A Comparative Analysis of International Classification Systems to Predict the Risk of Collapse in Single-Level Osteoporotic Vertebral Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Inclusion and Exclusion Criteria
- Patients diagnosed with acute OVF, identified on X-rays and CT.
- Patients with imaging follow-up of their fracture at least 6 months after diagnosis.
- Management with conservative medical treatment.
- Genant et al.’s grade 3 (loss of height/area > 40%) OVFs at initial diagnosis.
- More than 1 acute OVF.
- Patients treated by surgery or vertebral augmentation.
- Patients with poor-quality images, such as rotated, non-parallel radiographs.
2.3. Variables of the Study
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Classification of Osteoporotic Vertebral Fractures and Association with Collapse
3.3. Prediction of Vertebral Collapse: Regression and ROC Curve Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Willers, C.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; McCloskey, E.V.; Borgström, F.; Kanis, J.A.; SCOPE Review Panel of the IOF. Osteoporosis in Europe: A compendium of country-specific reports. Arch. Osteoporos. 2022, 17, 23. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.J.; Moraleda-Cabrera, B. Factors influencing vertebral collapse in osteoporotic vertebral fractures: A case-control study of symptomatic patients attended in the emergency department. Arch. Osteoporos. 2023, 19, 6. [Google Scholar] [CrossRef]
- Hsu, W.E.; Su, K.C.; Chen, K.H.; Pan, C.C.; Lu, W.H.; Lee, C.H. The Evaluation of Different Radiological Measurement Parameters of the Degree of Collapse of the Vertebral Body in Vertebral Compression Fractures. Appl. Bionics Biomech. 2019, 2019, 4021640. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.Y.; Kim, Y.H. Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos. Int. 2013, 24, 1207–1213. [Google Scholar] [CrossRef]
- Hoshino, M.; Tsujio, T.; Terai, H.; Namikawa, T.; Kato, M.; Matsumura, A.; Suzuki, A.; Takayama, K.; Takaoka, K.; Nakamura, H. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine 2013, 38, E641–E648. [Google Scholar] [CrossRef]
- López Zúñiga, D.; Láinez-Ramos-Bossini, A.J.; Ruiz Santiago, F. Radiographic diagnosis of osteoporotic vertebral fractures. An updated review. Med. Clin. 2022, 158, 125–132. [Google Scholar] [CrossRef]
- Genant, H.K.; Wu, C.Y.; van Kuijk, C.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef]
- Sugita, M.; Watanabe, N.; Mikami, Y.; Hase, H.; Kubo, T. Classification of vertebral compression fractures in the osteoporotic spine. Clin. Spine Surg. 2005, 18, 376–381. [Google Scholar] [CrossRef]
- Schnake, K.J.; Blattert, T.R.; Hahn, P.; Franck, A.; Hartmann, F.; Ullrich, B.; Verheyden, A.; Mörk, S.; Zimmermann, V.; Gonschorek, O.; et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018, 8, 46S–49S. [Google Scholar] [CrossRef]
- Mitani, K.; Takahashi, T.; Tokunaga, S.; Inoue, T.; Kanematsu, R.; Minami, M.; Hanakita, J. Therapeutic Prediction of Osteoporotic Vertebral Compression Fracture Using the AO Spine-DGOU Osteoporotic Fracture Classification and Classification-Based Score: A Single-Center Retrospective Observational Study. Neurospine 2023, 20, 1166–1176. [Google Scholar] [CrossRef] [PubMed]
- Lainez Ramos-Bossini, A.J.; Lopez Zuniga, D.; Ruiz Santiago, F. Percutaneous vertebroplasty versus conservative treatment and placebo in osteoporotic vertebral fractures: Meta-analysis and critical review of the literature. Eur. Radiol. 2021, 31, 8542–8553. [Google Scholar] [CrossRef] [PubMed]
- Blattert, T.R.; Schnake, K.J.; Gonschorek, O.; Gercek, E.; Hartmann, F.; Katscher, S.; Mörk, S.; Morrison, R.; Müller, M.; Partenheimer, A.; et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 50S–55S. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Oner, C.; Kepler, C.K.; Dvorak, M.; Schnake, K.; Bellabarba, C.; Reinhold, M.; Aarabi, B.; Kandziora, F.; Chapman, J.; et al. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine 2013, 38, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.r-project.org/ (accessed on 30 July 2024).
