | [2–3.25] | 0.357 | 0.74 | 0.58 |
| R2DAVM | 4 | [3–5] | 0.648 | 0.68 | 0.55 | 4.5 | [4–5] | 0.034 * | 0.70 | 0.55 |
| Features | ||||||||||
| Nidus size (SM) | 1 | [1–2] | 0.555 | 0.85 | 0.77 | 2 | [1–2] | 0.193 | 0.87 | 0.80 |
| Deep location | 14 | 08.64% | <0.001 * | 0.83 | 0.82 | 16 | 09.87% | <0.001 * | 0.67 | 0.66 |
| Eloquency | 55 | 33.95% | 0.021 * | 0.70 | 0.69 | 56 | 34.56% | 0.021 * | 0.71 | 0.70 |
| Fossa posterior | 13 | 08.02% | <0.001 * | 0.96 | 0.95 | 10 | 06.17% | <0.001 * | 1.00 | 1.00 |
| Nb. of feeders | 3 | [1.5–5] | 0.173 | 0.86 | 0.55 | 3 | [2–5] | 0.315 | 0.78 | 0.47 |
| Feeder size > 1 mm | 88 | 90.72 | <0.001 * | 0.71 | 0.71 | 81 | 90.00 | <0.001 * | 0.60 | 0.59 |
| Superf. ven. drain. | 61 | 59.80% | <0.001 * | 0.54 | 0.46 | 69 | 76.67 | 0.019 * | 0.20 | 0.16 |
| Nb. draining veins | 1 | [1–2] | 0.101 | 0.48 | 0.44 | 1 | [1–1] | <0.001 * | 0.30 | 0.20 |
| Nb. ven. aneurysm | 0 | [0–0.5] | <0.001 * | 0.27 | 0.24 | 0 | 0 | <0.001 * | 0.31 | 0.17 |
| Agreements between 4D-MRAs Techniques | ||||||
|---|---|---|---|---|---|---|
| Variables | CE-4D-MRA (Interobs.) | NCE-4D-MRA (Interobs.) | NCE- vs. CE-4D-MRA | |||
| Corr. Coeff. | Kappa | Corr. Coeff. | Kappa | Corr. Coeff. | Kappa | |
| Grading scales | ||||||
| SM | 0.84 | 0.67 | 0.74 | 0.54 | 0.68 | 0.53 |
| AVMES | 0.87 | 0.69 | 0.80 | 0.60 | 0.68 | 0.49 |
| Buffalo | 0.83 | 0.70 | 0.79 | 0.59 | 0.70 | 0.55 |
| R2DAVM | 0.52 | 0.29 | 0.60 | 0.38 | 0.60 | 0.48 |
| Features | ||||||
| Nidus size (SM) | 0.90 | 0.82 | 0.85 | 0.76 | 0.80 | 0.71 |
| Deep location | 0.80 | 0.68 | 0.69 | 0.44 | 0.58 | 0.58 |
| Eloquency | 0.65 | 0.46 | 0.57 | 0.33 | 0.51 | 0.51 |
| Fossa posterior | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Nb. of feeders | 0.92 | 0.79 | 0.82 | 0.65 | 0.73 | 0.56 |
| Feeder size > 1 mm | 0.47 | 0.19 | - | 0.03 | 0.40 | 0.39 |
| Superf. ven. drain. | 0.64 | 0.40 | 0.44 | 0.13 | 0.17 | 0.21 |
| Nb. draining veins | 0.79 | 0.35 | 0.46 | 0.10 | 0.28 | 0.21 |
| Nb. ven. aneurysm | 0.47 | 0.11 | - | 0.14 | 0.27 | 0.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chauvet, G.; Cheddad El Aouni, M.; Magro, E.; Sabardu, O.; Ben Salem, D.; Gentric, J.-C.; Ognard, J. Diagnostic Accuracy of Non-Contrast-Enhanced Time-Resolved MR Angiography to Assess Angioarchitectural Classification Features of Brain Arteriovenous Malformations. Diagnostics 2024, 14, 1656. https://doi.org/10.3390/diagnostics14151656
Chauvet G, Cheddad El Aouni M, Magro E, Sabardu O, Ben Salem D, Gentric J-C, Ognard J. Diagnostic Accuracy of Non-Contrast-Enhanced Time-Resolved MR Angiography to Assess Angioarchitectural Classification Features of Brain Arteriovenous Malformations. Diagnostics. 2024; 14(15):1656. https://doi.org/10.3390/diagnostics14151656
Chicago/Turabian StyleChauvet, Grégoire, Mourad Cheddad El Aouni, Elsa Magro, Ophélie Sabardu, Douraied Ben Salem, Jean-Christophe Gentric, and Julien Ognard. 2024. "Diagnostic Accuracy of Non-Contrast-Enhanced Time-Resolved MR Angiography to Assess Angioarchitectural Classification Features of Brain Arteriovenous Malformations" Diagnostics 14, no. 15: 1656. https://doi.org/10.3390/diagnostics14151656





