Morphological Analysis of the Anatomical Mandibular Lingual Concavity Using Cone Beam Computed Tomography Scans in East Asian Population—A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
- -
- Adults aged 19 years or older whose jawbone growth was completed.
- -
- Patients who visited Hallym University Sacred Heart Hospital and had their first and second molars present from 2020 to 2023.
- -
- Patients without systemic or local conditions, such as osteoporosis or periodontitis, that could alter the condition of the jawbone.
- -
- Individuals with no surgical history, such as the removal of benign tumors in the mandible.
- -
- Individuals who have not undergone radiation therapy in the oral cavity region.
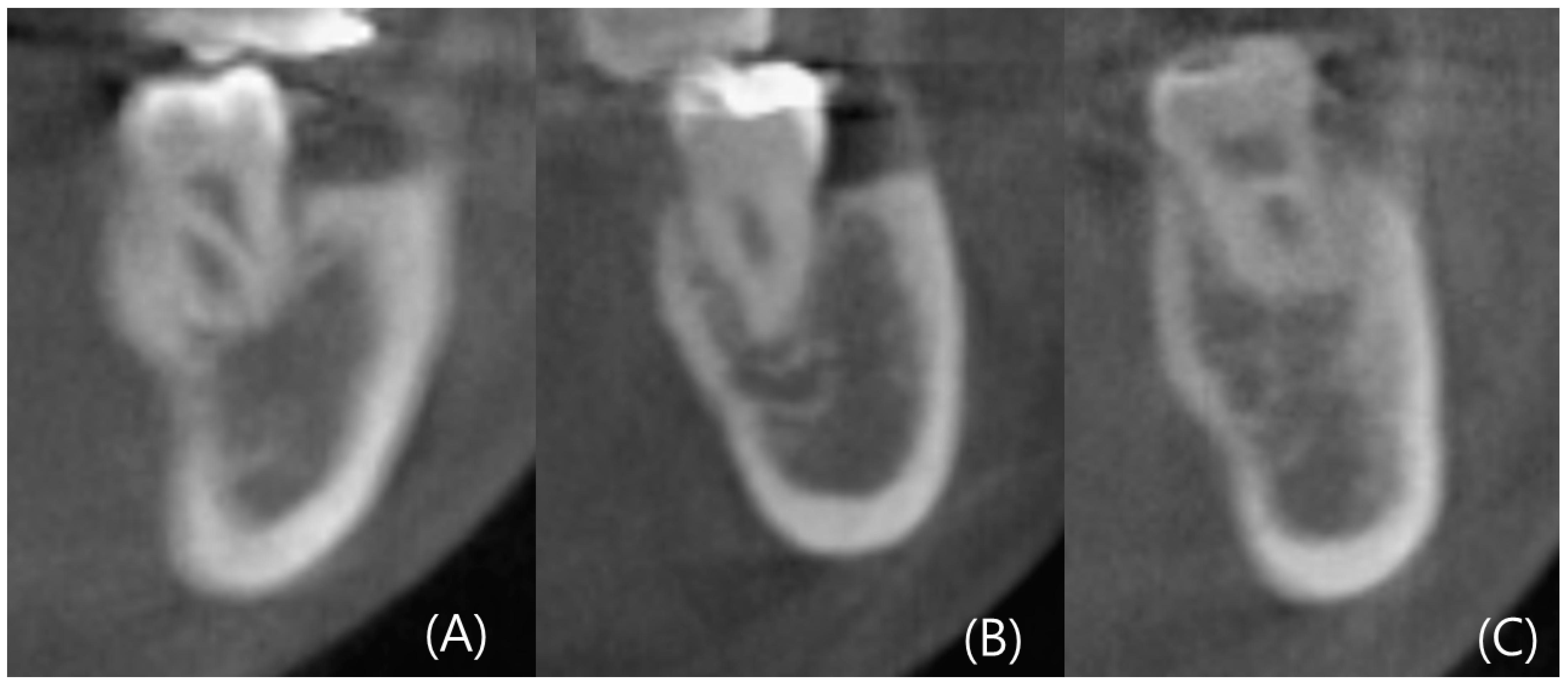
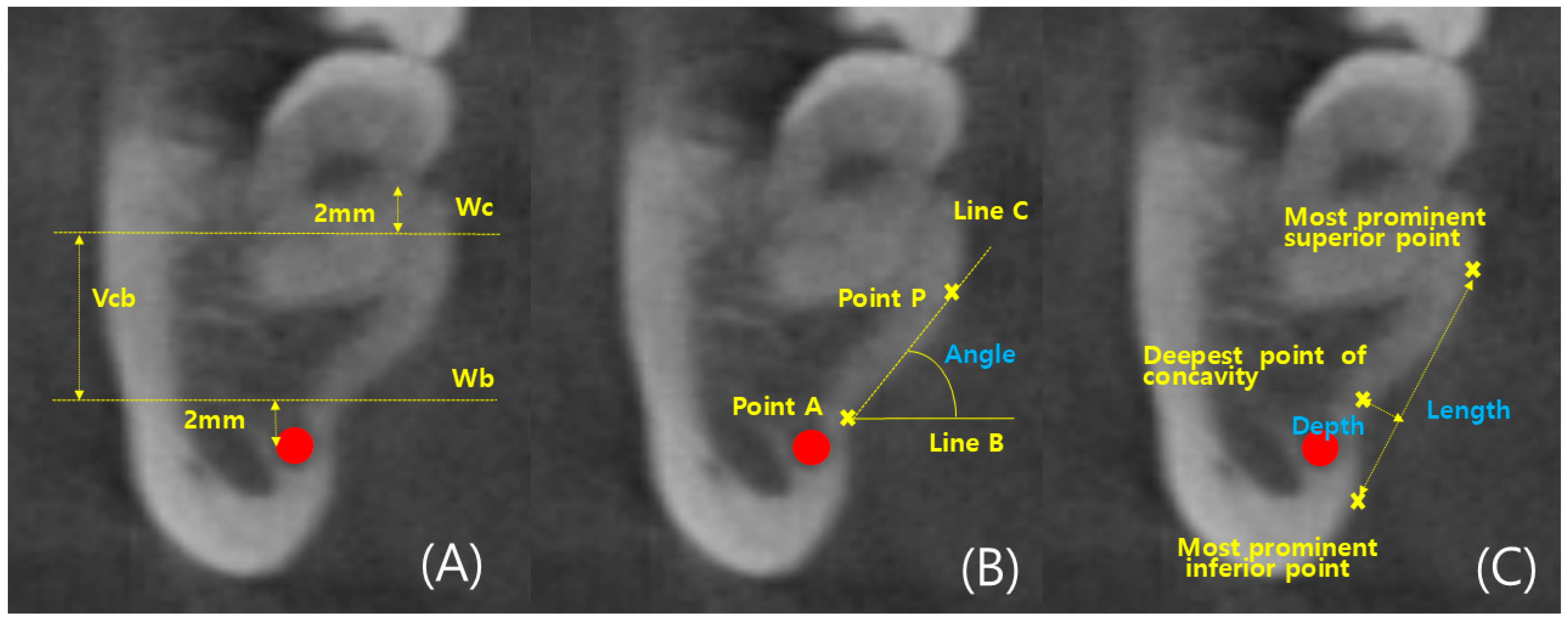
2.2. Measurements
2.3. Statistics
3. Results
3.1. Comparison between Left and Right Sides
3.2. Comparison by Tooth Type
3.3. Comparison by Gender
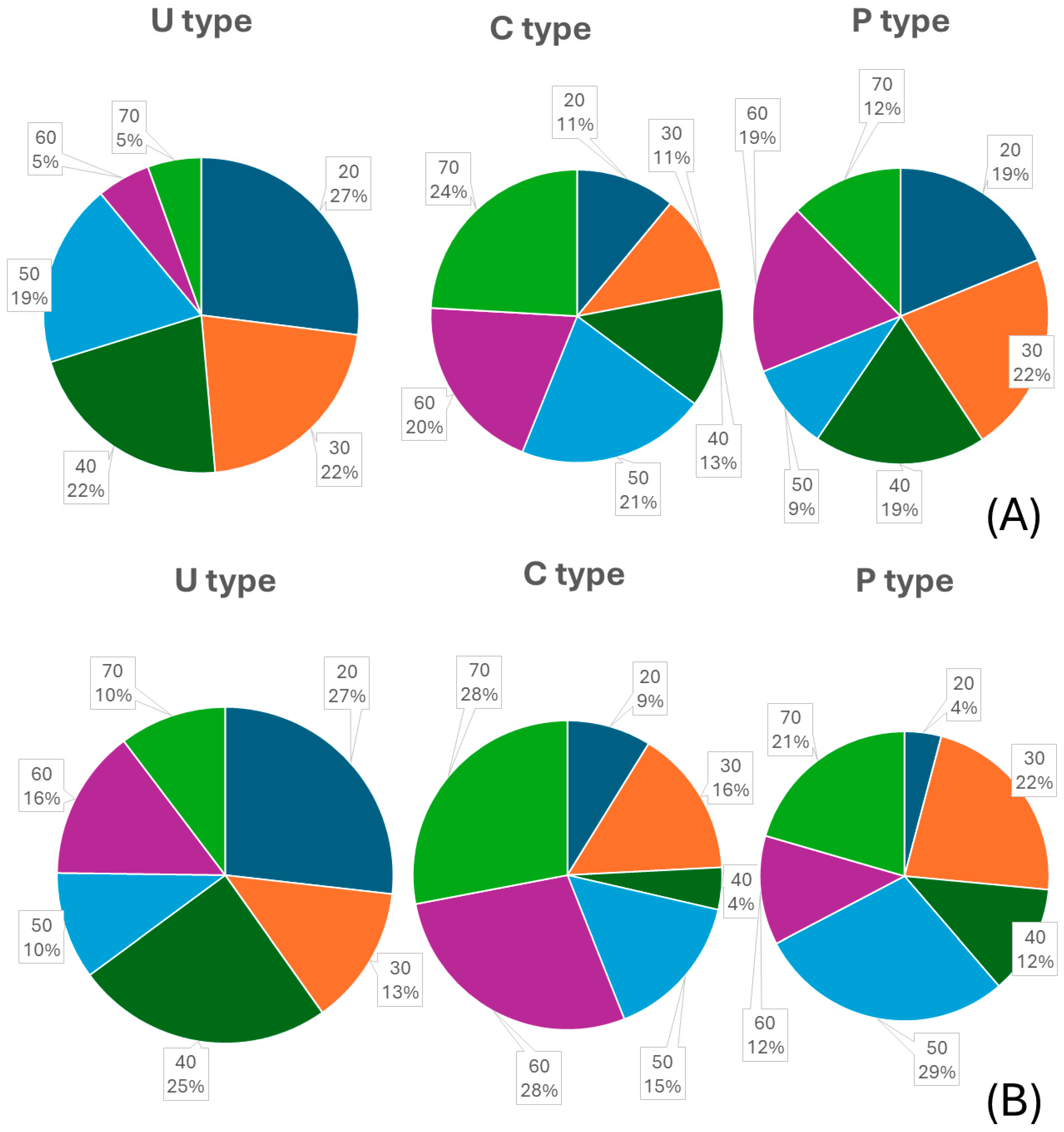
3.4. Comparison by Age
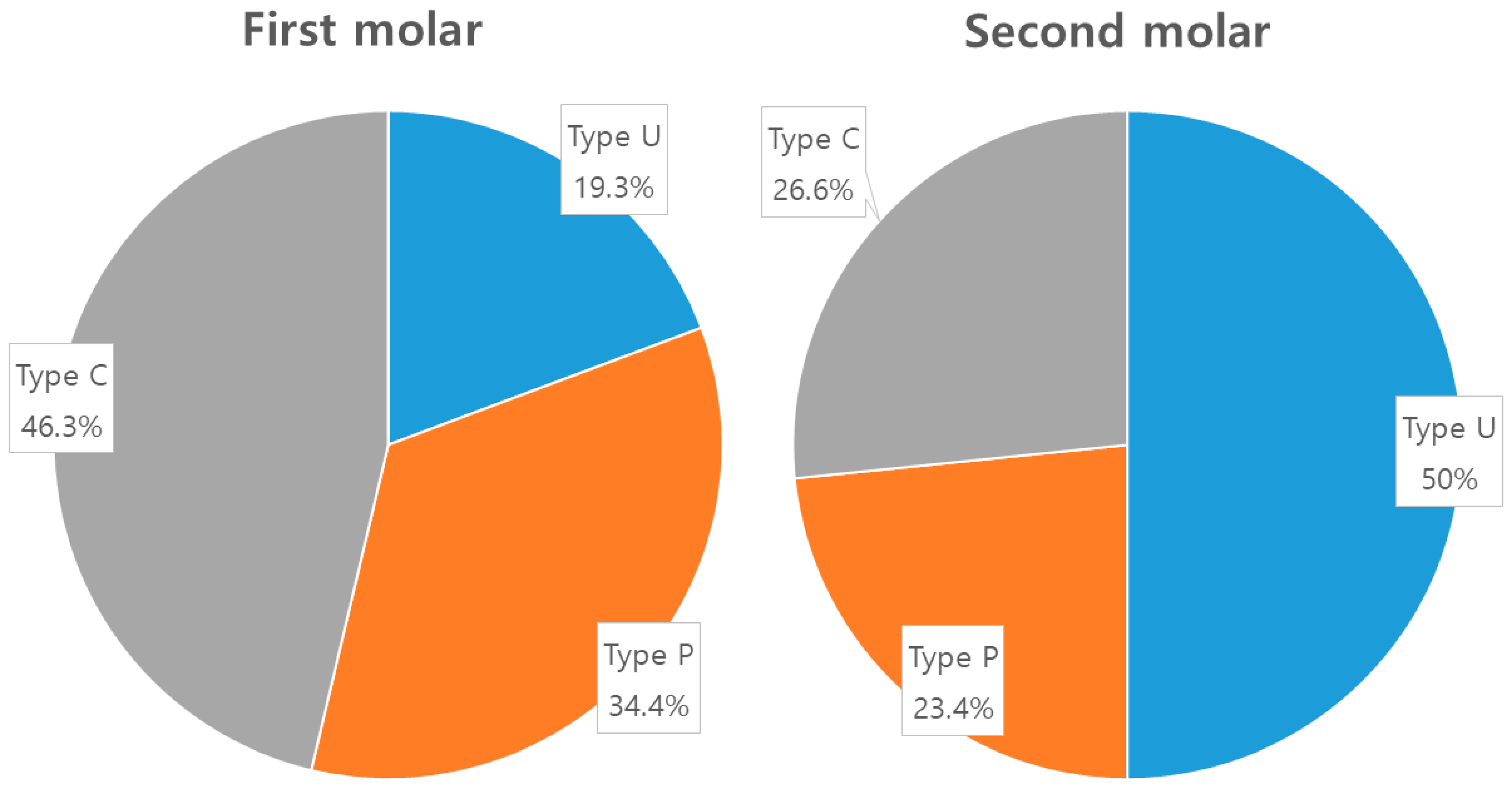
3.5. Analysis of Ridge Type Ratio
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Greenstein, G.; Cavallaro, J.; Romanos, G.; Tarnow, D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: A review. J. Periodontol. 2008, 79, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Cavallaro, J.; Tarnow, D. Practical application of anatomy for the dental implant surgeon. J. Periodontol. 2008, 79, 1833–1846. [Google Scholar] [CrossRef] [PubMed]
- Lekholm, U.; Zarb, G. Tissue Integrated Prosthesis: Osseointegration in Clinical Dentistry; Quintessence Publications Co., Inc.: Chicago, IL, USA, 1985. [Google Scholar]
- Jain, N.; Gulati, M.; Garg, M.; Pathak, C. Short implants: New horizon in implant dentistry. J. Clin. Diagn. Res. 2016, 10, ZE14. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral. Implantol. 2010, 3, 7–26. [Google Scholar]
