The Efficacy of Diagnostic Plaster Models in Orthodontic Diagnosis and Treatment Planning
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patient Record Selection
2.3. Expert Panel
2.4. Data Collection
- Scenario 1: The patient records used were digital treatment records per se (panoramic radiographs, cephalograms, and intra- and extraoral photographs).
- Scenario 2: The patient records used were digital records plus diagnostic physical orthodontic plaster models. This design was used to determine whether the plaster model affected the orthodontist’s treatment plan for any of the evaluated malocclusion cases.
- Orthodontist Demographics: Basic information about the orthodontist (e.g., gender and years of experience).
- Diagnostic Assessment: Orthodontists were asked to provide a comprehensive diagnosis based on the presented records.
- Treatment Planning: Orthodontists were required to outline a proposed treatment plan, specifying treatment modalities, timing, and whether diagnostic materials presented for each case in the two tested scenarios were sufficient to establish a valid treatment plan or if additional diagnostic information was required. This enabled the participating orthodontists to assess plaster models’ perceived benefits or limitations.
2.5. Data Analysis
2.6. Expected Outcome
3. Results
3.1. Impact of Digital Records vs. Physical Diagnostic Plaster Models for Diagnosis of Orthodontic Malocclusion Classes
3.2. Impact of Digital Records vs. Physical Diagnostic Plaster Models on Treatment Planning for Orthodontic Malocclusion Classes
3.2.1. Treatment Plan One (Comprehensive Treatment Plan vs. Limited Treatment Plan)
3.2.2. Treatment Plan Two (Surgical Intervention Treatment Plan vs. Non-Surgical Intervention Treatment Plan)
3.2.3. Treatment Plan Three (Extraction vs. Non-Extraction)
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Németh, O.; Uhrin, E.; Girasek, E.; Boros, J.; Győrffy, Z. The impact of digital healthcare and teledentistry on dentistry in the 21st Century: A survey of Hungarian dentists. BMC Oral. Health 2023, 23, 1025. [Google Scholar] [CrossRef] [PubMed]