- Franco, C.B.; da Cruz, P.H.S.C.; Moreno, C.C.L.; Meneses, I.O.; Dos Santos, L.G.; Fontoura, A.C.; Brandão, T.K.; Rodríguez, L.M.R.; Yonezaki, A.M. Epidemiology of traumatic fractures of the spine in Mario Covas hospital between 2015 and 2020. Acta Ortop. Bras. 2023, 31, e267571. [Google Scholar] [CrossRef]
- Bigdon, S.F.; Saldarriaga, Y.; Oswald, K.A.C.; Müller, M.; Deml, M.C.; Benneker, L.M.; Ecker, T.M.; Albers, C.E. Epidemiologic analysis of 8000 acute vertebral fractures: Evolution of treatment and complications at 10-year follow-up. J. Orthop. Surg. Res. 2022, 17, 270. [Google Scholar] [CrossRef] [PubMed]
- Alseddeeqi, E.; Bashir, N.; AlAli, K.F.; Ahmed, L.A. Characteristics of patients with low-trauma vertebral fractures in the United Arab Emirates: A descriptive multi-center analysis. Endocr. J. 2020, 67, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Petitt, J.C.; Desai, A.; Kashkoush, A.; Ahorukomeye, P.; Potter, T.O.; Stout, A.; Kelly, M.L. Failure of Conservatively Managed Traumatic Vertebral Compression Fractures: A Systematic Review. World Neurosurg. 2022, 165, 81–88. [Google Scholar] [CrossRef]
- Funayama, T.; Tatsumura, M.; Fujii, K.; Ikumi, A.; Okuwaki, S.; Shibao, Y.; Koda, M.; Yamazaki, M. Therapeutic Effects of Conservative Treatment with 2-Week Bed Rest for Osteoporotic Vertebral Fractures: A Prospective Cohort Study. J. Bone Jt. Surg. Am. 2022, 104, 1785–1795. [Google Scholar] [CrossRef]
- Kanchiku, T.; Taguchi, T.; Toyoda, K.; Fujii, K.; Kawai, S. Dynamic contrast-enhanced magnetic resonance imaging of osteoporotic vertebral fracture. Spine (Phila Pa 1976) 2003, 28, 2522–2526. [Google Scholar] [CrossRef]
- Láinez Ramos-Bossini, A.J.; Láinez Millán, B.; Ruiz Santiago, F.; Rivera Izquierdo, M. Impact of the COVID-19 pandemic on osteoporotic vertebral fracture incidence and follow-up at the emergency department. A retrospective study of a tertiary hospital in southern Spain. Signa Vitae 2022, 18, 15. [Google Scholar] [CrossRef]
