Abstract
Permanent pacemaker implantation is a low-risk procedure. However, complications may occur at a rate of around 4–8%. We present a case where initial implantation resulted in complications that could have been avoided by meticulous assessment of lead position in different projections and early post-procedure X-ray that would have delineated other serious complications. We present a case where the right ventricular lead was placed in the coronary sinus, which resulted in the loss of pacing capture with further syncope after the pacemaker implant. This was apparent in the post-procedure electrocardiogram (ECG) with right bundle branch pacing and the lead was repositioned in the right ventricular apex the following day. Furthermore, the patient was discharged home without a chest X-ray (CXR), and she represented a week later with a haemo-pneumothorax and pericardial effusion. A chest drain was placed and was discharged after a slow recovery following several complications that could have been avoidable.
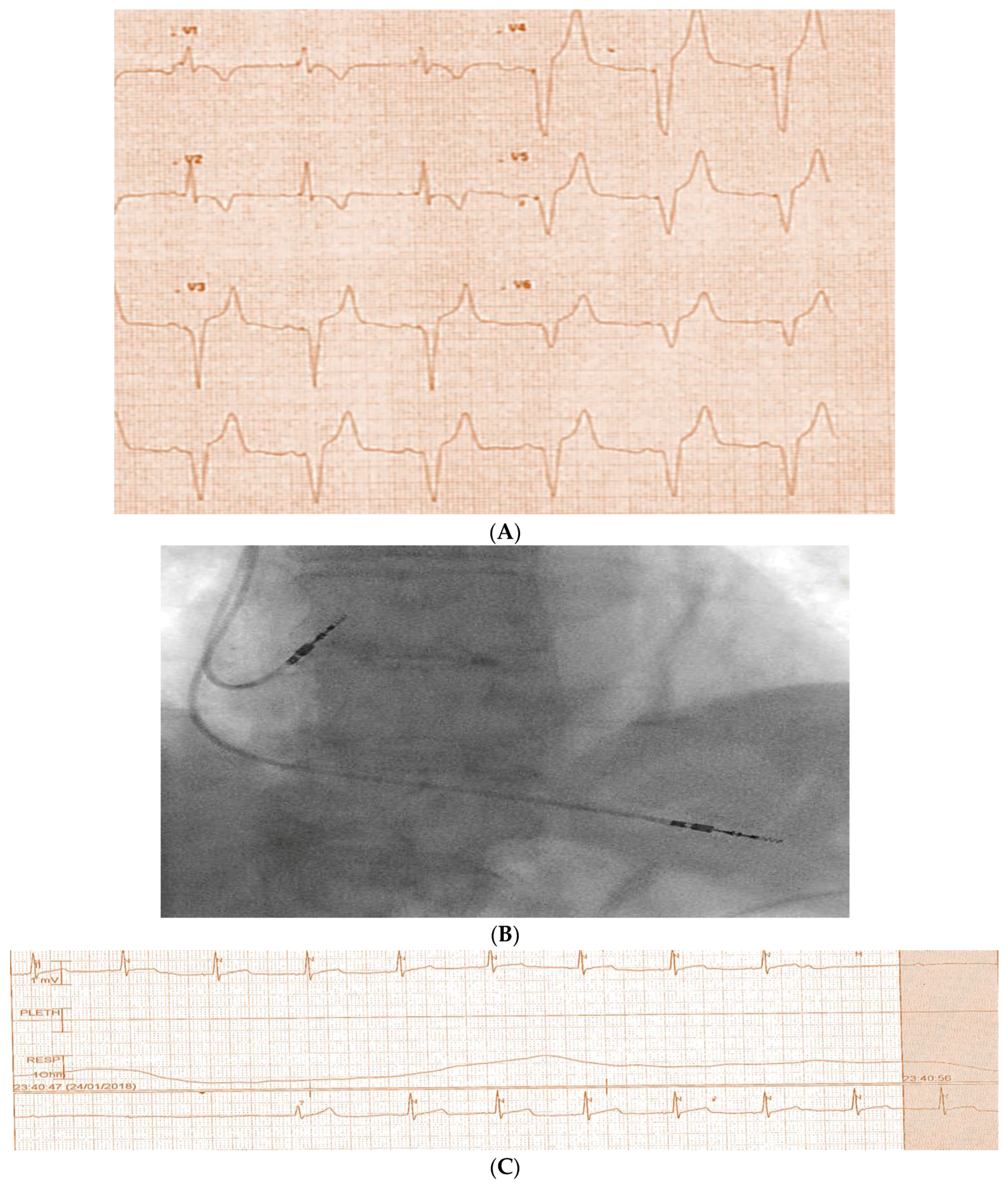
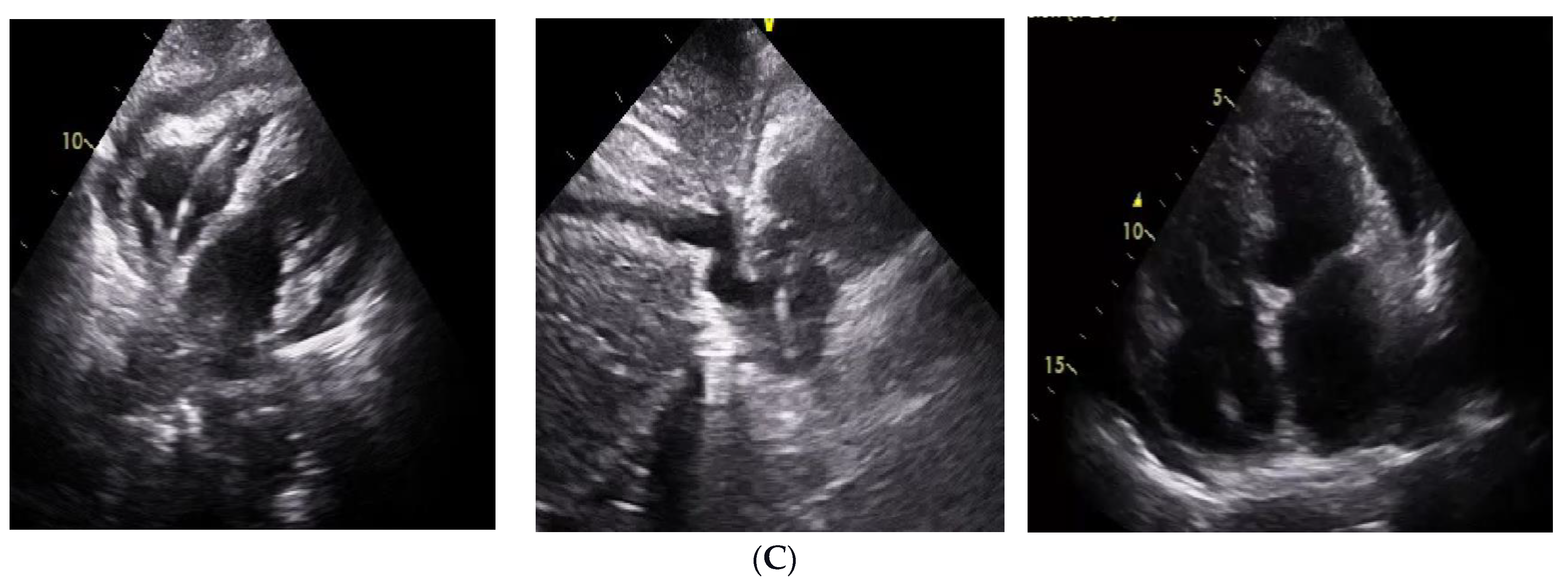
An eighty-seven-year-old female patient who has no co-morbidities and is not on any medications presented with syncope and a documented high-grade atrioventricular block (Figure 1). She had a dual chamber pacemaker implant with difficulty in placing the right ventricular (RV) lead, which was arduous, and multiple positions were checked until a final position was accepted. Afterward, she had another episode of syncope with loss of pacing capture in the cardiac care unit (Figure 2A–C). This was confirmed by pacing checks with loss of capture at the highest output.