- Tepper, G.; Hofschneider, U.B.; Gahleitner, A.; Ulm, C. Computed tomographic diagnosis and localization of bone canals in the mandibular interforaminal region for prevention of bleeding complications during implant surgery. Int. J. Oral Maxillofac. Implants 2001, 16, 68. [Google Scholar] [PubMed]
- Quirynen, M.; Mraiwa, N.; Steenberghe, D.; Jacobs, R. Morphology and dimensions of the mandibular jaw bone in the interforaminal region in patients requiring implants in the distal areas. Clin. Oral Implants Res. 2003, 14, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Benavides, E.; Yeh, C.Y.; Fu, J.H.; Rudek, I.E.; Wang, H.L. Risk assessment of lingual plate perforation in posterior mandibular region: A virtual implant placement study using cone-beam computed tomography. J. Periodontol. 2011, 82, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Herranz, A.J.; Marques, J.; Almendros, M.N.; Gay, E.C. Retrospective study of the bone morphology in the posterior mandibular region. Evaluation of the prevalence and the degree of lingual concavity and their possible complications. Med. Oral Patol. Oral Cir. Bucal. 2016, 21, e731. [Google Scholar]
- Kalpidis, C.D.; Setayesh, R.M. Hemorrhaging associated with endosseous implant placement in the anterior mandible: A review of the literature. J. Periodontol. 2004, 75, 631–645. [Google Scholar] [CrossRef]
- Givol, N.; Chaushu, G.; Halamish, S.T.; Taicher, S. Emergency tracheostomy following life threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J. Periodontol. 2000, 71, 1893–1895. [Google Scholar] [CrossRef]
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 817–826. [Google Scholar] [CrossRef]
