Predictive Factors and Risk Assessment for Hospitalization in Chest Pain Patients Admitted to the Emergency Department
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Physician Groups and Training Protocols
2.3. Data Collection
2.4. ECG Changes
2.5. Diagnosis at Admission
2.6. Statistical Methods
3. Results
3.1. Comparison of Demographic Characteristics and Chronic Illnesses Between the Two Cohorts
3.2. Clinical Symptoms and Laboratory Data
3.3. Diagnosis Classifications and Treatment at the ED
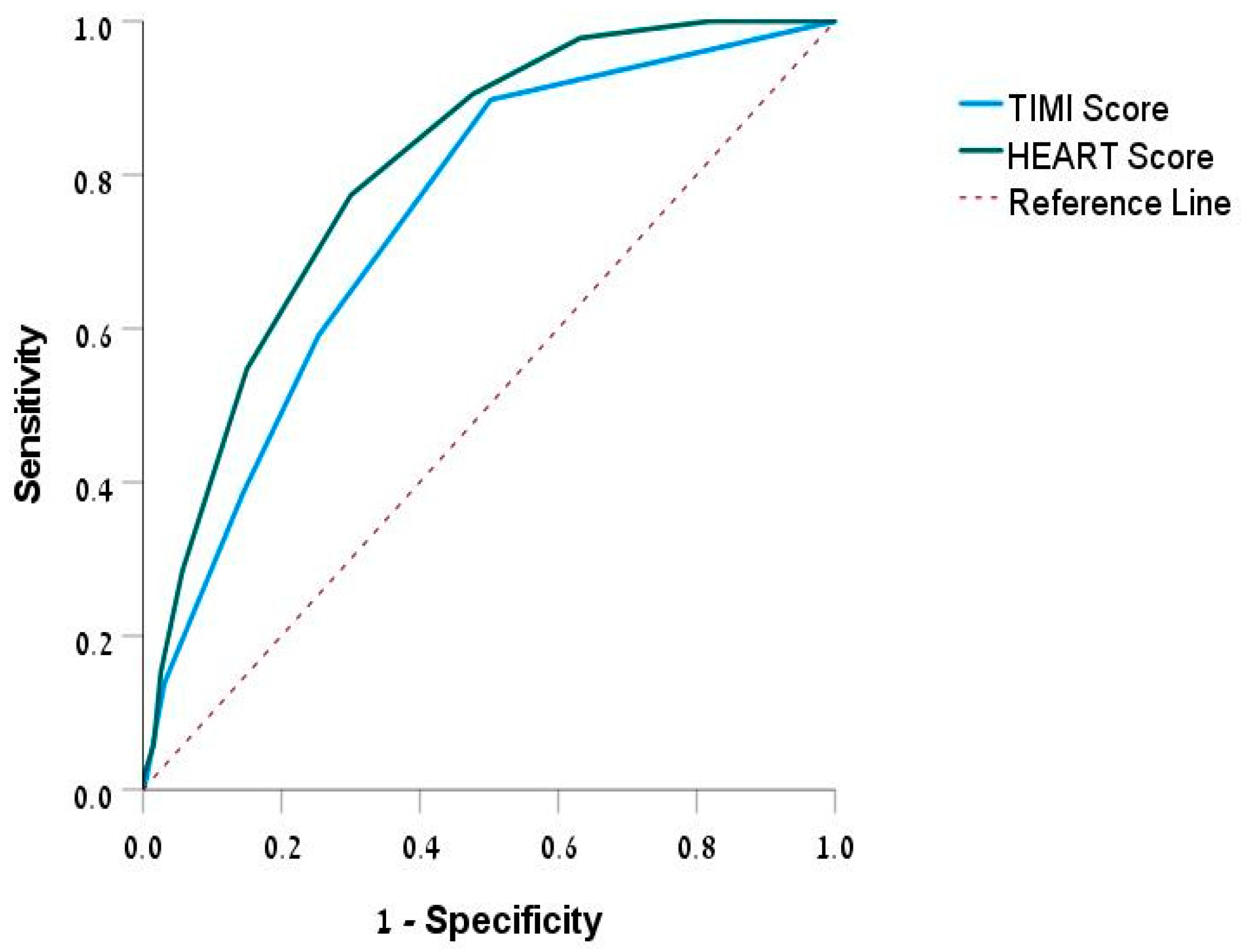
3.4. TIMI and HEART Scores
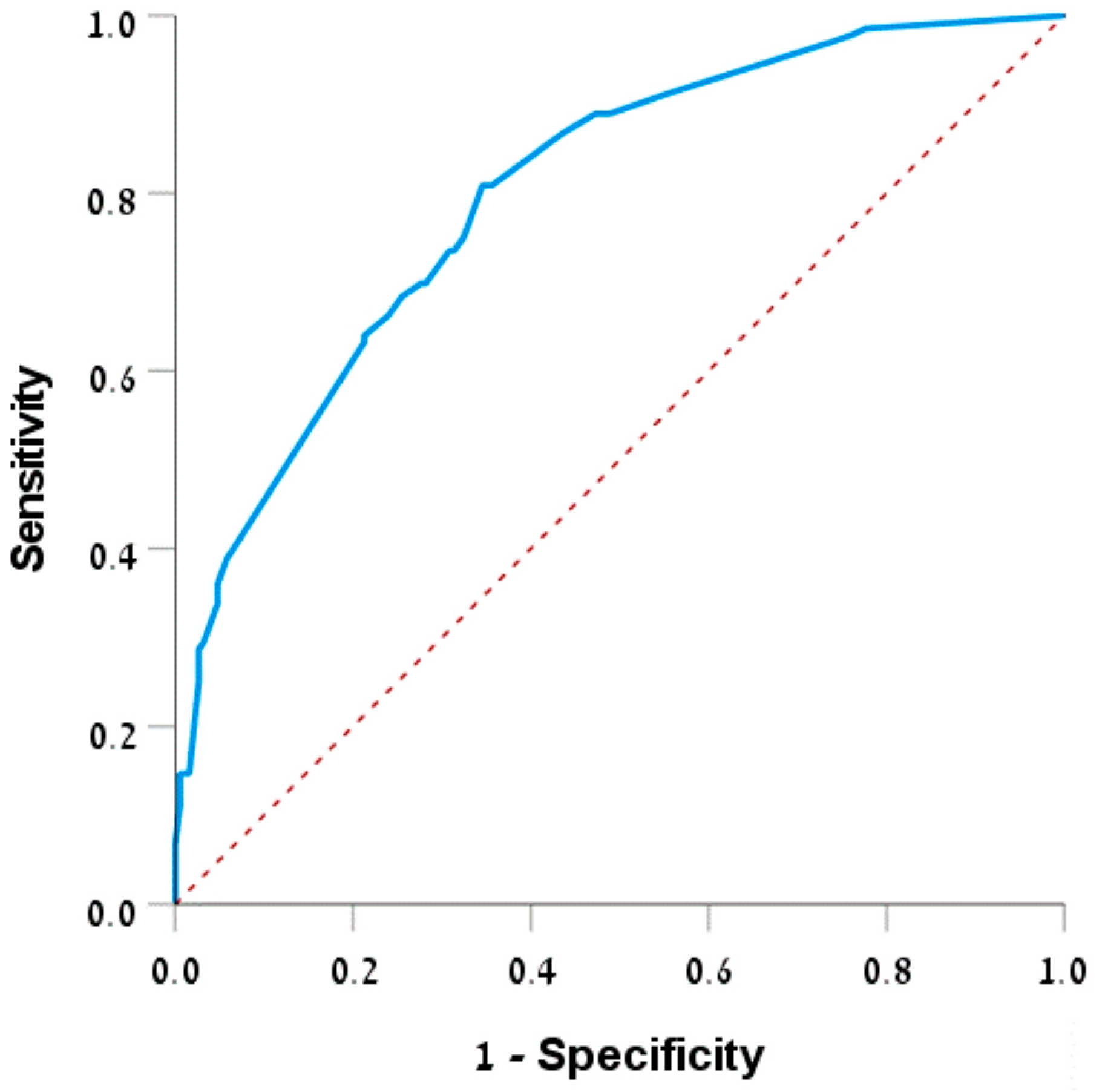
3.5. Factors Associated with Discharge/Hospitalization
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frieling, T. Non-Cardiac Chest Pain. Visc. Med. 2018, 34, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Lenfant, C. Chest Pain of Cardiac and Noncardiac Origin. Metabolism 2010, 59, S41–S46. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Lindsell, C.J.; Hornung, R.W.; Lewis, T.; Storrow, A.B.; Hoekstra, J.W.; Hollander, J.E.; Miller, C.D.; Peacock, W.F.; Pollack, C.V.; et al. The Elder Patient with Suspected Acute Coronary Syndromes in the Emergency Department. Acad. Emerg. Med. 2007, 14, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Kontos, M.C.; Diercks, D.B.; Kirk, J.D. Emergency Department and Office-Based Evaluation of Patients with Chest Pain. Mayo Clin. Proc. 2010, 85, 284–299. [Google Scholar] [CrossRef] [PubMed]
- Gruenberg, C.C.; Breaud, A.H.; Liu, J.H.; Mitchell, P.M.; Feldman, J.A.; Nelson, K.P.; Kahn, J.H. Are Geriatric Patients Placed in an Emergency Department Observation Unit on a Chest Pain Pathway More Likely Than Non-Geriatric Patients to Re-Present to the Hospital within 30 Days? J. Emerg. Med. 2018, 54, 302–306. [Google Scholar] [CrossRef]
- Durazzo, M.; Gargiulo, G.; Pellicano, R. Non-Cardiac Chest Pain: A 2018 Update. Minerva Cardioangiol. 2018, 66, 770–783. [Google Scholar] [CrossRef]
- Eslick, G.D.; Coulshed, D.S.; Talley, N.J. Review Article: The Burden of Illness of Non-Cardiac Chest Pain. Aliment. Pharmacol. Ther. 2002, 16, 1217–1223. [Google Scholar] [CrossRef]
- Jalil, N.A.; Prateepavanich, P.; Chaudakshetrin, P. Atypical Chest Pain from Myofascial Pain Syndrome of Subscapularis Muscle. J. Musculoskelet. Pain 2010, 18, 173–179. [Google Scholar] [CrossRef]
- Six, A.J.; Backus, B.E.; Kelder, J.C. Chest Pain in the Emergency Room: Value of the HEART Score. Neth. Heart J. 2008, 16, 191–196. [Google Scholar] [CrossRef]