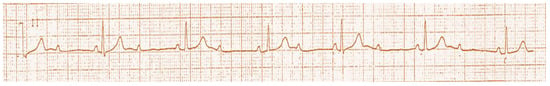
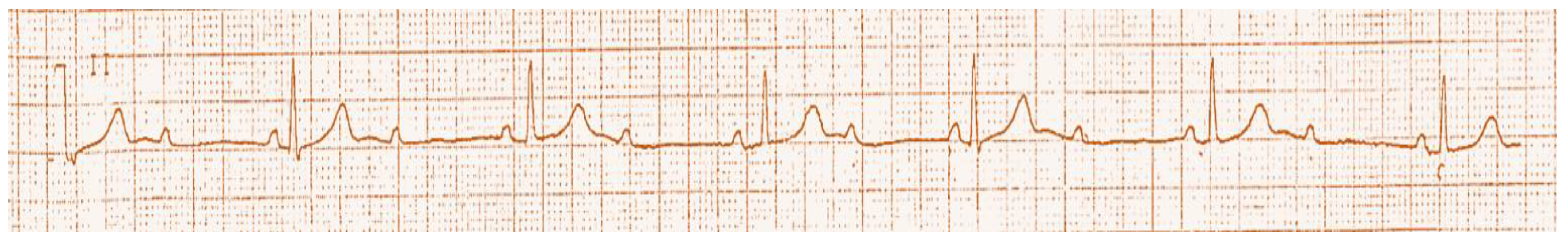
Figure 1.
Demonstration of the Mobitz type two, second-degree atrioventricular block.
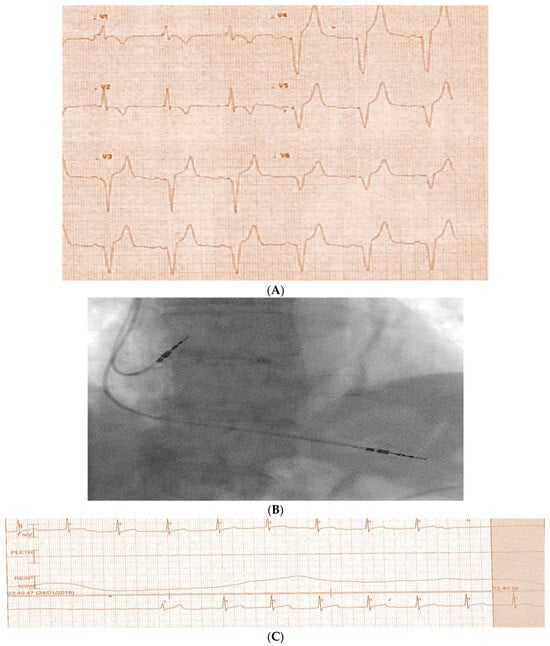
Figure 2.
(A) Demonstrates ECG-paced ventricular rhythm with right bundle branch block (RBBB) pattern. (B) Demonstrates dual chamber final implant by fluoroscopy, with right ventricular lead in the middle cardiac vein position rather than the right ventricular apex. (C) Telemetry monitor revealing sinus rhythm with a long pause after pacemaker implant.
