Assessment of Reliability, Agreement, and Accuracy of Masseter Muscle Ultrasound Thickness Measurement Using a New Standardized Protocol
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Study Design
2.2. Participants
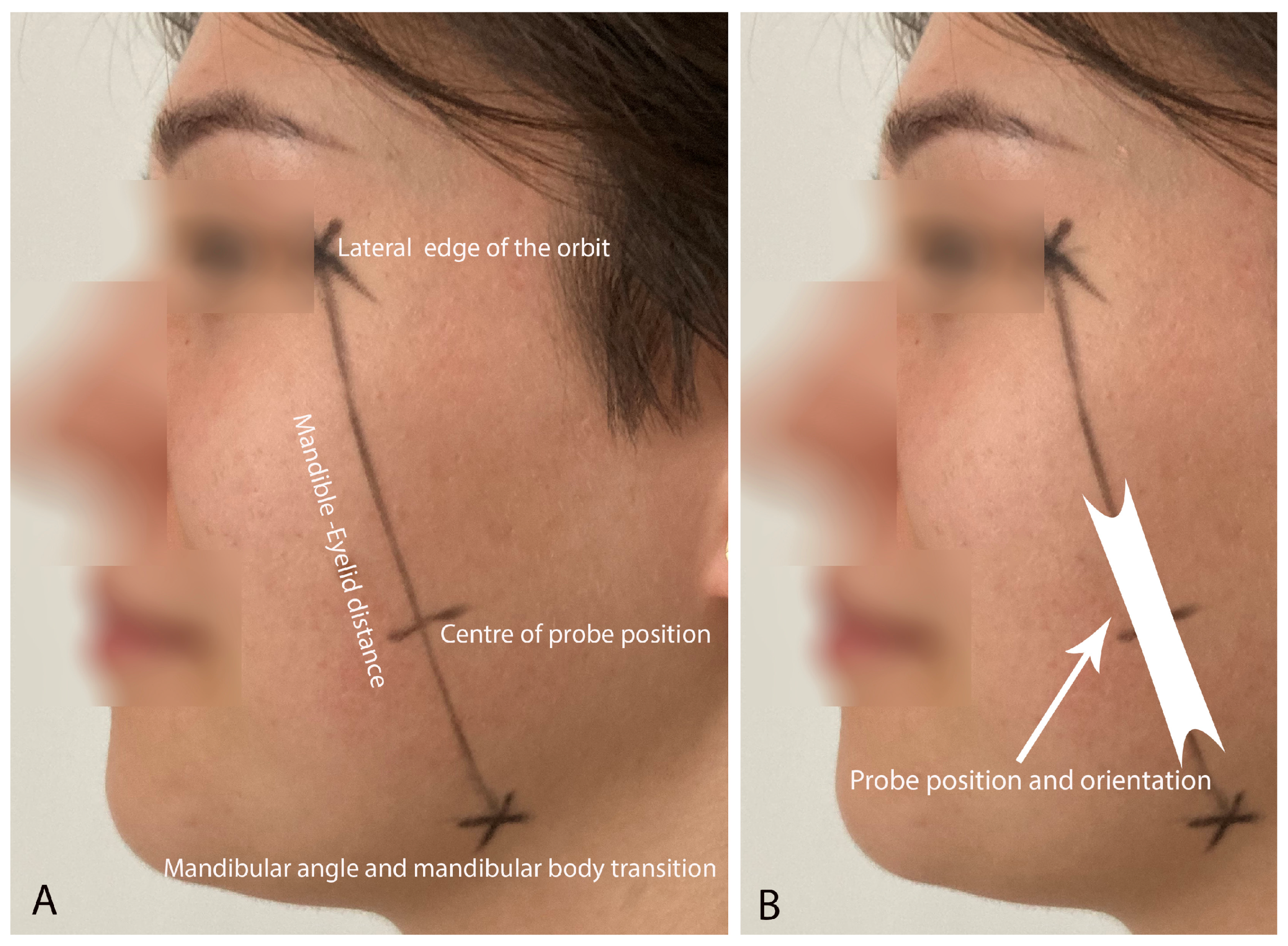
2.3. Ultrasound Measurements
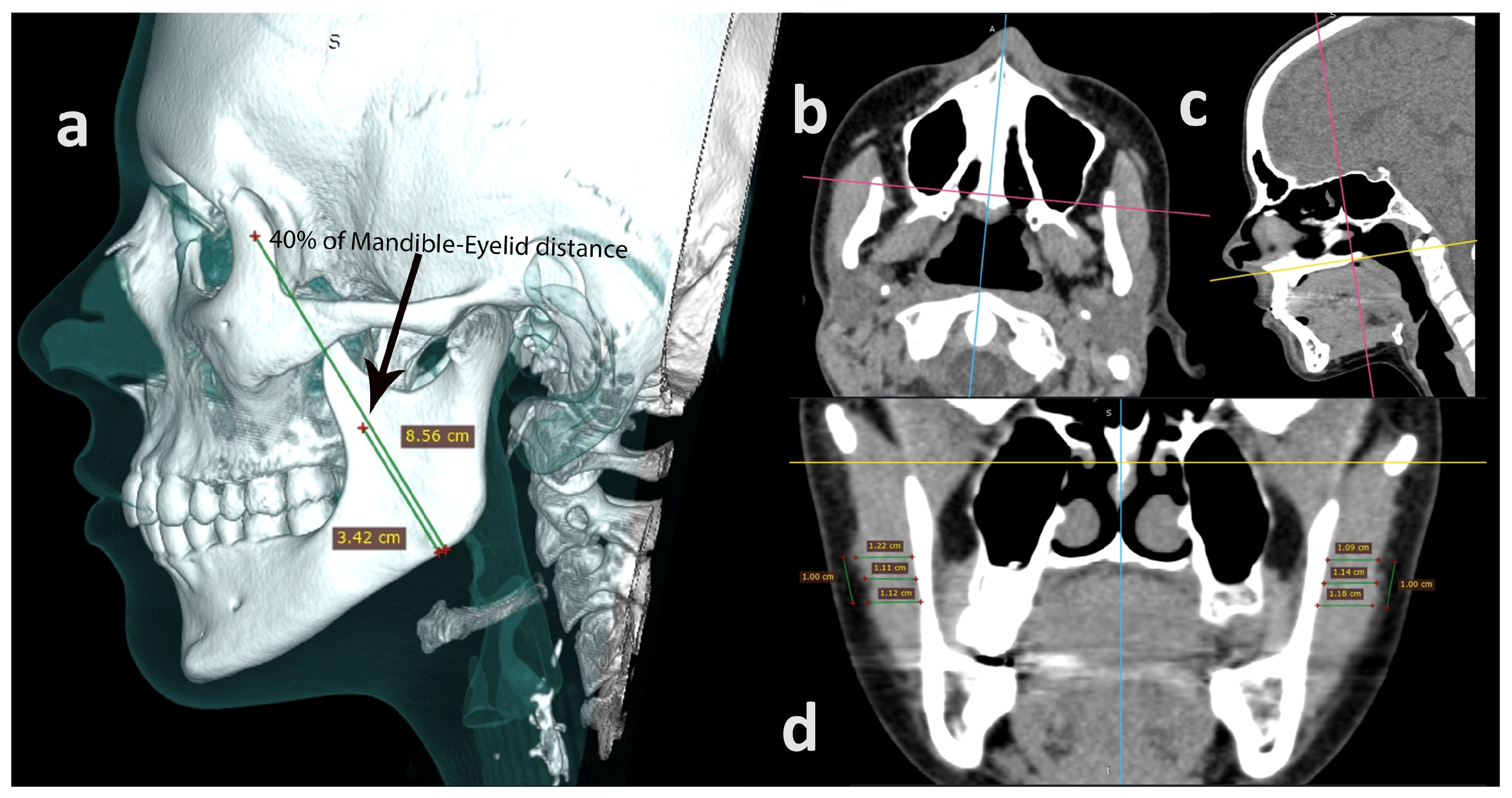
2.4. Computed Tomography
2.5. Data Analysis
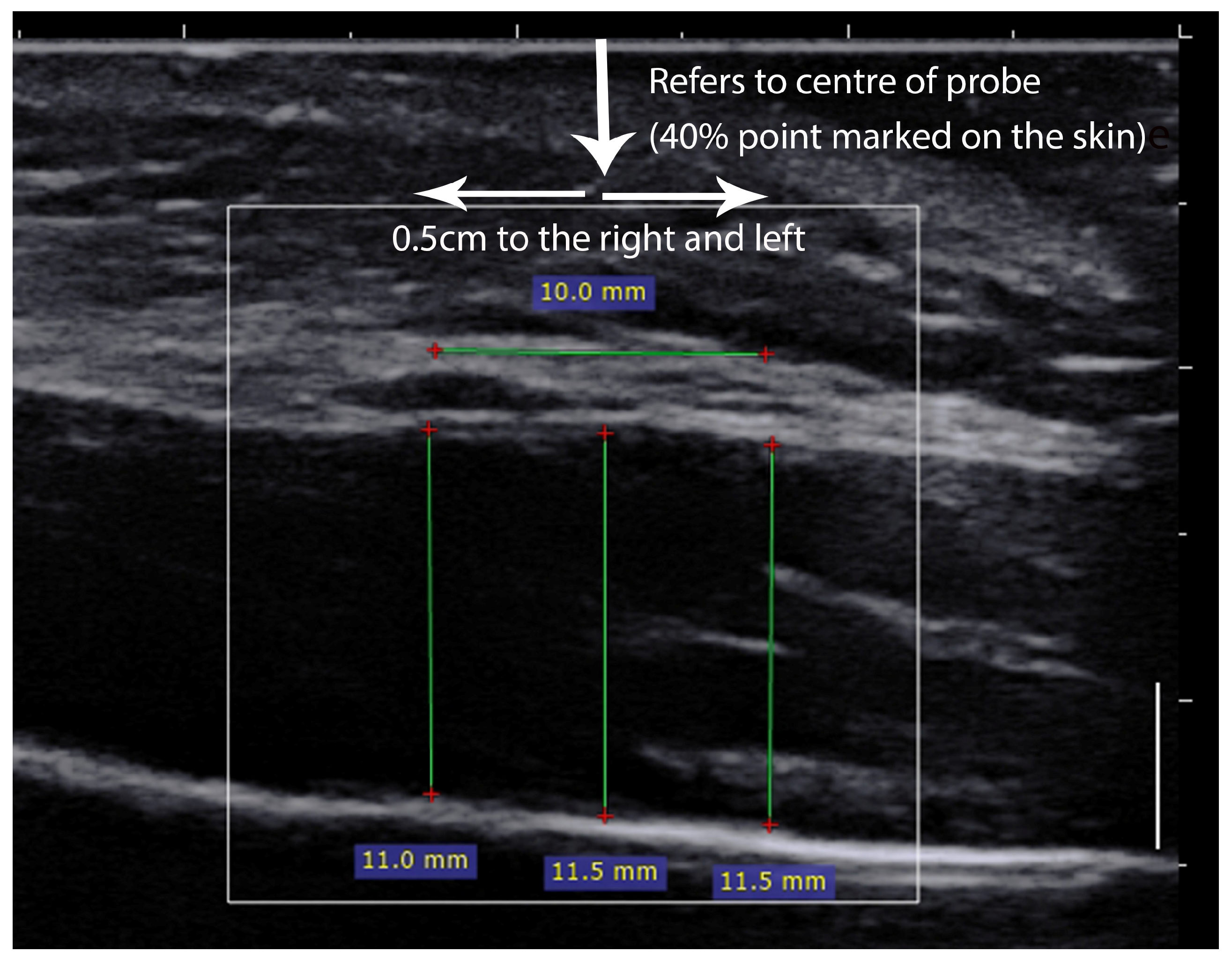
2.5.1. Ultrasound Parameters
2.5.2. Computed Tomography
2.6. Statistical Analyses
3. Results
3.1. Participants
3.2. Masseter Muscle Thickness (Reliability and Agreement)
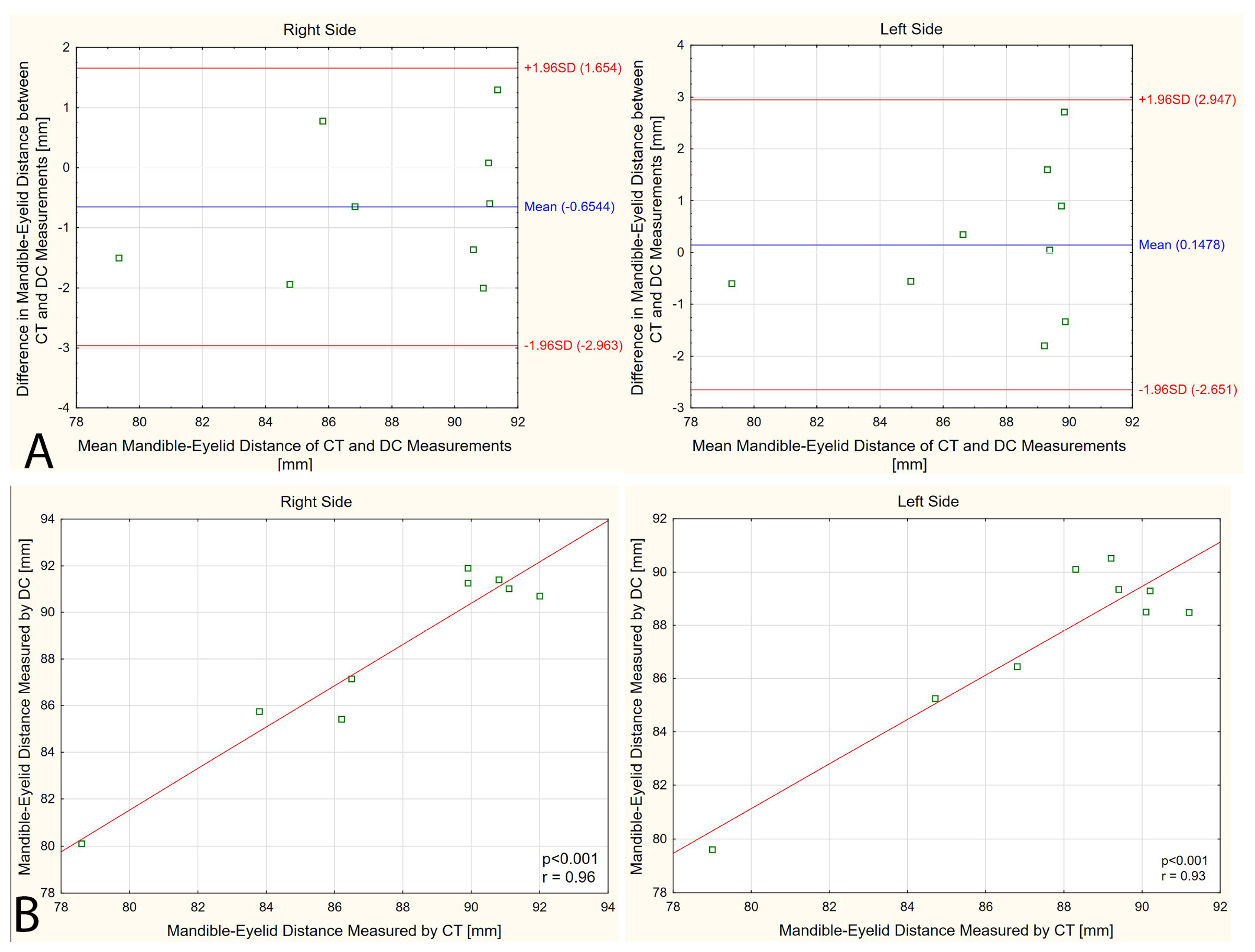
3.3. Mandible–Eyelid Distance
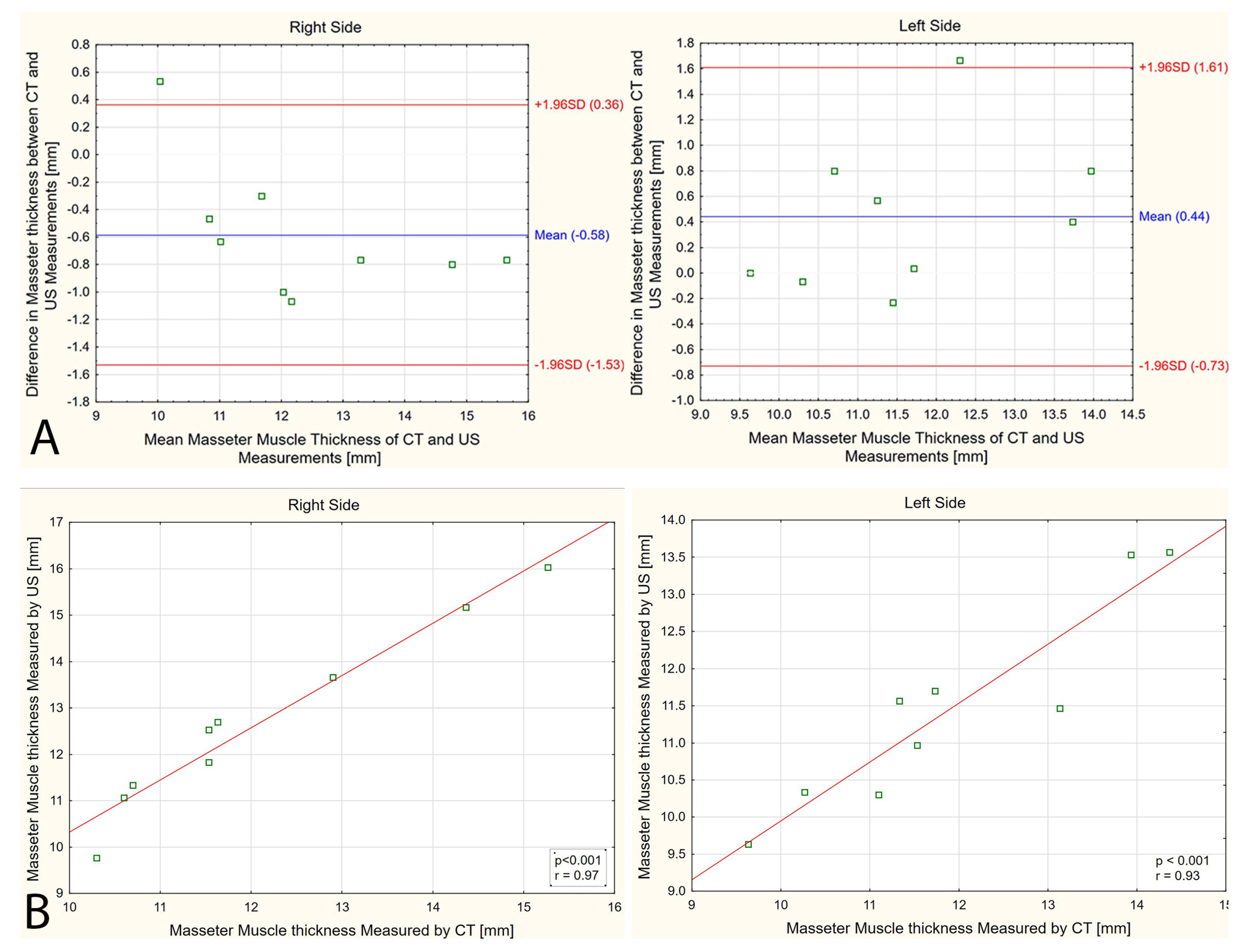
3.4. Masseter Muscle Thickness (CT versus US)
4. Discussion
Implications and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Iguchi, H.; Magara, J.; Nakamura, Y.; Tsujimura, T.; Ito, K.; Inoue, M. Changes in jaw muscle activity and the physical properties of foods with different textures during chewing behaviors. Physiol. Behav. 2015, 152 Pt A, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-S.; Wu, C.-Y.; Wu, S.-Y.; Chuang, K.-H.; Lin, H.-H.; Cheng, D.-H.; Lo, W.-L. Age- and sex-related differences in masseter size and its role in oral functions. J. Am. Dent. Assoc. 2017, 148, 644–653. [Google Scholar] [CrossRef]