- Helal, N.M.; Basri, O.A.; Baeshen, H.A. Significance of Cephalometric Radiograph in Orthodontic Treatment Plan Decision. J. Contemp. Dent. Pract. 2019, 20, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Bootvong, K.; Liu, Z.; McGrath, C.; Hagg, U.; Wong, R.W.; Bendeus, M.; Yeung, S. Virtual model analysis as an alternative approach to plaster model analysis: Reliability and validity. Eur. J. Orthod. 2010, 32, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Pachêco-Pereira, C.; De Luca, C.G.; Major, P.W.; Flores-Mir, C. Variation of orthodontic treatment decision-making based on dental model type: A systematic review. Angle Orthod. 2015, 85, 501–509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baciu, E.R.; Budală, D.G.; Vasluianu, R.-I.; Lupu, C.I.; Murariu, A.; Gelețu, G.L.; Zetu, I.N.; Diaconu-Popa, D.; Tatarciuc, M.; Nichitean, G.; et al. A Comparative Analysis of Dental Measurements in Physical and Digital Orthodontic Case Study Models. Medicina 2022, 58, 1230. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marya, A. Are orthodontic decisions consistent? Evid. Based Dent. 2022, 23, 120–121. [Google Scholar] [CrossRef]
- Alqerban, A.; Willems, G.; Bernaerts, C.; Vangastel, J.; Politis, C.; Jacobs, R. Orthodontic treatment planning for impacted maxillary canines using conventional records versus 3D CBCT. Eur. J. Orthod. 2014, 36, 698–707. [Google Scholar] [CrossRef]
- Ko, H.C.; Liu, W.; Hou, D.; Torkan, S.; Spiekerman, C.; Huang, G.J. Agreement of treatment recommendations based on digital vs plaster dental models. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 135–142. [Google Scholar] [CrossRef]
- Hou, D.; Capote, R.; Bayirli, B.; Chan, D.C.; Huang, G. The effect of digital diagnostic setups on orthodontic treatment planning. Am. J. Orthod. Dentofacial Orthop. 2020, 157, 542–549. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Mortadi, N.; Al-Khatib, A.; Alzoubi, K.H.; Khabour, O.F. Disinfection of dental impressions: Knowledge and practice among dental technicians. Clin. Cosmet. Investig. Dent. 2019, 11, 103–108. [Google Scholar] [CrossRef]