- Moons, K.G.M.; de Groot, J.A.H.; Bouwmeester, W.; Vergouwe, Y.; Mallett, S.; Altman, D.G.; Reitsma, J.B.; Collins, G.S. Critical Appraisal and Data Extraction for Systematic Reviews of Prediction Modelling Studies: The CHARMS Checklist. PLoS Med. 2014, 11, e1001744. [Google Scholar] [CrossRef]
- Antman, E.M.; Cohen, M.; Bernink, P.J.L.M.; McCabe, C.H.; Horacek, T.; Papuchis, G.; Mautner, B.; Corbalan, R.; Radley, D.; Braunwald, E. The TIMI Risk Score for Unstable Angina/Non-ST Elevation MI: A Method for Prognostication and Therapeutic Decision Making. J. Am. Med. Assoc. 2000, 284, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.; Guptha, S.; Rajalakshmi, K.V.; Kumaresan, A.P.; Bose, S.; Guptha, S., Sr.; Rajalakshmi, K.V.; Ananthakumar, P. Evaluating Cardiovascular Risks: The Platelet Lymphocyte Ratio and the Neutrophil Lymphocyte Ratio as High-Risk Heart Score Predictors in Non-ST Elevation Myocardial Infarction (NSTEMI) and Unstable Angina Patients. Cureus 2024, 16, 61279. [Google Scholar] [CrossRef] [PubMed]
- Pruc, M.; Kubica, J.; Banach, M.; Swieczkowski, D.; Rafique, Z.; Peacock, W.F.; Siudak, Z.; Kurek, K.; Nanayakkara, P.; Szarpak, Ł. Diagnostic and Prognostic Performance of the Neutrophil-to-Lymphocyte Ratio in Acute Coronary Syndromes: A Meta-Analysis of 90 Studies Including 45,990 Patients. Kardiol. Pol. 2024, 82, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Seaoud, E.; Mohamed, A.A.H.A.; Elkot, M.A. The Role of the Platelet/Lymphocyte Ratio and Neutrophil/Lymphocyte Ratio in Predicting High-Risk Heart Score in Patients Admitted with Non-ST Elevation Acute Coronary Syndrome. Pulse 2020, 8, 66–74. [Google Scholar] [CrossRef]
- George, N.; Abdallah, J.; Maradey-Romero, C.; Gerson, L.; Fass, R. Review Article: The Current Treatment of Non-Cardiac Chest Pain. Aliment. Pharmacol. Ther. 2016, 43, 213–239. [Google Scholar] [CrossRef]
- Fanaroff, A.C.; Rymer, J.A.; Goldstein, S.A.; Simel, D.L.; Newby, L.K. Does This Patient with Chest Pain Have Acute Coronary Syndrome? The Rational Clinical Examination Systematic Review. JAMA J. Am. Med. Assoc. 2015, 314, 1955–1965. [Google Scholar] [CrossRef]
- Castonguay, J.; Turcotte, S.; Fleet, R.P.; Archambault, P.M.; Dionne, C.E.; Denis, I.; Foldes-Busque, G. Physical Activity and Disability in Patients with Noncardiac Chest Pain: A Longitudinal Cohort Study. Biopsychosoc. Med. 2020, 14, 12. [Google Scholar] [CrossRef]
- Stochkendahl, M.J.; Christensen, H.W. Chest Pain in Focal Musculoskeletal Disorders. Med. Clin. N. Am. 2010, 94, 259–273. [Google Scholar] [CrossRef]
- Gupta, R.; Munoz, R. Evaluation and Management of Chest Pain in the Elderly. Emerg. Med. Clin. N. Am. 2016, 34, 523–542. [Google Scholar] [CrossRef]