- Mapelli, A.; Machado, B.C.Z.; Giglio, L.D.; Sforza, C.; De Felício, C.M. Reorganization of muscle activity in patients with chronic temporomandibular disorders. Arch. Oral Biol. 2016, 72, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Ariji, Y.; Ariji, E. Magnetic resonance and sonographic imagings of masticatory muscle myalgia in temporomandibular disorder patients. Jpn. Dent. Sci. Rev. 2017, 53, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Hara, K.; Namiki, C.; Yamaguchi, K.; Kobayashi, K.; Saito, T.; Nakagawa, K.; Ishii, M.; Okumura, T.; Tohara, H. Association between myotonometric measurement of masseter muscle stiffness and maximum bite force in healthy elders. J. Oral Rehabil. 2020, 47, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Ramazanoglu, E.; Turhan, B.; Usgu, S. Evaluation of the tone and viscoelastic properties of the masseter muscle in the supine position, and its relation to age and gender. Dent. Med. Probl. 2021, 58, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Strini, P.J.S.A.; Barbosa, T.d.S.; Gavião, M.B.D. Assessment of thickness and function of masticatory and cervical muscles in adults with and without temporomandibular disorders. Arch. Oral Biol. 2013, 58, 1100–1108. [Google Scholar] [CrossRef] [PubMed]
