Abstract
The aim of the study was to collect data about the prevalence and risk factors of apical periodontitis in a population of endodontically treated patients. The study group included 151 patients (52 males, 99 females; mean age 48.36 ± 15.708 yrs.) with 391 endodontically treated teeth (mean follow-up of 5.25 ± 1.759 yrs.). According to the initial tooth diagnosis, root-filled teeth were divided into Group A, root-filled teeth treated for pulpitis or for the purpose of prosthetic pulpectomies (vital pulp group), and Group B, root-filled teeth with non-vital pulp (necrotic pulp). Clinical and radiographic evaluation of the root and its periapical area were performed to establish the success/failure of endodontic therapy, the quality of the root canal fillings (length, density, taper), and coronal restoration. The presence of recurrent caries, periodontal pathology, or endo-periodontal lesions were also recorded. Univariate and multivariate analyses were used to determine the risk factors for apical periodontitis and calculate their odds ratios (ORs). For the root-filled vital pulp tooth group, the highest risks for apical periodontitis are associated with inadequate homogeneity (OR 30.938), periodontitis (OR 9.226), and over-filling (OR 8.800). For the root-filled non-vital pulp tooth group, the highest risks are associated with periodontitis (OR 4.235) and age over 60 yrs. (OR 4.875). For the necrotic pulp tooth group, multivariate analysis identified an age > 60 yrs., filled molars, intracanal posts, poor coronal restoration quality, under-filling, and periodontitis as significant combined risk factors. Inadequate root canal filling and periodontitis in both groups were risk factors associated with most cases of apical periodontitis. Other risk factors include age > 60 yrs., poor coronal restoration quality, and the presence of intracanal posts in root-filled teeth with necrotic pulp.
1. Introduction
The uncontrolled spread of pulp inflammation can progress to more advanced pulpitis, and potentially involving the apical tissues and requiring extirpation to alleviate pain, followed by nonsurgical root canal treatment to preserve the health of the apical tissues [1]. While pulp necrosis without microbial contamination often goes unnoticed, eventually pulpal necrosis and infection lead to apical inflammation, necessitating nonsurgical root canal treatment to manage the infection in the endodontic space. Early and accurate diagnostic may be challenging in this stage. Also, root canal treatment may be required for treatment of vital teeth as part of a prosthodontic plan or in cases of noncontaminated pulp necrosis resulting from traumatic dental injuries [2].
Apical periodontitis is the result of the complex processes generated by microbial factors penetration into apical areas and host defense reactions as a result of this invasion of the peri-radicular tissues [3]. Apical periodontitis can result from teeth with necrotic pulp or endodontically treated teeth and is an important cause of reoccurrence of endodontic infection and subsequent tooth extraction. Teeth with failed endodontic treatment present bacterial biofilm next to or at distance from the apical foramen. While intra-radicular biofilm can be effectively cleaned by using combination of ultrasounds and NaOCl 2% or lasers [4], extra-radicular biofilm, resistant to antibacterial agents [5] is an important factor of failed endodontic treatment this biofilm being detected in vitro on the apical external surface in teeth with necrotic pulp and radiographically visible periapical lesions [6].
Various non-surgical techniques [7,8,9,10,11] as well as surgical approach can be used to eliminate the bacterial infection of the endodontic space [12,13]. Asymptomatic periapical lesions in teeth with poor quality endodontic treatments usually harbor anaerobic microorganisms, in similar compositions with that of the infected and untreated teeth [14].
The signs of healing processes following treatment of apical periodontitis are as follows: repair process in apical area, absence of the increase in radiolucency in the peri-radicular areas, biological sealing, or even the presence of a fibrous capsule [15]. Also, a successful endodontic therapy is characterized by the absence of pain, proper endodontic sealing, adequate coronal sealing, as well as the presence of healing periapical processes [16]. Successful outcome of teeth with apical periodontitis ranges from 86% to 98% [17].
Despite the improvement of awareness, knowledge, techniques and materials in endodontic therapy, a 2% rate of annual loss of root-filled teeth [18] proves the relevance of various risk factors contributing to failure (newly developed or persistent periapical radiolucency around a root-filled tooth apex) [19].
Some of the factors influencing the outcome of endodontic treatment include the use of dam, intraoperative procedures (i.e., irrigation method), the extent of apical preparation, the use of antibacterial medications within the canal, as well as the number of sessions required to finish the treatment. However, the results can be impacted by the pre-operative symptoms, severity of bone loss in the apical areas, the anatomical complexity of the canal’s apical area, as well as the virulence and persistence of the bacterial infection [19].
The dynamic of host/infection interaction is influenced both by intra-operative therapeutic factors to sustain a microbial ecological shift and the role of the tooth and its marginal sealing to resist infection recurrence [14]. Regardless of factors implied, apical periodontitis is due bacteria and their byproducts present within the root canal system leading to host’ immune response [20]. The prevalence of failures in the endodontic therapy ranges from 32.8% [21] to 39% [22], 39.5% [23], 41% [24], and 72.1% [25].
The non-surgical treatment is recommended both for medium and severe apical periodontitis as the bone extension of the apical periodontitis is not correlated with the post-treatment evolution of the healing processes [23]. The decisions of monitorization and delay of endodontic treatment, retreatment, or extraction are influenced by the experience and competencies of the practitioner, tooth prosthetic value, aesthetic demands, cost/benefits analysis, patient’ systemic status, as well as the patient preferences [24,25]. The diagnostic of apical periodontitis in root-filled tooth may require retreatment which can decrease the success rate of the endodontic therapy [25], due to presence of resistant biofilm on external radicular surface [25,26].
Risk factors are those variables or conditions that increase the likelihood of a person developing a disease. The onset of diseases is influenced by a multitude of risk factors, which often intersect or overlap with each other [17,27,28,29,30]. These independent variables must be considered in the decision of non-surgical treatment in apical periodontitis. When tooth restorability is feasible, in routine dental practice most dentists and patients agree with the maintenance of a root-filled tooth with apical periodontitis to avoid further dental tissues degradation [17].
The aim of study was to assess and analyze the prevalence and risk factors of apical periodontitis in a population of endodontically treated patients to evaluate and better manage this category of patients in the context of a complex oral rehabilitation.
