The Radiogenomic Landscape of Clear Cell Renal Cell Carcinoma: Insights into Lipid Metabolism through Evaluation of ADFP Expression
Abstract
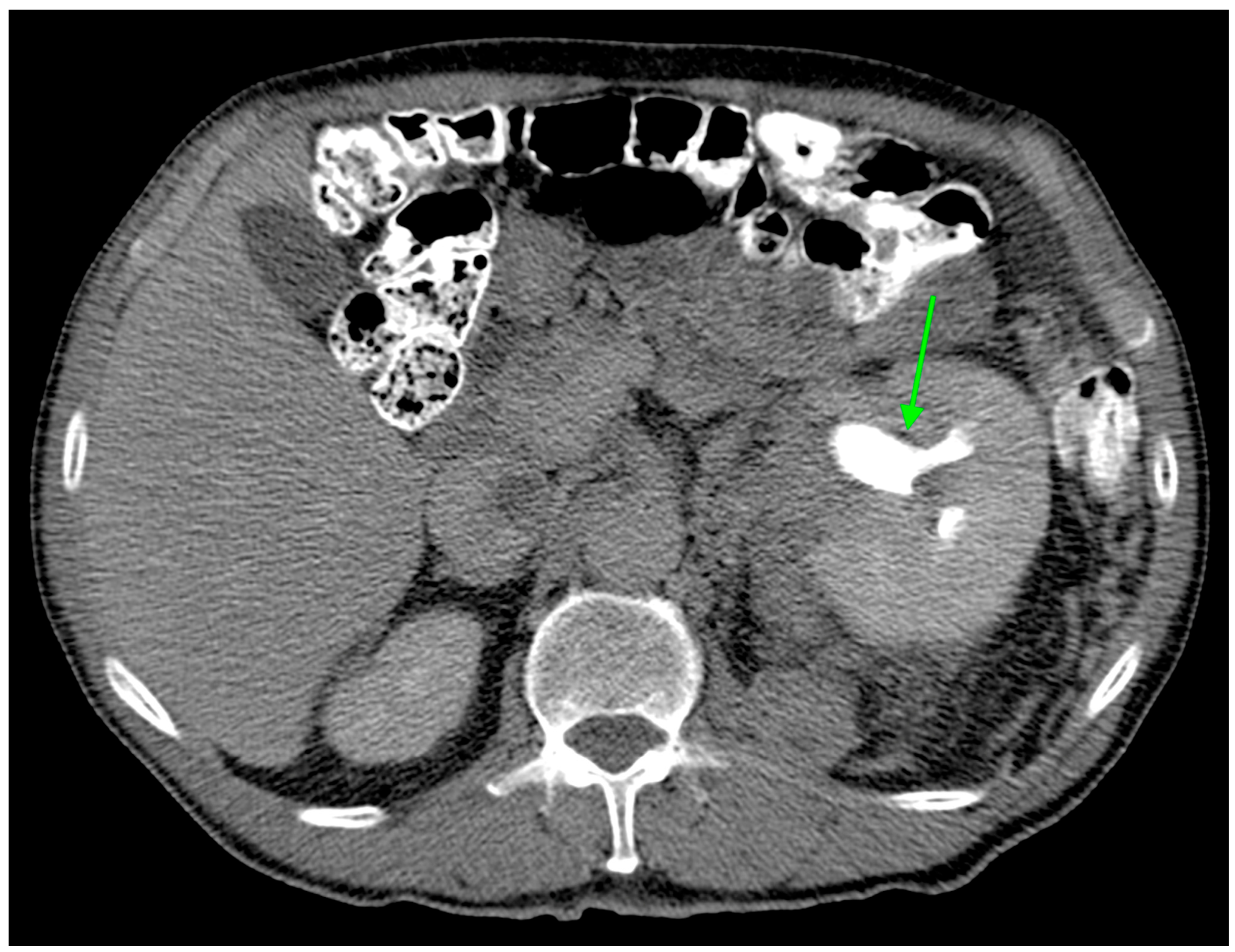
:1. Introduction
2. Materials and Methods
2.1. The Cancer Genome Atlas
2.2. Imaging Features
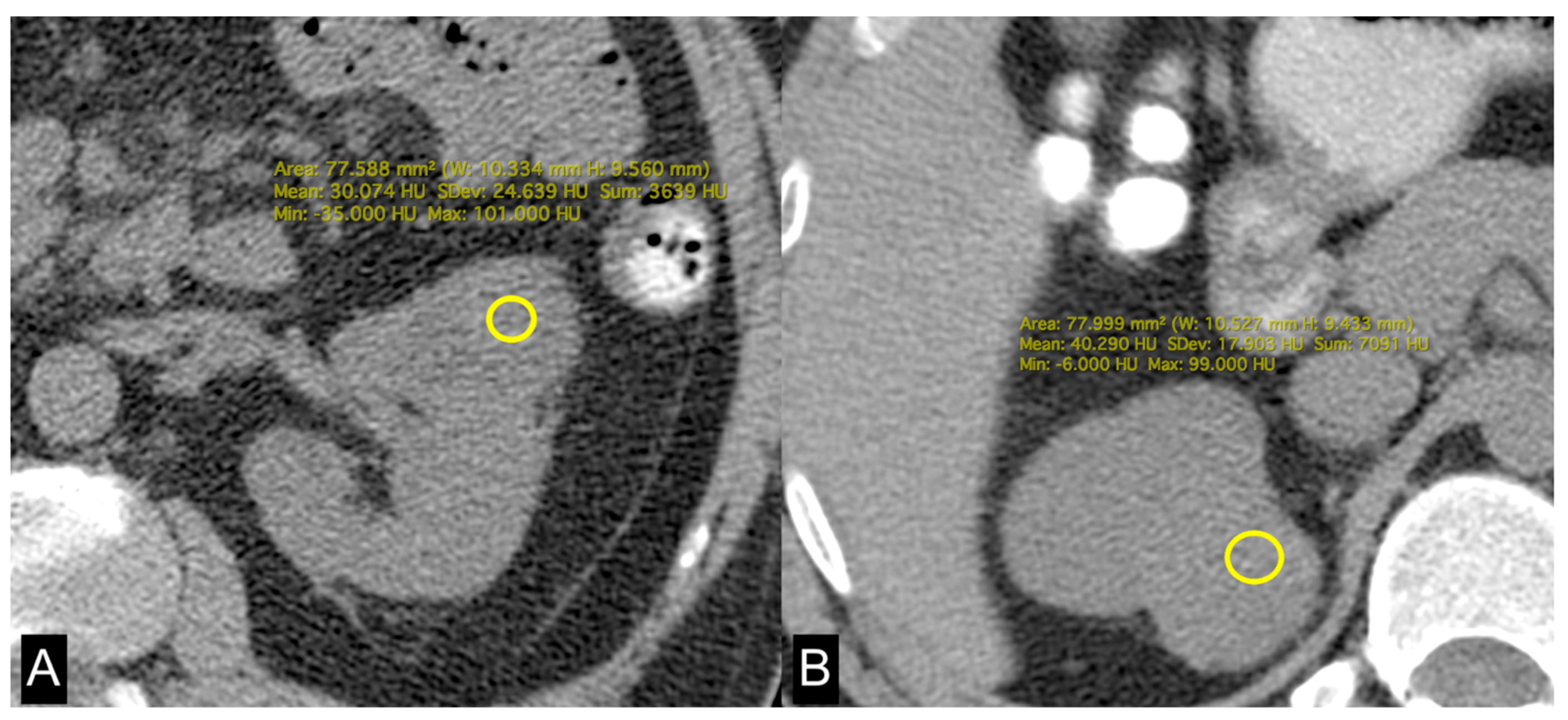
2.3. Lipid Metabolism Imaging Features
2.4. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alessandrino, F.; Krajewski, K.M.; Shinagare, A.B. Update on radiogenomics of clear cell renal cell carcinoma. Eur. Urol. Focus 2016, 2, 572–573. [Google Scholar] [CrossRef] [PubMed]
- Pinker, K.; Shitano, F.; Sala, E.; Do, R.K.; Young, R.J.; Wibmer, A.G.; Hricak, H.; Sutton, E.J.; Morris, E.A. Background, current role, and potential applications of radiogenomics. J. Magn. Reson. Imaging 2018, 47, 604–620. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Research Network. Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 2012, 499, 43–49. [Google Scholar]
- Akin, O.; Elnajjar, P.; Heller, M.; Jarosz, R.; Erickson, B.J.; Kirk, S.; Lee, Y.; Linehan, M.W.; Gautam, R.; Vikram, R.; et al. The Cancer Genome Atlas Kidney Renal Clear Cell Carcinoma Collection (TCGA-KIRC) (Version 3) [Data set]. Cancer Imaging Arch. 2016. [Google Scholar] [CrossRef]
- Greco, F.; Mallio, C.A. Relationship between visceral adipose tissue and genetic mutations (VHL and KDM5C) in clear cell renal cell carcinoma. Radiol. Med. 2021, 126, 645–651. [Google Scholar] [CrossRef]