- Kweh, B.T.S.; Tee, J.W.; Dandurand, C.; Vaccaro, A.R.; Lorin, B.M.; Schnake, K.; Vialle, E.; Rajasekaran, S.; El-Skarkawi, M.; Bransford, R.J.; et al. The AO Spine Thoracolumbar Injury Classification System and Treatment Algorithm in Decision Making for Thoracolumbar Burst Fractures Without Neurologic Deficit. Glob. Spine J. 2024, 14 (Suppl. S1), 32S–40S. [Google Scholar] [CrossRef]
- Pishnamaz, M.; Curfs, I.; Balosu, S.; Willems, P.; Van Hemert, W.; Pape, H.C.; Kobbe, P. Two-Nation Comparison of Classification and Treatment of Thoracolumbar Fractures: An Internet-Based Multicenter Study Among Spine Surgeons. Spine 2015, 40, 1749–1756. [Google Scholar] [CrossRef]
- Ito, M.; Harada, A.; Nakano, T.; Kuratsu, S.; Deguchi, M.; Sueyoshi, Y.; Machida, M.; Yonezawa, Y.; Matsuyama, Y.; Wakao, N. Retrospective multicenter study of surgical treatments for osteoporotic vertebral fractures. J. Orthop. Sci. 2010, 15, 289–293. [Google Scholar] [CrossRef]
- Schnake, K.; Hahn, P.; Pajenda, G.; Katscher, S.; Franck, A.; Ullrich, B.; Verheyden, A.; Mörk, S.; Zimmermann, V.; Gonschorek, O.; et al. Multicenter data collection of Hospital treatment for osteoporotic vertebral fractures. Eur. Spine J. 2012, 21, 2344. [Google Scholar]
- Krismann, O.; Rauschmann, M.; Sellei, R.; Medina-Govea, F.; Meyer, F.; Vinas-Rios, J.M. Operative results of AO A3 and A4 traumatic injuries in the thoracic and lumbar spine. A multicenter surveillance study of 4230 patients from the German Spine Registry (DWG-Register). J. Neurosurg. Sci. 2023, 67, 543–549. [Google Scholar] [CrossRef]
- Pazos Mohri, A.; Puente Sánchez, L.; Diez Ulloa, M.A. Immediate standing X-ray predicts the final vertebral collapse in elderly patients with thoracolumbar burst fracture. Rev. Esp. Cir. Ortop. Traumatol. 2023, 67, T68–T74. [Google Scholar] [CrossRef]
- Cho, S.T.; Shin, D.E.; Kim, J.W.; Yoon, S.; Lee, H.I.; Lee, S. Prediction of Progressive Collapse in Osteoporotic Vertebral Fractures Using Conventional Statistics and Machine Learning. Spine 2023, 48, 1535–1543. [Google Scholar] [CrossRef]
- Baum, T.; Grande Garcia, E.; Burgkart, R.; Gordijenko, O.; Liebl, H.; Jungmann, P.M.; Gruber, M.; Zahel, T.; Rummeny, E.J.; Waldt, S.; et al. Osteoporosis imaging: Effects of bone preservation on MDCT-based trabecular bone microstructure parameters and finite element models. BMC Med. Imaging 2015, 15, 22. [Google Scholar] [CrossRef]