2. Materials and Methods
The study group included 151 patients (52 males, 99 females; mean age 48.36 ± 15.708 yrs.), with 391 endodontically treated teeth (mean follow-up of 5.25 ± 1.759 yrs.). The patients attended a private dental clinic for the first time between the years 2014 and 2022. This study adhered to the principles outlined in the Declaration of Helsinki and was approved by the Ethics Department of the University of Medicine and Pharmacy “Grigore T. Popa” (Nr. 334/16.07.2023) in Iasi. All patients participating in the study provided informed consent by signing a consent form approved by the ethics committee of the University of Medicine and Pharmacy “Grigore T. Popa” in Iasi. The inclusion criteria were as follows: root-filled teeth with at least 24 months post-treatment; root canal fillings following pulpectomy (pulpitis, prosthetic pulpectomies) or endodontic treatment for necrotic pulp; all root-filled teeth had healthy periapical status (PAI 1, according to the Orstavik periapical index) [31] at the moment of the initiation of endodontic therapy; teeth with a composite resin filling or full coverage crown. The exclusion criteria were as follows: a systemic pathology that can negatively influence periapical healing (uncontrolled diabetes as well as its complications, osteoporosis, rheumatoid arthritis, head and cervical chemotherapy or radiotherapy, autoimmune diseases); medication administration (immunosuppressive medication, corticosteroids, bisphosphonates); subjects with teeth that have undergone apical resection.
According to the initial endodontic diagnosis, root-filled teeth were divided into two groups: Group A, vital pulp teeth (teeth treated for pulpitis, prosthetic pulpectomies) (n = 127), and Group B, necrotic pulp teeth (n = 391).
Table 1 exposes the social and demographic parameters of the subjects, while the study group variables are described in Table 2.

Table 1.
Description of the studied population.

Table 2.
Description of the study group.
All patients were evaluated by one calibrated experienced clinician (S.M.). The independent variables assessed as risk factors for endodontic therapy failure (presence of apical periodontitis) were as follows: dental groups, location (maxillary/mandibular), coronal restoration type (amalgam/composite fillings, full coverage crown), presence of intracanal posts, the quality of the root-canal fillings, the quality of the coronal restoration marginal sealing, recurrent caries, periodontal status, endo-periodontal lesions, the presence of an opposing tooth.
The Orstavik periapical index (PAI) [31] was used to assess periapical statuses in the study groups. In multi-rooted teeth, the worst PAI score was considered.
Endodontic therapy success was defined by the absence of clinical symptoms, radiographic images with rarefaction of the periapical area, and a periodontal ligament with normal width or that was slightly widened [32].
Failure of the endodontic therapy was defined by the clinical signs and symptoms of apical inflammation, widening of the periodontal ligament, or the presence of any periapical radiolucency with PAI > 2 [32].
The statuses of the root-canal fillings and coronal restoration marginal sealing were assessed as ‘adequate’ or ‘poor’ using the radiographic criteria shown in Table 3 [25,31].

Table 3.
Criteria for the assessment of root canal fillings and coronal restorations [25,31].
The root-canal filling length was measured on periapical radiographs to the nearest 0.1 mm. The assessed parameters of the endodontic treatment were as follows: length (adequate; poor); density (adequate; poor); conicity (adequate; poor).
The criteria for the assessment of the quality of the root canal fillings (length, density, taper) as well as the criteria for coronal restoration quality are shown in Table 3. Additionally, any tooth with fractured or absent coronal restoration was classified in the category of poor coronal restoration.
The presence of recurrent caries was diagnosed both in clinical examination and in radiographic images.
Periodontitis of an endodontically treated tooth was clinically diagnosed according to the 2018 AAP/EFP classification of periodontal and peri-implant diseases.
Statistical analysis. The statistical tests were performed in SPSS 29.0 software. Frequency distribution was used to characterize the qualitative variables. Descriptive statistics (mean values, standard deviations) were used to characterize the quantitative variables. The Chi-squared test was used to analyze the relationships between the socio-demographic variables, clinical and radiographic features, and the periapical status; the identified risk factors were characterized by calculating the associated ORs (odds ratios) using a model of univariate binary logistic regression. Their combined action over the periapical status was evaluated further using a multivariate binary logistic regression. The logistic regression models were generated using the Enter method, and their adequacy was evaluated using the Hosmer–Lemeshow goodness-of-fit test. p < 0.05 was the threshold for significance; p < 0.01 was evaluated as statistically highly significant.
3. Results
Apical periodontitis was diagnosed in 35 root-filled teeth in the vital pulp group (27.7% AP prevalence) and 146 teeth in the necrotic pulp group (55.3% AP prevalence). Figure 1a–d. exposes teeth with poor root-canal fillings diagnosed with apical periodontitis. Table 4 exposes the success/failure rates of the endodontic treatment, related to the assessed independent variables, for Group A (vital pulp) and Group B (necrotic pulp). Table 5 shows the univariate and multivariate analysis of the independent variables assessed for risk of apical periodontitis in Group A (vital pulp) and Group B (necrotic pulp).
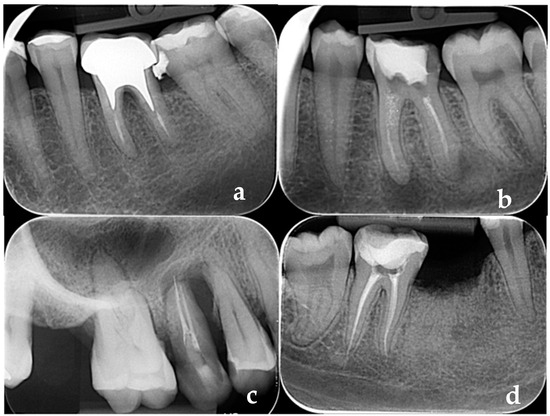
Figure 1.
(a–d) Apical periodontitis in teeth with poor quality root-canal fillings: (a,b) short fillings; (c,d) over-fillings.

Table 4.
Clinical and radiographic success/failure (absence/presence of apical periodontitis) according to assessed variables.

Table 5.
Univariate and multivariate logistic regression for the association of study variables with periapical status. (prevalence of AP and OR in relation to the assessed parameters).
Figure 1a–d illustrates teeth with poor root-canal fillings diagnosed with apical periodontitis.
