Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
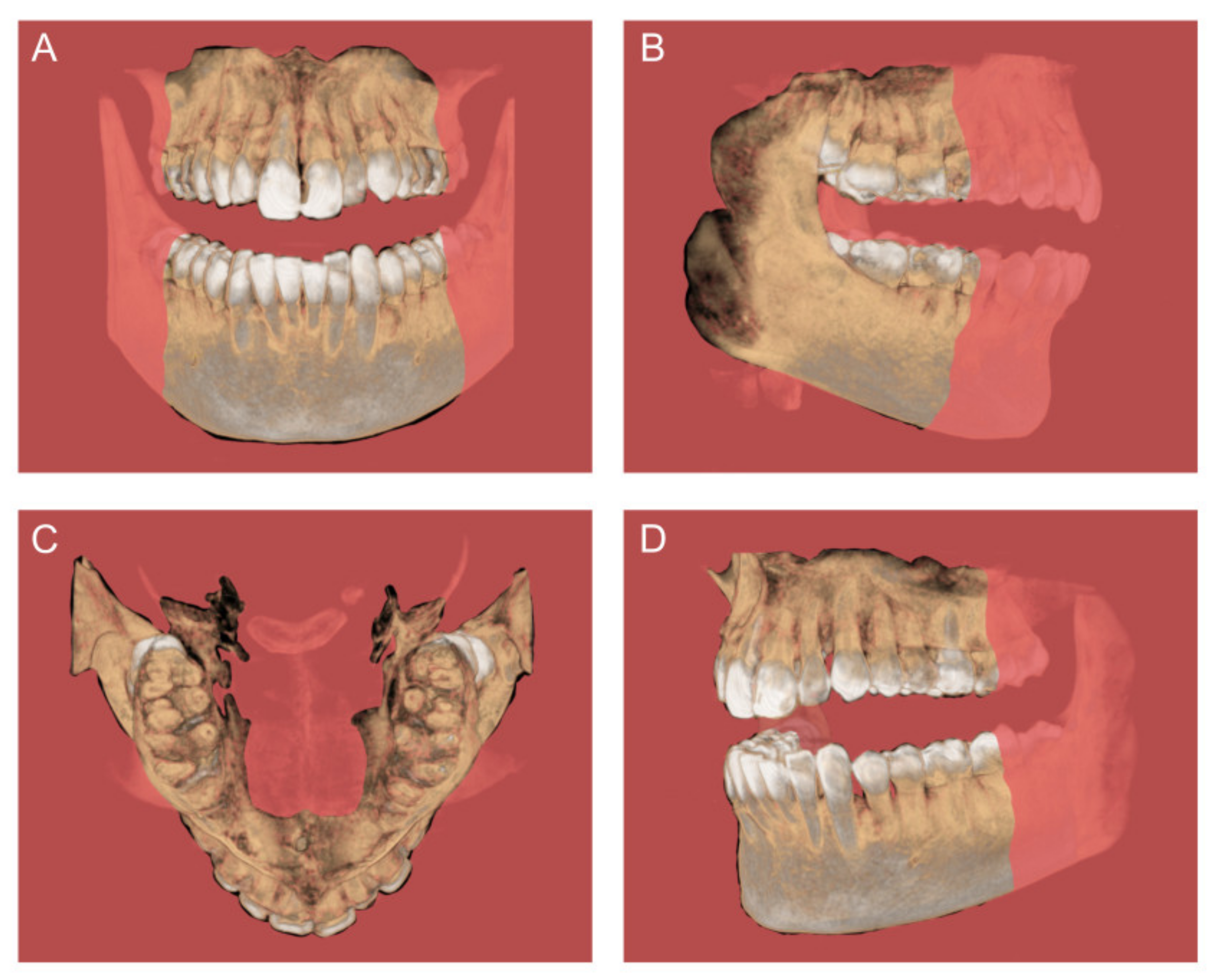
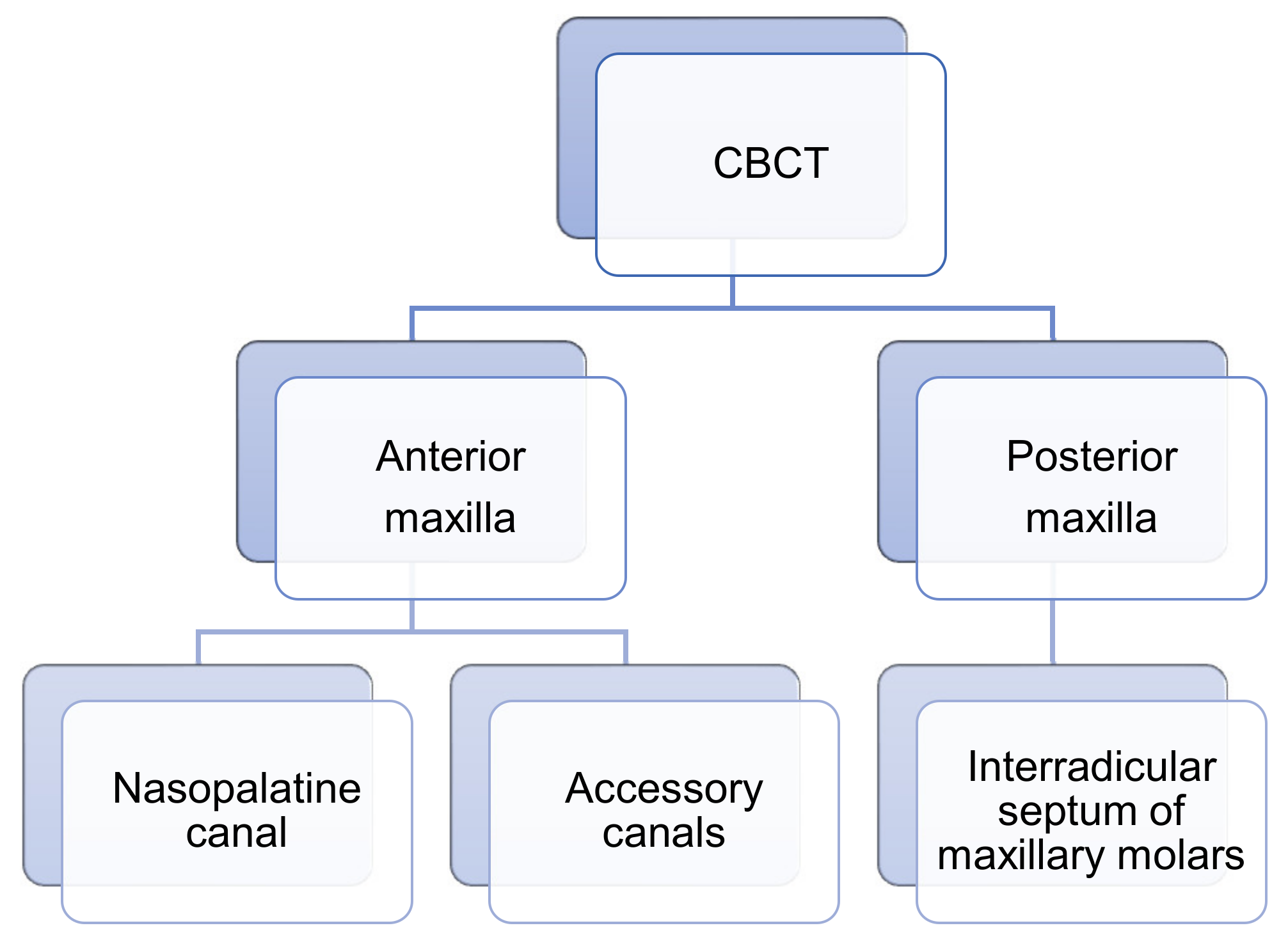
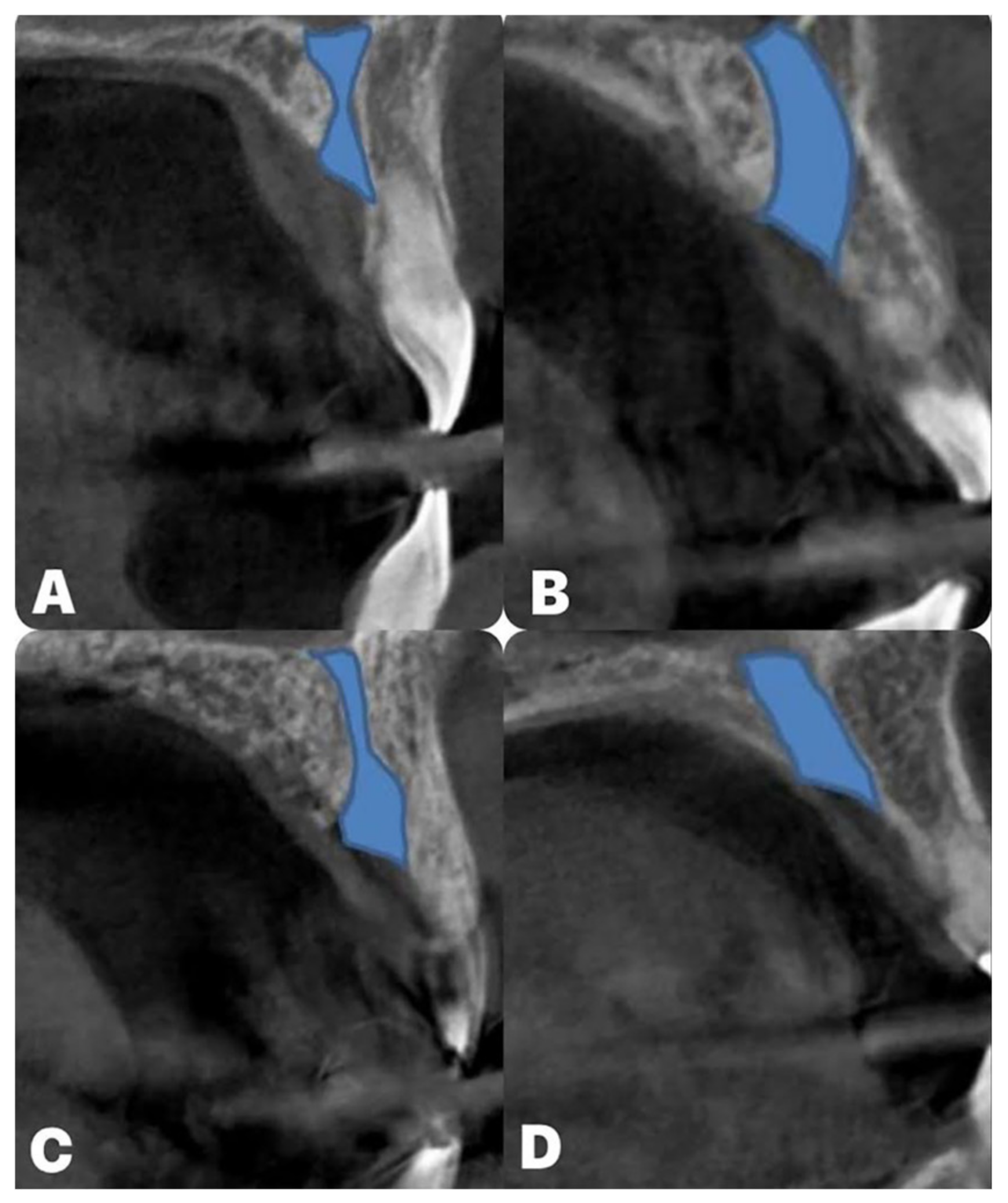
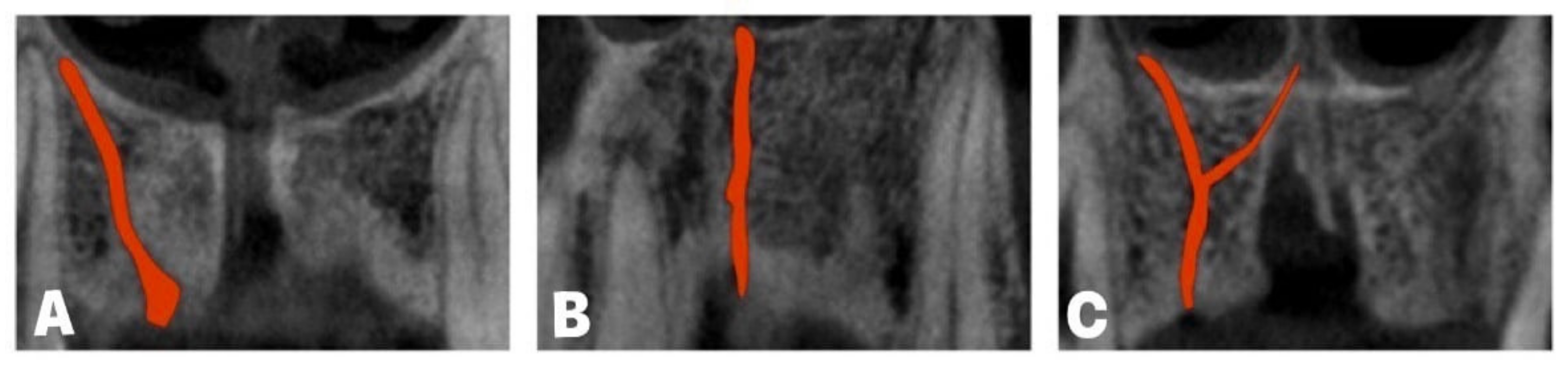
3. Benefits of CBCT Usage in Planning the Interventions in the Anterior Maxilla Region
4. Benefits of CBCT Usage in Planning the Interventions in the Maxillary Molar Region
5. Discussion
6. Conclusions
- The possibility for immediate implant placement may be affected by the NPC shape in the anterior maxilla, while the presence of ACs, in general, may increase the incidence of immediate implant placement complications;
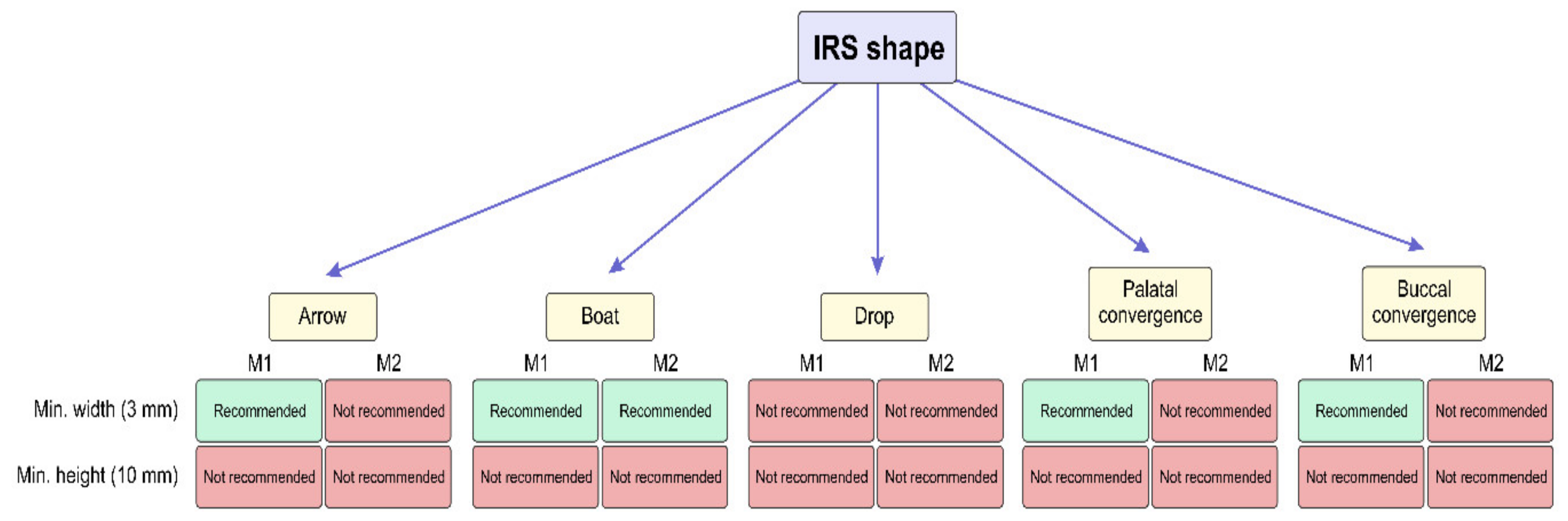
- The variations in IRS characteristics may be considered important criteria for choosing the implant properties required for successful immediate implant placement.
7. Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CBCT | Cone beam computed tomography |
| NPC | Nasopalatine canal |
| ACs | Accessory canals |
| IRS | Interradicular septum |
References
- Von Arx, T.; Lozanoff, S. Clinical Oral Anatomy; Springer: Cham, Switzerland, 2017. [Google Scholar] [CrossRef]
- Scarfe, W.C.; Farman, A.G. What is cone-beam CT and how does it work? Dent. Clin. N. Am. 2008, 52, 707–730. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Shanavas, M.; Sidappa, A.; Kiran, M. Cone beam computed tomography—Know its secrets. J. Int. Oral Health 2015, 7, 64–68. [Google Scholar] [PubMed]
- Hashimoto, K.; Kawashima, S.; Araki, M.; Iwai, K.; Sawada, K.; Akiyama, Y. Comparison of image performance between cone-beam computed tomography for dental use and four-row multidetector helical CT. J. Oral Sci. 2006, 48, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Shahbazian, M.; Vandewoude, C.; Wyatt, J.; Jacobs, R. Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin. Oral Investig. 2014, 18, 293–300. [Google Scholar] [CrossRef] [PubMed]
- DeVos, W.; Casselman, J.; Swennen, G.R. Cone beam computerized tomography (CBCT) imaging of oral and maxillofacial region: A systemic review of literature. Int. J. Oral Maxillofac. Surg. 2009, 38, 609–625. [Google Scholar] [CrossRef] [PubMed]
- Orhan, K.; KusakciSeker, B.; Aksoy, S.; Bayindir, H.; Berberoğlu, A.; Seker, E. Cone beam CT evaluation of maxillary sinus septa prevalence, height, location and morphology in children and an adult population. Med. Princ. Pract. 2013, 22, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Puigpelat, O.; Lázaro-Abdulkarim, A.; de Medrano-Reñé, J.M.; Gargallo-Albiol, J.; Cabratosa-Termes, J.; Hernández-Alfaro, F. Influence of Implant Position in Implant-Assisted Removable Partial Denture: A Three-Dimensional Finite Element Analysis. J. Prosthodont. 2019, 28, e675–e681. [Google Scholar] [CrossRef] [PubMed]
- Loubele, M.; Bogaerts, R.; Van Dijck, E.; Pauwels, R.; Vanheusden, S.; Suetens, P.; Marchal, G.; Sanderink, G.; Jacobs, R. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur. J. Radiol. 2009, 71, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Winter, A.A.; Pollack, A.S.; Frommer, H.H.; Koenig, L. Cone beam volumetric tomography vs. medical CT scanners. N. Y. State Dent. J. 2005, 71, 28–33. [Google Scholar]
- Von Arx, T.; Lozanoff, S.; Bornstein, M.M. Extraoral anatomy in CBCT—A literature review. Part 1: Nasoethmoidal region. Swiss Dent. J. 2019, 129, 804–815. [Google Scholar] [CrossRef] [PubMed]
- Hodez, C.; Griffaton-Taillandier, C.; Bensimon, I. Cone-beam imaging: Applications in ENT. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2011, 128, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Arnaut, A.; Milanovic, P.; Vasiljevic, M.; Jovicic, N.; Vojinovic, R.; Selakovic, D.; Rosic, G. The Shape of Nasopalatine Canal as a Determining Factor in Therapeutic Approach for Orthodontic Teeth Movement—A CBCT Study. Diagnostics 2021, 11, 2345. [Google Scholar] [CrossRef] [PubMed]
- Milanovic, P.; Selakovic, D.; Vasiljevic, M.; Jovicic, N.U.; Milovanović, D.; Vasovic, M.; Rosic, G. Morphological Characteristics of the Nasopalatine Canal and the Relationship with the Anterior Maxillary Bone—A Cone Beam Computed Tomography Study. Diagnostics 2021, 11, 915. [Google Scholar] [CrossRef] [PubMed]