- Tan, W.Y.; Ng, J.Z.L.; Bapat, R.A.; Chaubal, T.V.; Kanneppedy, S.K. Evaluation of anatomic variations of mandibular lingual concavities from cone beam computed tomography scans in a Malaysian population. J. Prosthet. Dent. 2021, 125, 766-e1. [Google Scholar] [CrossRef]
- Bodart, L.; Hanken, H.; Smeets, R.; Gosau, M.; Li, C.; Kluwe, L.; Klatt, J. Assessing the frequency of deep lingual concavities in 826 posterior mandible sockets. J. Cranio-Maxillofac. Surg. 2020, 48, 1045–1051. [Google Scholar] [CrossRef]
- Nickenig, H.J.; Wichmann, M.; Eitner, S.; Zoeller, J.E.; Kreppel, M. Lingual concavities in the mandible: A morphological study using cross-sectional analysis determined by CBCT. J. Cranio-Maxillofac. Surg. 2015, 43, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Mohammad, A.M.; Kurabayashi, T.; Aoki, H. Mandible size and morphology determined with CT on a premise of dental implant operation. Surg. Radiol. Anat. 2010, 32, 343–349. [Google Scholar] [CrossRef]
- Pan, Z.; Xu, S. Population genomics of East Asian ethnic groups. Hereditas 2020, 157, 49. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Vehmas, T.; Kortesniemi, M.; Robinson, S.; Peltolam, J. Accuracy of linear measurements using dental cone beam and conventional multi-slice computed tomography. Dentomaxillofac. Radiol. 2008, 37, 10–17. [Google Scholar] [CrossRef]
- Bolin, A.; Ellasson, S.; Von, B.M.; Jansson, L. Radiographic evaluation of mandibular posterior implant sites; correlation be tween panoramic and tomographic determinations. Clin. Oral Implants Res. 1996, 7, 354–359. [Google Scholar] [CrossRef]
- de Souza, L.A.; Souza, P.A.N.M.; Ribeiro, R.A.; Pires, C.A.C.; Devito, K.L. Assessment of mandibular posterior regional land marks using cone-beam computed tomography in dental implant surgery. Ann. Anat. 2016, 205, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Salemi, F.; Shokri, A.; Forouzandeh, M.; Karami, M.; Khalili, Z. Mandibular Lingual Concavity: A Cross-sectional Analysis us ing Cone Beam Computed Tomography. J. Clin. Diagn. Res. 2018, 12, 37. [Google Scholar] [CrossRef]
