The Validity of the Original and the Saudi-Modified Screening Tools for the Assessment of Malnutrition in Pediatrics: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Ethical Board Approval
2.4. Sociodemographic Data and Medical Variables of the Patient
2.5. Anthropometric Measurements
2.6. Nutritional Screening
2.6.1. The Original Screening Tool for the Assessment of Malnutrition in Pediatrics (oSTAMP)
2.6.2. Saudi Modified Screening Tool for the Assessment of Malnutrition in Pediatrics (S-mSTAMP)
2.7. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Nutrition Status Characteristics Based on Anthropometric Measurements
3.3. Nutritional Status Characteristics Based on the Original and the Saudi Modified Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP)
3.4. Anthropometric Characteristics of Hospitalized Children According to Original and Saudi Modified Screening Tool for the Assessment of Malnutrition in Pediatricsc (STAMP)
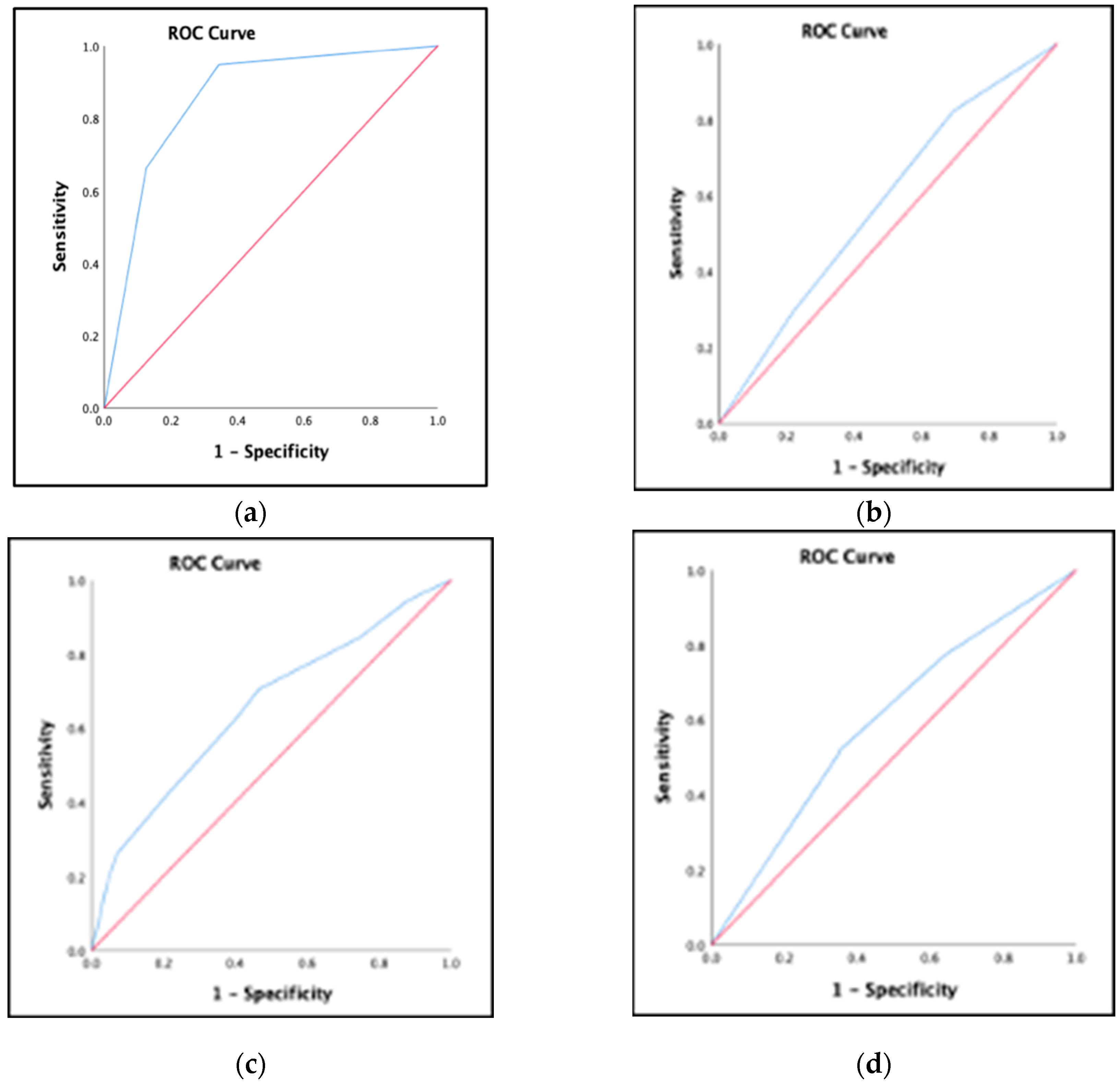
3.5. Prevalence of Patients at High Risk of Malnutrition, Validity, and Agreements of Saudi Modified Screening Tool for the Assessment of Malnutrition in Pediatrics Using Original Screening Tool for the Assessment of Malnutrition in Pediatrics
3.6. Prevalence of Patients at High Risk of Malnutrition, and Validity of Saudi-Modified Screening Tool for the Assessment of Malnutrition in Pediatrics Using Anthropometric Reference Standards
3.7. Prevalence of Patients at High Risk of Malnutrition and Validity of the Original Screening Tool for the Assessment of Malnutrition in Pediatrics Using Anthropometric Measurements and Dietary Intake as Reference Standard
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications for Practice and Future Direction