- Bremke, M.; Leppek, R.; Werner, J.A. Die digitale Volumen tomographie in der HNO-Heilkunde [Digital volume tomography in ENT medicine]. HNO 2010, 58, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Tschopp, M.; Bornstein, M.M.; Sendi, P.; Jacobs, R.; Goldblum, D. Dacryocystography using cone beam CT in patients with lacrimal drainage system obstruction. Ophthalmic Plast. Reconstr. Surg. 2014, 30, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Gaêta-Araujo, H.; Alzoubi, T.; Vasconcelos, K.F.; Orhan, K.; Pauwels, R.; Casselman, J.W.; Jacobs, R. Cone beam computed tomography in dentomaxillofacial radiology: A two-decade overview. Dentomaxillofac. Radiol. 2020, 49, 20200145. [Google Scholar] [CrossRef] [PubMed]
- Dula, K.; Benic, G.I.; Bornstein, M.M.; Dagassan Berndt, D.; Filippi, A.; Hicklin, S.; Kissling-Jeger, F.; Luebbers, H.T.; Sculean, A.; Sequeira-Byron, P.; et al. SADMFR guidelines for the use of cone beam computed tomography/digital volume tomography. Swiss Dent. J. 2015, 125, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontology 2000 2016, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Alkanderi, A.; Al Sakka, Y.; Koticha, T.; Li, J.; Masood, F.; Suárez-López Del Amo, F. Incidence of nasopalatine canal perforation in relation to virtual implant placement: A cone beam computed tomography study. Clin. Implant Dent. Relat. Res. 2020, 22, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Garaicoa-Pazmino, C.; Suarez, F.; Monje, A.; Benavides, E.; Oh, T.J.; Wang, H.L. Incidence of implant buccal plate fenestration in the esthetic zone: A cone beam computed tomography study. Int. J. Oral Maxillofac. Implants 2014, 29, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Lo, L.J. Three-dimensional computer-assisted surgical simulation and intraoperative navigation in orthognathic surgery: A literature review. J. Formos. Med. Assoc. 2015, 114, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Adolphs, N.; Haberl, E.J.; Liu, W.; Keeve, E.; Menneking, H.; Hoffmeister, B. Virtual planning for craniomaxillofacial surgery—7 Years of experience. J. Cranio-Maxillofac. Surg. 2014, 42, e289–e295. [Google Scholar] [CrossRef] [PubMed]
- Zinser, M.J.; Mischkowski, R.A.; Dreiseidler, T.; Thamm, O.C.; Rothamel, D.; Zöller, J.E. Computer-assisted orthognathic surgery: Waferless maxillary positioning, versatility, and accuracy of an image-guided visualisation display. Br. J. Oral Maxillofac. Surg. 2013, 51, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 34. [Google Scholar] [CrossRef] [PubMed]
- Deporter, D.; EbrahimiDastgurdi, M.; Rahmati, A.; G Atenafu, E.; Ketabi, M. CBCT data relevant in treatment planning for immediate maxillary molar implant placement. J. Adv. Periodontol. Implant Dent. 2021, 2, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, H.J.; Eitner, S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J. Craniomaxillofac. Surg. 2007, 4–5, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, M.; Giri; Raja, R.; Subramonian; Karthik; Narendrakumar, R. Implant surgical guides: From the past to the present. J. Pharm. Bioallied Sci. 2013, 1, S98–S102. [Google Scholar] [CrossRef] [PubMed]
- Abdelhamid, A.; Omran, M.; Bakhshalian, N.; Tarnow, D.; Zadeh, H.H. An open randomized controlled clinical trial to evaluate ridge preservation and repair using SocketKAPTM and SocketKAGETM: Part 2—Three-dimensional alveolar bone volumetric analysis of CBCT imaging. Clin. Oral Implants Res. 2015, 27, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Gorla, L.F.; Spin-Neto, R.; Boos, F.B.; Pereira Rdos, S.; Garcia Junior, I.R.; Hochuli-Vieira, E. Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: A prospective, randomized, volumetric computed tomography study. Int. J. Oral Maxillofac. Surg. 2015, 44, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Markovic, A.; Misic, T.; Calvo-Guirado, J.L.; Delgado-Ruız, R.A.; Janjic, B.; Abboud, M. Two-center prospective, randomized, clinical, and radiographic study comparing osteotome sinus floor elevation with or without bone graft and simultaneous implant placement. Clin. Implant Dent. Relat. Res. 2016, 18, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Kuchler, U.; Chappuis, V.; Gruber, R.; Lang, N.P.; Salvi, G.E. Immediate implant placement with simultaneous guided bone regeneration in the esthetic zone: 10-year clinical and radiographic outcomes. Clin. Oral Implants Res. 2016, 27, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.T.