- Zaia, A.; Maponi, P.; Sallei, M.; Galeazzi, R.; Scendoni, P. Measuring Drug Therapy Effect on Osteoporotic Fracture Risk by Trabecular Bone Lacunarity: The LOTO Study. Biomedicines 2023, 11, 781. [Google Scholar] [CrossRef]
- Pappou, I.P.; Papadopoulos, E.C.; Swanson, A.N.; Cammisa, F.P.; Girardi, F.P. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kümmel’s disease). Orthopedics 2008, 31, 61–66. [Google Scholar] [PubMed]
- Goldstein, S.; Smorgick, Y.; Mirovsky, Y.; Anekstein, Y.; Blecher, R.; Tal, S. Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J. Clin. Neurosci. 2016, 31, 122–126. [Google Scholar] [CrossRef]


| Type of Fracture | Total Sample n (%) 1 | No Collapse (n = 85) n (%) | Collapse (n = 143) n (%) | p-Value |
|---|---|---|---|---|
| Genant (morphological) | a | a | ||
| Wedge | 91 (43.8) | 54 (51.9) | 50 (48.1) | 0.01 * |
| Biconcave | 104 (50) | 64 (70.3) | 27 (29.7) | |
| Crush | 13 (6.3) | 5 (38.5) | 8 (61.5) | |
| Genant (semiquantitative grading) | ||||
| Grade 0.5 | 99 (47.6) | 58 (58.6) | 41 (41.4) | 0.843 |
| Grade 1 | 46 (22.1) | 26 (56.5) | 20 (43.5) | |
| Grade 2 | 63 (30.3) | 39 (61.9) | 24 (38.1) | |
| Sugita | ||||
| Swelled-front | 32 (15.4) | 12 (37.5) | 20 (62.5) | 0.008 * |
| Bow-shaped | 128 (61.5) | 88 (68.8) | 40 (31.3) | |
| Projecting | 26 (12.5) | 12 (46.2) | 14 (53.8) | |
| Concave | 11 (5.3) | 5 (45.5) | 6 (54.5) | |
| Dented | 11 (5.3) | 6 (54.5) | 5 (45.5) | |
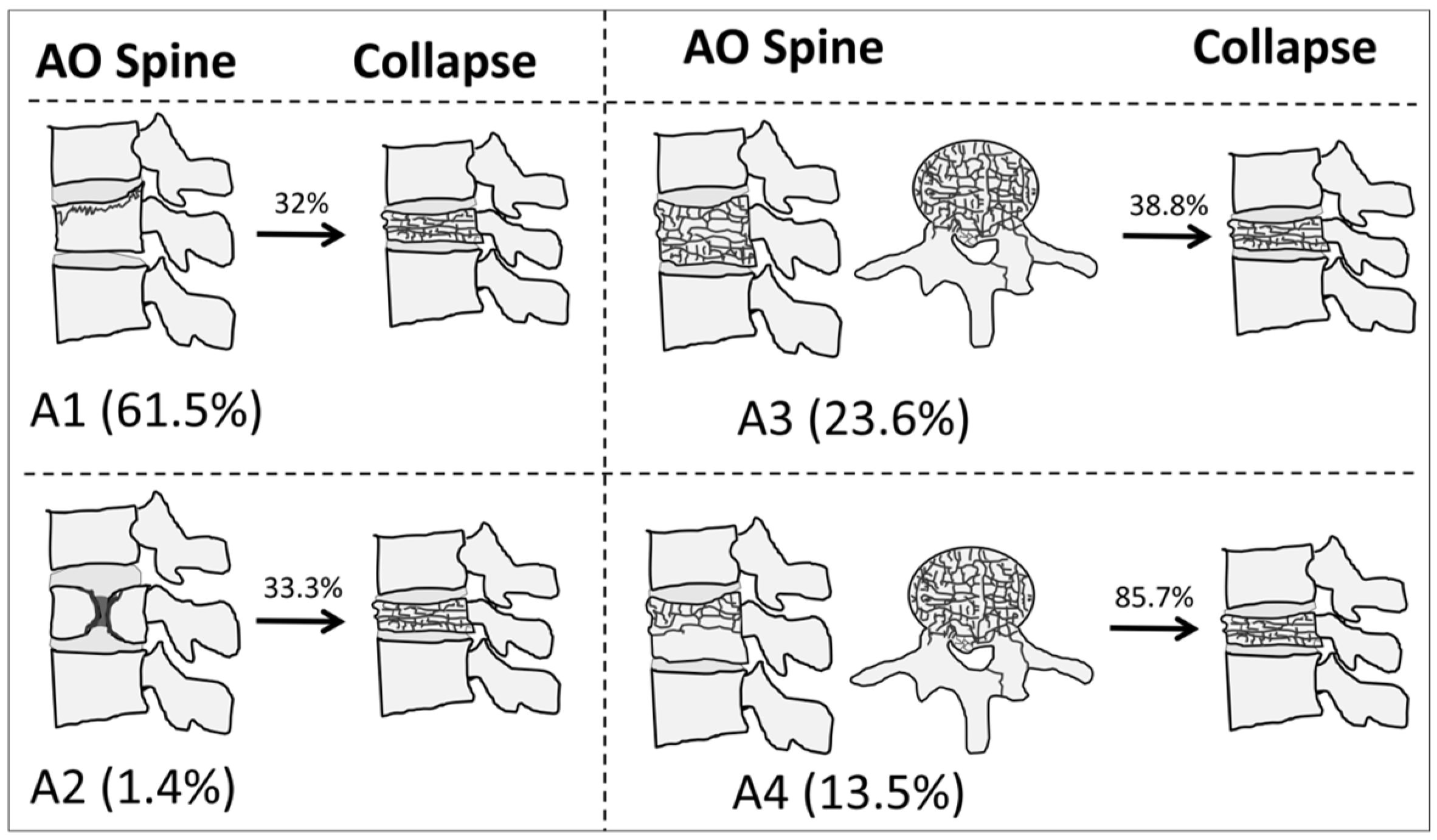
| AO Spine | ||||
| A1 | 128 (61.5) | 87 (68) | 41 (32) | <0.001 * |
| A2 | 3 (1.4) | 2 (66.7) | 1 (33.3) | |
| A3 | 49 (23.6) | 30 (61.2) | 19 (38.8) | |
| A4 | 28 (13.5) | 4 (14.3) | 24 (85.7) | |
| DGOU | ||||
| OF1 | 9 (4.3) | 7 (77.8) | 2 (22.2) | 0.049 * |
| OF2 | 154 (74) | 97 (63) | 57 (37) | |
| OF3 | 39 (18.8) | 17 (43.6) | 22 (56.4) | |
| OF4 | 6 (2.9) | 2 (33.3) | 4 (66.7) |
| Classification System | p-Value [Univariate] | OR [95% CI] | p-Value [Multivariate] | aOR [95%CI] |
|---|---|---|---|---|