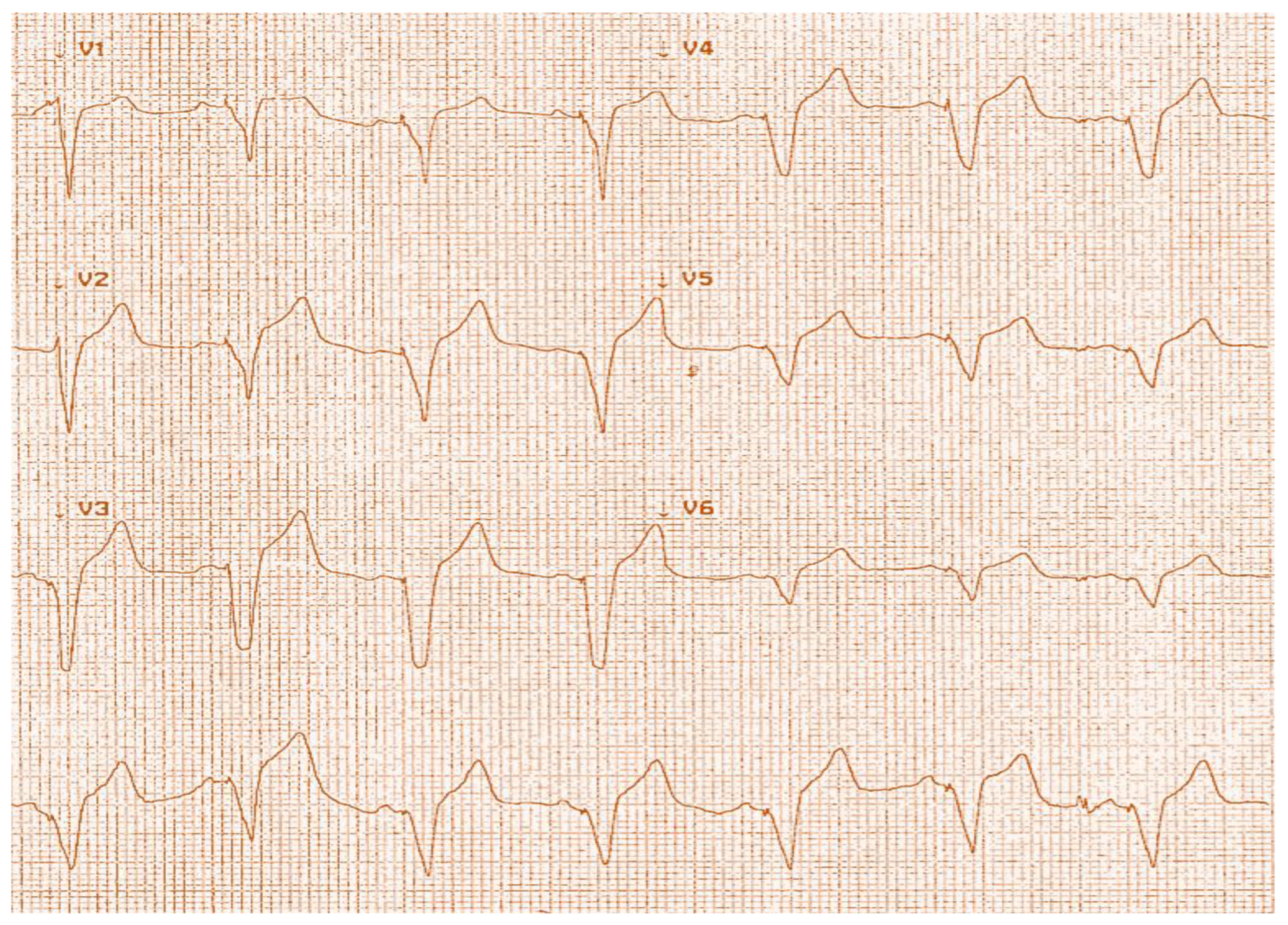
The patient had repositing of the RV lead in the right ventricular apex, and the following ECG showed left bundle branch block (LBBB) pattern pacing (Figure 3). Pacing checks were satisfactory after repositioning, and she was discharged home without a CXR.
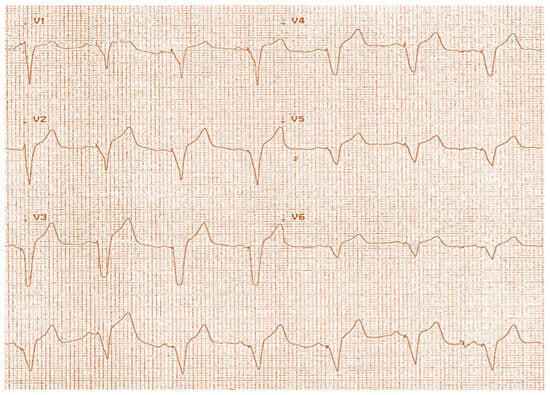
Figure 3.
ECG showing LBBB pattern pacing.