- Kannel, W.B.; Dawber, T.R.; Kagan, A.; Revotskie, N.; Stokes, J. Factors of Risk in the Development of Coronary Heart Disease--Six Year Follow-up Experience. The Framingham Study. Ann. Intern. Med. 1961, 55, 33–50. [Google Scholar] [CrossRef]
- Martsolf, G.R.; Martsolf, G.R.; Nuckols, T.K.; Nuckols, T.K.; Fingar, K.R.; Barrett, M.L.; Stocks, C.; Stocks, C.; Owens, P.L. Nonspecific Chest Pain and Hospital Revisits within 7 Days of Care: Variation across Emergency Department, Observation and Inpatient Visits. BMC Health Serv. Res. 2020, 20, 516. [Google Scholar] [CrossRef] [PubMed]
- Vrints, C.J.M. Update on the Emergency Department Diagnosis and Risk Stratification of Acute Chest Pain. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Simonetto, C.; Rospleszcz, S.; Kaiser, J.C.; Furukawa, K. Heterogeneity in Coronary Heart Disease Risk. Sci. Rep. 2022, 12, 10131. [Google Scholar] [CrossRef] [PubMed]
- Obermeyer, Z.; Cohn, B.; Wilson, M.; Jena, A.B.; Cutler, D.M. Early Death after Discharge from Emergency Departments: Analysis of National US Insurance Claims Data. BMJ 2017, 356, j239. [Google Scholar] [CrossRef]
- Nagurney, J.M.; Fleischman, W.; Han, L.; Leo-Summers, L.; Allore, H.G.; Gill, T.M. Emergency Department Visits Without Hospitalization Are Associated with Functional Decline in Older Persons. Ann. Emerg. Med. 2017, 69, 426–433. [Google Scholar] [CrossRef]
- Wong, R.Y.; Miller, W.C. Adverse Outcomes Following Hospitalization in Acutely Ill Older Patients. BMC Geriatr. 2008, 8, 10. [Google Scholar] [CrossRef]
- Schattner, A. The Spectrum of Hospitalization-Associated Harm in the Elderly. Eur. J. Intern. Med. 2023, 115, 29–33. [Google Scholar] [CrossRef]
- Templeton, Z.S.; Apathy, N.C.; Konetzka, R.T.; Skira, M.M.; Werner, R.M. The Health Effects of Nursing Home Specialization in Post-Acute Care. J. Health Econ. 2023, 92, 102823. [Google Scholar] [CrossRef]
- O’Keefe-McCarthy, S.; McGillion, M.H.; Victor, J.C.; Jones, J.; McFetridge-Durdle, J. Prodromal Symptoms Associated with Acute Coronary Syndrome Acute Symptom Presentation. Eur. J. Cardiovasc. Nurs. 2016, 15, e52–e59. [Google Scholar] [CrossRef]
- García-Blas, S.; Cordero, A.; Diez-Villanueva, P.; Martinez-Avial, M.; Ayesta, A.; Ariza-Solé, A.; Mateus-Porta, G.; Martínez-Sellés, M.; Escribano, D.; Gabaldon-Perez, A.; et al. Acute Coronary Syndrome in the Older Patient. J. Clin. Med. 2021, 10, 4132. [Google Scholar] [CrossRef]