- DaSilva, A.F.; Robinson, M.A.; Shi, W.; McCauley, L.K. The Forefront of Dentistry—Promising Tech-Innovations and New Treatments. JDR Clin. Transl. Res. 2022, 7 (Suppl. 1), 16S–24S. [Google Scholar] [CrossRef] [PubMed]
- Stevens, D.R.; Flores-Mir, C.; Nebbe, B.; Raboud, D.W.; Heo, G.; Major, P.W. Validity, reliability, and reproducibility of plaster vs digital study models: Comparison of peer assessment rating and Bolton analysis and their constituent measurements. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 794–803. [Google Scholar] [CrossRef] [PubMed]
- Rischen, R.J.; Breuning, K.H.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M. Records Needed for Orthodontic Diagnosis and Treatment Planning: A Systematic Review. PLoS ONE 2013, 8, e74186. [Google Scholar] [CrossRef] [PubMed]
- Dinesh, A.; Mutalik, S.; Feldman, J.; Tadinada, A. Value-addition of lateral cephalometric radiographs in orthodontic diagnosis and treatment planning. Angle Orthod. 2020, 90, 665–671. [Google Scholar] [CrossRef]
- Salari, B.; Tofangchiha, M.; Padisar, P.; Reda, R.; Zanza, A.; Testarelli, L. Diagnostic accuracy of conventional orthodontic radiographic modalities and cone-beam computed tomography for localization of impacted maxillary canine teeth. Sci. Prog. 2024, 107, 368504241228077. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaasalainen, T.; Ekholm, M.; Siiskonen, T.; Kortesniemi, M. Dental cone beam CT: An updated review. Phys. Medica 2021, 88, 193–217. [Google Scholar] [CrossRef]