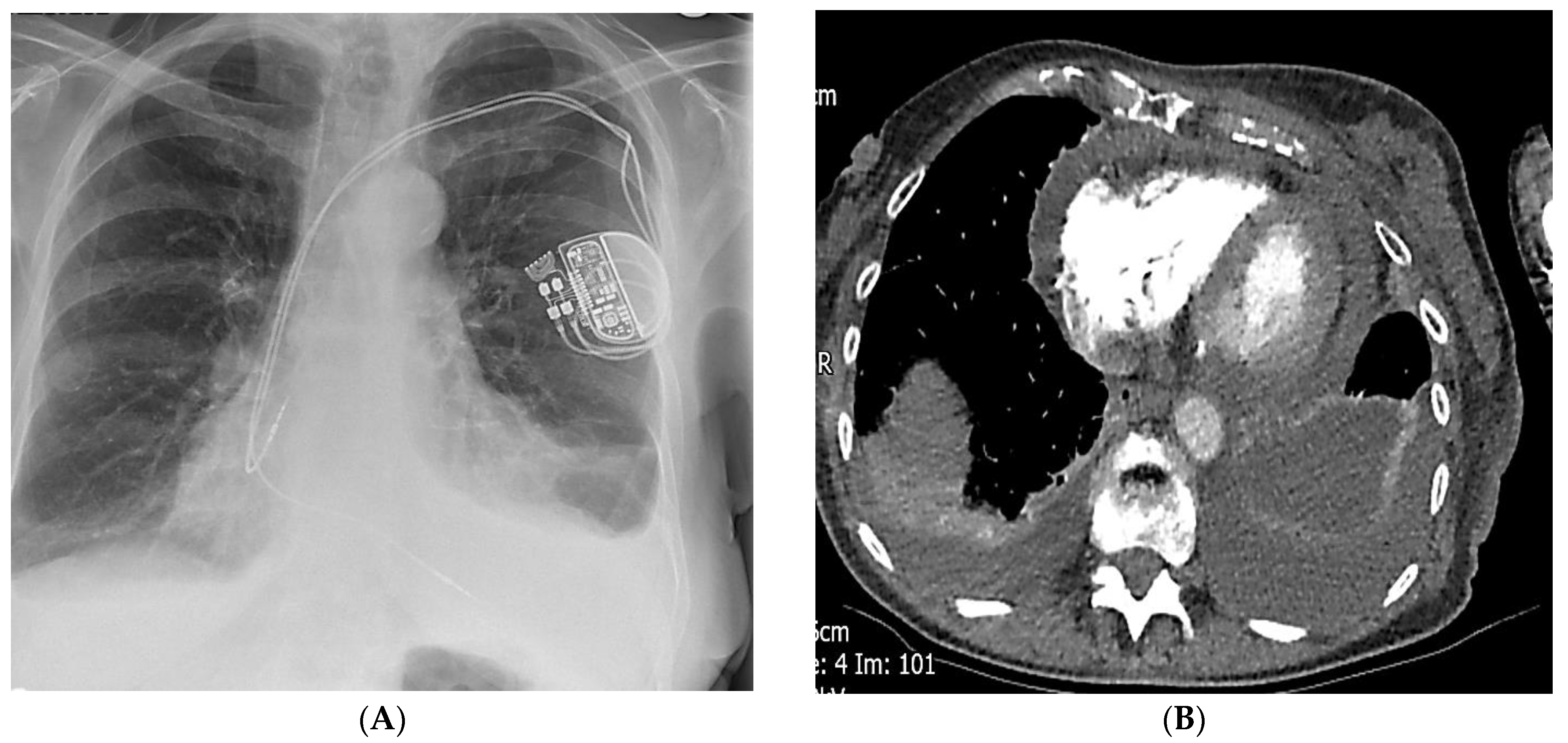
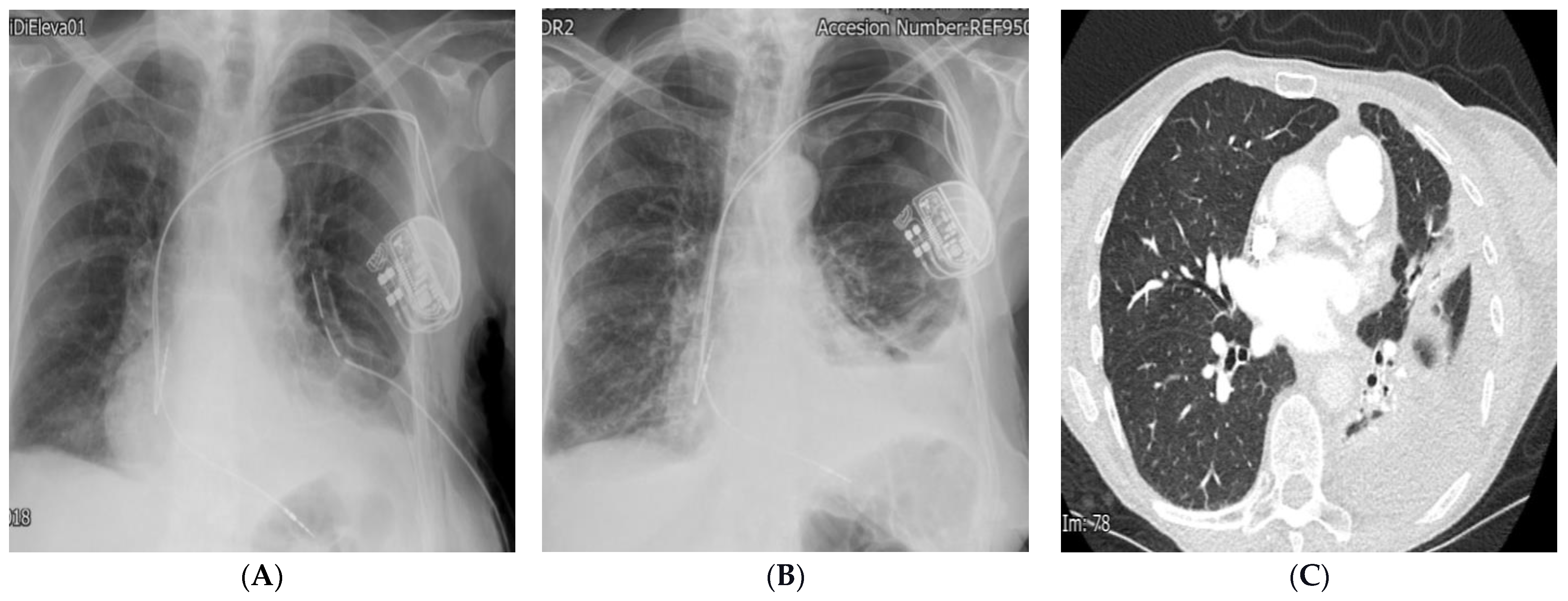
A week later, she was re-admitted with worsening dyspnoea. CXR and CT revealed haemopericardium and haemothorax, and she was treated with a chest drain and conservatively managed for pericardial effusion (Figure 4 and Figure 5). She had a slow recovery and was discharged home after treatment with no further symptoms during follow-up in the pacing clinic.