- Canto, J.G.; Rogers, W.J.; Goldberg, R.J.; Peterson, E.D.; Wenger, N.K.; Vaccarino, V.; Kiefe, C.I.; Frederick, P.D.; Sopko, G.; Zheng, Z.J. Association of Age and Sex with Myocardial Infarction Symptom Presentation and In-Hospital Mortality. JAMA 2012, 307, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Keijzers, G.; Kelly, A.M.; Cullen, L.; Klim, S.; Graham, C.A.; Craig, S.; Kuan, W.S.; Jones, P.; Holdgate, A.; Lawoko, C.; et al. Heart Failure in Patients Presenting with Dyspnoea to the Emergency Department in the Asia Pacific Region: An Observational Study. BMJ Open 2017, 7, e013812. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A. The Clinical Epidemiology of Fatigue in Newly Diagnosed Heart Failure. BMC Cardiovasc. Disord. 2017, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Fass, R.; Achem, S.R. Noncardiac Chest Pain: Epidemiology, Natural Course and Pathogenesis. J. Neurogastroenterol. Motil. 2011, 17, 110. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.; Rosengren, A.; Ekman, I. Symptoms in Acute Coronary Syndromes: Does Sex Make a Difference? Am. Heart J. 2004, 148, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Gorski, J.K.; Batt, R.J.; Otles, E.; Shah, M.N.; Hamedani, A.G.; Patterson, B.W. The Impact of Emergency Department Census on the Decision to Admit. Acad. Emerg. Med. 2017, 24, 13–21. [Google Scholar] [CrossRef]
- Aaronson, E.L.; Aaronson, E.L.; Yun, B.J.; Yun, B.J. Emergency Department Shifts and Decision to Admit: Is There a Lever to Pull to Address Crowding? BMJ Qual. Saf. 2020, 29, 443–445. [Google Scholar] [CrossRef]
- Vermeulen, M.J.; Guttmann, A.; Stukel, T.A.; Kachra, A.; Sivilotti, M.L.A.; Rowe, B.H.; Dreyer, J.; Bell, R.; Schull, M. Are Reductions in Emergency Department Length of Stay Associated with Improvements in Quality of Care? A Difference-in-Differences Analysis. BMJ Qual. Saf. 2016, 25, 489–498. [Google Scholar] [CrossRef]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association between Rotating Night Shiftwork and Risk of Coronary Heart Disease among Women. JAMA J. Am. Med. Assoc. 2016, 315, 1726–1734. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Mensah, G.A.; Turco, J.V.; Fuster, V.; Roth, G.A. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J. Am. Coll. Cardiol. 2022, 80, 2361–2371. [Google Scholar] [CrossRef]
- Khan, R.; Zarak, M.S.; Munir, U.; Ahmed, K.; Ullah, A. Thrombolysis in Myocardial Infarction (TIMI) Risk Score Assessment for Complications in Acute Anterior Wall ST Elevation Myocardial Infarction. Cureus 2020, 12, e8646. [Google Scholar] [CrossRef] [PubMed]