The prevalence of apical periodontitis in both study groups is exposed in Table 4. Regarding the effectiveness of the endodontic treatment in relation to gender, AP prevalence was higher in the root-filled teeth with necrotic pulp (52.8%-males, 56.3%-females) when compared with the vital pulp group (20.9%-males, 31%-females). In the necrotic pulp group, root-filled teeth in patients > 60 yrs. had significant higher AP prevalence (81.8%) when compared with other age groups (p = 0.024*); significant differences were not found between age groups in the vital pulp tooth group. Regarding the root-filled tooth location, molars (63.4%) had significantly higher AP prevalence than premolars (44.3%) in the necrotic pulp group, while the maxillary/mandibular location was not associated with any significant difference in both groups (p > 0.05). The follow-up duration (2–4 yrs. vs. 5–9 yrs.) was not significantly associated with AP prevalence (p > 0.05). In the vital pulp tooth group, root-filled teeth reconstructed with composite resin restorations had a higher AP prevalence rate (50%) than those with full coverage crowns (23.4%), with significant statistical difference (p = 0.014 *); this difference was not found in the necrotic pulp group (p > 0.05). Within necrotic pulp group teeth, reconstruction with intra-canal posts was significantly associated with AP (66.3%) when compared with teeth without intra-canal posts (33.3%) (p = 0.007 **). Significant statistical difference (p = 0.007 **) in AP prevalence was found in the vital pulp tooth group between root-filled teeth with good-quality coronal restoration (15.8%) and poor-quality coronal marginal sealing (37.1%). In the vital pulp tooth group, 42.1% of root-filled teeth with low-quality root canal fillings were diagnosed with AP, while all teeth with adequate endodontic treatments were diagnosed with healthy periapical status. In the necrotic pulp group, 60.4% of root-filled teeth with inadequate root canal fillings were diagnosed with AP, while only 28.6% of teeth with adequate root canal fillings had apical pathology (p ≤ 0.001 **). Related to the categories of technical errors, all types of inadequate root canal fillings (over-fillings, under-fillings, inadequate homogeneity, inadequate taper) lead to significant statistical differences in AP prevalence (in both groups) when compared with adequate root canal fillings (p < 0.001 **). Root-filled teeth with caries adjacent to coronal restorations in the necrotic pulp group had significantly higher AP prevalence (60.7%) when compared with those without caries adjacent to coronal restorations (45.8%) (p = 0.019 *). Also, teeth with caries adjacent to coronal restorations in the vital pulp group had significantly higher AP prevalence (42.4%) when compared with those without caries adjacent to coronal restorations (11.5%) (p < 0.001 **). Periodontal pathology of the root-filled teeth in the necrotic pulp group was associated with significantly higher AP prevalence (74.8%) when compared to periodontally healthy root-filled teeth (41.2%) (p < 0.001 **). Also, periodontal pathology of the teeth in the vital pulp group was associated with significant higher AP prevalence (42.5%) when compared to periodontally healthy teeth (7.4%) (p < 0.001 **). Root-filled teeth with endo-periodontal lesions had 100% prevalence of apical periodontitis in both groups. The presence of an antagonist tooth in occlusal contact with a root-filled tooth was not associated with apical periodontitis (p > 0.05).
Univariate regression analysis showed that presence of composite resin filling, poor coronal restoration quality, inadequate root canal filling quality (under-filling, over-filling, inadequate homogeneity), the presence of an opposing tooth, the presence of caries adjacent to coronal restorations, and presence of periodontitis, for the vital pulp tooth group, were identified as risk factors associated with a higher rate of apical periodontitis (Table 5). The highest risks are associated with inadequate homogeneity (OR 30.938), periodontitis (OR 9.226), and over-filling (OR 8.800). For the vital pulp tooth group, multivariate analysis did not prove other associations. In vital pulp teeth, a combination of the identified risk factors will not significantly influence the presence of apical periodontitis. The presence of these combined risk factors results in a greater chance of apical periodontitis when compared to teeth with adequate coronal restoration, adequate root canal filling quality, and healthy gingival status. Univariate regression analysis in the necrotic pulp group showed that an age over 60 yrs., filled molars, the presence of intracanal posts, poor coronal restoration quality, inadequate root canal filling quality (under-filling, over-filling, inadequate homogeneity), the presence of caries adjacent to coronal restorations or periodontitis, and endo-periodontal lesions were identified as risk factors associated with a higher rate of apical periodontitis. The highest risks are associated with periodontitis (OR 4.235) and an age over 60 yrs. (OR 4.875). For the necrotic pulp tooth group, multivariate analysis identified as significant combined risk factors an age over 60 yrs., filled molars, intracanal posts, poor coronal restoration quality, under-filling, and periodontitis. The presence of these combined risk factors results in a greater chance of apical periodontitis than root-filled teeth treated for necrotic pulp in patients with an age under 60 yrs., filled premolars, adequate coronal restoration, an absence of caries adjacent to coronal restorations, adequate root canal filling quality, and healthy gingival status (Table 5).
4. Discussion
Our study analyzed the influence of various potential risk factors on the prevalence of apical periodontitis related to the treatment of teeth with vital pulp (pulpitis, prosthetic pulpectomies) or necrotic pulp. Various systemic conditions (chronic debilitation, uncontrolled diabetes, metabolic disorders, osteoporosis) can decrease the ability of the immune system to heal the periapical tissues and thus increase the failure rate even after proper endodontic treatment [33]. In our study, we aimed to focus on some risk factors that can be controlled by dentists; thus, the presence of systemic pathologies that can be related to disrupted healing processes was an exclusion criterion.
According to logistic regression analysis, socio-demographic variables of the patients with root-filled teeth were not found to be associated with apical periodontitis in root-filled teeth with vital pulp before endodontic treatment, while the age group over 60 yrs. is significantly associated with apical periodontitis in teeth treated for necrotic pulp. Data regarding the relation between the failure of endodontic treatment and sociodemographic parameters are controversial. Frisk et al. (2015) reported that age was found to be a predictor, while gender was not associated with apical periodontitis [34]. Hussain et al. (2024) found gender (females) to be a significant predictor, while age was not associated with the presence of apical periodontitis [35].
Molars had significantly higher AP prevalence than premolars in root-filled teeth treated for pulp necrosis. Their complex anatomy, root canal curvatures, and ramifications complicate both the biochemical cleaning stage and the root canal shaping and filling [36]. Microcracks and even root fractures can occur in teeth where root canals are prepared using multi-rotary devices. However, some multi-file rotary systems have less risk of microcracks than others. Proper selection of a multi-rotary system and endodontist experience can contribute to a significant decrease in tooth fracture risk [37]. Regarding the use of prosthetic crowns versus composite resin fillings, a research group found low quality evidence for the effects of crowns when compared to conventional fillings for the coronal restoration of root-filled teeth [38].
In our study, direct composite restoration of root-filled teeth treated for pulpitis or prosthetic pulpectomies significantly increased the rate of apical periodontitis. Proper marginal sealing is crucial for preventing microleakage and ensuring the longevity of the restoration and endodontic treatment, as it minimizes the risk of caries adjacent to the restorations, especially in Class II composite resin restorations [39,40]. Root-filled teeth restored with indirect restorations have a better survival rate when compared to teeth restored with direct restorations, but the difference was not significant, and the type of coronal restoration was not considered a risk factor for apical periodontitis [17]. However, Dawson et al. (2016) did not find statistical differences between the rates of apical periodontitis in root-filled teeth restored with resin composite, amalgam, or crowns [41].
