Model for End-Stage Liver Disease Including Na, Age, and Sex Is Powerful Predictor of Survival in COVID-19 Patients on Extracorporeal Membrane Oxygenation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Patients
2.2. Study Design
2.3. Ethics
2.4. Data Analysis
3. Results
3.1. COVID-19 Patients
3.1.1. Patient Characteristics
3.1.2. MELD Scores
3.1.3. ECMO and Weaning
3.1.4. In-Hospital Mortality
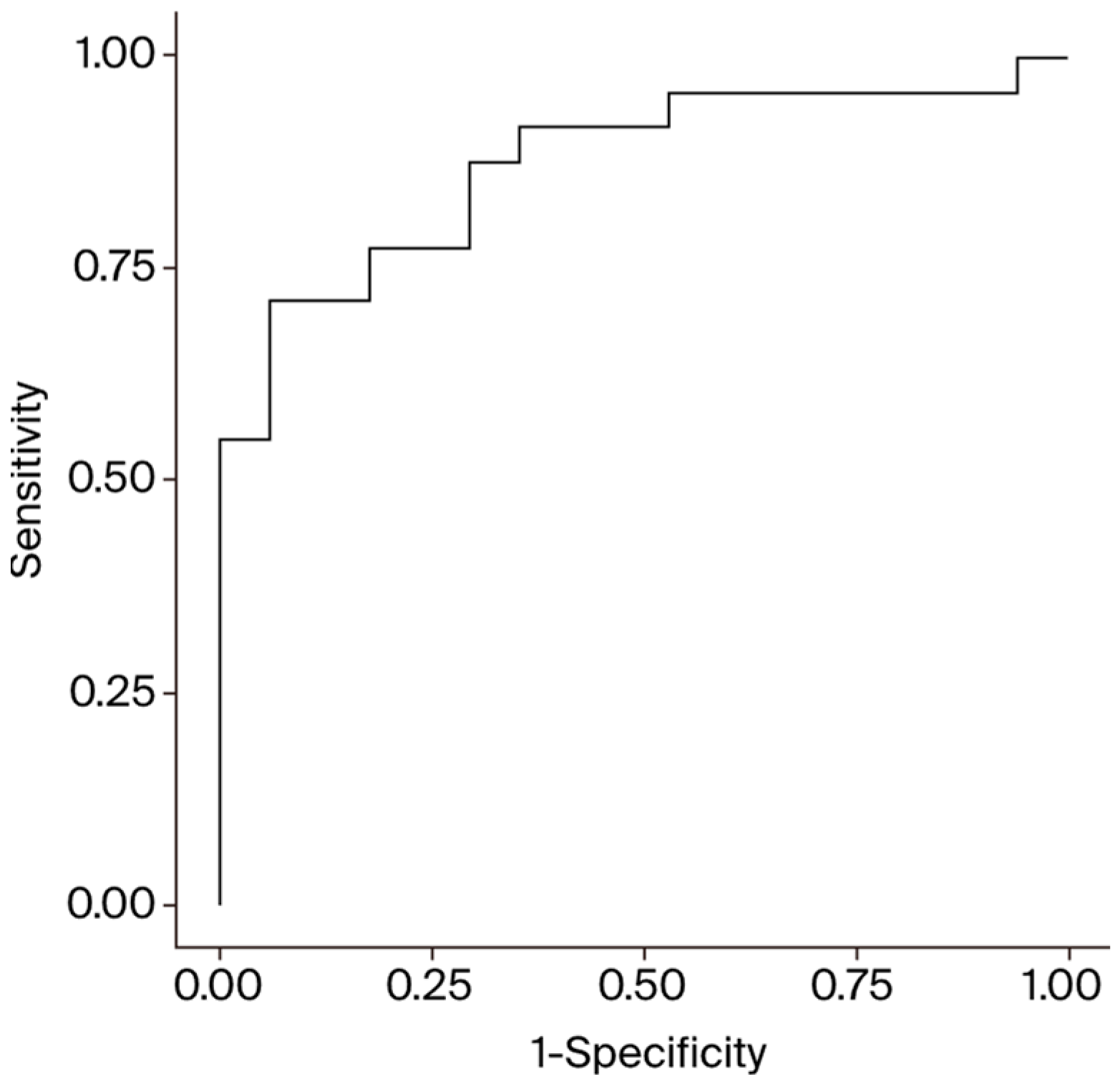
3.2. Non-COVID-19 Patients
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gajkowski, E.F.; Herrera, G.; Hatton, L.; Velia Antonini, M.; Vercaemst, L.; Cooley, E. ELSO Guidelines for Adult and Pediatric Extracorporeal Membrane Oxygenation Circuits. ASAIO J. 2022, 68, 133–152. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, K.; Antognini, D.; Combes, A.; Paden, M.; Zakhary, B.; Ogino, M.; MacLaren, G.; Brodie, D.; Shekar, K. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir. Med. 2020, 8, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Guo, Z.; Li, B.; Zhang, X.; Tian, R.; Wu, W.; Zhang, Z.; Lu, Y.; Chen, N.; Clifford, S.P. Extracorporeal Membrane Oxygenation for Coronavirus Disease 2019 in Shanghai, China. ASAIO J. 2020, 66, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Chommeloux, J.; Valentin, S.; Winiszewski, H.; Adda, M.; Pineton de Chambrun, M.; Moyon, Q.; Mathian, A.; Capellier, G.; Guervilly, C.; Levy, B.; et al. One-Year Mental and Physical Health Assessment in Survivors After ECMO for COVID-19-related ARDS. Am. J. Respir. Crit. Care Med. 2023, 207, 150–159. [Google Scholar] [CrossRef]
- Lorusso, R.; De Piero, M.E.; Mariani, S.; Di Mauro, M.; Folliguet, T.; Taccone, F.S.; Camporota, L.; Swol, J.; Wiedemann, D.; Belliato, M.; et al. In-hospital and 6-month outcomes in patients with COVID-19 supported with extracorporeal membrane oxygenation (EuroECMO-COVID): A multicentre, prospective observational study. Lancet Respir. Med. 2023, 11, 151–162. [Google Scholar] [CrossRef]
- Pappalardo, F.; Pieri, M.; Greco, T.; Patroniti, N.; Pesenti, A.; Arcadipane, A.; Ranieri, V.M.; Gattinoni, L.; Landoni, G.; Holzgraefe, B.; et al. Predicting mortality risk in patients undergoing venovenous ECMO for ARDS due to influenza A (H1N1) pneumonia: The ECMOnet score. Intensive Care Med. 2013, 39, 275–281. [Google Scholar] [CrossRef]