- Aldemir, K.; Üstüner, E.; Erdem, E.; Demiralp, A.S.; Oztuna, D. Ultrasound evaluation of masseter muscle changes in stabilization splint treatment of myofascial type painful temporomandibular diseases. Oral Surgery Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 377–383. [Google Scholar] [CrossRef]
- Chakarvarty, A.; Panat, S.R.; Sangamesh, N.C.; Aggarwal, A.; Jha, P.C. Evaluation of masseter muscle hypertrophy in oral submucous fibrosis patients -an ultrasonographic study. J. Clin. Diagn. Res. 2014, 8, ZC45. [Google Scholar] [CrossRef]
- Kant, P.; Bhowate, R.R.; Sharda, N. Assessment of cross-sectional thickness and activity of masseter, anterior temporalis and orbicularis oris muscles in oral submucous fibrosis patients and healthy controls: An ultrasonography and electromyography study. Dentomaxillofacial Radiol. 2014, 43, 20130016. [Google Scholar] [CrossRef]
- Bhoyar, P.S.; Godbole, S.R.; Thombare, R.U.; Pakhan, A.J. Effect of complete edentulism on masseter muscle thickness and changes after complete denture rehabilitation: An ultrasonographic study. J. Investig. Clin. Dent. 2012, 3, 45–50. [Google Scholar] [CrossRef]
- Müller, F.; Hernandez, M.; Grütter, L.; Aracil-Kessler, L.; Weingart, D.; Schimmel, M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: A cross-sectional multicenter study. Clin. Oral Implant. Res. 2012, 23, 144–150. [Google Scholar] [CrossRef]