| Sugita | 0.852 | 1.024 [0.800–1.309] | - | - |
| Genant (morphological) | 0.266 | 0.770 [0.485–1.221] | - | - |
| Genant (quantitative) | 0.709 | 0.941 [0.683–1.296] | - | - |
| AO Spine | <0.001 | 1.418 [1.192–1.686] | 0.001 | 1.356 [1.130–1.626] |
| DGOU | 0.007 | 2.059 [1.215–3.490] | 0.121 | 1.545 [0.891–2.679] |
| AO Spine [Ref 1, A1] | Estimate | Std. Error | p-Value | OR [95%CI] |
|---|---|---|---|---|
| Intercept | −0.752 | 0.189 | <0.001 * | 0.47 [0.32–0.68] |
| A2 | 0.059 | 1.239 | 0.926 | 1.06 [0.05–11.38] |
| A3 | 0.296 | 0.349 | 0.397 | 1.34 [0.67–2.65] |
| A4 | 2.544 | 0.572 | <0.001 * | 12.73 [4.57–45.47] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Láinez Ramos-Bossini, A.J.; Jiménez Gutiérrez, P.M.; Luengo Gómez, D.; Rivera Izquierdo, M.; Benítez, J.M.; Ruiz Santiago, F. A Comparative Analysis of International Classification Systems to Predict the Risk of Collapse in Single-Level Osteoporotic Vertebral Fractures. Diagnostics 2024, 14, 2152. https://doi.org/10.3390/diagnostics14192152
Láinez Ramos-Bossini AJ, Jiménez Gutiérrez PM, Luengo Gómez D, Rivera Izquierdo M, Benítez JM, Ruiz Santiago F. A Comparative Analysis of International Classification Systems to Predict the Risk of Collapse in Single-Level Osteoporotic Vertebral Fractures. Diagnostics. 2024; 14(19):2152. https://doi.org/10.3390/diagnostics14192152
Chicago/Turabian StyleLáinez Ramos-Bossini, Antonio Jesús, Paula María Jiménez Gutiérrez, David Luengo Gómez, Mario Rivera Izquierdo, José Manuel Benítez, and Fernando Ruiz Santiago. 2024. "A Comparative Analysis of International Classification Systems to Predict the Risk of Collapse in Single-Level Osteoporotic Vertebral Fractures" Diagnostics 14, no. 19: 2152. https://doi.org/10.3390/diagnostics14192152
APA StyleLáinez Ramos-Bossini, A. J., Jiménez Gutiérrez, P. M., Luengo Gómez, D., Rivera Izquierdo, M., Benítez, J. M., & Ruiz Santiago, F. (2024). A Comparative Analysis of International Classification Systems to Predict the Risk of Collapse in Single-Level Osteoporotic Vertebral Fractures. Diagnostics, 14(19), 2152. https://doi.org/10.3390/diagnostics14192152