However, intracanal posts placed to increase retention of composite fillings or complete coverage crowns were found to be risk factors for apical periodontitis both in univariate (OR 2.114) and multivariate analyses (OR 2.177) of the root-filled teeth treated for pulp necrosis. The relation between the presence of an intracanal post and apical periodontitis is controversial. A research group also reported a 16% increase in apical periodontitis rates in root-filled teeth restored with composite resin restorations or complete coverage crowns and intracanal posts [42].
Adequate root canal filling can provide complete sealing in order to hinder the communication between the endodontic space and the periapical tissue [9]. In our study, the quality of root canal fillings (length, homogeneity, taper) was found to be a risk factor of apical periodontitis in univariate and multivariate analyses both for root-filled teeth treated for pulpitis or prosthetic pulpectomies and teeth treated for pulp necrosis. Hussain et al. (2024) also reported that poor root canal fillings had a 7.92 times higher risk of apical periodontitis when compared to root-filled teeth with proper-quality endodontic treatment [35]. We found that root-filled teeth with canal overfilling had an 11.214 times higher risk of the presence of apical periodontitis; teeth with poor density of the root-canal filling had a 4.824 times higher risk of endodontic treatment failure; and short fillings had a 1.733 times higher risk of apical periodontitis when compared to root-filled teeth with adequate root canal fillings. A research group found short fillings to have a higher risk of apical periodontitis (OR 2.77), while canal overfilling had a significantly lower risk of apical periodontitis (OR 1.08) when compared to the result reported by our study [43]. Root canal filling quality was also found to be a predictor of apical periodontitis by Frisk et al. (2015) [34]. Root canal fillings at 1–2 mm distance to apex had significantly higher success rates when compared with root-filled teeth with short fillings and over-fillings [44,45]. Poor homogeneity of the root canal filling and canal overfilling are significant risk factors for apical periodontitis [25,46], while the rate of apical periodontitis increases significantly in teeth with short root canal fillings when compared to teeth with proper root canal fillings [25,47,48].
In univariate analysis and multivariate analysis, we found poor coronal marginal sealing to be a risk factor for apical periodontitis both for the vital pulp group and teeth with necrotic pulp before the endodontic treatment. Multivariable multilevel logistic regression performed by Keratiotis et al. (2024) revealed that adequate density of the root canal fillings and coronal restorations with adequate quality reduced the likelihood of apical periodontitis [49]. Other previous studies found the coexistence of poor coronal restorations with poor root canal fillings to be a predictor of apical periodontitis [24,48,49,50,51,52,53,54]. AP was significantly associated with inadequacy of root canal filling but not with inadequacy of coronal restoration [55].
These results show that failure to achieve elimination of bacterial infection from the endodontic space, tooth cavities, failure to achieve asepsis during dental procedures, unacceptable root canal obturation, and re-infection because of unsound coronal restoration during or after root canal treatment are the main reasons for formation of periapical pathology.
The presence of caries adjacent to coronal restorations was found to be a risk factor for apical periodontitis in the root-filled teeth with vital pulp before endodontic therapy. This pathology is related both to patient cariogenic risk and poor coronal marginal sealing [56]. Various research groups have reported controversial data about the role of caries adjacent to coronal restorations in teeth with adequate root canal fillings. The presence of recurrent caries was not associated with apical periodontitis in one study [34], while another research group found recurrent caries to be a risk factor for endodontic treatment failure [48].
The presence of the periodontal pathology (BOP and PPD ≥ 3 mm) was a significant risk factor for endodontic failure in our study (OR 3.403 in univariate analysis, OR 3.334 in multivariate analysis). Periodontal pathology can pose significant additional risks for the longevity of affected teeth and can worsen a tooth’s overall long-term prognosis [57,58]. This can be remedied through thorough root debridement and non-surgical therapy and surgical complex therapy [59,60]. Adjunctive periodontal therapy, such as photo-disinfection, laser, application of local anti-inflammatory and antibiotic substances, etc., can also bring great benefits to patients with impaired wound healing such as smokers or patients with systemic conditions [61,62,63,64,65,66,67,68]. The periodontal–endodontic pathway can spread infection from periodontal pockets in apical areas in teeth with poor root canal fillings. Marginal bone loss was associated with apical periodontitis in root-filled teeth, while the rate of apical periodontitis was significantly lower in patients that had received periodontal treatment when compared with untreated periodontal patients [69,70,71]. Ruiz et al. observed that the risk of developing AP in endodontically treated teeth is 5.19 times higher for patients with periodontal disease compared with patients without periodontal disease. Severe periodontal disease was also a significant risk factor in a study that investigated the relation between sociodemographic/clinical factors and apical periodontitis [70]. Kato et al. (2020) found a significant relation between poor-quality root canal fillings, BOP, and periodontal pocket depth [72].
The presence of endo-periodontal lesions can worsen the prognosis of a previously correctly treated tooth, and the complex retreatment does not guarantee success [7]. The local and systemic inflammatory load is elevated in patients with endo-periodontal syndrome, especially in those with severe periodontitis. The authors state that these individuals have a much higher risk of developing and worsening of systemic maladies, such as diabetes mellitus, since local inflammation can affect the general inflammatory status [73].
If endodontic pathology reoccurs, loco-regional complications can appear, such as odontogenic sinusitis, thus leading to a more radical treatment plan and the extraction of the causing tooth [74].
Radiographic diagnostics had lower sensitivity in the diagnosis of early periapical lesions when compared to cone-beam CT in evaluation of periapical status [74,75,76,77,78,79]. The AI demonstrated high sensitivity and high specificity in detecting apical periodontitis in CBCT images but lower sensitivity in OPG images. [80]. Thus, root-filled teeth with incipient periapical lesions undetected in digital radiographic images were excluded from the study group.
While prospective studies can assess the effectiveness of irrigating solutions in biochemical and mechanical disinfection of the endodontic space, smear-layer removal, and the proper use of intracanal dressing, these are risk factors that cannot be assessed in longitudinal studies. Failure to achieve elimination of bacterial infection from the endodontic space during chemo-mechanical preparation as well as failure to achieve asepsis during dental procedures are correlated to the presence of apical periodontitis [45].
The use of a dam to limit microbial contamination is essential for successful endodontic treatment [81]. Also, the use of additional methods for disinfection of the endodontic canals, such as photoactivation or laser, has been proven useful and could be considered as a viable adjuvant therapy [82].
Our paper highlights some differences in AP prevalence and risk factors between root-filled teeth with vital pulp and necrotic pulp preoperatively. Thus, the higher prevalence of endodontic treatment failure in root-filled teeth treated for necrotic pulp proves that treatment should not be delayed in cases of irreversible pulpal disease or necrotic pulp, as timely intervention is more effective in preventing rather than resolving apical periodontitis. Also, the clinical approach for these two conditions must adhere to standard guidelines to prevent apical periodontitis by maintaining an aseptic technique and avoiding infection through coronal leakage [2].