- Bayrak, S.; Demirturk, K.H.; Yaprak, E.; Ustaoglu, G.; Noujeim, M. Correlation between the visibility of submandibular fossa and mandibular canal cortication on panoramic radiographs and submandibular fossa depth on CBCT. Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e105. [Google Scholar] [CrossRef] [PubMed]
- Rajput, B.S.; Merita, S.; Parihar, A.S.; Vyas, T.; Kaur, P.; Chansoria, S. Assessment of Lingual Concavities in SubmandibularFossa Region in Patients requiring Dental Implants—A Cone Beam Computed Tomography Study. J. Contemp. Dent. Pract. 2018, 19, 1329–1333. [Google Scholar] [PubMed]
- Chan, H.L.; Brooks, S.L.; Fu, J.H.; Yeh, C.Y.; Rudek, I.; Wang, H.L. Cross-sectional analysis of the mandibular lingual concavity using cone beam computed tomography. Clin. Oral Implants Res. 2011, 22, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Yoon, T.Y.; Patel, M.; Michaud, R.A.; Manibo, A.M. Cone beam computerized tomography analysis of the posterior and anterior mandibular lingual concavity for dental implant patients. J. Oral Implantol. 2017, 43, 12–18. [Google Scholar] [CrossRef] [PubMed]
- von Wowern, N.; Stoltze, K.A.J. Pattern of age related bone loss in mandibles. Eur. J. Oral Sci. 1980, 88, 134–146. [Google Scholar] [CrossRef]

| Tooth Type | Dimensional Measurements | Degree of Lingual Concavity | |||||
|---|---|---|---|---|---|---|---|
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | ||
| First molar | Left [SD] | 14.25 [2.33] | 13.66 [2.14] | 9.06 [1.61] | 60.2 [7.8] | 9.0 [1.6] | 1.8 [0.6] |
| Right [SD] | 14.13 [2.23] | 13.62 [2.24] | 9.11 [1.65] | 61.1 [7.9] | 9.0 [2.0] | 2.1 [0.6] | |
| p | 0.71 | 0.89 | 0.97 | 0.72 | 0.99 | 0.24 | |