- Sathasivasubramanian, S.; Venkatasai, P.M.; Divyambika, C.V.; Mandava, R.; Jeffrey, R.; Jabeen, N.A.N.; Kumar, S.S. Masseter muscle thickness in unilateral partial edentulism: An ultrasonographic study. J. Clin. Imaging Sci. 2017, 7, 44. [Google Scholar] [CrossRef]
- Schimmel, M.; Loup, A.; Duvernay, E.; Gaydarov, N.; Muller, F. The effect of mandibular denture abstention on masseter muscle thickness in a 97-year-old patient: A case report. Int. J. Prosthodont. 2010, 23, 418–420. [Google Scholar] [PubMed]
- Trawitzki, L.V.; Dantas, R.O.; Elias-Júnior, J.; Mello-Filho, F.V. Masseter muscle thickness three years after surgical correction of class III dentofacial deformity. Arch. Oral Biol. 2011, 56, 799–803. [Google Scholar] [CrossRef]
- Umeki, K.; Watanabe, Y.; Hirano, H.; Edahiro, A.; Ohara, Y.; Yoshida, H.; Obuchi, S.; Kawai, H.; Murakami, M.; Takagi, D.; et al. The relationship between masseter muscle thickness and appendicular skeletal muscle mass in Japanese community-dwelling elders: A cross-sectional study. Arch. Gerontol. Geriatr. 2018, 78, 18–22. [Google Scholar] [CrossRef]