Some limitations of the study are the more ample division of possible therapeutic situations, the use of CBCT at baseline and retreatment, the use of AI in the interpretation of radiographic images, and the more equal distribution of vital pulp teeth and necrotic pulp teeth (at initial diagnosis).
Further studies must also investigate other factors such as the enlargement of the apical foramen, zips, ledges, perforations, and transport of the root canals.
5. Conclusions
Most cases of apical periodontitis were associated with inadequate root canal filling and periodontitis in root-filled teeth with vital and necrotic pulp. Other significant risk factors include an age > 60 yrs., poor coronal restoration quality, and the presence of intracanal posts in root-filled teeth with necrotic pulp. The analysis of patient risk factors in the planning of the endodontic treatment can decrease the burden of apical periodontitis. Care should be taken concerning the quality of root canal fillings, the seal of the coronal cavity, and periodontal infection control.
Author Contributions
Conceptualization, M.S. and A.M.; data curation, C.G., C.A., C.C. and T.H.; formal analysis, C.D.; methodology, M.S. and A.M.; resources, M.S. and A.M.; software, C.D.; supervision, M.S. and M.-A.M.; validation A.M.; visualization, M.-A.M.; writing—original draft preparation, M.-A.M. and C.T.; writing—review and editing, M.-A.M. and C.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Medicine and Pharmacy “Grigore T. Popa” in Iasi (Nr. 334/16.07.2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting reported results can be provided by the corresponding authors upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ricucci, D.; Loghin, S.; Siqueira, J.F., Jr. Correlation between clinical and histologic pulp diagnoses. J. Endod. 2014, 40, 1932–1939. [Google Scholar] [CrossRef] [PubMed]
- Rossi-Fedele, G.; Ng, Y.L. Effectiveness of root canal treatment for vital pulps compared with necrotic pulps in the presence or absence of signs of periradicular pathosis: A systematic review and meta-analysis. Int. Endod. J. 2023, 56 (Suppl. S3), 370–394. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.F.A.; Herrera, D.R. Etiologic role of root canal infection in apical periodontitis and its relationship with clinical symptomatology. Braz. Oral Res. 2018, 32 (Suppl. S1), e69. [Google Scholar] [CrossRef] [PubMed]
- Josic, U.; Mazzitelli, C.; Maravic, T.; Fidler, A.; Breschi, L.; Mazzoni, A. Biofilm in Endodontics: In Vitro Cultivation Possibilities, Sonic-, Ultrasonic- and Laser-Assisted Removal Techniques and Evaluation of the Cleaning Efficacy. Polymers 2022, 14, 1334. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.J.; Wang, J.D. Bacterial biofilm on the apical external root surfaces of human teeth associated with chronic periradicular lesions. J. Peking Univ. Health Sci. 2009, 41, 571–574. [Google Scholar]
- Leonardo, M.R.; Rossi, M.A.; Silva, L.A.; Ito, I.Y.; Bonifácio, K.C. EM evaluation of bacterial biofilm and microorganisms on the apical external root surface of human teeth. J. Endod. 2002, 28, 815–818. [Google Scholar] [CrossRef]
- Karamifar, K.; Tondari, A.; Saghiri, M.A. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur. Endod. J. 2020, 5, 54. [Google Scholar] [CrossRef]
- Abusrewil, S.; Alshanta, O.A.; Albashaireh, K.; Alqahtani, S.; Nile, C.J.; Scott, J.A.; McLean, W. Detection, treatment and prevention of endodontic biofilm infections: What’s new in 2020? Crit. Rev. Microbiol. 2020, 46, 194–212. [Google Scholar] [CrossRef]
- Jurič, I.B.; Anić, I. The Use of Lasers in Disinfection and Cleanliness of Root Canals: A Review. Acta Stomatol. Croat. 2014, 48, 6–15. [Google Scholar] [CrossRef]
- Giuroiu, C.L.; Andrian, S.; Stoleriu, S.; Scurtu, M.; Tanculescu, O.; Poroch, V.; Salceanu, M. The combination of diode laser and ozonated water in the treatment of complicated pulp gangrene. Appl. Sci. 2020, 10, 4203. [Google Scholar] [CrossRef]
- Aminov, L.; Moscalu, M.; Melian, A.; Salceanu, M.; Hamburda, T.; Vataman, M. Clinical-radiological study on the role of biostimulating materials in iatrogenic furcation lesions. Rev. Med. Chir. Soc. Med. Nat. Iasi 2012, 116, 907–913. [Google Scholar]
- Corbella, S.; Walter, C.; Tsesis, I. Effectiveness of root resection techniques compared with root canal retreatment or apical surgery for the treatment of apical periodontitis and tooth survival: A systematic review. Int. Endod. J. 2023, 56 (Suppl. S3), 487–498. [Google Scholar] [CrossRef] [PubMed]
- Budacu, C.; Cioranu, S.V.I.; Chiscop, I.; Salceanu, M.; Melian, A. Apicoectomy—Endodontical surgical procedure. Rev. Chim. 2017, 68, 2654–2657. [Google Scholar] [CrossRef]
- Uraba, S.; Ebihara, A.; Komatsu, K.; Ohbayashi, N.; Okiji, T. Ability of cone-beam computed tomography to detect periapical lesions that were not detected by periapical radiography: A retrospective assessment according to tooth group. J. Endod. 2016, 42, 1186–1190. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Kim, H.C.; Lee, W.; Kim, E. Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J. Endod. 2011, 37, 1516–1519. [Google Scholar] [CrossRef] [PubMed]
- Holland, R.; Gomes Filho, J.E.; Cintra, L.T.A.; Queiroz, Í.O.D.A.; Estrela, C. Factors affecting the periapical healing process of endodontically treated teeth. J. Appl. Oral Sci. 2017, 25, 465–476. [Google Scholar] [CrossRef]
- Fransson, H.; Dawson, V. Tooth survival after endodontic treatment. Int. Endod. J. 2023, 56 (Suppl. S2), 140–153. [Google Scholar] [CrossRef]