- Schierz, O.; Hirsch, C.; Krey, K.F.; Ganss, C.; Kämmerer, P.W.; Schlenz, M.A. DIGITAL DENTISTRY AND ITS IMPACT ON ORAL HEALTH-RELATED QUALITY OF LIFE. J. Evid. Based Dent. Pract. 2024, 24, 101946. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Hao, J.; Lin, H.; Pan, W.; Yang, J.; Feng, Y.; Wang, G.; Li, J.; Jin, Z.; Zhao, Z.; et al. Deep learning-enabled 3D multimodal fusion of cone-beam CT and intraoral mesh scans for clinically applicable tooth-bone reconstruction. Patterns 2023, 4, 100825. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fleming, P.S.; Marinho, V.; Johal, A. Orthodontic measurements on digital study models compared with plaster models: A systematic review. Orthod. Craniofac. Res. 2011, 14, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Grewal, B.; Lee, R.T.; Zou, L.; Johal, A. Royal London space analysis: Plaster versus digital model assessment. Eur. J. Orthod. 2017, 39, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Whetten, J.L.; Williamson, P.C.; Heo, G.; Varnhagen, C.; Major, P.W. Variations in orthodontic treatment planning decisions of Class II patients between virtual 3-dimensional models and traditional plaster study models. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Durão, A.R.; Alqerban, A.; Ferreira, A.P.; Jacobs, R. Influence of lateral cephalometric radiography in orthodontic diagnosis and treatment planning. Angle Orthod. 2015, 85, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Mok, C.W.; Zhou, L.; Mcgrath, C.; Hägg, U.; Bendeus, M. Digital images as an alternative to orthodontic casts in assessing malocclusion and orthodontic treatment need. Acta Odontol. Scand. 2007, 65, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.A.; Phillip, A.; Kumar, S.; Rawat, A.; Priya, S.; Kumaran, V. Digital model as an alternative to plaster model in assessment of space analysis. J. Pharm. Bioallied Sci. 2015, 7 (Suppl. 2), S465–S469. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yilmaz, H.; Ozlu, F.C.; Karadeniz, C.; Karadeniz, E.I. Efficiency and Accuracy of Three-Dimensional Models Versus Dental Casts: A Clinical Study. Turk. J. Orthod. 2019, 32, 214–218. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Rheude, B.; Sadowsky, P.L.; Ferriera, A.; Jacobson, A. An evaluation of the use of digital study models in orthodontic diagnosis and treatment planning. Angle Orthod. 2005, 75, 300–304. [Google Scholar] [CrossRef]