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 186–215. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.M.; Jensen, O.T.; Pikos, M.A.; Malmquist, J.P. Vertical bone augmentation using recombinant bone morphogenetic protein, mineralized bone allograft, and titanium mesh: A retrospective cone beam computed tomography study. Int. J. Oral Maxillofac. Implants 2015, 30, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Spin-Neto, R.; Stavropoulos, A.; Coletti, F.L.; Pereira, L.A.; Marcantonio, E., Jr.; Wenzel, A. Remodeling of cortical and corticocancellous fresh-frozen allogenic block bone grafts—A radiographic and histomorphometric comparison to autologous bone grafts. Clin. Oral Implants Res. 2015, 26, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.A.; Kim, S.J.; Choi, Y.J.; Kim, K.-H.; Chung, C.J. Morphologic evaluation of the incisive canal and its proximity to the maxillary central incisors using computed tomography images. Angle Orthod. 2015, 86, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Gull, M.A.B.; Maqbool, S.; Mushtaq, M.; Ahmad, A. Evaluation of Morphologic Features and Proximity of Incisive Canal to the Maxillary Central Incisors Using Cone Beam Computed Tomography. IOSR J. Dent. Med. Sci. 2018, 17, 46–50. [Google Scholar]
- Bornstein, M.M.; Balsiger, R.; Sendi, P.; von Arx, T. Morphology of the nasopalatine canal and dental implant surgery: A radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin. Oral Implants Res. 2011, 22, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Lambrichts, I.; Liang, X.; Martens, W.; Mraiwa, N.; Adriaensens, P.; Gelan, J. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Lake, S.; Iwanaga, J.; Kikuta, S.; Oskouian, R.J.; Loukas, M.; Tubbs, R.S. The Incisive Canal: A Comprehensive Review. Cureus 2018, 10, e3069. [Google Scholar] [CrossRef] [PubMed]
- Keith, D.A. Phenomenon of mucous retention in the incisive canal. J. Oral Surg. 1979, 37, 832–834. [Google Scholar] [PubMed]
- Mardinger, O.; Namani-Sadan, N.; Chaushu, G.; Schwartz-Arad, D. Morphologic Changes of the Nasopalatine Canal Related to Dental Implantation: A Radiologic Study in Different Degrees of Absorbed Maxillae. J. Periodontol. 2008, 79, 1659–1662. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, M.; Matsunaga, S.; Odaka, K.; Oomine, Y.; Kasahara, M.; Yamamoto, M.; Abe, S. Three-dimensional analysis of incisive canals in human dentulous and edentulous maxillary bones. Int. J. Implant Dent. 2015, 1, 12. [Google Scholar] [CrossRef] [PubMed]
- Gil-Marques, B.; Sanchis-Gimeno, J.A.; Brizuela-Velasco, A.; Perez-Bermejo, M.; Larrazábal-Morón, C. Differences in the shape and direction-course of the nasopalatine canal among dentate, partially edentulous and completely edentulous subjects. Anat. Sci. Int. 2020, 95, 76–84. [Google Scholar] [CrossRef] [PubMed]
- De Lima, A.C.N.M.; Peniche, D.A.; Coutinho, T.M.C.; Guedes, F.R.; Visconti, M.A.; Risso, P.A. The nasopalatine canal and its relationship with the maxillary central incisors: A cone-beam computed tomography study. Res. Soc. Dev. 2021, 10, e351101522978. [Google Scholar] [CrossRef]
- Etoz, M.; Sisman, Y. Evaluation of the nasopalatine canal and variations with cone-beam computed tomography. Surg. Radiol. Anat. 2014, 36, 805–812. [Google Scholar] [CrossRef]
- Botermans, A.; Lidén, A.; de Carvalho Machado, V.; Chrcanovic, B.R. Immediate Implant Placement in the Maxillary Aesthetic Zone: A Cone Beam Computed Tomography Study. J. Clin. Med. 2021, 10, 5853. [Google Scholar] [CrossRef] [PubMed]
- Vasiljevic, M.; Milanovic, P.; Jovicic, N.; Vasovic, M.; Milovanovic, D.; Vojinovic, R.; Selakovic, D.; Rosic, G. Morphological and Morphometric Characteristics of Anterior Maxilla Accessory Canals and Relationship with Nasopalatine Canal Type-A CBCT Study. Diagnostics 2021, 11, 1510. [Google Scholar] [CrossRef] [PubMed]