- Vasconcelos, P.B.; Palinkas, M.; De Sousa, L.G.; Regalo, S.C.H.; Santos, C.M.; De Rossi, M.; Semprini, M.; Scalize, P.H.; Siessere, S. The influence of maxillary and mandibular osteoporosis on maximal bite force and thickness of masticatory muscles. Acta Odontol. Latinoam. 2015, 28, 22–27. [Google Scholar] [CrossRef]
- González-Fernández, M.; Perez-Nogueras, J.; Serrano-Oliver, A.; Torres-Anoro, E.; Sanz-Arque, A.; Arbones-Mainar, J.M.; Sanz-Paris, A. Masseter Muscle Thickness Measured by Ultrasound as a Possible Link with Sarcopenia, Malnutrition and Dependence in Nursing Homes. Diagnostics 2021, 11, 1587. [Google Scholar] [CrossRef]
- Emshoff, R.; Emshoff, I.; Rudisch, A.; Bertram, S. Reliability and temporal variation of masseter muscle thickness measurements utilizing ultrasonography. J. Oral Rehabil. 2003, 30, 1168–1172. [Google Scholar] [CrossRef] [PubMed]
- Serra, M.D.; Gavião, M.B.D.; Uchôa, M.N.d.S. The use of ultrasound in the investigation of the muscles of mastication. Ultrasound Med. Biol. 2008, 34, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Gawriołek, K.; Klatkiewicz, T.; Przystańska, A.; Maciejewska-Szaniec, Z.; Gedrange, T.; Czajka-Jakubowska, A. Standardization of the ultrasound examination of the masseter muscle with size-independent calculation of records. Adv. Clin. Exp. Med. 2021, 30, 441–447. [Google Scholar] [CrossRef]