- Greco, F.; Tafuri, A.; Grasso, R.F.; Beomonte Zobel, B.; Mallio, C.A. Clinicopathological and Body Composition Analysis of VHL and TTN Gene Mutations in Clear Cell Renal Cell Carcinoma: An Exploratory Study. Appl. Sci. 2022, 12, 9502. [Google Scholar] [CrossRef]
- Jiang, H.P.; Serrero, G. Isolation and characterization of a full-length cDNA coding for an adipose differentiation-related protein. Proc. Natl. Acad. Sci. USA 1992, 89, 7856–7860. [Google Scholar] [CrossRef] [PubMed]
- Londos, C.; Brasaemle, D.L.; Schultz, C.J.; Segrest, J.P.; Kimmel, A.R. Perilipins, ADRP, and other proteins that associate with intracellular neutral lipid droplets in animal cells. Semin. Cell Dev. Biol. 1999, 10, 51–58. [Google Scholar] [CrossRef]
- Yao, M.; Tabuchi, H.; Nagashima, Y.; Baba, M.; Nakaigawa, N.; Ishiguro, H.; Hamada, K.; Inayama, Y.; Kishida, T.; Hattori, K.; et al. Gene expression analysis of renal carcinoma: Adipose differentiation-related protein as a potential diagnostic and prognostic biomarker for clear-cell renal carcinoma. J. Pathol. 2005, 205, 377–387. [Google Scholar] [CrossRef]
- Brasaemle, D.L.; Barber, T.; Wolins, N.E.; Serrero, G.; Blanchette-Mackie, E.J.; Londos, C. Adipose differentiation-related protein is an ubiquitously expressed lipid storage droplet-associated protein. J. Lipid. Res. 1997, 38, 2249–2263. [Google Scholar] [CrossRef]