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pelletier, D.L.; Frongillo, E.A.; Habicht, J.P. Epidemiologic evidence for a potentiating effect of malnutrition on child mortality. Am. J. Public Health 1993, 83, 1130–1133. [Google Scholar] [CrossRef] [PubMed]
- Pollack, M.M.; Ruttimann, U.E.; Wiley, J.S. Nutritional Depletions in Critically Ill Children: Associations with Physiologic Instability and Increased Quantity of Care. J. Parenter. Enter. Nutr. 1985, 9, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Campanozzi, A.; Russo, M.; Catucci, A.; Rutigliano, I.; Canestrino, G.; Giardino, I.; Romondia, A.; Pettoello-Mantovani, M. Hospital-acquired malnutrition in children with mild clinical conditions. Nutrition 2009, 25, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.J.; Zhou, H.J.; Liu, P.J.; Liu, G.L.; Zheng, Y.; Wei, B.; Hao, C.X.; Zhang, Y.; Kang, H.Q.; Lu, X.L. Risks of undernutrition and malnutrition in hospitalized pediatric patients with spinal cord injury. Spinal Cord. 2017, 55, 247–254. [Google Scholar] [CrossRef][Green Version]
- WHO (World Health Organization). Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 20 July 2023).
- Mehta, N.M.; Corkins, M.R.; Lyman, B.; Malone, A.; Goday, P.S.; Carney, L.; Monczka, J.L.; Plogsted, S.W.; Schwenk, W.F. Defining Pediatric Malnutrition. J. Parenter. Enter. Nutr. 2013, 37, 460–481. [Google Scholar] [CrossRef]
- National Health Service. Malnutrition. Available online: https://www.nhs.uk/conditions/malnutrition/causes/#:~:text=Some%20health%20conditions%20that%20can,as%20chronic%20obstructive%20pulmonary%20disease) (accessed on 3 October 2023).
- World Health Organization. 10 Facts on Child Health. Children: Reducing Mortality. Available online: http://www.who.int/mediacentre/factsheets/fs178/en/ (accessed on 20 October 2023).
