Abstract
Skeletal Class III malocclusion is one type of dentofacial deformity that significantly affects patients’ facial aesthetics and oral health. The orthodontic treatment of skeletal Class III malocclusion presents challenges due to uncertainties surrounding mandibular growth patterns and treatment outcomes. In recent years, disease-specific radiographic features have garnered interest from researchers in various fields including orthodontics, for their exceptional performance in enhancing diagnostic precision and treatment effect predictability. The aim of this narrative review is to provide an overview of the valuable radiographic features in the diagnosis and management of skeletal Class III malocclusion. Based on the existing literature, a series of analyses on lateral cephalograms have been concluded to identify the significant variables related to facial type classification, growth prediction, and decision-making for tooth extractions and orthognathic surgery in patients with skeletal Class III malocclusion. Furthermore, we summarize the parameters regarding the inter-maxillary relationship, as well as different anatomical structures including the maxilla, mandible, craniofacial base, and soft tissues from conventional and machine learning statistical models. Several distinct radiographic features for Class III malocclusion have also been preliminarily observed using cone beam computed tomography (CBCT) and magnetic resonance imaging (MRI).
1. Introduction
As one type of malocclusion classified by Edward H. Angle, Class III malocclusion is a sagittal positional discrepancy that is characterized by a mesial molar relationship [1]. It was reported to affect over 7% of the global population and the prevalence is even higher in Southeast Asians, ranging from 12.58% to 26.67% [2]. Notably, the majority of Class III malocclusion cases display skeletal discrepancies to varying degrees. Skeletal Class III malocclusion patients exhibit a concave facial type due to maxillary retrusion and/or mandibular prognathism, suffering from the negative impact on their oral health, facial aesthetics, psychosocial well-being, and oral health-related quality of life [3,4,5]. When addressing skeletal Class III malocclusion, various treatment strategies are available, including early orthopedic treatment during growth, camouflage orthodontic treatment, and orthognathic surgery after growth completion [6,7]. However, choosing the appropriate treatment and determining the intervention timing can be challenging, especially for less-experienced orthodontists. The difficulties in treating skeletal Class III malocclusion stem from variations in mandibular growth patterns, diverse treatment options, a high risk of relapse, and irreversible changes following orthodontic extractions [8]. Generally, orthodontists make subjective decisions on the treatment of skeletal Class III malocclusion, relying on their prior training or experience, which may lead to a potential impact on the accuracy of treatment selection.
Radiographic imaging, such as cephalograms, cone beam computed tomography (CBCT) and magnetic resonance imaging (MRI), is a non-invasive examination that provides visual representations of dentoskeletal characteristics in orthodontics. There exist numerous radiographic features that could potentially aid in decision-making for skeletal Class III cases in clinical practice. Previous studies have focused on developing various analytic models to generalize these disease-specific radiographic features. Early in the 1970s, Schulhof et al. built a simple formula based on the measurements in lateral cephalograms, for the first time, to predict the facial growth of skeletal Class III malocclusion patients [9]. Later, significant indicators for the diagnosis and treatment of Class III malocclusion were identified by conventional statistical models, including cluster analysis, discriminant analysis, and regression analysis [10,11,12]. In the 1980s, Stensland et al. identified certain predictors for the relapse of Class III malocclusion in children after combined retractor and chin-cup therapy using discriminant analysis [11]. Nevertheless, although plenty of indicators for the diagnosis and treatment of Class III malocclusion have been investigated through conventional models, it is still hard to find them with consensus and satisfactory accuracy [13].
In the past few years, artificial intelligence (AI) technology, including machine learning (ML) algorithms, has witnessed a rapid advancement in identifying valuable radiographic features based on the measurement input. Thanks to its capacity to process enormous amounts of data through high-dimensional analytical methods, AI technology has been dramatically applied in orthodontic diagnosis, such as cephalometric analysis and skeletal-maturation-stage determination, treatment planning, such as treatment outcome prediction, as well as clinical practice, such as remote care [14]. Specifically, ML has been used for the diagnosis and treatment of Class III malocclusion to improve prediction accuracy, which is expected to aid in the diagnosis and treatment planning of Class III malocclusion cases, especially for non-specialists [8]. In 2009, Kim et al. compared the prediction accuracy between the ML algorithm and traditional discriminant analysis for the prediction of Class III malocclusion treatment outcomes among children, where the authors found that the ML analysis might be an effective alternative to the conventional model for prognosis prediction [13]. With increasing attention given to the value of medical images themselves, the requirement for quantitative imaging analysis gave rise to radiomics in 2012 [15]. Radiomics is an approach enabling the extraction of a large number of quantitative features in medical images and providing a detailed characterization of the underlying tissue properties [15]. It has been explored in the automatic diagnosis and prognosis prediction of maxillofacial diseases, particularly in detecting head and neck tumors [16,17].