- Saarikoski, S.T.; Rivera, S.P.; Hankinson, O. Mitogen-inducible gene 6 (MIG-6), adipophilin and tuftelin are inducible by hypoxia. FEBS Lett. 2002, 530, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Brugarolas, J. Molecular genetics of clear-cell renal cell carcinoma. J. Clin. Oncol. 2014, 32, 1968–1976. [Google Scholar] [CrossRef] [PubMed]
- Stebbins, C.E.; Kaelin, W.G., Jr.; Pavletich, N.P. Structure of the VHL-ElonginC–ElonginB complex: Implications for VHL tumor suppressor function. Science 1999, 284, 455–461. [Google Scholar] [CrossRef]
- Maxwell, P.H.; Wiesener, M.S.; Chang, G.W.; Clifford, S.C.; Vaux, E.C.; Cockman, M.E.; Wykoff, C.C.; Pugh, C.W.; Maher, E.R.; Ratcliffe, P.J. The tumor suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 1999, 399, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Kase, A.M.; George, D.J.; Ramalingam, S. Clear Cell Renal Cell Carcinoma: From Biology to Treatment. Cancers 2023, 15, 665. [Google Scholar] [CrossRef] [PubMed]
- Tomczak, K.; Czerwińska, P.; Wiznerowicz, M. The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge. Contemp. Oncol. 2015, 19, A68–A77. [Google Scholar] [CrossRef] [PubMed]
- CIP TCGA Radiology Initiative—The Cancer Imaging Archive (TCIA) Public Access—Cancer Imaging Archive Wiki. Available online: https://www.cancerimagingarchive.net/collection/tcga-kirc/ (accessed on 1 November 2019).