- Wang, H.; Abbas, K.M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; Abolhassani, H.; Abreu, L.G.; Abrigo, M.R. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [Google Scholar] [CrossRef]
- Asiri, A.M.; Alomary, S.A.; AL Qahtani, S.A.; Adam, I.F.; Amer, S.A. Determinants of the Underlying Causes of Mortality during the First Wave of COVID-19 Pandemic in Saudi Arabia: A Descriptive National Study. Int. J. Environ. Res. Public Health 2021, 18, 12647. [Google Scholar] [CrossRef]
- Agostoni, C.; Axelson, I.; Colomb, V.; Goulet, O.; Koletzko, B.; Michaelsen, K.F.; Puntis, J.W.L.; Rigo, J.; Shamir, R.; Szajewska, H. The Need for Nutrition Support Teams in Pediatric Units: A Commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2005, 41, 8–11. [Google Scholar]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Wonoputri, N.; Djais, J.T.B.; Rosalina, I. Validity of Nutritional Screening Tools for Hospitalized Children. J. Nutr. Metab. 2014, 2014, 1–6. [Google Scholar] [CrossRef]
- Chourdakis, M.; Hecht, C.; Gerasimidis, K.; Joosten, K.F.; Karagiozoglou-Lampoudi, T.; Koetse, H.A.; Ksiazyk, J.; Lazea, C.; Shamir, R.; Szajewska, H.; et al. Malnutrition risk in hospitalized children: Use of 3 screening tools in a large European population. Am. J. Clin. Nutr. 2016, 103, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Hartman, C.; Shamir, R.; Hecht, C.; Koletzko, B. Malnutrition screening tools for hospitalized children. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Huysentruyt, K.; Devreker, T.; Dejonckheere, J.; De-Schepper, J.; Vandenplas, Y.; Cools, F. Accuracy of Nutritional Screening Tools in Assessing the Risk of Undernutrition in Hospitalized Children. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 159–166. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, H.; Dixon, M.; Crabtree, I.; Eaton-Evans, M.J.; McNulty, H. The development and evaluation of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP©) for use by healthcare staff. J. Hum. Nutr. Diet. 2012, 25, 311–318. [Google Scholar] [CrossRef]
- Becker, P.J.; Bellini, S.G.; Vega, M.W.; Corkins, M.R.; Spear, B.A.; Spoede, E.; Hoy, M.K.; Piemonte, T.A.; Rozga, M. Validity and Reliability of Pediatric Nutrition Screening Tools for Hospital, Outpatient, and Community Settings: A 2018 Evidence Analysis Center Systematic Review. J. Acad. Nutr. Diet. 2020, 120, 288–318. [Google Scholar] [CrossRef]
- Carey, A.; McCarthy, H.; Thompson, A.; McNulty, H. A pilot study evaluating the use of STAMP© nutrition screening tool in hospitalized infants. Clin. Nut. ESPEN 2015, 10, 174–212. [Google Scholar]
- Klanjsek, P.; Pajnkihar, M.; Marcun, V.N.; Povalej, B.P. Screening and assessment tools for early detection of malnutrition in hospitalised children: A systematic review of validation studies. BMJ Open 2019, 9, e025444. [Google Scholar] [CrossRef]
- Sayed, S.; El-Shabrawi, M.H.F.; Abdelmonaem, E.; El-Koofy, N.; Tarek, S. Value of Nutritional Screening Tools Versus Anthropometric Measurements in Evaluating Nutritional Status of Children in a Low/Middle-Income Country. Pediatr. Gastroenterol. Hepatol. Nutr. 2023, 26, 213. [Google Scholar] [CrossRef]
- Becker, P.J.; Nieman, C.L.; Corkins, M.R.; Monczka, J.; Smith, E.; Smith, S.E.; Spear, B.A.; White, J.V. Consensus Statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Indicators Recommended for the Identification and Documentation of Pediatric Malnutrition (Undernutrition). J. Acad. Nutr. Diet. 2014, 114, 1988–2000. [Google Scholar] [CrossRef]
- Katsagoni, C.N.; Cheirakaki, O.; Hatzoglou, A.; Zerva, O.; Koulieri, A.; Loizou, K.; Vasileiadi, E.; Toilou, M.; Poulia, K.A.; Kontogianni, M.D. Malnutrition in Hospitalised Children—An Evaluation of the Efficacy of Two Nutritional Screening Tools. Nutrients 2021, 13, 1279. [Google Scholar] [CrossRef]
- El-Mouzan, M.; Al-Herbish, A.; Al-Salloum, A.; Qurachi, M.; Al-Omar, A. Growth charts for Saudi children and adolescents. Saudi Med. J. 2007, 28, 1555–1568. [Google Scholar] [PubMed]
- Pérez-Solís, D.; Larrea-Tamayo, E.; Menéndez-Arias, C.; Molinos-Norniella, C.; Bueno-Pardo, S.; Jiménez-Treviño, S.; Bousoño-Garcia, C.; Díaz-Martín, J.J. Assessment of Two Nutritional Screening Tools in Hospitalized Children. Nutrients 2020, 12, 1221. [Google Scholar] [CrossRef] [PubMed]
- Toledano-Toledano, F.; Rodríguez-Rey, R.; Moral-de-la-Rubia, J.; Luna, D. A Sociodemographic variables questionnaire (Q-SV) for research on family caregivers of children with chronic disease. BMC Psychol. 2019, 7, 85. [Google Scholar] [CrossRef]
- Klanjšek, P.; Pajnkihar, M.; Marčun, V.N.; Močnik, M.; Golob-Jančič, S.; Povalej-Bržan, P. Development and Validation of a New Screening Tool with Non-Invasive Indicators for Assessment of Malnutrition Risk in Hospitalised Children. Children 2022, 9, 731. [Google Scholar] [CrossRef] [PubMed]
- NACS. Nutrition Assessment and Classification. Available online: https://www.fantaproject.org/sites/default/files/resources/NACS-Users-Guide-Module2-May2016.pdf (accessed on 19 December 2022).