- Schmidt, M.; Zogheib, E.; Rozé, H.; Repesse, X.; Lebreton, G.; Luyt, C.E.; Trouillet, J.L.; Bréchot, N.; Nieszkowska, A.; Dupont, H.; et al. The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med. 2013, 39, 1704–1713. [Google Scholar] [CrossRef]
- Schmidt, M.; Bailey, M.; Sheldrake, J.; Hodgson, C.; Aubron, C.; Rycus, P.T.; Scheinkestel, C.; Cooper, D.J.; Brodie, D.; Pellegrino, V.; et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure: The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am. J. Respir. Crit. Care Med. 2014, 189, 1374–1382. [Google Scholar] [CrossRef]
- Roch, A.; Hraiech, S.; Masson, E.; Grisoli, D.; Forel, J.-M.; Boucekine, M.; Morera, P.; Guervilly, C.; Adda, M.; Dizier, S.; et al. Outcome of acute respiratory distress syndrome patients treated with extracorporeal membrane oxygenation and brought to a referral center. Intensive Care Med. 2014, 40, 74–83. [Google Scholar] [CrossRef]
- Hilder, M.; Herbstreit, F.; Adamzik, M.; Beiderlinden, M.; Bürschen, M.; Peters, J.; Frey, U.H. Comparison of mortality prediction models in acute respiratory distress syndrome undergoing extracorporeal membrane oxygenation and development of a novel prediction score: The prediction of Survival on ECMO Therapy-Score (PRESET-Score). Crit. Care 2017, 21, 301. [Google Scholar] [CrossRef]
- Pratt, E.H.; Morrison, S.; Green, C.L.; Rackley, C.R. Ability of the respiratory ECMO survival prediction (RESP) score to predict survival for patients with COVID-19 ARDS and non-COVID-19 ARDS: A single-center retrospective study. J. Intensive Care 2023, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Kamath, P.S.; Wiesner, R.H.; Malinchoc, M.; Kremers, W.K.; Therneau, T.M.; D’Amico, G.; Dickson, E.R.; Kim, W.R. A model to predict survival in patients with end-stage liver disease. Gastroenterology 2001, 120, 464–470. [Google Scholar] [CrossRef]