- Baena-Caldas, G.; Rengifo-Miranda, H.; Heerera-Rubio, A.; Peckham, X.; Zúñiga, J. Frequency of canalissinuosus and its anatomic variations in cone beam computed tomography images. Int. J. Morphol. 2019, 37, 852–857. [Google Scholar] [CrossRef]
- Machado, V.C.; Chrcanovic, B.R.; Felippe, M.B.; Manhães Júnior, L.R.; de Carvalho, P.S. Assessment of accessory canals of the canalissinuosus: A study of 1000 cone beam computed tomography examinations. Int. J. Oral Maxillofac. Surg. 2016, 45, 1586–1591. [Google Scholar] [CrossRef] [PubMed]
- Von Arx, T.; Lozanoff, S.; Sendi, P.; Bornstein, M.M. Assessment of bone channels other than the nasopalatine canal in the anterior maxilla using limited cone beam computed tomography. Surg. Radiol. Anat. 2013, 35, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Tomrukçu, D.N.; Köse, T.E. Assesment of accessory branches of canalissinuosus on CBCT images. Med. Oral Patol. Oral Cir. Bucal. 2020, 25, e124–e130. [Google Scholar] [CrossRef] [PubMed]
- Wanzeler, A.M.; Marinho, C.G.; Alves Junior, S.M.; Manzi, F.R.; Tuji, F.M. Anatomical study of the canalissinuosus in 100 cone beam computed tomography examinations. Oral Maxillofac. Surg. 2015, 19, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Anatoly, A.; Sedov, Y.; Gvozdikova, E.; Mordanov, O.; Kruchinina, L.; Avanesov, K.; Vinogradova, A.; Golub, S.; Khaydar, D.; Hoang, N.G.; et al. Radiological and Morphometric Features of CanalisSinuosus in Russian Population: Cone-Beam Computed Tomography Study. Int. J. Dent. 2019, 2019, 2453469. [Google Scholar] [CrossRef] [PubMed]
- Manhães Júnior, L.R.; Villaça-Carvalho, M.F.; Moraes, M.E.; Lopes, S.L.; Silva, M.B.; Junqueira, J.L. Location and classification of Canalissinuosus for cone beam computed tomography: Avoiding misdiagnosis. Braz. Oral Res. 2016, 30, e49. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira-Santos, C.; Rubira-Bullen, I.R.; Monteiro, S.A.; León, J.E.; Jacobs, R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin. Oral Implants Res. 2013, 24, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.G.; Park, C.J. Ideal implant positioning in an anterior maxillary extraction socket by creating an apico-palatal guiding slot: A technical note. Int. J. Oral Maxillofac. Implants 2008, 23, 121–122. [Google Scholar] [PubMed]
- Greenstein, G.; Tarnow, D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J. Periodontol. 2006, 77, 1933–1943. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Narkhede, S.; Sonawane, S.; Gangurde, P. Evaluation of Patient’s Personal Reasons and Experience with Orthodontic Treatment. J. Int. Oral Health 2013, 5, 78–81. [Google Scholar] [PubMed]
- Chung, C.J.; Nguyen, T.; Lee, J.; Kim, K. Incisive canal remodelling following maximum anterior retraction reduces apical root resorption. Orthod. Craniofacial. Res. 2021, 24, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Pavlovic, Z.R.; Milanovic, P.; Vasiljevic, M.; Jovicic, N.; Arnaut, A.; Colic, D.; Petrovic, M.; Stevanovic, M.; Selakovic, D.; Rosic, G. Assessment of Maxillary Molars Interradicular Septum Morphological Characteristics as Criteria for Ideal Immediate Implant Placement—The Advantages of Cone Beam Computed Tomography Analysis. Diagnostics 2022, 12, 1010. [Google Scholar] [CrossRef] [PubMed]
- Milenkovic, J.; Vasiljevic, M.; Jovicic, N.; Milovanovic, D.; Selakovic, D.; Rosic, G. Criteria for the Classification of the Interradicular Septum Shape in Maxillary Molars with Clinical Importance for Prosthetic-Driven Immediate Implant Placement. Diagnostics 2022, 12, 1432. [Google Scholar] [CrossRef] [PubMed]
- Bleyan, S.; Gaspar, J.; Huwais, S.; Schwimer, C.; Mazor, Z.; Mendes, J.J.; Neiva, R. Molar Septum Expansion with Osseodensification for Immediate Implant Placement, Retrospective Multicenter Study with Up-to-5-Year Follow-Up, Introducing a New Molar Socket Classification. J. Funct. Biomater. 2021, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.B.; Tarnow, D.P. Classification of molar extraction sites for immediate dental implant placement: Technical note. Int. J. Oral Maxillofac. Implants 2013, 28, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Agostinelli, C.; Agostinelli, A.; Berardini, M.; Trisi, P. Anatomical and Radiologic Evaluation of the Dimensions of Upper Molar Alveoli. Implant Dent. 2018, 27, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Padhye, N.; Shirsekar, V. Tomographic evaluation of mandibular molar alveolar bone for immediate implant placement—A retrospective cross-sectional study. Clin. Oral Implants Res. 2019, 30, 265. [Google Scholar] [CrossRef]