- Rawski, A.A.; Brehmer, B.; Knutsson, K.; Petersson, K.; Reit, C.; Rohlin, M. The major factors that influence endodontic retreatment decisions. Swed. Dent. J. 2003, 27, 23–29. [Google Scholar]
- Gulabivala, K.; Ng, Y.L. Factors that affect the outcomes of root canal treatment and retreatment-A reframing of the principles. Int. Endod. J. 2023, 56 (Suppl. S2), 82–115. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F., Jr. Biofilms and apical periodontitis: Study of prevalence and association with clinical and histopathologic findings. J. Endod. 2010, 36, 1277–1288. [Google Scholar] [CrossRef]
- Bürklein, S.; Schäfer, E.; Jöhren, H.P.; Donnermeyer, D. Quality of root canal fillings and prevalence of apical radiolucencies in a German population: A CBCT analysis. Clin. Oral Investig. 2020, 24, 1217–1227. [Google Scholar] [CrossRef]
- Tibúrcio-Machado, C.S.; Michelon, C.; Zanatta, F.B.; Gomes, M.S.; Marin, J.A.; Bier, C.A. The global prevalence of apical periodontitis: A systematic review and meta-analysis. Int. Endod. J. 2021, 54, 712–735. [Google Scholar] [CrossRef] [PubMed]
- Chala, S.; Abouqal, R.; Abdallaoui, F. Prevalence of apical periodontitis and factors associated with the periradicular status. Acta Odontol. Scand. 2011, 69, 355–359. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Nikolic, N.; Jacimovic, J.; Pavlovic, O.; Milicic, B.; Beljic-Ivanovic, K.; Miletic, M.; Andric, M.; Milasin, J. Prevalence of Apical Periodontitis and Conventional Nonsurgical Root Canal Treatment in General Adult Population: An Updated Systematic Review and Meta-Analysis of Cross-Sectional Studies Published between 2012 and 2020. J Endod. 2020, 46, 1371–1386.e8. [Google Scholar] [CrossRef]
- El Ouarti, I.; Chala, S.; Sakout, M.; Abdallaoui, F. Prevalence and risk factors of Apical periodontitis in endodontically treated teeth: Cross-sectional study in an Adult Moroccan subpopulation. BMC Oral Health 2021, 21, 124. [Google Scholar] [CrossRef] [PubMed]
- Prada, I.; Micó-Muñoz, P.; Giner-Lluesma, T.; Micó-Martínez, P.; Collado-Castellano, N.; Manzano-Saiz, A. Influence of microbiology on endodontic failure. Literature review. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e364–e372. [Google Scholar] [CrossRef]
- Burt, B.A. Definitions of risk. J. Dent. Educ. 2001, 65, 1007–1008. [Google Scholar] [CrossRef] [PubMed]
- Baseri, M.; Radmand, F.; Milani, A.S.; Gavgani, L.F.; Salehnia, F.; Dianat, O. The effect of periapical lesion size on the success rate of different endodontic treatments: A systematic review and meta-analysis. Evid. Based Dent. 2023, 24, 43. [Google Scholar] [CrossRef]
- Iqbal, M.K.; Kim, S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J. Endod. 2008, 34, 519–529. [Google Scholar] [CrossRef]
- Chugal, N.M.; Clive, J.M.; Spångberg, L.S. Endodontic treatment outcome: Effect of the permanent restoration. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 576–582. [Google Scholar] [CrossRef]
- Orstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Nur, B.G.; Ok, E.; Altunsoy, M.; Ağlarci, O.S.; Çolak, M.; Güngör, E. Evaluation of technical quality and periapical health of root-filled teeth by using cone-beam CT. J. Appl. Oral Sci. 2014, 22, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Bergenholtz, G. Assessment of treatment failure in endodontic therapy. J. Oral Rehabil. 2016, 43, 753–758. [Google Scholar] [CrossRef]
- Frisk, F.; Hugosson, A.; Kvist, T. Is apical periodontitis in root filled teeth associated with the type of restoration? Acta Odontol. Scand. 2015, 73, 169–175. [Google Scholar] [CrossRef]
- Hussain, M.A.; Singh, S.K.; Naz, S.; Haque, M.; Shah, H.K.; Singh, A. Predictors of apical periodontitis in root canal treated teeth from an adult Nepalese subpopulation: A cross-sectional study. BMC Oral Health 2024, 24, 400. [Google Scholar] [CrossRef] [PubMed]
- Estrela, C.; Holland, R.; Estrela, C.R.; Alencar, A.H.; Sousa-Neto, M.D.; Pécora, J.D. Characterization of successful root canal treatment. Braz. Dent. J. 2014, 25, 3–11. [Google Scholar] [CrossRef]
- Godiny, M.; Jalali, S.K.; Khavid, A.; Fatahy, A. Simulated Evaluation of Tooth Fracture Resistance during Instrumentation with Single-and Multi-file Rotary Systems. Iran. Endod. J. 2021, 16, 232–237. [Google Scholar]
- Sequeira-Byron, P.; Fedorowicz, Z.; Carter, B.; Nasser, M.; Alrowaili, E.F. Single crowns versus conventional fillings for the restoration of root-filled teeth. Cochrane Database Syst. Rev. 2015, 2015, CD009109. [Google Scholar] [CrossRef]
- Tiron, B.; Forna, N.; Topoliceanu, C.; Ghiorghe, A.; Stoleriu, S.; Pancu, G.; Nica, I.; Georgescu, A.; Brânzan, R.; Iovan, G. Assessment of factors influencing the esthetic, functional and biological status of posterior composite resins restorations. Rom. J. Oral Rehabil. 2023, 15, 29–41. [Google Scholar]
- Pancu, G.; Georgescu, A.; Moldovanu, A.; Ghiorghe, A.; Stoleriu, S.; Nica, I.; Tărăboanţă, I.; Iovan, A.; Andrian, S.; Topoliceanu, C. Non-intervention versus repair/replacement decisions in posterior composite restorations aged 3–5 years: A retrospective study. Rom. J. Oral Rehabil. 2024, 16, 186–195. [Google Scholar]
- Dawson, V.S.; Petersson, K.; Wolf, E.; Åkerman, S. Periapical Status of Root-filled Teeth Restored with Composite, Amalgam, or Full Crown Restorations: A Cross-sectional Study of a Swedish Adult Population. J. Endod. 2016, 42, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Boucher, Y.; Matossian, L.; Rilliard, F.; Machtou, P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int. Endod. J. 2002, 35, 229–238. [Google Scholar] [CrossRef]