- Greco, F.; Panunzio, A.; Tafuri, A.; Bernetti, C.; Pagliarulo, V.; Beomonte Zobel, B.; Scardapane, A.; Mallio, C.A. CT-Based Radiogenomics of P4HA3 Expression in Clear Cell Renal Cell Carcinoma. Acad. Radiol. 2023, 31, 902–908. [Google Scholar] [CrossRef]
- Greco, F.; Panunzio, A.; Tafuri, A.; Bernetti, C.; Pagliarulo, V.; Beomonte Zobel, B.; Scardapane, A.; Mallio, C.A. Radiogenomic Features of GIMAP Family Genes in Clear Cell Renal Cell Carcinoma: An Observational Study on CT Images. Genes 2023, 14, 1832. [Google Scholar] [CrossRef] [PubMed]
- Greco, F.; Panunzio, A.; Bernetti, C.; Tafuri, A.; Beomonte Zobel, B.; Mallio, C.A. Exploring the ADAM12 Expression in Clear Cell Renal Cell Carcinoma: A Radiogenomic Analysis on CT Imaging. Acad. Radiol. 2024. [Google Scholar] [CrossRef]
- Noumura, Y.; Kamishima, T.; Sutherland, K.; Nishimura, H. Visceral adipose tissue area measurement at a single level: Can it represent visceral adipose tissue volume? Br. J. Radiol. 2017, 90, 20170253. [Google Scholar] [CrossRef]
- Greco, F.; Quarta, L.G.; Grasso, R.F.; Beomonte Zobel, B.; Mallio, C.A. Increased visceral adipose tissue in clear cell renal cell carcinoma with and without peritumoral collateral vessels. Br. J. Radiol. 2020, 93, 20200334. [Google Scholar] [CrossRef] [PubMed]
- de Cubas, A.A.; Rathmell, W.K. Epigenetic modifiers: Activities in renal cell carcinoma. Nat. Rev. Urol. 2018, 15, 599–614. [Google Scholar] [CrossRef] [PubMed]
- Fischer-Posovszky, P.; Wabitsch, M.; Hochberg, Z. Endocrinology of adipose tissue—An update. Horm. Metab. Res. 2007, 39, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Raucci, R.; Rusolo, F.; Sharma, A.; Colonna, G.; Castello, G.; Costantini, S. Functional and structural features of adipokine family. Cytokine 2013, 61, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Mazumder, S.; Higgins, P.J.; Samarakoon, R. Downstream Targets of VHL/HIF-α Signaling in Renal Clear Cell Carcinoma Progression: Mechanisms and Therapeutic Relevance. Cancers 2023, 15, 1316. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B.; Ackerman, D.; Sanchez, D.J.; Li, B.; Ochocki, J.D.; Grazioli, A.; Bobrovnikova-Marjon, E.; Diehl, J.A.; Keith, B.; Simon, M.C. HIF2α-Dependent Lipid Storage Promotes Endoplasmic Reticulum Homeostasis in Clear-Cell Renal Cell Carcinoma. Cancer Discov. 2015, 5, 652–667. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Lee, Y.J.; Yun, Z. Differentiation arrest by hypoxia. J. Biol. Chem. 2006, 281, 30678–30683. [Google Scholar] [CrossRef] [PubMed]
- Yun, Z.; Maecker, H.L.; Johnson, R.S.; Giaccia, A.J. Inhibition of PPARγ2 gene expression by the HIF-1-regulated gene DEC1/Stra13: A mechanism for regulation of adipogenesis by hypoxia. Dev. Cell. 2002, 2, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Gao, Z.; Yin, J.; He, Q. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am. J. Physiol. Endocrinol. Metab. 2007, 293, E1118–E1128. [Google Scholar] [CrossRef]