- Nunes, L.S.; Bornstein, M.M.; Sendi, P.; Buser, D. Anatomical characteristics and dimensions of edentulous sites in the posterior maxillae of patients referred for implant therapy. Int. J. Periodontics Restor. Dent. 2013, 33, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Pai, U.Y.; Rodrigues, S.J.; Talreja, K.S.; Mundathaje, M. Osseodensification—A novel approach in implant dentistry. J. Indian Prosthodont. Soc. 2018, 18, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Alhayati, J.Z.; Al-Anee, A.M. Evaluation of crestal sinus floor elevations using versah burs with simultaneous implant placement, at residual bone height ≥2.0_<6.0 mm. A prospective clinical study. Oral Maxillofac. Surg. 2023, 27, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Demirkol, N.; Demirkol, M. The Diameter and Length Properties of Single Posterior Dental Implants: A Retrospective Study. Cumhur. Dent. J. 2019, 22, 276–282. [Google Scholar] [CrossRef]
- Thirunavakarasu, R.; Arun, M.; Abhinav, R.P.; Ganesh, B.S. Commonly Used Implant Dimensions in the Posterior Maxilla—A Retrospective Study. J. Long-Term Eff. Med. Implants 2022, 32, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Ghoncheh, Z.; Zade, B.M.; Kharazifard, M.J. Root Morphology of the Maxillary First and Second Molars in an Iranian Population Using Cone Beam Computed Tomography. J. Dent. 2017, 14, 115–122. [Google Scholar]
- Wang, H.M.; Shen, J.W.; Yu, M.F.; Chen, X.Y.; Jiang, Q.H.; He, F.M. Analysis of facial bone wall dimensions and sagittal root position in the maxillary esthetic zone: A retrospective study using cone beam computed tomography. Int. J. Oral Maxillofac. Implants 2014, 29, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, Y.; Obama, T. Dental cone beam computed tomography analyses of postoperative labial bone thickness in maxillary anterior implants: Comparing immediate and delayed implant placement. Int. J. Periodontics Restor. Dent. 2011, 31, 215–225. [Google Scholar]
- Grunder, U.; Gracis, S.; Capelli, M. Influence of the 3-D bone-to-implant relationship on esthetics. Int. J. Periodontics Restor. Dent. 2005, 25, 113–119. [Google Scholar]
- Zhan, W.; Skrypczak, A.; Weltman, R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health 2015, 15, 65. [Google Scholar]
- Safi, Y.; Moshfeghi, M.; Rahimian, S.; Kheirkhahi, M.; Manouchehri, M.E. Assessment of Nasopalatine Canal Anatomic Variations Using Cone Beam Computed Tomography in a Group of Iranian Population. Iran. J. Radiol. 2017, 14, e13480. [Google Scholar] [CrossRef]
- Bahşi, I.; Orhan, M.; Kervancıoğlu, P.; Yalçın, E.D.; Aktan, A.M. Anatomical evaluation of nasopalatine canal on cone beam computed tomography images. Folia. Morphol. 2019, 78, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Güncü, G.N.; Yıldırım, Y.D.; Yılmaz, H.G.; Galindo-Moreno, P.; Velasco-Torres, M.; Al-Hezaimi, K.; Al-Shawaf, R.; Karabulut, E.; Wang, H.L.; Tözüm, T.F. Is there a gender difference in anatomic features of incisive canal and maxillary environmental bone? Clin. Oral Implants Res. 2013, 24, 1023–1026. [Google Scholar] [CrossRef] [PubMed]
- Jornet, P.L.; Boix, P.P.; Perez, A.S.; Boracchia, A. Morphological Characterization of the Anterior Palatine Region Using Cone Beam Computed Tomography. Clin. Implant Dent. Relat. Res. 2014, 17, 459–464. [Google Scholar]
- Chen, K.; Li, Z.; Liu, X.; Liu, Q.; Chen, Z.; Sun, Y.; Chen, Z.; Huang, B. Immediate Implant Placement with Buccal Bone Augmentation in the Anterior Maxilla with Thin Buccal Plate: A One-Year Follow-Up Case Series. J. Prosthodont. 2021, 30, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Bodereau, E.F.; Flores, V.Y.; Naldini, P.; Torassa, D.; Tortolini, P. Clinical Evaluation of the Nasopalatine Canal in Implant-Prosthetic Treatment: A Pilot Study. Dent. J. 2020, 8, 30. [Google Scholar] [CrossRef]