- Price, R.R.; Jones, T.B.; Goddard, J.; James, A.E., Jr. Basic concepts of ultrasonic tissue characterization. Radiol. Clin. N. Am. 1980, 18, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-M.; Choi, E.; Kwak, E.-J.; Kim, S.; Park, W.; Jeong, J.-S.; Kim, K.-D. The relationship between masseter muscle thickness measured by ultrasonography and facial profile in young Korean adults. Imaging Sci. Dent. 2018, 48, 213–221. [Google Scholar] [CrossRef]
- Şatıroğlu, F.; Arun, T.; Işık, F. Comparative data on facial morphology and muscle thickness using ultrasonography. Eur. J. Orthod. 2005, 27, 562–567. [Google Scholar] [CrossRef]
- Volk, G.F.; Sauer, M.; Pohlmann, M.; Guntinas-Lichius, O. Reference values for dynamic facial muscle ultrasonography in adults. Muscle Nerve 2014, 50, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Blicharz, G.; Rymarczyk, M.; Rogulski, M.; Linek, P. Methods of Masseter and Temporal Muscle Thickness and Elasticity Measurements by Ultrasound Imaging: A Literature Review. Curr. Med. Imaging 2021, 17, 707–713. [Google Scholar] [CrossRef]
- Cicchetti, D.; Sparrow, S. Developing criteria for establishing interrater reliability of specific items—Applications to assessment of adaptive-behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar] [PubMed]