- Mahler, S.A.; Riley, R.F.; Hiestand, B.C.; Russell, G.B.; Hoekstra, J.W.; Lefebvre, C.W.; Nicks, B.A.; Cline, D.M.; Askew, K.L.; Elliott, S.B.; et al. The HEART Pathway Randomized Trial: Identifying Emergency Department Patients with Acute Chest Pain for Early Discharge. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Backus, B.E.; Six, A.J.; Kelder, J.C.; Bosschaert, M.A.R.; Mast, E.G.; Mosterd, A.; Veldkamp, R.F.; Wardeh, A.J.; Tio, R.; Braam, R.; et al. A Prospective Validation of the HEART Score for Chest Pain Patients at the Emergency Department. Int. J. Cardiol. 2013, 168, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Poldervaart, J.M.; Langedijk, M.; Backus, B.E.; Dekker, I.M.C.; Six, A.J.; Doevendans, P.A.; Hoes, A.W.; Reitsma, J.B. Comparison of the GRACE, HEART and TIMI Score to Predict Major Adverse Cardiac Events in Chest Pain Patients at the Emergency Department. Int. J. Cardiol. 2017, 227, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Reaney, P.D.W.; Elliott, H.I.; Noman, A.; Cooper, J.G. Risk Stratifying Chest Pain Patients in the Emergency Department Using HEART, GRACE and TIMI Scores, with a Single Contemporary Troponin Result, to Predict Major Adverse Cardiac Events. Emerg. Med. J. 2018, 35, 420–427. [Google Scholar] [CrossRef]
- Jentzer, J.C.; Lawler, P.R.; Van Houten, H.K.; Yao, X.; Kashani, K.B.; Dunlay, S.M. Cardiovascular Events Among Survivors of Sepsis Hospitalization: A Retrospective Cohort Analysis. J. Am. Heart Assoc. 2023, 12, e027813. [Google Scholar] [CrossRef]
- Björklund, J.; Pettersson, L.; Agvall, B. Factors Affecting Hospitalization and Mortality in a Retrospective Study of Elderly Patients with Heart Failure. BMC Cardiovasc. Disord. 2024, 24, 227. [Google Scholar] [CrossRef]
| Total | Discharged | Hospitalized | ||||||
|---|---|---|---|---|---|---|---|---|
| 330 | (%) | 193 | 58.5% | 137 | 41.5% | P | ||
| Gender | Men | 190 | 57.6% | 117 | 60.6% | 73 | 53.3% | 0.184 |
| Women | 140 | 42.4% | 76 | 39.4% | 64 | 46.7% | ||
| Marital status | married | 236 | 71.7% | 138 | 71.5% | 98 | 72.1% | 0.007 |
| widowed | 29 | 8.8% | 13 | 6.7% | 16 | 11.8% | ||
| single | 37 | 11.2% | 30 | 15.5% | 7 | 5.1% | ||
| divorced | 27 | 8.2% | 12 | 6.2% | 15 | 11% | ||
| Age group | Below 65 | 145 | 43.9% | 112 | 58% | 33 | 24.1% | <0.001 |
| Age 65–74 | 112 | 33.9% | 51 | 26.4% | 61 | 44.5% | ||
| Age 75–84 | 53 | 16.1% | 21 | 10.9% | 32 | 23.4% | ||
| Age 85+ | 20 | 6.1% | 9 | 4.7% | 11 | 8% | ||
| Age (IQR) | 66 | 46–73 | 57 | 38.5–70.5 | 70 | 65–76.5 | <0.001 | |
| Primary residence | Home | 227 | 68.8% | 113 | 58.5% | 114 | 83.2% | <0.001 |
| Nursing home | 103 | 31.2% | 80 | 41.5% | 23 | 16.8% | ||
| Basic physical function | dependent | 16 | 4.8% | 6 | 3.1% | 10 | 7.3% | 0.081 |
| independent | 314 | 95.2% | 187 | 96.9% | 127 | 92.7% | ||
| Basic cognitive function | preserved | 326 | 98.8% | 191 | 99% | 135 | 98.5% | >0.999 |