- Kalra, A.; Wedd, J.P.; Biggins, S.W. Changing prioritization for transplantation: MELD-Na, hepatocellular carcinoma exceptions, and more. Curr. Opin. Organ Transplant. 2016, 21, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Heuman, D.M.; Mihas, A.A.; Habib, A.; Gilles, H.S.; Stravitz, R.T.; Sanyal, A.J.; Fisher, R.A. MELD-XI: A rational approach to “Sickest first” liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liver Transplant. 2007, 13, 30–37. [Google Scholar] [CrossRef]
- Critsinelis, A.; Kurihara, C.; Volkovicher, N.; Kawabori, M.; Sugiura, T.; Manon, M.; Wang, S.; Civitello, A.B.; Morgan, J.A. Model of End-Stage Liver Disease-eXcluding International Normalized Ratio (MELD-XI) Scoring System to Predict Outcomes in Patients Who Undergo Left Ventricular Assist Device Implantation. Ann. Thorac. Surg. 2018, 106, 513–519. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, Y.X.; Seto, W.K.; Wu, M.Z.; Yu, Y.J.; Lam, Y.M.; Au, W.K.; Chan, D.; Sit, K.Y.; Ho, L.M.; et al. Prognostic value of hepatorenal function by modified model for end-stage liver disease (MELD) score in patients undergoing tricuspid annuloplasty. J. Am. Heart Assoc. 2018, 7, e009020. [Google Scholar] [CrossRef]
- Watanabe, S.; Kurihara, C.; Manerikar, A.; Thakkar, S.; Saine, M.; Bharat, A. MELD Score Predicts Outcomes in Patients Undergoing Venovenous Extracorporeal Membrane Oxygenation. ASAIO J. 2021, 67, 871–877. [Google Scholar] [CrossRef]
- Sern Lim, H. Baseline MELD-XI score and outcome from veno-arterial extracorporeal membrane oxygenation support for acute decompensated heart failure. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 82–88. [Google Scholar] [CrossRef]
- Ayers, B.; Wood, K.; Melvin, A.; Prasad, S.; Gosev, I. MELD-XI is predictive of mortality in venoarterial extracorporeal membrane oxygenation. J. Card. Surg. 2020, 35, 1275–1282. [Google Scholar] [CrossRef]
- Wernly, B.; Lichtenauer, M.; Franz, M.; Kabisch, B.; Muessig, J.; Masyuk, M.; Hoppe, U.C.; Kelm, M.; Jung, C. Model for end-stage liver disease excluding INR (MELD-XI) score in critically ill patients: Easily available and of prognostic relevance. PLoS ONE 2017, 12, e0170987. [Google Scholar] [CrossRef]
- Sandrio, S.; Thiel, M.; Krebs, J. The Outcome Relevance of Pre-ECMO Liver Impairment in Adults with Acute Respiratory Distress Syndrome. J. Clin. Med. 2023, 12, 4860. [Google Scholar] [CrossRef] [PubMed]
