Parathyroid Adenoma Detected in 68Ga-PSMA PET/CT but Not in the Dedicated Imaging Modalities
Abstract
1. Introduction
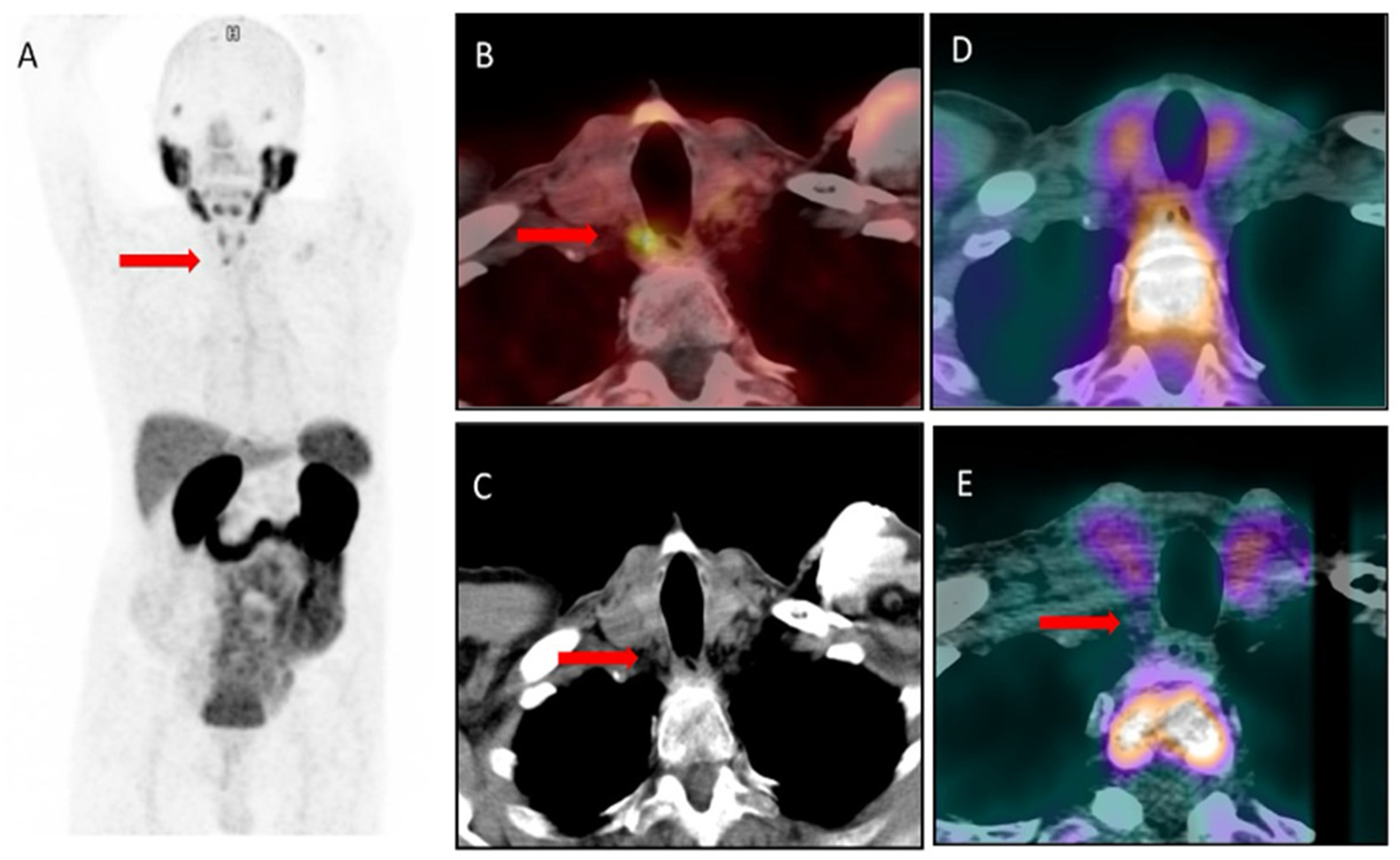
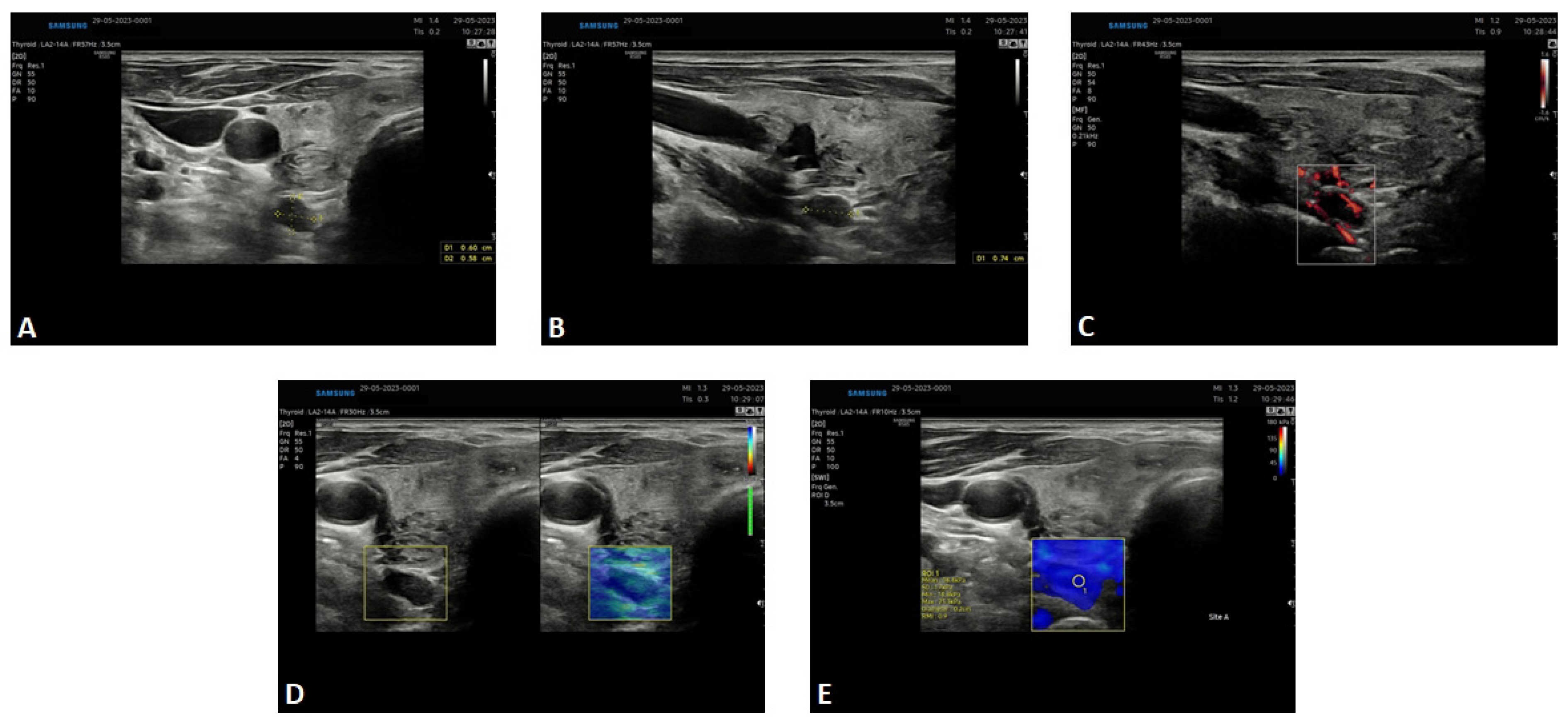
2. Results—Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Walker, M.D.; Silverberg, S.J. Primary hyperparathyroidism. Nat. Rev. Endocrinol. 2017, 14, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Bromińska, B.; Milewska, E.; Szczepanek-Parulska, E.; Czepczyński, R.; Ruchała, M. Diagnostic workup of a patient with severe hypercalcemia and a history of malignancy. Pol. Arch. Intern. Med. 2021, 131, 727–729. [Google Scholar] [CrossRef] [PubMed]
- Petranović Ovčariček, P.; Giovanella, L.; Carrió Gasset, I.; Hindié, E.; Huellner, M.W.; Luster, M.; Piccardo, A.; Weber, T.; Talbot, J.N.; Verburg, F.A. The EANM practice guidelines for parathyroid imaging. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2801–2822. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazurek, A.; Dziuk, M.; Witkowska-Patena, E.; Chudzinski, W.; Piszczek, S.; Gizewska, A.; Saracyn, M. The utility of 18F-fluorocholine PET/CT in the imaging of parathyroid adenomas. Endokrynol. Pol. 2022, 73, 43–48. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, D.S.; Su, S.L.; Bacich, D.J.; Horiguchi, Y.; Luo, Y.; Powell, C.T.; Zandvliet, D.; Russell, P.J.; Molloy, P.L.; Nowak, N.J.; et al. Mapping, genomic organization and promoter analysis of the human prostate-specific membrane antigen gene. Biochim. Biophys. Acta 1998, 1443, 113–127. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, D.S.; Bacich, D.J.; Huang, S.S.; Heston, W.D.W. A Perspective on the Evolving Story of PSMA Biology, PSMA-Based Imaging, and Endoradiotherapeutic Strategies. J. Nucl. Med. 2018, 59, 1007–1013. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ceci, F.; Oprea-Lager, D.E.; Emmett, L.; Adam, J.A.; Bomanji, J.; Czernin, J.; Eiber, M.; Haberkorn, U.; Hofman, M.S.; Hope, T.A.; et al. E-PSMA: The EANM standardized reporting guidelines v1.0 for PSMA-PET. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1626–1638. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chang, S.S.; Reuter, V.E.; Heston, W.D.; Bander, N.H.; Grauer, L.S.; Gaudin, P.B. Five different anti-prostate-specific membrane antigen (PSMA) antibodies confirm PSMA expression in tumor-associated neovasculature. Cancer Res. 1999, 59, 3192–3198. [Google Scholar] [PubMed]
- Grant, C.L.; Caromile, L.A.; Ho, V.; Durrani, K.; Rahman, M.M.; Claffey, K.P.; Fong, G.H.; Shapiro, L.H. Prostate specific membrane antigen (PSMA) regulates angiogenesis independently of VEGF during ocular neovascularization. PLoS ONE 2012, 7, e41285, Erratum in PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Galiza Barbosa, F.; Queiroz, M.A.; Nunes, R.F.; Costa, L.B.; Zaniboni, E.C.; Marin, J.F.G.; Cerri, G.G.; Buchpiguel, C.A. Nonprostatic diseases on PSMA PET imaging: A spectrum of benign and malignant findings. Cancer Imaging 2020, 20, 23. [Google Scholar] [CrossRef] [PubMed]
- Kunikowska, J.; Czepczyński, R.; Pawlak, D.; Koziara, H.; Pełka, K.; Królicki, L. Expression of glutamate carboxypeptidase II in the glial tumor recurrence evaluated in vivo using radionuclide imaging. Sci. Rep. 2022, 12, 652. [Google Scholar] [CrossRef] [PubMed]