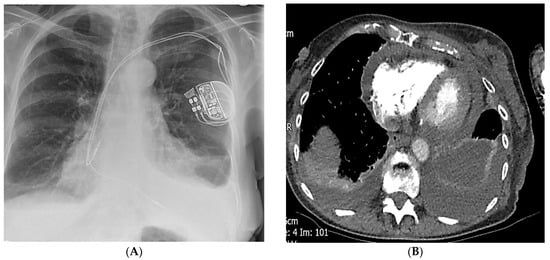
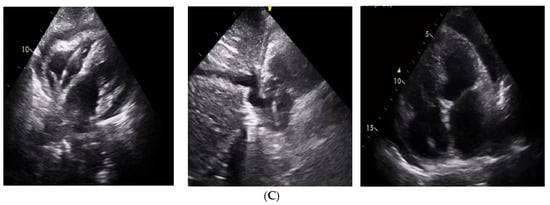
Figure 4.
(A) CXR demonstrates haemo-pneumothorax with dual chamber pacemaker leads in position. (B) CT showing bilateral pleural and pericardial effusion. (C) Echocardiography from subcoastal and apical windows showing moderate pericardial effusion, with inferior vena cava (IVC) collapse of more than 50%.
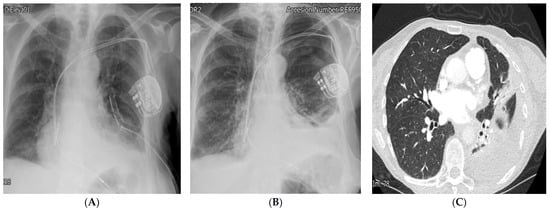
Figure 5.