- Ferreira, M.L.; Buligon, M.P.; Sfreddo, C.S.; Liedke, G.S.; Morgental, R.D. Factors related to apical periodontitis in a southern Brazilian population: A multilevel analysis. Braz. Oral Res. 2022, 36, e112. [Google Scholar] [CrossRef]
- Suzuki, P.; de Souza, V.; Holland, R.; Gomes-Filho, J.E.; Murata, S.S.; Dezan Junior, E.; Passos, T.R. Tissue reaction to Endométhasone sealer in root canal fillings short of or beyond the apical foramen. J. Appl. Oral Sci. 2011, 19, 511–516. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suzuki, P.; de Souza, V.; Holland, R.; Murata, S.S.; Gomes-Filho, J.E.; Dezan Junior, E.; Rodrigues Dos Passos, T. Tissue reaction of the EndoREZ in root canal fillings short of or beyond an apical foramen-like communication. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e94–e99. [Google Scholar] [CrossRef] [PubMed]
- Alves Dos Santos, G.N.; Faria-E-Silva, A.L.; Ribeiro, V.L.; Pelozo, L.L.; Candemil, A.P.; Oliveira, M.L.; Lopes-Olhê, F.C.; Mazzi-Chaves, J.F.; Sousa-Neto, M.D. Is the quality of root canal filling obtained by cone-beam computed tomography associated with periapical lesions? A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 5105–5116. [Google Scholar] [CrossRef]
- Ali, A.H.; Mahdee, A.F.; Fadhil, N.H.; Shihab, D.M. Prevalence of periapical lesions in non-endodontically and endodontically treated teeth in an urban Iraqi adult subpopulation: A retrospective CBCT analysis. J. Clin. Exp. Dent. 2022, 14, e953–e958. [Google Scholar] [CrossRef] [PubMed]
- Meirinhos, J.; Martins, J.; Pereira, B.; Baruwa, A.; Gouveia, J.; Quaresma, S.; Monroe, A.; Ginjeira, A. Prevalence of apical periodontitis and its association with previous root canal treatment, root canal filling length and type of coronal restoration—A cross-sectional study. Int. Endod. J. 2020, 53, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Keratiotis, G.; Spineli, L.; De Bruyne, M.A.A.; De Moor, R.J.G.; Meire, M.A. A 22-year follow-up cross-sectional study on periapical health in relation to the quality of root canal treatment in a Belgian population. Int. Endod. J. 2024, 57, 533–548. [Google Scholar] [CrossRef]
- Song, M.; Park, M.; Lee, C.Y.; Kim, E. Periapical status related to the quality of coronal restorations and root fillings in a Korean population. J. Endod. 2014, 40, 182–186. [Google Scholar] [CrossRef]
- Nascimento, E.H.L.; Gaêta-Araujo, H.; Andrade, M.F.S.; Freitas, D.Q. Prevalence of technical errors and periapical lesions in a sample of endodontically treated teeth: A CBCT analysis. Clin. Oral Investig. 2018, 22, 2495–2503. [Google Scholar] [CrossRef] [PubMed]
- Di Filippo, G.; Sidhu, S.; Chong, B. Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London. Br. Dent. J. 2014, 216, E22. [Google Scholar] [CrossRef] [PubMed]
- Kalender, A.; Orhan, K.; Aksoy, U.; Basmaci, F.; Er, F.; Alankus, A. Influence of the quality of endodontic treatment and coronal restorations on the prevalence of apical periodontitis in a Turkish Cypriot population. Med. Princ. Pract. 2013, 22, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Jersa, I.; Kundzina, R. Periapical status and quality of root fillings in a selected adult Riga population. Stomatologija 2013, 15, 73–77. [Google Scholar]
- Gillen, B.M.; Looney, S.W.; Gu, L.S.; Loushine, B.A.; Weller, R.N.; Loushine, R.J.; Pashley, D.H.; Tay, F.R. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: A systematic review and meta-analysis. J. Endod. 2011, 37, 895–902. [Google Scholar] [CrossRef]
- Nicolae, V.; Neamtu, B.; Picu, O.; Stefanache, M.A.M.; Cioranu, V.S.I. The comparative evaluation of salivary biomarkers (Calcium, Phosphate, Salivary pH) in Cario-resistance versus Cario-activity. Rev. Chim. 2016, 67, 821–824. [Google Scholar]
- Popa, C.G.; Luchian, I.; Ioanid, N.; Goriuc, A.; Martu, I.; Bosinceanu, D.; Martu, M.A.; Tirca, T.; Martu, S. ELISA Evaluation of RANKL Levels in Gingival Fluid in Patients with Periodontitis and Occlusal Trauma. Rev. Chim. 2018, 69, 1578–1580. [Google Scholar] [CrossRef]
- Cristea, I.; Agop-Forna, D.; Martu, M.-A.; Dascălu, C.; Topoliceanu, C.; Török, R.; Török, B.; Bardis, D.; Bardi, P.M.; Forna, N. Oral and Periodontal Risk Factors of Prosthetic Success for 3-Unit Natural Tooth-Supported Bridges versus Implant-Supported Fixed Dental Prostheses. Diagnostics 2023, 13, 852. [Google Scholar] [CrossRef]
- Solomon, S.M.; Timpu, D.; Forna, D.A.; Stefanache, M.A.; Martu, S.; Stoleriu, S. AFM comparative study of root surface morphology after three methods of scaling. Mater. Plast. 2016, 53, 546–549. [Google Scholar]
- Solomon, S.M.; Stoleriu, S.; Agop Forna, D.; Timpu, D.; Martu Stefanache, M.A.; Ursarescu, I.G.; Martu, S. The quantitative and qualitative assessment of dental substance loss as consequence of root planing by three different techniques. Mater. Plast. 2016, 53, 305–307. [Google Scholar]
- Mârtu, S.; Amalinei, C.; Tatarciuc, M.; Rotaru, M.; Potârnichie, O.; Liliac, L.; Caruntu, I.D. Healing process and laser therapy in the superficial periodontium: A histological study. Rom. J. Morphol. Embryol. 2012, 53, 111–116. [Google Scholar] [PubMed]
- Martu, M.-A.; Luchian, I.; Mares, M.; Solomon, S.; Ciurcanu, O.; Danila, V.; Rezus, E.; Foia, L. The Effectiveness of Laser Applications and Photodynamic Therapy on Relevant Periodontal Pathogens (Aggregatibacter actinomycetemcomitans) Associated with Immunomodulating Anti-Rheumatic Drugs. Bioengineering 2023, 10, 61. [Google Scholar] [CrossRef]
- Nicolae, V.D.; Chiscop, I.; Cioranu, V.S.I.; Mârțu, M.-A.; Luchian, A.I.; Mârțu, S.; Solomon, S.M. The use of photoactivated blue-O toluidine for periimplantitis treatment in patients with periodontal disease. Rev. Chim. 2016, 66, 2121–2123. [Google Scholar]