- Conway, R.E.; Rojas, C.; Alt, J.; Nováková, Z.; Richardson, S.M.; Rodrick, T.C.; Fuentes, J.L.; Richardson, N.H.; Attalla, J.; Stewart, S.; et al. Prostate-specific membrane antigen (PSMA)-mediated laminin proteolysis generates a pro-angiogenic peptide. Angiogenesis 2016, 19, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Dassie, J.P.; Liu, X.Y.; Thomas, G.S.; Whitaker, R.M.; Thiel, K.W.; Stockdale, K.R.; Meyerholz, D.K.; McCaffrey, A.P.; McNamara, J.O., II; Giangrande, P.H. Systemic administration of optimized aptamer-siRNA chimeras promotes regression of PSMA-expressing tumors. Nat. Biotechnol. 2009, 27, 839–846. [Google Scholar] [CrossRef] [PubMed]
- Andryszak, N.; Świniuch, D.; Wójcik, E.; Ramlau, R.; Ruchała, M.; Czepczyński, R. Head-to-Head Comparison of [18F]PSMA-1007 and [18F]FDG PET/CT in Patients with Triple-Negative Breast Cancer. Cancers 2024, 16, 667. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Broos, W.A.; van der Zant, F.M.; Knol, R.J. Incidental Detection of Parathyroid Adenoma on 18F-PSMA PET/CT. Clin. Nucl. Med. 2023, 48, 1082–1083. [Google Scholar] [CrossRef] [PubMed]
- Piek, M.W.; de Vries, L.H.; Donswijk, M.L.; de Keizer, B.; de Boer, J.P.; Lodewijk, L.; van Leeuwaarde, R.S.; Vriens, M.R.; Hartemink, K.J.; van der Ploeg, I.M.C. Retrospective analysis of PSMA PET/CT thyroid incidental uptake in adults: Incidence, diagnosis, and treatment/outcome in a tertiary cancer referral center and University Medical Center. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2392–2400. [Google Scholar] [CrossRef] [PubMed]