- Scher, E.L. Use of the incisive canal as a recipient site for root form implants: Preliminary clinical reports. Implant Dent. 1994, 1, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Singhal, M.K.; Dandriyal, R.; Aggarwal, A.; Agarwal, A.; Yadav, S.; Baranwal, P. Implant Placement into the Nasopalatine Foramen: Considerations from Anatomical and Surgical Point of View. Ann. Maxillofac. Surg. 2018, 2, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Gargallo-Albiol, J.; Barootchi, S.; Marqués-Guasch, J.; Wang, H.L. Fully Guided Versus Half-Guided and Freehand Implant Placement: Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implants 2020, 35, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- Yeap, C.W.; Danh, D.; Chan, J.; Parashos, P. Examination of canalis sinuosus using cone beam computed tomography in an Australian population. Aust. Dent. J. 2022, 67, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Milanovic, P.; Vasiljevic, M. Gender Differences in the Morphological Characteristics of the Nasopalatine Canal and the Anterior Maxillary Bone—CBCT Study. Serb. J. Exp. Clin. Res. 2021. [CrossRef]
- Rosano, G.; Testori, T.; Clauser, T.; Massimo Del Fabbro, M. Management of a neurological lesion involving Canalis Sinuosus: A case report. Clin. Implant Dent. Relat. Res. 2021, 23, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Kaur, S. Evaluation of Post-operative Complication Rate of Le Fort I Osteotomy: A Retrospective and Prospective Study. J. Maxillofac. Oral Surg. 2014, 13, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.; Hu, W.; Meng, H. Relationship of central incisor implant placement to the ridge configuration anterior to the nasopalatine canal in dentate and partially edentulous individuals: A comparative study. PeerJ 2015, 3, e1315. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCrea, S.J.J. Aberrations Causing Neurovascular Damage in the Anterior Maxilla during Dental Implant Placement. Case Rep. Dent. 2017, 2017, 5969643. [Google Scholar] [CrossRef] [PubMed]
- Shelley, A.; Tinning, J.; Yates, J.; Horner, K. Potential neurovascular damage as a result of dental implant placement in the anterior maxilla. Br. Dent. J. 2019, 226, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Salehinejad, J.; Saghafi, S.; Zare-Mahmoodabadi, R.; Ghazi, N.; Kermani, H. Glandular odontogenic cyst of the posterior maxilla. Arch. Iran Med. 2011, 14, 416–418. [Google Scholar] [PubMed]
- Khojasteh, A.; Nazeman, P.; Tolstunov, L. Tuberosity-alveolar block as a donor site for localized augmentation of the maxilla: A retrospective clinical study. Br. J. Oral Maxillofac. Surg. 2016, 54, 950–955. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.A.; Wong, C.W.; Allen, J.C., Jr. Maxillary third molar: Patterns of impaction and their relation to oroantral perforation. J. Oral Maxillofac. Surg. 2012, 70, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, J.; Blume, M.; Korzinskas, T.; Ghanaati, S.; Sader, R.A. Short implants in the posterior maxilla to avoid sinus augmentation procedure: 5-year results from a retrospective cohort study. Int. J. Implant. Dent. 2019, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.K.; Fung, S.C.; Li, T.; Samman, N. Posterior maxillary anatomy: Implications for Le Fort I osteotomy. Int. J. Oral Maxillofac. Surg. 1998, 27, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Arul, A.S.; Verma, S.; Arul, A.S.; Verma, R. Infiltrative odontogenic myxoma of the posterior maxilla: Report of a case. J. Nat. Sci. Biol. Med. 2013, 4, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Elmasry, M.; Hammerle, C.H. Novel digital imaging techniques to assess the outcome in oral rehabilitation with dental implants: A narrative review. Clin. Oral Implants Res. 2015, 26, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Whyte, A.; Boeddinghaus, R. The maxillary sinus: Physiology, development and imaging anatomy. Dentomaxillofac. Radiol. 2019, 48, 20190205. [Google Scholar] [CrossRef] [PubMed]