- Nijkamp, P.G.; Habets, L.L.; Aartman, I.H.; Zentner, A. The influence of cephalometrics on orthodontic treatment planning. Eur. J. Orthod. 2008, 30, 630–635. [Google Scholar] [CrossRef]
- Mavreas, D.; Kuppens, E.; Buyl, R.; Vannet, B.V. How orthodontic records can influence torque choice decisions? Eur. J. Orthod. 2016, 38, 212–216. [Google Scholar] [CrossRef][Green Version]
- Leung, C.Y.V.; Yang, Y.; Liao, C.; Hägg, U.; Wong, R.W.; McGrath, C.; Gu, M. Digital Models as an Alternative to Plaster Casts in Assessment of Orthodontic Treatment Outcomes. Sci. World J. 2018, 2018, 9819384. [Google Scholar] [CrossRef]
- Kardach, H.; Szponar-Żurowska, A.; Biedziak, B. A Comparison of Teeth Measurements on Plaster and Digital Models. J. Clin. Med. 2023, 12, 943. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
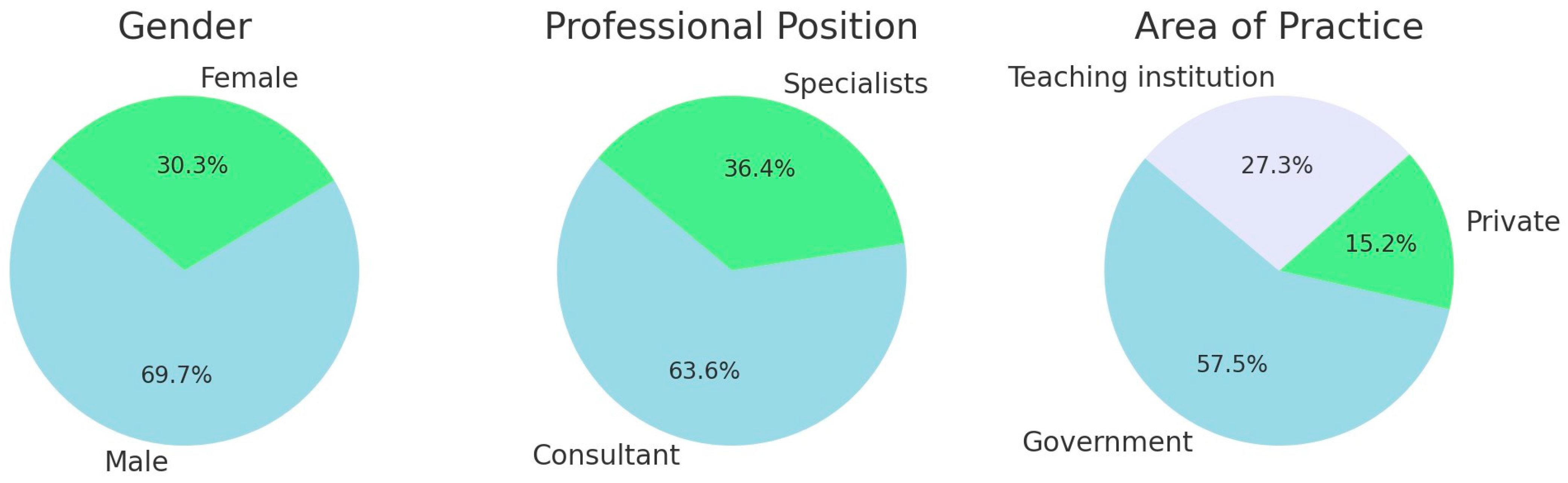


| Characteristics | No.(%) |
|---|---|
| Gender | |
| Male | 23(69.7) |
| Female | 10(30.3) |
| Professional position | |
| Consultant | 21(63.6) |
| Specialists | 12(36.4) |
| Area of practice | |
| Government | 19(57.6) |
| Private | 5(15.2) |
| Teaching institution | 9(27.3) |
| With Plaster Models | Total No. (%) | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Diagnosis | ||||||||
| Class I | Class II | Class III | |||||||
| Without Plaster Models | Diagnosis Class I | 53 | 72.6% | 16 | 24.2% | 10 | 16.9% | 79 (39.3) | <0.0001 |
| 67.1% | 20.3% | 12.7% | 100% | ||||||
| Class II | 3 | 4.1% | 49 | 74.2% | 3 | 5.1% | 55 (27.8) | ||
| 5.5% | 89.1% | 5.5% | 100% | ||||||
| Class III | 17 | 23.3% | 1 | 1.5% | 46 | 78% | 64 (32.3) | ||
| 26.6% | 1.6% | 71.9% | 100% | ||||||
| Total No. (%) | 73 (36.9) | 100% | 66 (33.3) | 100% | 59 (29.8) | 100% | 198 (100) | ||
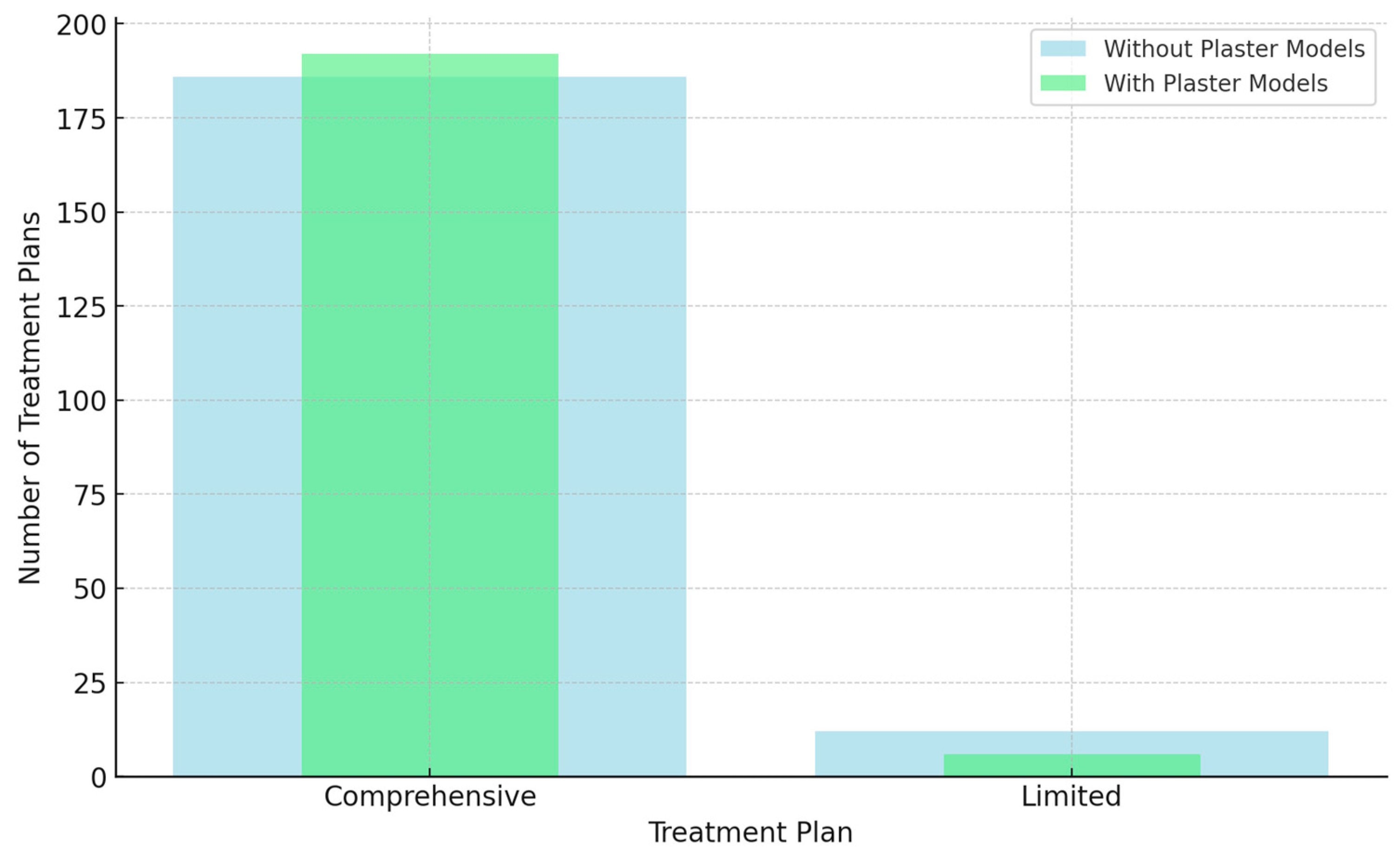
| Treatment 1 Comprehensive | Treatment 1 | Total No. (%) | 0.146 | ||||||
| Comprehensive | Limited | ||||||||