- Halberg, N.; Khan, T.; Trujillo, M.E.; Wernstedt-Asterholm, I.; Attie, A.D.; Sherwani, S.; Wang, Z.V.; Landskroner-Eiger, S.; Dineen, S.; Magalang, U.J.; et al. Hypoxia-inducible factor 1alpha induces fibrosis and insulin resistance in white adipose tissue. Mol. Cell. Biol. 2009, 29, 4467–4483. [Google Scholar] [CrossRef]
- Shimba, S.; Wada, T.; Hara, S.; Tezuka, M. EPAS1 promotes adipose differentiation in 3T3-L1 cells. J. Biol. Chem. 2004, 279, 40946–40953. [Google Scholar] [CrossRef] [PubMed]
- Novick, A.C.; Campbell, S.C. Renal tumors. In Campbell’s Urology, 8th ed.; Walsh, P.C., Retik, A.B., Vaughan, E.D., Jr., Wein, A.J., Eds.; Saunders: Philadelphia, PA, USA, 2002; pp. 2672–2817. [Google Scholar]
- Thoenes, W.; Störkel, S.; Rumpelt, H.J. Histopathology and classification of renal cell tumors (adenomas, oncocytomas and carcinomas). The basic cytological and histopathological elements and their use for diagnostics. Pathol. Res. Pract. 1986, 181, 125–143. [Google Scholar] [CrossRef] [PubMed]
- Yao, M.; Huang, Y.; Shioi, K.; Hattori, K.; Murakami, T.; Nakaigawa, N.; Kishida, T.; Nagashima, Y.; Kubota, Y. Expression of adipose differentiation-related protein: A predictor of cancer-specific survival in clear cell renal carcinoma. Clin. Cancer Res. 2007, 13, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Sung, D.J.; Yang, K.S.; Kim, K.A.; Yeom, S.K.; Sim, K.C.; Han, N.Y.; Park, B.J.; Kim, M.J.; Cho, S.B.; et al. Small (<4 cm) clear cell renal cell carcinoma: Correlation between CT findings and histologic grade. Abdom. Radiol. 2016, 41, 1160–1169. [Google Scholar]
- Chen, C.; Zhao, W.; Lu, X.; Ma, Y.; Zhang, P.; Wang, Z.; Cui, Z.; Xia, Q. AUP1 regulates lipid metabolism and induces lipid accumulation to accelerate the progression of renal clear cell carcinoma. Cancer Sci. 2022, 113, 2600–2615. [Google Scholar] [CrossRef] [PubMed]
- Klasson, T.D.; LaGory, E.L.; Zhao, H.; Huynh, S.K.; Papandreou, I.; Moon, E.J.; Giaccia, A.J. ACSL3 regulates lipid droplet biogenesis and ferroptosis sensitivity in clear cell renal cell carcinoma. Cancer Metab. 2022, 10, 14. [Google Scholar] [CrossRef]


| Characteristic | Overall n = 197 1 | ADFP Expression | p-Value 2 | |
|---|---|---|---|---|
| Yes n = 45 (22.8%) 1 | No n = 152 (77.2%) 1 | |||
| Clinical–pathological features | ||||
| Age (years) | 59 (51, 69) | 58 (53, 68) | 60 (50, 69) | 0.8 |
| Sex (Males) | 130 (66.0%) | 31 (68.9%) | 99 (65.1%) | 0.6 |
| Race/ethnicity (Caucasian) | 182 (91.5%) | 42 (93.3%) | 140 (92.1%) | 0.9 |
| History of cancer | 35 (17.8%) | 9 (20.0%) | 26 (17.1%) | 0.7 |
| Primary tumor size (mm) | 53 (38, 81) | 54 (45, 76) | 53 (37, 83) | 0.4 |
| Laterality (left) | 92 (46.7%) | 23 (51.1%) | 69 (45.4%) | 0.5 |
| Tumor grade (Fuhrman) | 0.08 | |||
| Low-grade (G1–2) | 79 (40.1%) | 13 (28.9%) | 66 (43.4%) | |
| High-grade (G3–4) | 118 (59.9%) | 32 (71.1%) | 86 (56.6%) | |
| Tumor stage | 0.5 | |||
| Stage I | 103 (52.3%) | 22 (48.9%) | 81 (53.3%) | |
| Stage II | 18 (9.1%) | 2 (4.4%) | 16 (10.5%) | |
| Stage III | 49 (24.9%) | 14 (31.1%) | 35 (23.0%) | |
| Stage IV | 27 (13.7%) | 7 (15.6%) | 20 (13.2%) | |
| CT-based features | ||||