- Neelemaat, F.; Meijers, J.; Kruizenga, H.; van-Ballegooijen, H.; van-Bokhorst-de-van-der-Schueren, M. Comparison of five malnutrition screening tools in one hospital inpatient sample. J. Clin. Nurs. 2011, 20, 2144–2152. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Central of Disease Control and Prevention. Saudi Arabia Top 10 Causes of Death. 2019. Available online: https://stacks.cdc.gov/view/cdc/82200 (accessed on 12 October 2023).
- World Health Organization. Child and Adolescent Health. Available online: https://www.emro.who.int/child-adolescent-health/data-statistics/saudi-arabia.html (accessed on 12 October 2023).
- El-Mouzan, M.; Al-Salloum, A.; Alqurashi, M.; Al-Herbish, A.; Al-Omar, A. The LMS and Z scale growth reference for Saudi school-age children and adolescents. Saudi J. Gastroenterol. 2016, 22, 331. [Google Scholar] [CrossRef]
- El-Mouzan, M.I.; Shaffi, A.; Al-Salloum, A.; Alqurashi, M.M.; Al-Herbish, A.; Al-Omer, A. Z-score growth reference data for Saudi preschool children. Ann. Saudi Med. 2017, 37, 10–15. [Google Scholar] [CrossRef]
- Ong, S.H.; Chee, W.S.S.; Lapchmanan, L.M.; Ong, S.N.; Lua, Z.C.; Yeo, J.X.N. Validation of the Subjective Global Nutrition Assessment (SGNA) and Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP) to Identify Malnutrition in Hospitalized Malaysian Children. J. Trop. Pediatr. 2019, 65, 39–45. [Google Scholar] [CrossRef]
- Reed, M.; Mullaney, K.; Ruhmann, C.; March, P.; Conte, V.H.; Noyes, L.; Bleazard, M. Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) in the Electronic Health Record: A Validation Study. Nutr. Clin. Pract. 2020, 35, 1087–1093. [Google Scholar] [CrossRef]
- Tuokkola, J.; Hilpi, J.; Kolho, K.L.; Orell, H.; Merras-Salmio, L. Nutritional risk screening—A cross-sectional study in a tertiary pediatric hospital. J. Health Popul. Nutr. 2019, 38, 8. [Google Scholar] [CrossRef]
| Patient’s Characteristics | |
|---|---|
| Wight (kg) ** All (n = 307) | Median & (IQR) |
| 15.2 (13.5) | |
| Length/Height (cm) * All (n = 307) | Mean ± SD |
| 104.2 ± 26.73 | |
| MUAC (mm) * All (n = 307) | Mean ± SD |
| 153.37 ± 40.69 | |
| BMI (kg/m2) * All (n = 307) | Mean ± SD |
| 17.12 ± 4.69 | |
| Admission Diagnosis Documented *** All (n = 307) | Number and Percentage |
| Bowel failure, intractable diarrhea | 11 (3.6%) |
| Burns and major trauma | 4 (1.3%) |
| Liver disease | 3 (1%) |
| Major surgery | 6 (2%) |
| Food allergies/intolerance | 4 (1.3%) |
| Oncology on active treatments | 1 (0.3%) |
| Renal disease/failure | 8 (2.6%) |
| Inborn errors of metabolism | 14 (4.6%) |
| Coeliac disease | 1 (0.3%) |
| Gastro-esophageal reflux | 12 (3.9%) |
| Diabetes | 9 (2.9%) |
| Respiratory syncytial virus | 1 (0.3%) |
| Minor surgery | 1 (0.3%) |
| Asthma | 104 (33.9%) |
| Neuromuscular conditions | 18 (5.9%) |
| Under investigation | 177 (57.7%) |
| Pneumonia | 38 (12.4%) |
| Acute diarrhea | 12 (3.9%) |
| Respiratory Infection | 16 (5.2%) |
| Neonatal disorder | 7 (2.3%) |
| Variables | Sample Size |
|---|---|
| Number and Percentage | |
| Weight-for-height Z-score (WHO/CDC) * | N = 155 (age < 59 months) |