- Martu, M.-A.; Maftei, G.-A.; Luchian, I.; Stefanescu, O.M.; Scutariu, M.M.; Solomon, S.M. The Effect of Acknowledged and Novel Anti-Rheumatic Therapies on Periodontal Tissues—A Narrative Review. Pharmaceuticals 2021, 14, 1209. [Google Scholar] [CrossRef]
- Budala, D.G.; Martu, M.-A.; Maftei, G.-A.; Diaconu-Popa, D.A.; Danila, V.; Luchian, I. The Role of Natural Compounds in Optimizing Contemporary Dental Treatment—Current Status and Future Trends. J. Funct. Biomater. 2023, 14, 273. [Google Scholar] [CrossRef]
- Sufaru, I.-G.; Martu, M.-A.; Luchian, I.; Stoleriu, S.; Diaconu-Popa, D.; Martu, C.; Teslaru, S.; Pasarin, L.; Solomon, S.M. The Effects of 810 nm Diode Laser and Indocyanine Green on Periodontal Parameters and HbA1c in Patients with Periodontitis and Type II Diabetes Mellitus: A Randomized Controlled Study. Diagnostics 2022, 12, 1614. [Google Scholar] [CrossRef] [PubMed]
- Martu, M.-A.; Surlin, P.; Lazar, L.; Maftei, G.A.; Luchian, I.; Gheorghe, D.-N.; Rezus, E.; Toma, V.; Foia, L.-G. Evaluation of Oxidative Stress before and after Using Laser and Photoactivation Therapy as Adjuvant of Non-Surgical Periodontal Treatment in Patients with Rheumatoid Arthritis. Antioxidants 2021, 10, 226. [Google Scholar] [CrossRef]
- Anton, D.-M.; Martu, M.-A.; Maris, M.; Maftei, G.-A.; Sufaru, I.-G.; Tatarciuc, D.; Luchian, I.; Ioanid, N.; Martu, S. Study on the Effects of Melatonin on Glycemic Control and Periodontal Parameters in Patients with Type II Diabetes Mellitus and Periodontal Disease. Medicina 2021, 57, 140. [Google Scholar] [CrossRef]
- Stassen, I.G.; Hommez, G.M.; De Bruyn, H.; De Moor, R.J. The relation between apical periodontitis and root-filled teeth in patients with periodontal treatment need. Int. Endod. J. 2006, 39, 299–308. [Google Scholar] [CrossRef]
- Ruiz, X.F.; Duran-Sindreu, F.; Shemesh, H.; García Font, M.; Vallés, M.; Roig Cayón, M.; Olivieri, J.G. Development of Periapical Lesions in Endodontically Treated Teeth with and without Periodontal Involvement: A Retrospective Cohort Study. J. Endod. 2017, 43, 1246–1249. [Google Scholar] [CrossRef]
- Buligon, M.P.; Marin, J.A.; Wolle, C.F.B.; Liedke, G.S.; Sfreddo, C.S.; Bier, C.A.S.; Moreira, C.H.C.; Morgental, R.D. Apical periodontitis and associated factors in a rural population of southern Brazil: A multilevel analysis. Clin. Oral Investig. 2023, 27, 2887–2897. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Fujiwara, N.; Kuraji, R.; Numabe, Y. Relationship between periodontal parameters and non-vital pulp in dental clinic patients: A cross-sectional study. BMC Oral Health 2020, 20, 109. [Google Scholar] [CrossRef]
- Zaharescu, A.; Solomon, S.M.; Luca, M.G.; Toma, V.; Luchian, I.; Sufaru, I.G.; Martu, S. Quantification of proinflammatory molecules (IL1-α, IL1-β, IL2, IL12, IFN-γ, TNF-α) in crevicular fluid and serum in patients with endo-periodontal lesions. Rev. Chim. 2019, 70, 2252–2255. [Google Scholar] [CrossRef]
- Martu, C.; Martu, M.-A.; Maftei, G.-A.; Diaconu-Popa, D.A.; Radulescu, L. Odontogenic Sinusitis: From Diagnosis to Treatment Possibilities—A Narrative Review of Recent Data. Diagnostics 2022, 12, 1600. [Google Scholar] [CrossRef] [PubMed]
- Nardi, C.; Calistri, L.; Grazzini, G.; Desideri, I.; Lorini, C.; Occhipinti, M.; Mungai, F.; Colagrande, S. Is Panoramic Radiography an Accurate Imaging Technique for the Detection of Endodontically Treated Asymptomatic Apical Periodontitis? J. Endod. 2018, 44, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Antohi, C.; Salceanu, M.; Aminov, L.; Martu, M.-A.; Dascalu, C.G.; Dodi, G.; Stoica, G.; Bandol, G.; Iancu, D.; Dobrovat, B.; et al. Assessment of Systemic and Maxillary Bone Loss in Cancer Patients with Endo-Periodontal Lesions Using Dkk-1 Biomarker and Dental Radiological Examinations. Appl. Sci. 2022, 12, 5235. [Google Scholar] [CrossRef]
- Sălceanu, M.; Vataman, M.; Aminov, L.; Giuroiu, C.; Topoliceanu, C.; Decolli, Y.; Ghiorghe, C.-A.; Melian, A. Diagnosis and follow-up of the periapical lesions in the non-surgical endodontic treatment: A CBCT study. Rom. J. Oral Rehabil. 2017, 9, 32–36. [Google Scholar]
- Leonardi Dutra, K.; Haas, L.; Porporatti, A.L.; Flores-Mir, C.; Nascimento Santos, J.; Mezzomo, L.A.; Corrêa, M.; De Luca Canto, G. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J. Endod. 2016, 42, 356–364. [Google Scholar] [CrossRef]
- Siqueira Junior, J.F.; Rôças, I.D.N.; Marceliano-Alves, M.F.; Pérez, A.R.; Ricucci, D. Unprepared root canal surface areas: Causes, clinical implications, and therapeutic strategies. Braz. Oral Res. 2018, 32 (Suppl. S1), e65. [Google Scholar] [CrossRef]
- Kazimierczak, W.; Wajer, R.; Wajer, A.; Kiian, V.; Kloska, A.; Kazimierczak, N.; Janiszewska-Olszowska, J.; Serafin, Z. Periapical Lesions in Panoramic Radiography and CBCT Imaging-Assessment of AI’s Diagnostic Accuracy. J. Clin. Med. 2024, 13, 2709. [Google Scholar] [CrossRef]
- Ahmed, H.M.; Cohen, S.; Lévy, G.; Steier, L.; Bukiet, F. Rubber dam application in endodontic practice: An update on critical educational and ethical dilemmas. Aust. Dent. J. 2014, 59, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Zaharescu, A.; Mârțu, I.; Luchian, A.I.; Mârțu, M.A.; Șufaru, I.G.; Mârțu, C.; Solomon, S.M. Role of adjunctive therapy with subantimicrobial doses of doxycycline in glycemic control (HbA1c) in patients with diabetes and endo-periodontal lesions to prevent sinus complications. Exp. Ther. Med. 2021, 21, 277. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).