| Second molar | Left [SD] | 15.13 [2.46] | 15.79 [2.47] | 8.56 [1.65] | 56.1 [6.3] | 9.3 [1.9] | 2.1 [1.6] |
| Right [SD] | 15.43 [2.87] | 16.11 [2.63] | 8.51 [1.55] | 56.1 [6.0] | 9.3 [1.8] | 2.2 [1.9] | |
| p | 0.431 | 0.402 | 0.824 | 0.993 | 0.992 | 0.171 | |
| Tooth | Dimensional Measurements | Degree of Lingual Concavity | |||||
|---|---|---|---|---|---|---|---|
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | ||
| First molar | Mean [SD] | 14.19 [2.27] | 13.64 [2.18] | 9.09 [1.62] | 60.7 [7.7] | 9.0 [1.8] | 2.0 [1.6] |
| Second molar | Mean [SD] | 15.28 [2.67] | 15.95 [2.54] | 8.54 [1.59] | 56.1 [6.1] | 9.3 [1.8] | 2.1 [1.8] |
| All | Mean [SD] | 14.74 [2.47] | 14.80 [2.21] | 8.82 [1.77] | 58.4 [10.4] | 9.2 [1.8] | 2.0 [1.9] |
| p | 0.004 * | 0.003 * | 0.003 * | 0.002 * | 0.507 | 0.062 | |
| Sex | Left First Molar | Left Second Molar | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimensional Measurements | Degree of Lingual Concavity | Dimensional Measurements | Degree of Lingual Concavity | ||||||||||
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | Base Width | Crest Width | Ridge Height | Angle | Length | Depth | ||
| Male | Mean [SD] | 13.89 [2.23] | 14.23 [1.92] | 9.21 [1.71] | 59.8 [5.1] | 9.3 [1.8] | 1.8 [0.4] | 15.69 [2.45] | 16.13 [2.21] | 8.89 [1.79] | 54.3 [6.0] | 9.7 [2.1] | 2.1 [1.6] |
| Female | Mean [SD] | 13.62 [2.27] | 13.09 [2.21] | 8.92 [1.50] | 60.6 [9.9] | 8.8 [1.5] | 1.9 [0.7] | 14.57 [2.36] | 15.46 [2.68] | 8.23 [1.43] | 57.3 [6.2] | 9.0 [1.6] | 2.1 [1.8] |
| All | Mean [SD] | 13.26 [3.12] | 13.66 [3.01] | 9.07 [1.61] | 60.2 [7.8] | 9.0 [1.6] | 1.8 [0.6] | 15.13 [2.88] | 15.80 [2.64] | 8.56 [1.53] | 56.1 [6.3] | 9.3 [1.8] | 2.2 [1.9] |
| p | 0.006 * | 0.008 * | 0.853 | 0.852 | 0.541 | 0.878 | 0.022 * | 0.043 * | 0.179 | 0.043 * | 0.216 | 0.743 | |