| Basic physical function | dependent | 16 | 4.8% | 6 | 3.1% | 10 | 7.3% | 0.081 |
| IHD | 99 | 30% | 45 | 23.3% | 54 | 39.4% | 0.002 | |
| CRF | 20 | 6.1% | 5 | 2.6% | 15 | 10.9% | 0.002 | |
| Past MI | 72 | 21.8% | 30 | 15.5% | 42 | 30.7% | 0.001 | |
| Catheterization background | 88 | 26.7% | 37 | 19.2% | 51 | 37.2% | <0.001 | |
| s/p CVA_TIA | 17 | 5.2% | 4 | 2.1% | 13 | 9.5% | 0.003 | |
| Arrhythmia | 50 | 15.2% | 21 | 10.9% | 29 | 21.2% | 0.01 | |
| Hyperlipidemia | 149 | 45.2% | 56 | 29% | 93 | 67.9% | <0.001 | |
| Hypertension | 170 | 51.5% | 73 | 37.8% | 97 | 70.8% | <0.001 | |
| Diabetes | 104 | 31.5% | 45 | 23.3% | 59 | 43.1% | <0.001 | |
| Polypharmacy | 126 | 38.3% | 48 | 24.9% | 78 | 57.4% | <0.001 | |
| Total | Discharge | Hospitalization | ||||||
|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | P | ||
| Level of consciousness | Full consciousness | 329 | 99.7% | 193 | 100% | 136 | 99.3% | 0.415 |
| Moderately reduced | 1 | 0.3% | 0 | 0% | 1 | 0.7% | ||
| Condition at admission | Stable | 328 | 99.4% | 193 | 100% | 135 | 98.5% | 0.172 |
| Fatigue | 57 | 17.5% | 24 | 12.7% | 33 | 24.3% | 0.007 | |
| Dizziness | 19 | 5.8% | 9 | 4.8% | 10 | 7.4% | 0.326 | |
| Diaphoresis | 24 | 7.4% | 4 | 2.1% | 20 | 14.7% | <0.001 | |
| Confusion | 1 | 0.3% | 1 | 0.5% | 0 | 0% | >0.999 | |
| Palpitations | 31 | 9.5% | 14 | 7.4% | 17 | 12.5% | 0.123 | |
| Dyspnea | 77 | 23.8% | 29 | 15.4% | 48 | 35.3% | <0.001 | |
| Nausea | 28 | 8.6% | 15 | 7.9% | 13 | 9.6% | 0.607 | |
| Pain duration | No data | 97 | 29.7% | 73 | 38.4% | 24 | 17.5% | <0.001 |
| Hours before admission | 120 | 36.7% | 67 | 35.3% | 53 | 38.7% | ||
| Days before admission | 85 | 26% | 38 | 20% | 47 | 34.3% | ||
| Fluctuating during period | 23 | 7% | 11 | 5.8% | 12 | 8.8% | ||
| Radiating pain | 81 | 27.4% | 39 | 21.5% | 42 | 36.5% | 0.005 | |
| Epigastric pain | 40 | 12.3% | 28 | 14.8% | 12 | 8.8% | 0.105 | |
| Chest pain | 313 | 94.8% | 176 | 91.2% | 137 | 100% | <0.001 | |
| ECG changes | Without ischemic changes | 229 | 75.1% | 142 | 81.1% | 87 | 66.9% | <0.001 |
| With ischemic changes | 20 | 6.6% | 2 | 1.1% | 18 | 13.8% | ||
| Non-specific changes | 20 | 6.6% | 12 | 6.9% | 8 | 6.2% | ||
| Other dysrhythmias without ischemic changes | 36 | 11.8% | 19 | 10.9% | 17 | 13.1% | ||
| Total | Discharge | Hospitalization | P | |||||
|---|---|---|---|---|---|---|---|---|
| Total blood test | 320 | 97.9% | 184 | 96.8% | 136 | 99.3% | 0.246 | |
| WBC (IQR) | 1000/µL | 8.1 | 6.45–9.7 | 8.3 | 6.475–9.625 | 8 | 6.4–9.9 | 0.652 |
| HB (IQR) | g/dL | 13.6 | 12.575–14.7 | 13.9 | 12.9–14.925 | 13.4 | 11.925–14.2 | <0.001 |