- Stanley, J.N. Wheeler’s dental anatomy. In Physiology and Occlusion, 9th ed.; Saunders Elsevier: St. Louis, MO, USA, 2010. [Google Scholar]
- Rodriguez-Tizcareño, M.H.; Bravo-Flores, C. Anatomically guided implant site preparation technique at molar sites. Implant Dent. 2009, 5, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Prosper, L.; Crespi, R.; Valenti, E.; Capparé, P.; Gherlone, E. Five-year follow-up of wide-diameter implants placed in fresh molar extraction sockets in the mandible: Immediate versus delayed loading. Int. J. Oral Maxillofac. Implants 2010, 25, 607–612. [Google Scholar] [PubMed]
- Iglesia-Puig, M.A.; Solana, F.J.; Holtzclaw, D.; Toscano, N. Immediate Implant Considerations for Interradicular Bone in Maxillary Molars: Case Reports. J. Implant Adv. Clin. Dent. 2012, 4, 19–31. [Google Scholar]
- Atieh, M.A.; Payne, A.G.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P. Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implants 2010, 25, 401–415. [Google Scholar] [PubMed]
- Peñarrocha, M.; Uribe, R.; Balaguer, J. Immediate implants after extraction. A review of the current situation. A review of the current situation. Med. Oral 2004, 9, 234–242. [Google Scholar] [PubMed]
- McAllister, B.S.; Haghighat, K. Bone augmentation techniques. J. Periodontol. 2007, 78, 377–396. [Google Scholar] [CrossRef] [PubMed]
- Rominger, J.W.; Triplett, R.G. The use of guided tissue regeneration to improve implant osseointegration. J. Oral Maxillofac. Surg. 1994, 52, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Almog, D.M.; Sanchez, R. Correlation between planned prosthetic and residual bone trajectories in dental implants. J. Prosthet. Dent. 1999, 81, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Shokry, M.M.; Taalab, M.R. Immediate implant placement through inter-radicular bone drilling before versus after roots extraction in mandibular molar area (a randomized controlled clinical study). Egypt. Dent. J. 2022, 68, 1377–1388. [Google Scholar] [CrossRef]
- Pavlovic, Z.R.; Petrovic, M. Morphological Characteristics of Maxillary Molars Interradicular Septum and Clinical Implications—What Do We Know So Far? Serb. J. Exp. Clin. Res. 2022. [CrossRef]
- Sayed, A.J.; Shaikh, S.S.; Shaikh, S.Y.; Hussain, M.A. Interradicular bone dimensions in primary stability of immediate molar implants—A cone beam computed tomography retrospective analysis. Saudi Dent. J. 2021, 33, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Avila-Ortiz, G.; Elangovan, S.; Kramer, K.W.; Blanchette, D.; Dawson, D.V. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Ohba, S.; Sumita, Y.; Nakatani, Y.; Noda, S.; Asahina, I. Alveolar bone preservation by a hydroxyapatite/collagen composite material after tooth extraction. Clin. Oral Investig. 2019, 23, 2413–2419. [Google Scholar] [CrossRef] [PubMed]
- Covani, U.; Giammarinaro, E.; Marconcini, S. Alveolar socket remodeling: The tug-of-war model. Med. Hypotheses 2020, 142, 109746. [Google Scholar] [CrossRef] [PubMed]
- Covani, U.; Giammarinaro, E.; Panetta, D.; Salvadori, P.A.; Cosola, S.; Marconcini, S. Alveolar Bone Remodeling with or without Collagen Filling of the Extraction Socket: A High-Resolution X-ray Tomography Animal Study. J. Clin. Med. 2022, 11, 2493. [Google Scholar] [CrossRef]
- Lekovic, V.; Camargo, P.M.; Klokkevold, P.R.; Weinlaender, M.; Kenney, E.B.; Dimitrijevic, B.; Nedic, M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J. Periodontol. 1998, 69, 1044–1049. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Zhou, L.; Lin, J.; Chen, J.; Huang, W.; Chen, Y. Immediate implant placement in anterior teeth with grafting material of autogenous tooth bone vs xenogenic bone. BMC Oral Health 2019, 19, 266. [Google Scholar] [CrossRef] [PubMed]
- Zaki, J.; Yusuf, N.; El-Khadem, A.; Scholten, R.J.P.M.; Jenniskens, K. Efficacy of bone-substitute materials use in immediate dental implant placement: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2021, 23, 506–519. [Google Scholar] [CrossRef] [PubMed]
- Artzi, Z.; Parson, A.; Nemcovsky, C.E. Wide-diameter implant placement and internal sinus membrane elevation in the immediate postextraction phase: Clinical and radiographic observations in 12 consecutive molar sites. Int. J. Oral Maxillofac. Implants 2003, 18, 242–249. [Google Scholar] [PubMed]