| Sex | Right First Molar | Right Second Molar | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimensional Measurements | Degree of Lingual Concavity | Dimensional Measurements | Degree of Lingual Concavity | ||||||||||
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | Base Width | Crest Width | Ridge Height | Angle | Length | Depth | ||
| Male | Mean [SD] | 14.65 [2.14] | 14.26 [2.12] | 9.29 [1.76] | 60.0 [6.9] | 9.5 [1.3] | 2.2 [0.6] | 16.21 [2.96] | 16.59 [2.23] | 8.64 [1.65] | 53.9 [5.4] | 9.8 [2.2] | 2.2 [2.0] |
| Female | Mean [SD] | 13.60 [2.23] | 12.97 [2.22] | 8.93 [1.53] | 62.1 [8.8] | 8.7 [2.4] | 2.0 [0.7] | 14.65 [2.69] | 15.62 [2.87] | 8.38 [1.45] | 57.5 [6.1] | 8.9 [1.4] | 2.2 [1.9] |
| All | Mean [SD] | 14.13 [2.20] | 13.62 [2.16] | 9.11 [1.66] | 61.1 [7.9] | 9.0 [2.0] | 2.1 [0.6] | 15.43 [2.82] | 16.11 [2.55] | 8.51 [1.55] | 56.1 [6.0] | 9.3 [1.8] | 2.2 [1.9] |
| p | 0.022 * | 0.003 * | 0.302 | 0.568 | 0.403 | 0.494 | 0.011 * | 0.073 | 0.396 | 0.023 * | 0.152 | 0.298 | |
| Age | N | Left First Molar | Left Second Molar | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimensional Measurements | Degree of Lingual Concavity | Dimensional Measurements | Degree of Lingual Concavity | |||||||||||
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | Base Width | Crest Width | Ridge Height | Angle | Length | Depth | |||
| 20~29 a | 16 | Mean [SD] | 13.67 [2.04] | 13.89 [1.61] | 10.76 [1.61] | 57.5 [11.7] | 9.9 [2.4] | 2.2 [0.7] | 14.06 [1.70] | 16.38 [2.20] | 10.44 [1.73] | 54.5 [7.3] | 10.9 [1.6] | 2.3 [0.3] |
| 30~39 b | 16 | Mean [SD] | 14.08 [3.14] | 14.02 [2.37] | 9.24 [1.48] | 66.5 [4.1] | 9.3 [0.8] | 1.5 [0.6] | 15.83 [3.04] | 16.28 [2.86] | 8.48 [1.22] | 59.0 [4.2] | 8.8 [1.3] | 2.0 [0.5] |