| Na (IQR) | mmol/L | 138 | 137–140 | 138 | 137–140 | 138 | 137–140 | 0.170 |
| K (IQR) | mmol/L | 4.1 | 3.9–4.4 | 4.1 | 3.8–4.3 | 4.2 | 3.9–4.6 | 0.004 |
| CPK (IQR) | U/L | 92 | 62–148.50 | 95 | 66–149 | 86 | 56.50–148.50 | 0.282 |
| D Dimer (IQR | ng/mL | 710 | 229.50–1632.50 | 229.50 | 157–1295.75 | 1362 | 503.50–4151 | 0.190 |
| CRE (IQR) | mg/dL | 0.86 | 0.73–0.99 | 0.86 | 0.71–0.96 | 0.865 | 0.74–1.025 | 0.114 |
| eGFR (mean ± sd) | mL/min/1.73 m2 | 82.353 + 27.263 | 86.907 + 24.825 | 76.389 + 29.199 | 0.001 | |||
| CRP (IQR) | mg/L | 3.44 | 1.32–9.93 | 3.125 | 1.21–6.232 | 6.17 | 1.77–23 | 0.003 |
| Troponin (IQR | ng/L | 0.013 | 0.013–0.02 | 0.013 | 0.013–0.013 | 0.013 | 0.013–0.03 | <0.001 |
| Saturation (IQR) | % | 98 | 97–99 | 98 | 97–100 | 98 | 96–99 | 0.033 |
| Total | Discharge | Hospitalization | ||||||
|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | P | ||
| ED diagnosis classification | Abdominal cause | 19 | 5.8% | 16 | 8.3% | 3 | 2.2% | <0.001 |
| ACS | 18 | 5.5% | 1 | 0.5% | 17 | 12.4% | ||
| Respiratory | 12 | 3.6% | 5 | 2.6% | 7 | 5.1% | ||
| Trauma | 14 | 4.2% | 11 | 5.7% | 3 | 2.2% | ||
| Arrhythmia | 11 | 3.3% | 6 | 3.1% | 5 | 3.6% | ||
| Chest pain | 224 | 67.9% | 134 | 69.4% | 90 | 65.7% | ||
| Other | 32 | 9.7% | 20 | 10.4% | 12 | 8.8% | ||
| Time in minutes from reception to triage (IQR) | 9 | 3–20.50 | 14.50 | 4.25–24.75 | 6 | 2–16.5 | <0.001 | |
| Time in minutes from reception to first MD (IQR) | 65.50 | 41–115 | 82.50 | 47–133.75 | 54 | 37–88 | <0.001 | |
| Time in minutes from reception to decision (IQR) | 234 | 172–318 | 224.50 | 161–317.25 | 241 | 183–321.50 | 0.159 | |
| Time in minutes from decision to hospitalization (IQR) | 41 | 6.50–73.50 | NA | NA | 41 | 6.50–73.50 | NA | |
| Opiates | 6 | 1.8% | 1 | 0.5% | 5 | 3.6% | 0.086 | |
| Oxygen treatment | 5 | 1.5% | 0 | 0% | 5 | 3.6% | 0.012 | |
| Fluid infusion | 16 | 4.9% | 5 | 2.6% | 11 | 8% | 0.026 | |
| ED cardiologist consultant | 43 | 13.1% | 7 | 3.7% | 36 | 26.3% | <0.001 | |
| Nurse shift | 23:00–7:00 | 178 | 53.9% | 93 | 48.2% | 85 | 62% | 0.042 |
| 15:00–23:00 | 108 | 32.7% | 70 | 36.3% | 38 | 27.7% | ||
| 07:00–15:00 | 44 | 13.3% | 30 | 15.5% | 14 | 10.2% | ||
| Weekdays | First day of the week | 50 | 15.2% | 28 | 14.5% | 22 | 16.1% | 0.571 |
| Weekdays | 203 | 61.5% | 116 | 60.1% | 87 | 63.5% | ||
| Weekend | 77 | 23.3% | 49 | 25.4% | 28 | 20.4% | ||
| Total | Discharge n = 193 | Hospitalization n = 137 | |||||
|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | P | |
| TIMI Score 0 | 110 | 33.3% | 96 | 49.7% | 14 | 10.2% | <0.001 |
| 1–3 | 195 | 59.1% | 91 | 47.2% | 104 | 75.9% | |