- Riben, C.; Thor, A. The Maxillary Sinus Membrane Elevation Procedure: Augmentation of Bone around Dental Implants without Grafts-A Review of a Surgical Technique. Int. J. Dent. 2012, 2012, 105483. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, R.; Wang, M.; Yang, J. Immediate implant placement combined with maxillary sinus floor elevation utilizing the transalveolar approach and nonsubmerged healing for failing teeth in the maxillary molar area: A randomized controlled trial clinical study with one-year follow-up. Clin. Implant Dent. Relat. Res. 2019, 21, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Olivares, L.A.; Cortés-Bretón Brinkmann, J.; Martínez-Rodríguez, N.; Martínez-González, J.M.; López-Quiles, J.; Leco-Berrocal, I.; Meniz-García, C. Management of Schneiderian membrane perforations during maxillary sinus floor augmentation with lateral approach in relation to subsequent implant survival rates: A systematic review and meta-analysis. Int. J. Implant Dent. 2021, 7, 91. [Google Scholar] [CrossRef] [PubMed]
- Testori, T.; Weinstein, T.; Taschieri, S.; Wallace, S.S. Risk factors in lateral window sinus elevation surgery. Periodontology 2000 2019, 81, 91–123. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Liboni, P.; Faccioni, P.; Zangani, A.; D’Agostino, A.; Nocini, P.F. Short and Ultra-Short Implants, in Association with Simultaneous Internal Sinus Lift in the Atrophic Posterior Maxilla: A Five-Year Retrospective Study. Materials 2022, 15, 7995. [Google Scholar] [CrossRef] [PubMed]
- Bechara, S.; Lukosiunas, A.; Dolcini, G.A.; Kubilius, R. Fixed Full Arches Supported by Tapered Implants with Knife-Edge Thread Design and Nanostructured, Calcium-Incorporated Surface: A Short-Term Prospective Clinical Study. Biomed. Res. Int. 2017, 2017, 4170537. [Google Scholar] [CrossRef] [PubMed]
- Hoekstra, J.W.M.; van Oirschot, B.A.; Jansen, J.A.; van den Beucken, J.J. Innovative implant design for continuous implant stability: A mechanical and histological experimental study in the iliac crest of goats. J. Mech. Behav. Biomed. Mater. 2021, 122, 104651. [Google Scholar] [CrossRef] [PubMed]
- Baldi, D.; Lombardi, T.; Colombo, J.; Cervino, G.; Perinetti, G.; Di Lenarda, R.; Stacchi, C. Correlation between Insertion Torque and Implant Stability Quotient in Tapered Implants with Knife-Edge Thread Design. Biomed. Res. Int. 2018, 2018, 7201093. [Google Scholar] [CrossRef] [PubMed]



| NPC Shape | ||||
|---|---|---|---|---|
| The Horizontal Dimensions of the Anterior Maxilla at Different Levels | Banana | Hourglass | Cylindrical | Funnel |
| Level A | 2.3 | 3.2 | 2.9 | 3.5 |
| Level B | 1.4 | 3.4 | 3.2 | 3 |
| Level C | 1.6 | 4 | 3.6 | 3.7 |
| Level D | 2 | 5.9 | 5.7 | 5.8 |
| NPC Shape | ||||
|---|---|---|---|---|
| ACs–MCIs Distance at the Different Levels | Banana | Hourglass | Cylindrical | Funnel |
| Level A | 1.18 | 0.9 | 0.8 | 1.05 |
| Level B | 1.19 | 1.1 | 1.08 | 1.17 |
| Level C | 0.8 | 1.25 | 1.7 | 1.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasiljevic, M.; Selakovic, D.; Rosic, G.; Stevanovic, M.; Milanovic, J.; Arnaut, A.; Milanovic, P. Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review. Diagnostics 2024, 14, 1697. https://doi.org/10.3390/diagnostics14151697
Vasiljevic M, Selakovic D, Rosic G, Stevanovic M, Milanovic J, Arnaut A, Milanovic P. Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review. Diagnostics. 2024; 14(15):1697. https://doi.org/10.3390/diagnostics14151697
Chicago/Turabian StyleVasiljevic, Milica, Dragica Selakovic, Gvozden Rosic, Momir Stevanovic, Jovana Milanovic, Aleksandra Arnaut, and Pavle Milanovic. 2024. "Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review" Diagnostics 14, no. 15: 1697. https://doi.org/10.3390/diagnostics14151697
APA StyleVasiljevic, M., Selakovic, D., Rosic, G., Stevanovic, M., Milanovic, J., Arnaut, A., & Milanovic, P. (2024). Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review. Diagnostics, 14(15), 1697. https://doi.org/10.3390/diagnostics14151697