| 40~49 c | 16 | Mean [SD] | 13.91 [1.66] | 13.78 [1.54] | 8.88 [1.24] | 59.7 [5.6] | 8.7 [0.6] | 8.7 [1.3] | 15.18 [2.36] | 16.66 [1.98] | 8.55 [1.29] | 57.4 [7.5] | 8.8 [1.0] | 1.9 [0.5] |
| 50~59 d | 16 | Mean [SD] | 14.26 [2.56] | 13.49 [2.38] | 8.79 [1.15] | 57.9 [5.5] | 8.7 [1.3] | 1.9 [0.3] | 15.34 [2.81] | 15.64 [2.56] | 8.17 [1.31] | 56.8 [4.9] | 10.7 [1.7] | 2.6 [0.3] |
| 60~69 e | 16 | Mean [SD] | 15.52 [1.67] | 14.31 [2.25] | 8.13 [1.43] | 57.6 [NA] | 6.2 [NA] | 1.1 [NA] | 15.46 [1.59] | 15.3 [1.54] | 7.61 [1.49] | 52.5 [4.1] | 7.5 [1.5] | 1.7 [0.3] |
| 70~79 f | 16 | Mean [SD] | 14.08 [2.44] | 13.57 [2.39] | 7.59 [1.54] | NA | NA | NA | 14.92 [2.89] | 14.51 [3.04] | 7.13 [1.40] | 57.6 [5.0] | 7.9 [1.6] | 2.1 [0.2] |
| All | 96 | p | 0.283 | 0.281 | 0.002 * | 0.373 | 0.642 | 0.434 | 0.443 | 0.132 | 0.001 * | 0.043 * | 0.002 * | 0.043 * |
| Scheffe post-hoc test | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | |||||||||
| Age | N | Right First Molar | Right Second Molar | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimensional Measurements | Degree of Lingual Concavity | Dimensional Measurements | Degree of Lingual Concavity | |||||||||||
| Base Width | Crest Width | Ridge Height | Angle | Length | Depth | Base Width | Crest Width | Ridge Height | Angle | Length | Depth | |||
| 20~29 a | 16 | Mean [SD] | 13.65 [1.90] | 13.68 [1.56] | 10.91 [1.67] | 53.0 [3.6] | 10.2 [2.5] | 2.3 [0.9] | 14.01 [2.25] | 16.55 [2.22] | 9.95 [1.84] | 53.6 [5.3] | 10.6 [1.6] | 2.9 [0.5] |
| 30~39 b | 16 | Mean [SD] | 14.06 [2.89] | 14.06 [1.49] | 8.89 [1.90] | 69.2 [3.8] | 8.3 [2.6] | 1.7 [0.7] | 15.66 [3.07] | 16.22 [3.07] | 8.98 [1.21] | 59.8 [2.3] | 9.1 [1.3] | 2.2 [0.2] |
| 40~49 c | 16 | Mean [SD] | 13.67 [1.45] | 13.76 [1.55] | 9.32 [1.17] | 61.5 [5.8] | 8.0 [1.4] | 2.0 [0.5] | 15.30 [2.61] | 17.01 [2.46] | 8.84 [1.02] | 55.7 [4.6] | 8.5 [1.5] | 2.1 [0.7] |