| 183 | 95.3% | 3 | 50% | 186 (93.9) | |||||
| 98.4% | 1.6% | 100% | |||||||
| Limited | 9 | 4.7% | 3 | 50% | 12 (6.1) | ||||
| 75% | 25% | 100% | |||||||
| Total No. (%) | 192 (97) | 100% | 6 (3) | 100% | 198 (100) | ||||
| Treatment 2 Surgical | Treatment 2 | Total No. (%) | 0.026 | ||||||
| Surgical | Non-Surgical | ||||||||
| 27 | 41.5% | 20 | 15% | 47(23.7) | |||||
| 57.4% | 42.6% | 100% | |||||||
| Non-Surgical | 38 | 58.5% | 113 | 85% | 151 (76.3) | ||||
| 25.2% | 74.8% | 100% | |||||||
| Total No. (%) | 65 (32.8) | 100% | 133 (67.2) | 100% | 198 (100) | ||||
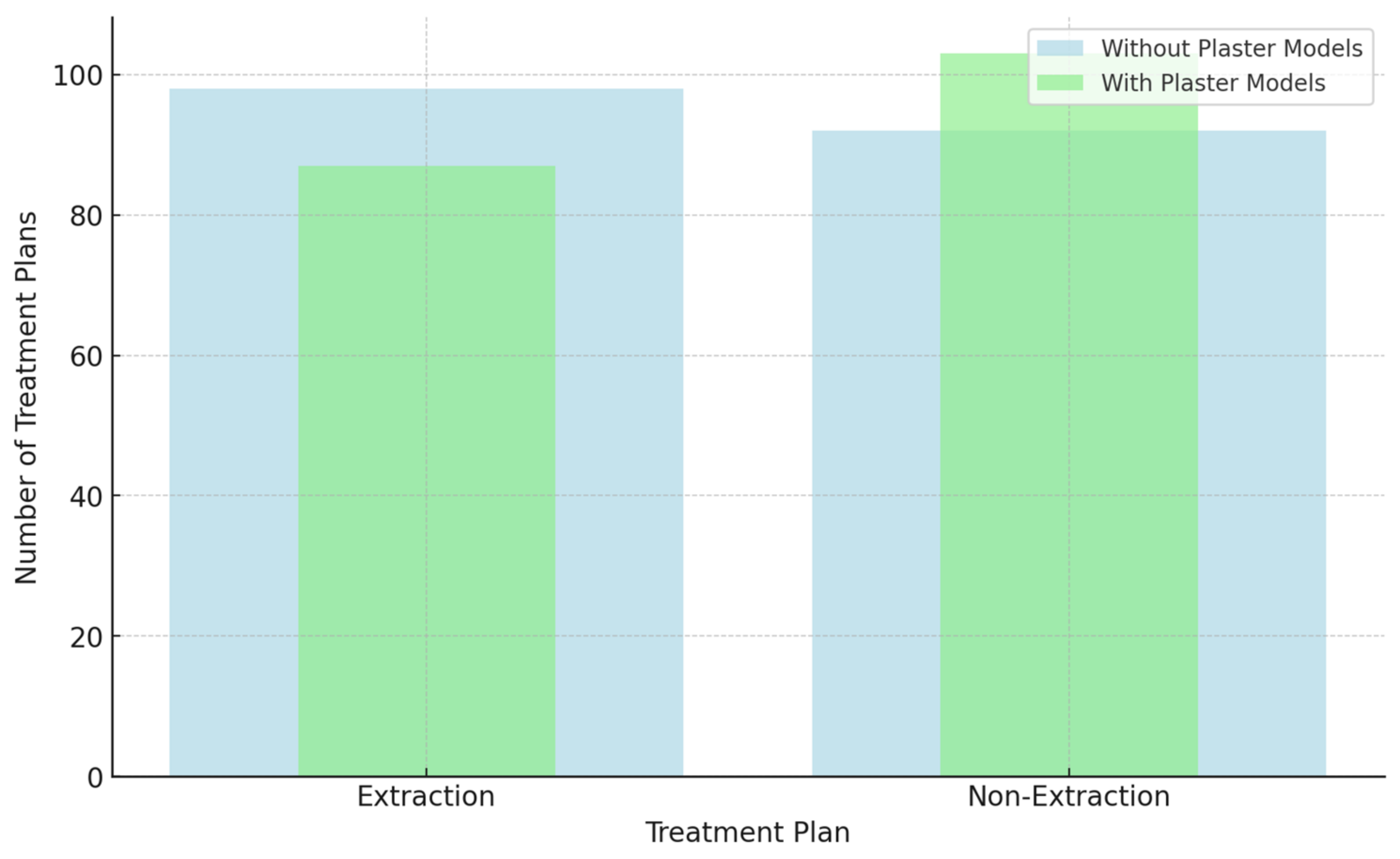
| Treatment 3 Extraction | Treatment 3 | Total | 0.266 | ||||||
| Extraction | Non-Extraction | ||||||||
| 52 | 59.8% | 46 | 44.7% | 98 (51.6) | |||||
| 53.1% | 46.9% | 100% | |||||||
| Non-Extraction | 35 | 40.2% | 57 | 55.3% | 92 (48.4) | ||||
| 38% | 62% | 100% | |||||||
| Total No. (%) | 87 (45.8) | 100% | 103 (54.2) | 100% | 190 (100) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almudhi, A.; Almohammad, I.; Alswayyed, S.; Eldwakhly, E.; Almugairin, S. The Efficacy of Diagnostic Plaster Models in Orthodontic Diagnosis and Treatment Planning. Diagnostics 2024, 14, 2124. https://doi.org/10.3390/diagnostics14192124
Almudhi A, Almohammad I, Alswayyed S, Eldwakhly E, Almugairin S. The Efficacy of Diagnostic Plaster Models in Orthodontic Diagnosis and Treatment Planning. Diagnostics. 2024; 14(19):2124. https://doi.org/10.3390/diagnostics14192124
Chicago/Turabian StyleAlmudhi, Abdullazez, Iman Almohammad, Sara Alswayyed, Elzahraa Eldwakhly, and Sarah Almugairin. 2024. "The Efficacy of Diagnostic Plaster Models in Orthodontic Diagnosis and Treatment Planning" Diagnostics 14, no. 19: 2124. https://doi.org/10.3390/diagnostics14192124
APA StyleAlmudhi, A., Almohammad, I., Alswayyed, S., Eldwakhly, E., & Almugairin, S. (2024). The Efficacy of Diagnostic Plaster Models in Orthodontic Diagnosis and Treatment Planning. Diagnostics, 14(19), 2124. https://doi.org/10.3390/diagnostics14192124