| 4+ | 25 | 7.6% | 6 | 3.1% | 19 | 13.9% | |
| HEART Score ≤3 | 166 | 50.3% | 135 | 69.9% | 31 | 22.6% | <0.001 |
| 4–6 | 138 | 41.8% | 53 | 27.5% | 85 | 62% | |
| 7+ | 26 | 7.9% | 5 | 2.6% | 21 | 15.3% | |
| Risk Factors for Hospitalization | OR (95%CI) | P |
|---|---|---|
| Primary residence nursing home | 0.387 (0.198–0.759) | 0.006 |
| Nurse shift 23:00–07:00 | 0.047 | |
| 15:00–23:00 | 0.494 (0.259–0.942) | 0.032 |
| 07:00–15:00 | 0.440 (0.174–1.115) | 0.083 |
| s/p CVA TIA | 3.188 (0.844–12.039) | 0.087 |
| Hyperlipidemia | 3.514 (1.968–6.275) | <0.001 |
| ECG changes without ischemic changes | 0.027 | |
| with ischemic changes | 7.992 (1.555–41.073) | 0.013 |
| Dysrhythmias without ischemic changes | 0.679 (0.274–1.686) | 0.405 |
| Diaphoresis | 7.043 (1.939–25.581) | 0.003 |
| Dyspnea | 3.641 (1.828–7.252) | <0.001 |
| Troponin TIMI | 3.820 (1.245–11.715) | 0.019 |
| Risk Factors for Hospitalization | OR (95%CI) | P |
|---|---|---|
| Primary residence—nursing home | 0.381 (0.201–0.722) | 0.003 |
| Hyperlipemia | 3.246 (1.794–5.876) | <0.001 |
| Hypertension | 1.959 (1.055–3.640) | 0.033 |
| Fatigue | 1.885 (0.953–3.730) | 0.069 |
| Diaphoresis | 8.525 (2.562–28.364) | <0.001 |
| Dyspnea | 2.897 (1.538–5.455) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kagansky, N.; Mazor, D.; Wajdi, A.; Maler Yaron, Y.; Sharfman, M.; Ziv Baran, T.; Kagansky, D.; Pachys, G.; Levy, Y.; Trotzky, D. Predictive Factors and Risk Assessment for Hospitalization in Chest Pain Patients Admitted to the Emergency Department. Diagnostics 2024, 14, 2733. https://doi.org/10.3390/diagnostics14232733
Kagansky N, Mazor D, Wajdi A, Maler Yaron Y, Sharfman M, Ziv Baran T, Kagansky D, Pachys G, Levy Y, Trotzky D. Predictive Factors and Risk Assessment for Hospitalization in Chest Pain Patients Admitted to the Emergency Department. Diagnostics. 2024; 14(23):2733. https://doi.org/10.3390/diagnostics14232733
Chicago/Turabian StyleKagansky, Nadya, David Mazor, Ayashi Wajdi, Yulia Maler Yaron, Miya Sharfman, Tomer Ziv Baran, Dana Kagansky, Gal Pachys, Yochai Levy, and Daniel Trotzky. 2024. "Predictive Factors and Risk Assessment for Hospitalization in Chest Pain Patients Admitted to the Emergency Department" Diagnostics 14, no. 23: 2733. https://doi.org/10.3390/diagnostics14232733
APA StyleKagansky, N., Mazor, D., Wajdi, A., Maler Yaron, Y., Sharfman, M., Ziv Baran, T., Kagansky, D., Pachys, G., Levy, Y., & Trotzky, D. (2024). Predictive Factors and Risk Assessment for Hospitalization in Chest Pain Patients Admitted to the Emergency Department. Diagnostics, 14(23), 2733. https://doi.org/10.3390/diagnostics14232733