| Malnutrition | 48 (31%) |
| Absence of malnutrition | 107 (69%) |
| Weight-for-height Z-score (Saudi) * | N = 155 (age < 59 months) |
| Malnutrition | 36 (23.2%) |
| Absence of malnutrition | 119 (76.8%) |
| BMI-for-age Z-score (CDC) * | N = 152 (age > 59 months) |
| Malnutrition | 43 (28.3%) |
| Absence of malnutrition | 109 (71.7%) |
| BMI-for-age Z-score (Saudi) * | N = 152 (age > 59 months) |
| Malnutrition | 39 (25.7%) |
| Absence of malnutrition | 113 (74.3%) |
| STEPs | Original STAMP | Saudi-Modified STAMP |
|---|---|---|
| Number and Percentage | ||
| STEP 1—DIAGNOSIS * Does the child have a diagnosis that has any nutritional implications? | ||
| Definite nutritional implications | 51 (16.6%) | 80 (26.1%) |
| Possible nutritional implications | 27 (8.8%) | 72 (23.5%) |
| No nutritional implications | 229 (74.6%) | 155 (50.5%) |
| STEP 2—NUTRITIONAL INTAKE * What is the child’s nutritional intake? | ||
| No change in eating patterns and good nutritional intake | 160 (52.1%) | 75 (24.4%) |
| Recently decreased or poor nutritional intake | 124 (40.4%) | 154 (50.2%) |
| No nutritional intake | 23 (7.5%) | 78 (25.4%) |
| STEP 3—WEIGHT AND HEIGHT * Using the centile quick-reference tables to determine the child’s measurements | ||
| 0 to 1 centile spaces/columns apart | 175 (57%) | 94 (30.6%) |
| >2 centile spaces/=2 columns apart | 93 (30.3%) | 85 (27.7%) |
| >3 centile spaces/≥3 columns apart (or weight < 2nd centile) | 39 (12.7%) | 128 (41.7%) |
| STEP 4—OVERALL RISK OF MALNUTRITION * Add the scores from steps 1–3 together to calculate the child’s overall risk of malnutrition. | ||
| High risk | 72 (23.5%) | 189 (61.5%) |
| Medium risk | 121 (39.4%) | 92 (30%) |
| Low risk | 114 (37.1%) | 26 (8.5%) |
| Nutritional status * | ||
| At high risk | 193 (62.9%) | 281 (91.5%) |
| At low risk | 114 (37.1%) | 26 (8.5%) |
| Anthropometric Measurements | Nutritional Status | All | At Low Risk | At High Risk | p-Value |
|---|---|---|---|---|---|
| Number and Percentage | |||||
| Overall Original STAMP Score (n = 307) | |||||
| Saudi weight-for-height Z-scores (n = 155) * | Malnutrition | 36 (23.2%) | 12 (18.7%) | 24 (26.4%) | 0.268 a |
| Absence of malnutrition | 119 (76.8%) | 52 (81.3%) | 67 (73.6%) | ||
| Saudi BMI-for-age Z-scores (n = 152) * | Malnutrition | 39 (25.7%) | 10 (20%) | 29 (28.4%) | 0.263 a |
| Absence of malnutrition | 113 (74.3%) | 40 (80%) | 73 (71.6%) | ||
| WHO and CDC weight-for-height Z-scores (n = 155) * | Malnutrition | 48 (31%) | 16 (24.6%) | 32 (35.6%) | 0.146 a |
| Absence of malnutrition | 107 (69%) | 49 (75.4%) | 58 (64.4%) | ||
| CDC BMI-for-age Z-scores (n = 152) * | Malnutrition | 43 (28.3%) | 13 (26.5%) | 30 (29.1%) | 0.740 a |
| Absence of malnutrition | 109 (71.7%) | 36 (73.5%) | 73 (70.9%) | ||
| Overall Saudi-Modified STAMP Score (n = 307) | |||||
| Saudi weight-for-height Z-scores (n = 155) * | Malnutrition | 36 (23.2%) | 2 (18.2%) | 34 (23.6%) | 1 a |
| Absence of malnutrition | 119 (76.8%) | 9 (81.8%) | 110 (76.4%) | ||