- Pfob, C.H.; Karimov, I.; Jesinghaus, M.; Novotny, A.; Weber, W.A.; Eiber, M.; Feuerecker, B. Pitfalls in Ga-68-PSMA-PET/CT: Incidental finding of parathyroid adenoma. Eur. J. Nucl. Med. Mol. Imaging 2018, 46, 1041. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, Y.; Kuratsukuri, K.; Landas, S.; Imaida, K.; Rovito, P.M.; Wang, C.Y.; Haas, G.P. Expression of prostate-specific membrane antigen in normal and malignant human tissues. World J. Surg. 2006, 30, 628–636. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cieślewicz, M.; Andryszak, N.; Pełka, K.; Szczepanek-Parulska, E.; Ruchała, M.; Kunikowska, J.; Czepczyński, R. Parathyroid Adenoma Detected in 68Ga-PSMA PET/CT but Not in the Dedicated Imaging Modalities. Diagnostics 2024, 14, 1690. https://doi.org/10.3390/diagnostics14151690
Cieślewicz M, Andryszak N, Pełka K, Szczepanek-Parulska E, Ruchała M, Kunikowska J, Czepczyński R. Parathyroid Adenoma Detected in 68Ga-PSMA PET/CT but Not in the Dedicated Imaging Modalities. Diagnostics. 2024; 14(15):1690. https://doi.org/10.3390/diagnostics14151690
Chicago/Turabian StyleCieślewicz, Maja, Natalia Andryszak, Kacper Pełka, Ewelina Szczepanek-Parulska, Marek Ruchała, Jolanta Kunikowska, and Rafał Czepczyński. 2024. "Parathyroid Adenoma Detected in 68Ga-PSMA PET/CT but Not in the Dedicated Imaging Modalities" Diagnostics 14, no. 15: 1690. https://doi.org/10.3390/diagnostics14151690
APA StyleCieślewicz, M., Andryszak, N., Pełka, K., Szczepanek-Parulska, E., Ruchała, M., Kunikowska, J., & Czepczyński, R. (2024). Parathyroid Adenoma Detected in 68Ga-PSMA PET/CT but Not in the Dedicated Imaging Modalities. Diagnostics, 14(15), 1690. https://doi.org/10.3390/diagnostics14151690