Based on various analytic models, numerous radiographic features have been identified for skeletal Class III malocclusion. Staying updated on the latest findings regarding these radiographic features is essential for clinicians to make informed decisions in diagnosing and treating patients, and for researchers working on developing robust prediction models to enhance the understanding and management of skeletal Class III malocclusion. In a previous study, Piotr Fudalej et al. conducted a review of significant predictors for early orthodontic or orthopedic treatment outcomes in children with Class III malocclusion [18]. However, this review did not address radiographic parameters for all patients with skeletal Class III malocclusion, especially those requiring orthognathic surgery. Additionally, the analysis using advanced technologies such as ML has not been examined and updated. Therefore, the aim of this narrative review is to provide a comprehensive summary of radiographic features associated with patients with skeletal Class III malocclusion in the application of facial type classification, growth prediction, and decision-making for tooth extractions and orthognathic surgery. This review outlines radiographic features from both conventional statistical models and ML algorithms across multiple domains, encompassing inter-maxillary relationships and different anatomical structures. Furthermore, the review discusses the potential future application of radiographic features in diagnosing and treating skeletal Class III malocclusion.
2. Radiographic Features for Inter-Maxillary Relationship in the Diagnosis and Treatment of Skeletal Class III Malocclusion
Since the jaw’s development follows a specific spatiotemporal pattern, peaking in the transverse, sagittal, and vertical dimensions in sequence, we show the parameters in radiographic images involving inter-maxillary relationship by dimensions (Table 1 and Figure 1) [19].

Table 1.
Studies evaluating the association of inter-maxillary relationship with radiographic features on cephalograms using conventional statistical methods or machine learning approaches.
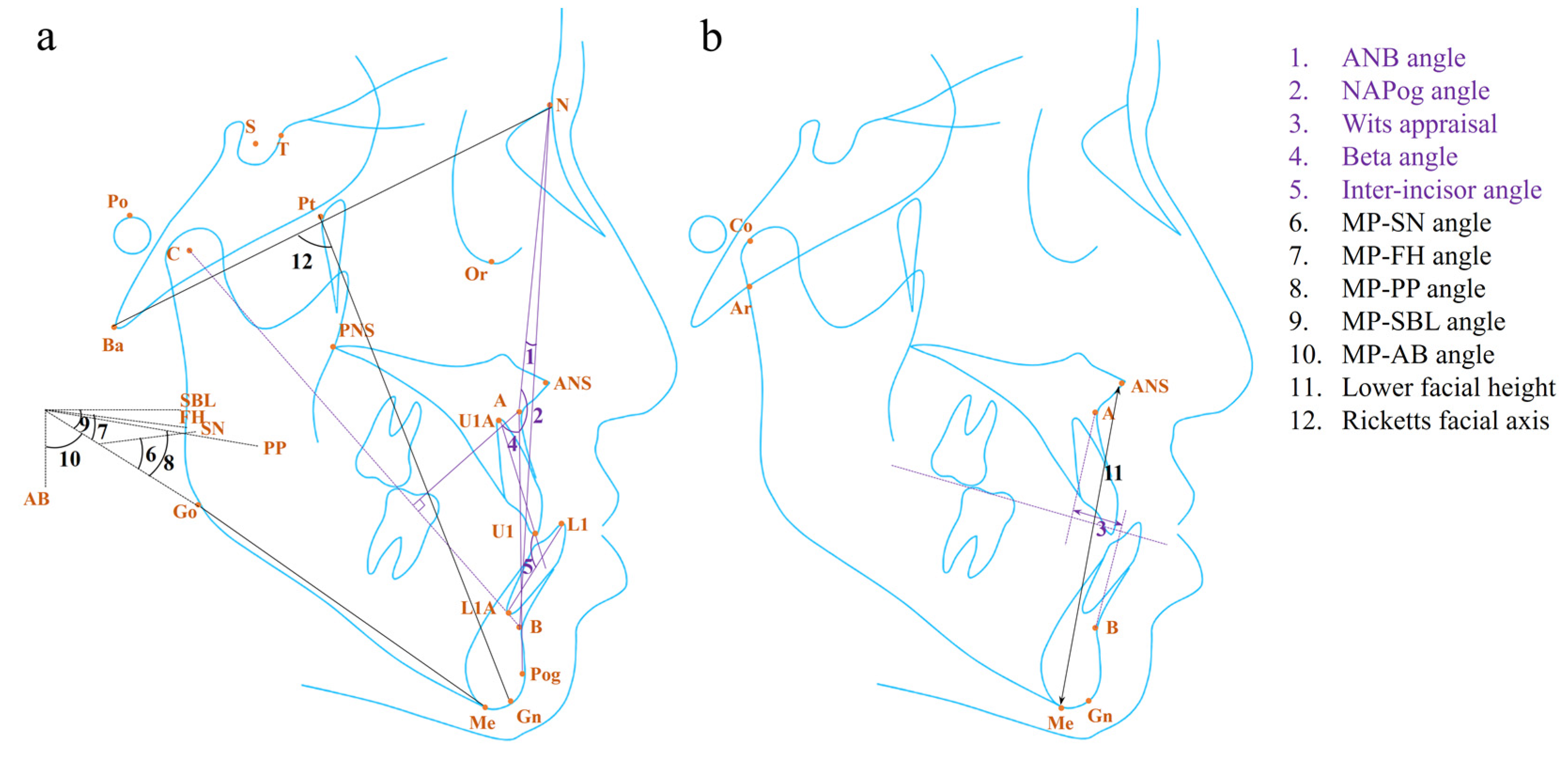
Figure 1.
The (a) angular, (b) linear, and proportional measurements related to the sagittal (purple) and vertical (black) inter-maxillary relationship for diagnosis and treatment of skeletal Class III malocclusion in the existing literature. For the proportional values, only the involved landmark was labeled. The detailed information for the landmark, plane, and measurement is listed in Table S1.