- Karnib, M.; Haraf, R.; Tashtish, N.; Zanath, E.; Elshazly, T.; Garcia, R.A.; Billings, S.; Fetros, M.; Bradigan, A.; Zacharias, M.; et al. MELD score is predictive of 90-day mortality after veno-arterial extracorporeal membrane oxygenation support. Int. J. Artif. Organs 2022, 45, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Xie, H.; Yang, F.; Wang, L.; Hou, X. Risk factors of acute renal injury and in-hospital mortality in adult patients with postcardiotomy cardiogenic shock requiring veno-arterial extracorporeal membrane oxygenation: Utility of MELD-XI score. Perfusion 2022, 37, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, Q.; Green, A.; Chandel, A.; Lantry, J.; Desai, M.; Simou, J.; Osborn, E.; Singh, R.; Puri, N.; Moran, P.; et al. Impact of Noninvasive Respiratory Support in Patients with COVID-19 Requiring V-V ECMO. ASAIO J. 2022, 68, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Fuset-Cabanes, M.P.; Hernández-Platero, L.; Sabater-Riera, J.; Gordillo-Benitez, M.; Di Paolo, F.; Cárdenas-Campos, P.; Maisterra-Santos, K.; Pons-Serra, M.; Sastre-Pérez, P.; García-Zaloña, A.; et al. Days spent on non-invasive ventilation support: Can it determine when to initiate VV- ECMO? Observational study in a cohort of Covid-19 patients. BMC Pulm. Med. 2023, 23, 310. [Google Scholar] [CrossRef]
- Sharma, J.; Rajput, R.; Bhatia, M.; Arora, P.; Sood, V. Clinical Predictors of COVID-19 Severity and Mortality: A Perspective. Front. Cell. Infect. Microbiol. 2021, 11, 674277. [Google Scholar] [CrossRef]
| Variable | MELD [9] | MELD Na [10] | MELD XI [11] |
|---|---|---|---|
| Bilirubin | x | x | x |
| INR | x | x | |
| Creatinine | x | x | x |
| Sodium | x |
| Variable | All (n = 66) |
|---|---|
| Sex (% male) | 83.3% |
| Age in years, median (IQR) | 58.5 (51–62) |
| BMI, median (IQR) | 29.0 (26–32) |
| History of CPR (%) | 3.0% |
| History of MI (%) | 1.5% |
| Active smoker (%) | 4.5% |
| Diabetes (%) | 18.2% |
| Hyperlipidemia (%) | 4.5% |
| Hypertension (%) | 45.5% |
| COPD (%) | 10.6% |
| Dialysis at admission (%) | 16.7% |
| Ventilated at admission (%) | 72.7% |
| Symptoms to ECMO in days, median (IQR) | 18.0 (11–21) |