(A) CXR demonstrates a left-sided chest drain. (B) CXR demonstrates residual left haemo-pneumothorax after drain removal. (C) CT revealing residual loculated haemothorax.
- Learning Points
Pacemaker complications may occur at a rate of around 4–8% [1].
ECG evaluation post-pacemaker implantation is essential, and pseudo RBBB with late V4 transition should raise the suspicion of coronary sinus pacing of the right ventricular lead [2].
ST elevation with injury current is an essential step during implant that alerts the operator to extracardiac placement and post-procedure complications [3].
LAO (Left anterior Oblique) projection will allow the operator to identify right ventricular versus coronary sinus lead placement during the procedure [2,3,4].
Chest X-ray and pacing interrogation are essential after all pacemaker implantations [5].
- Conclusions
This case revealed several valuable learning points that are highly educational. The puncture site caused the pneumothorax, which would have been noticed by CXR had it been performed before discharge. We suggest a simple CXR protocol to all patients, even if the cephalic approach was accessed, which will identify lead positions, displacements, or loose connections to the pacemaker box [5].
In addition, we believe that the first positioning of the right ventricular lead led to perforation into the right ventricle, which caused pericardial effusion. This was noticed with pacing checks with ST depression injury pattern rather than elevation, so it was repositioned but, unfortunately, was placed in the middle cardiac vein. Adopting a post-procedure quick bedside echocardiography after any patient with ST depression injury pattern during implant will unveil effusion and prevent mortality with tamponade [3]. This will identify patients who can be discharged early versus those who need longer monitoring.
Furthermore, had the last position of the right ventricular lead been checked in LAO projection, it would have shown the position in the middle cardiac vein of the coronary sinus and would have been repositioned rather than accepting an unstable position with lead movement and loss of capture, resulting in further syncope and the need for another procedure. We promote the importance of the LAO approach to identify the true position of the right ventricular lead, identifying the coronary sinus position if the right ventricular lead crosses the midline [2,4].
Author Contributions
Conceptualization, N.W.; Data curation, N.W.; Project administration, N.W. and M.I.; Supervision, N.W. and M.I.; Validation, N.W., M.I., C.B., A.A., K.H. and J.P.; Writing—original draft, N.W. and M.I.; Writing—review and editing, N.W. and M.I. All authors have read and agreed to the published version of the manuscript.
Funding
The authors confirmed that no funding was received.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, the ethical approval is not needed, as not a study, just a single patient.
Informed Consent Statement
The patient had agreed in a written consent and informed consent for publication for this study because none of the data in the paper reveal the patient’s identity.
Data Availability Statement
The data are available on request from the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Carrión-Camacho, M.R.; Marín-León, I.; Molina-Doñoro, J.M.; González-López, J.R. Safety of Permanent Pacemaker Implantation: A Prospective Study. J. Clin. Med. 2019, 8, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muthumala, A.; Herring, N.; Wong, K. A case of difficult RV lead placement. Heart 2013, 100, 434–435. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, A.; Farmer, D.M.; Homoud, M. Pacemaker Interrogation and Programming. In Cardiology Procedures; Hendel, R.C., Kimmelstiel, C., Eds.; Springer: Cham, Switzerland, 2013. [Google Scholar] [CrossRef]
- Squara, F.; Scarlatti, D.; Riccini, P.; Garret, G.; Moceri, P.; Ferrari, E. Individualized Left Anterior Oblique Projection. A Highly Reliable Patient-Tailored Fluoroscopy Criterion for Right Ventricular Lead Positioning. Circ. Arrhythmia Electrophysiol. 2018, 11, e006107. [Google Scholar] [CrossRef] [PubMed]
- Mathew, R.P.; Alexander, T.; Patel, V.; Low, G. Chest radiographs of cardiac devices (Part 1): Cardiovascular implantable electronic devices, cardiac valve prostheses and Amplatzer occluder devices. SA J. Radiol. 2019, 23, 1730, Erratum in SA J. Radiol. 2021, 25, 2256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).