- Ispir, N.G.; Toraman, M. The relationship of masseter muscle thickness with face morphology and parafunctional habits: An ultrasound study. Dentomaxillofacial. Radiol. 2022, 51, 20220166. [Google Scholar] [CrossRef]
| Masseter Muscle Thickness | |||
|---|---|---|---|
| Right Side | Left Side | ||
| Computer Tomography | |||
| Intra-rater reliability Radiologist (seven-day interval) | ICC3.1 (95% CI) 1 | 0.99 (0.97–0.99) | 0.98 (0.93–0.99) |
| SEM (mm) | 0.17 | 0.22 | |
| CV (%) | 1.22 | 0.81 | |
| Bias 3 (mm) | −0.21 2 | −0.14 | |
| Intra-rater reliability Dentist (seven-day interval) | ICC3.1 (95% CI) 1 | 0.98 (0.91–0.99) | 0.97 (0.89–0.99) |
| SEM (mm) | 0.27 | 0.26 | |
| CV (%) | 0.28 | 0.40 | |
| Bias 3 (mm) | 0.05 | 0.07 | |
| Inter-rater reliability | ICC2.1 (95% CI) 1 | 0.88 (0.60–0.97) | 0.98 (0.92–0.99) |
| SEM (mm) | 0.63 | 0.22 | |
| CV (%) | 1.33 | 0.89 | |
| Bias 3 (mm) | −0.23 | −0.22 | |
| Ultrasonography | |||
| Intra-session reliability First physiotherapist | ICC3.1 (95% CI) 1 | 0.85 (0.47–0.96) | 0.87 (0.53–0.97) |
| SEM (mm) | 0.68 | 0.56 | |
| CV (%) | 1.97 | 3.59 | |
| Bias 3 (mm) | −0.36 | −0.60 | |
| Intra-session reliability Second physiotherapist | ICC3.1 (95% CI) 1 | 0.98 (0.93–0.97) | 0.94 (0.76–0.99) |
| SEM (mm) | 0.25 | 0.41 | |
| CV (%) | 0.30 | 0.55 | |
| Bias 3 (mm) | 0.05 | 0.09 | |