| 50~59 d | 16 | Mean [SD] | 14.09 [2.73] | 13.41 [2.41] | 8.79 [1.11] | 60.3 [5.0] | 9.0 [0.9] | 2.2 [0.3] | 15.48 [3.02] | 15.71 [2.75] | 8.69 [1.35] | 56.6 [6.0] | 10.1 [2.2] | 2.2 [0.1] |
| 60~69 e | 16 | Mean [SD] | 15.13 [1.57] | 14.21 [2.42] | 8.41 [1.14] | 52.8 [NA] | 8.3 [NA] | 1.6 [NA] | 15.52 [1.67] | 14.31 [2.25] | 8.13 [1.43] | 52.0 [1.7] | 7.8 [1.6] | 1.9 [0.4] |
| 70~79 f | 16 | Mean [SD] | 14.14 [2.46] | 12.56 [2.68] | 8.36 [1.49] | 65.8 [1.1] | 10.2 [2.7] | 2.4 [0.2] | 14.08 [2.44] | 12.57 [2.39] | 7.59 [1.54] | 55.4 [4.0] | 9.0 [1.2] | 1.9 [0.2] |
| All | 96 | p | 0.143 | 0.372 | 0.001 * | 0.138 | 0.583 | 0.624 | 0.341 | 0.492 | 0.001 * | 0.043 * | 0.005 * | 0.011 * |
| Scheffe post-hoc test | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | e,f < a,b,c,d | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, H.-J.; Byun, S.-H.; Che, S.-A.; Park, S.-Y.; Yi, S.-M.; Park, I.-Y.; On, S.-W.; Yang, B.-E. Morphological Analysis of the Anatomical Mandibular Lingual Concavity Using Cone Beam Computed Tomography Scans in East Asian Population—A Retrospective Study. Diagnostics 2024, 14, 1792. https://doi.org/10.3390/diagnostics14161792
Ahn H-J, Byun S-H, Che S-A, Park S-Y, Yi S-M, Park I-Y, On S-W, Yang B-E. Morphological Analysis of the Anatomical Mandibular Lingual Concavity Using Cone Beam Computed Tomography Scans in East Asian Population—A Retrospective Study. Diagnostics. 2024; 14(16):1792. https://doi.org/10.3390/diagnostics14161792
Chicago/Turabian StyleAhn, Hee-Ju, Soo-Hwan Byun, Sung-Ah Che, Sang-Yoon Park, Sang-Min Yi, In-Young Park, Sung-Woon On, and Byoung-Eun Yang. 2024. "Morphological Analysis of the Anatomical Mandibular Lingual Concavity Using Cone Beam Computed Tomography Scans in East Asian Population—A Retrospective Study" Diagnostics 14, no. 16: 1792. https://doi.org/10.3390/diagnostics14161792