| Variable | Survivors (n = 17) | Non-Survivors (n = 49) | p-Value |
|---|---|---|---|
| MELD, median (IQR) | 9.1 (3.8–12.7) | 15.5 (8.6–22.6) | 0.006 * |
| MELD Na, median (IQR) | 10.6 (4.8–13.6) | 15.7 (11.5–23.6) | 0.005 * |
| MELD XI, median (IQR) | 8.2 (5.7–13.4) | 13.9 (8.2–22.8) | 0.020 * |
| Creatinine (mg/dL), median (IQR) | 0.9 (0.6–1.2) | 1.5 (0.9–2.4) | 0.008 * |
| Bilirubin (mg/dL), median (IQR) | 0.5 (0.4–1.0) | 0.80 (0.5–1.7) | 0.124 |
| Sodium (mmol/L), median (IQR) | 136 (135–140) | 136 (134–139) | 0.621 |
| INR, median (IQR) | 1.2 (1.2–1.4) | 1.3 (1.2–1.5) | 0.727 |
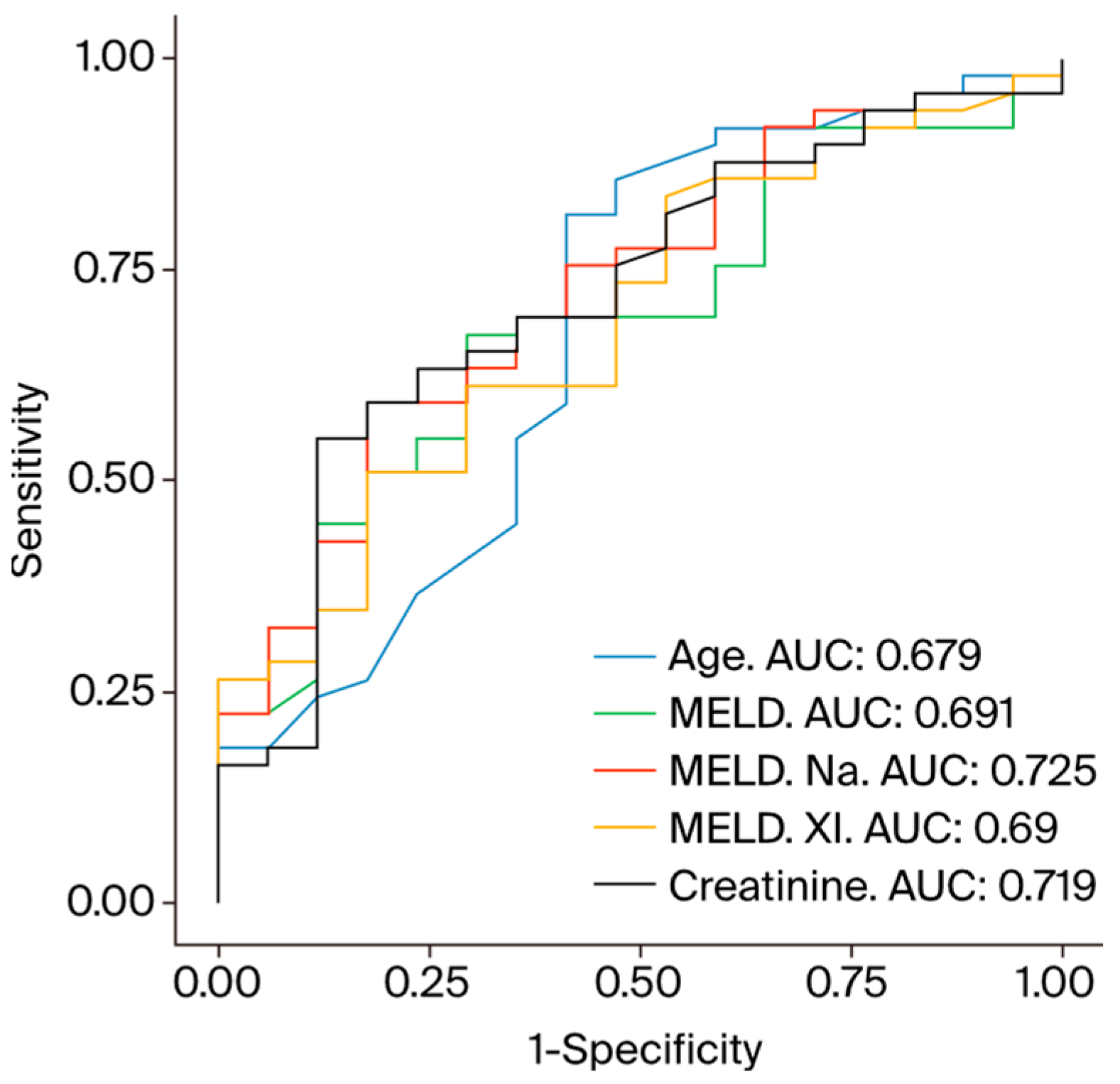
| Variable | AUC | p-Value | Optimal Cut-Off | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Age (years) | 0.680 | 0.014 * | 53.3 | 58.8% | 81.6% |
| MELD | 0.692 | 0.010 * | 10.7 | 70.6% | 67.3% |
| MELD Na | 0.725 | 0.003 * | 13.8 | 82.4% | 59.2% |
| MELD XI | 0.690 | 0.010 * | 13.9 | 82.4% | 51.0% |
| Creatinine (mg/dL) | 0.719 | 0.004 * | 1.4 | 88.2% | 55.1% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jenkins, F.S.; Morjan, M.; Minol, J.-P.; Yilmaz, E.; Dalyanoglu, I.; Immohr, M.B.; Korbmacher, B.; Boeken, U.; Lichtenberg, A.; Dalyanoglu, H. Model for End-Stage Liver Disease Including Na, Age, and Sex Is Powerful Predictor of Survival in COVID-19 Patients on Extracorporeal Membrane Oxygenation. Diagnostics 2024, 14, 1954. https://doi.org/10.3390/diagnostics14171954
Jenkins FS, Morjan M, Minol J-P, Yilmaz E, Dalyanoglu I, Immohr MB, Korbmacher B, Boeken U, Lichtenberg A, Dalyanoglu H. Model for End-Stage Liver Disease Including Na, Age, and Sex Is Powerful Predictor of Survival in COVID-19 Patients on Extracorporeal Membrane Oxygenation. Diagnostics. 2024; 14(17):1954. https://doi.org/10.3390/diagnostics14171954
Chicago/Turabian StyleJenkins, Freya Sophie, Mohammed Morjan, Jan-Philipp Minol, Esma Yilmaz, Ismail Dalyanoglu, Moritz Benjamin Immohr, Bernhard Korbmacher, Udo Boeken, Artur Lichtenberg, and Hannan Dalyanoglu. 2024. "Model for End-Stage Liver Disease Including Na, Age, and Sex Is Powerful Predictor of Survival in COVID-19 Patients on Extracorporeal Membrane Oxygenation" Diagnostics 14, no. 17: 1954. https://doi.org/10.3390/diagnostics14171954