| Inter-rater reliability | ICC2.1 (95% CI) 1 | 0.92 (0.71–0.98) | 0.87 (0.44–0.97) |
| SEM (mm) | 0.54 | 0.53 | |
| CV (%) | 1.48 | 2.93 | |
| Bias 3 (mm) | 0.26 | −0.48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogulski, M.; Pałac, M.; Wolny, T.; Linek, P. Assessment of Reliability, Agreement, and Accuracy of Masseter Muscle Ultrasound Thickness Measurement Using a New Standardized Protocol. Diagnostics 2024, 14, 1771. https://doi.org/10.3390/diagnostics14161771
Rogulski M, Pałac M, Wolny T, Linek P. Assessment of Reliability, Agreement, and Accuracy of Masseter Muscle Ultrasound Thickness Measurement Using a New Standardized Protocol. Diagnostics. 2024; 14(16):1771. https://doi.org/10.3390/diagnostics14161771
Chicago/Turabian StyleRogulski, Mateusz, Małgorzata Pałac, Tomasz Wolny, and Paweł Linek. 2024. "Assessment of Reliability, Agreement, and Accuracy of Masseter Muscle Ultrasound Thickness Measurement Using a New Standardized Protocol" Diagnostics 14, no. 16: 1771. https://doi.org/10.3390/diagnostics14161771
APA StyleRogulski, M., Pałac, M., Wolny, T., & Linek, P. (2024). Assessment of Reliability, Agreement, and Accuracy of Masseter Muscle Ultrasound Thickness Measurement Using a New Standardized Protocol. Diagnostics, 14(16), 1771. https://doi.org/10.3390/diagnostics14161771