| Saudi BMI-for-age Z-scores (n = 152) * | Malnutrition | 39 (25.7%) | 2 (13.3%) | 37 (27%) | 0356 a |
| Absence of malnutrition | 113 (74.3%) | 13 (86.7%) | 100 (73%) | ||
| WHO and CDC weight-for-height Z-scores (n = 155) * | Malnutrition | 48 (31%) | 1 (9.1%) | 47 (32.6%) | 0.174 a |
| Absence of malnutrition | 107 (69%) | 10 (90.9%) | 97 (67.4%) | ||
| CDC BMI-for-age Z-scores (n = 152) * | Malnutrition | 43 (28.3%) | 2 (13.3%) | 41 (29.9%) | 0.235 a |
| Absence of malnutrition | 109 (71.7%) | 13 (86.7%) | 96 (70.1%) | ||
| Statistical Parameters of Concurrent Validity | Diagnosis | Nutritional Intake | Anthropometrics | Overall Nutritional Status |
|---|---|---|---|---|
| Sensitivity | 94.8% | 82.3% | 75.8% | 94.3% |
| Specificity | 65.7% | 30.6% | 36% | 13.2% |
| Positive Predictive Value | 48% | 52.2% | 47.2% | 64.8% |
| Negative Predictive Value | 97.4% | 65.3% | 66.3% | 57.7% |
| AUC (CI 95%) | 0.856 (0.810–0.902), p = 0.001 | 0.576 (0.512–0.640), p = 0.021 | 0.595 (0.531–0.659), p = 0.04 | 0.654 (0.592–0.715), p = 0.001 |
| Statistical Parameters of Concurrent Validity | WHO and CDC Weight-for-Height Z-Score | CDC BMI-for-Age Z-Score | Saudi Weight-for-Height Z-Score | Saudi BMI-for-Age Z-Score |
|---|---|---|---|---|
| Sensitivity | 97.9% | 95.3% | 94.4% | 94.9% |
| Specificity | 9.3% | 11.9% | 7.6% | 11.5% |
| Positive Predictive Value | 32.6% | 29.9% | 23.6% | 27% |
| Negative Predictive Value | 90.9% | 86.7% | 81.8% | 86.7% |
| Statistical Parameters of Concurrent Validity | WHO and CDC Weight-for-Height Z-Score | CDC BMI-for-Age Z-Score | Saudi Weight-for-Height Z-Score | Saudi BMI-for-Age Z-Score |
|---|---|---|---|---|
| Sensitivity | 54.2% | 69.8% | 66.7% | 74.4% |
| Specificity | 33.3% | 33% | 43.7 | 35.4% |
| Positive Predictive Value | 64.4% | 29% | 26.4% | 28.4% |
| Negative Predictive Value | 24.6% | 73.5% | 81.3% | 80% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, S.; Aldubayan, K.; Alshehri, S.; Almuhareb, G.; Mahnashi, A. The Validity of the Original and the Saudi-Modified Screening Tools for the Assessment of Malnutrition in Pediatrics: A Cross-Sectional Study. Diagnostics 2024, 14, 2256. https://doi.org/10.3390/diagnostics14202256
Alqahtani S, Aldubayan K, Alshehri S, Almuhareb G, Mahnashi A. The Validity of the Original and the Saudi-Modified Screening Tools for the Assessment of Malnutrition in Pediatrics: A Cross-Sectional Study. Diagnostics. 2024; 14(20):2256. https://doi.org/10.3390/diagnostics14202256
Chicago/Turabian StyleAlqahtani, Sheikha, Khalid Aldubayan, Saleh Alshehri, Ghada Almuhareb, and Amal Mahnashi. 2024. "The Validity of the Original and the Saudi-Modified Screening Tools for the Assessment of Malnutrition in Pediatrics: A Cross-Sectional Study" Diagnostics 14, no. 20: 2256. https://doi.org/10.3390/diagnostics14202256
APA StyleAlqahtani, S., Aldubayan, K., Alshehri, S., Almuhareb, G., & Mahnashi, A. (2024). The Validity of the Original and the Saudi-Modified Screening Tools for the Assessment of Malnutrition in Pediatrics: A Cross-Sectional Study. Diagnostics, 14(20), 2256. https://doi.org/10.3390/diagnostics14202256