| Collateral vascular supply | 111 (57.5%) | 28 (63.6%) | 83 (55.3%) | 0.3 |
| Tumor margins | 0.5 | |||
| Ill defined | 69 (35.0%) | 14 (31.1%) | 55 (36.2%) | |
| Well-defined | 128 (65.0%) | 31 (68.9%) | 97 (63.8%) | |
| Tumor composition | 0.5 | |||
| Solid | 183 (92.9%) | 41 (91.1%) | 142 (93.4%) | |
| Cystic | 14 (7.1) | 4 (8.9%) | 10 (6.6%) | |
| Tumor necrosis | 0.13 | |||
| 0% | 12 (6.0%) | 5 (11.1%) | 7 (4.6%) | |
| 1–33% | 117 (59.4%) | 29 (64.4%) | 88 (57.9%) | |
| 34–66% | 47 (23.9%) | 6 (13.3%) | 41 (27.0%) | |
| >66% | 21 (10.7%) | 5 (11.2%) | 16 (10.5%) | |
| Tumor growth pattern | 0.3 | |||
| Endophytic | 13 (6.6%) | 1 (2.2%) | 12 (7.9%) | |
| Exophytic < 50% | 59 (29.9%) | 17 (37.8%) | 92 (60.5%) | |
| Exophytic ≥ 50% | 125 (63.5%) | 27 (60.0%) | 48 (31.6%) | |
| Calcifications | 39 (19.9%) | 10 (22.2%) | 29 (19.2%) | 0.7 |
| Signs of infiltration | 5 (2.5%) | 2 (4.4%) | 3 (2.1%) | 0.3 |
| Hydronephrosis | 6 (3.0%) | 4 (8.9%) | 2 (1.3%) | 0.025 |
| Thrombosis or infiltration of renal artery | 4 (2.0%) | 0 (0%) | 4 (2.6%) | 0.6 |
| Thrombosis or infiltration of renal vein | 15 (7.6%) | 3 (6.6%) | 12 (7.8%) | 0.9 |
| Collecting system invasion | 61 (31.0%) | 15 (33.3%) | 46 (30.3%) | 0.7 |
| Perinephric fat stranding | 103 (53.9%) | 24 (55.8%) | 79 (53.4%) | 0.8 |
| Gerota’s fascia thickening | 74 (37.6%) | 13 (29.5%) | 61 (41.5%) | 0.2 |
| Intralesional hemorrhage | 5 (2.5%) | 1 (2.2%) | 4 (2.6%) | 0.9 |
| No ADFP Expression (n = 152) | |||
| Low-grade (G1–2) n = 66 (43.4%) 1 | High-grade (G3–4) n = 86 (56.6%) 1 | p-value 2 | |
| VAT (cm2) | 213 (105, 299) | 196 (107, 245) | 0.6 |
| SAT (cm2) | 187 (141, 278) | 195 (148, 274) | 0.9 |
| TAT (cm2) | 430 (274, 530) | 381 (288, 506) | 0.6 |
| HU | 34 (27, 37) | 36 (32, 42) | 0.021 |
| ADFP Expression (n = 45) | |||
| Low-grade (G1–2) n = 13 (29%) 1 | High-grade (G3–4) n = 32 (71%) 1 | p-value 2 | |
| VAT (cm2) | 273 (225, 343) | 159 (95, 240) | 0.003 |
| SAT (cm2) | 226 (159, 419) | 158 (112, 228) | 0.045 |
| TAT (cm2) | 486 (423, 733) | 333 (200, 442) | 0.004 |
| HU | 30 (24, 32) | 37 (33, 40) | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Greco, F.; Panunzio, A.; Bernetti, C.; Tafuri, A.; Beomonte Zobel, B.; Mallio, C.A. The Radiogenomic Landscape of Clear Cell Renal Cell Carcinoma: Insights into Lipid Metabolism through Evaluation of ADFP Expression. Diagnostics 2024, 14, 1667. https://doi.org/10.3390/diagnostics14151667
Greco F, Panunzio A, Bernetti C, Tafuri A, Beomonte Zobel B, Mallio CA. The Radiogenomic Landscape of Clear Cell Renal Cell Carcinoma: Insights into Lipid Metabolism through Evaluation of ADFP Expression. Diagnostics. 2024; 14(15):1667. https://doi.org/10.3390/diagnostics14151667
Chicago/Turabian StyleGreco, Federico, Andrea Panunzio, Caterina Bernetti, Alessandro Tafuri, Bruno Beomonte Zobel, and Carlo Augusto Mallio. 2024. "The Radiogenomic Landscape of Clear Cell Renal Cell Carcinoma: Insights into Lipid Metabolism through Evaluation of ADFP Expression" Diagnostics 14, no. 15: 1667. https://doi.org/10.3390/diagnostics14151667