2.1. Radiographic Features for Sagittal Inter-Maxillary Relationship
Patients with skeletal Class III malocclusion are mainly characterized by the concave facial type in the sagittal dimension. The parameters identified in this dimension, including the ANB angle, Wits appraisal, beta angle, jaw length ratio, and inter-incisor angle, hold great significance in the precise diagnosis of and treatment plan-making for Class III malocclusion.
As one of the most widely used means for evaluating the antero–posterior relationship of the jaws, the ANB angle, introduced by Riedel in 1952, was sometimes used to define the skeletal Class III malocclusion (Figure 1a) [40]. It was reported as one of the best predictors of relapse after treatment for Class III malocclusion in children, as well as facial type classification among children and adults [20,21,24]. In addition, it was one of the components that explained the variance of the mandibular prognathic subtype and the borderline Class III subtype [12]. Instead of the ANB angle, some researchers identified the NAPog angle as the predictor for the relapse of Class III malocclusion in children, where there was a higher risk of relapse in patients with a larger NAPog angle (Figure 1a) [22]. It suggested that the ANB angle might not be a perfect parameter without considering the chin protrusion.
Without the disturbance by the displacement of nasion, the Wits appraisal could be the most decisive parameter in the sagittal dimension for Class III malocclusion as it was identified most often from various studies (Figure 1b) [8,12,27,29,30,32,33,34,35]. In the past, Chi et al. recognized the Wits appraisal as one of the principal components that explained the variance of the borderline Class III subtype [12]. In those cases, the Wits appraisal may work together with the ANB angle as they belong to different reference systems and need to be considered at the same time. For growing patients with skeletal Class III malocclusion, a smaller Wits appraisal was later identified as a negative predictor for the long-term success of treatment for Class III malocclusion, including face mask, chin-cup, headgear, and fixed appliance therapy [24,25,27,28]. However, the critical value of the Wits appraisal for orthopedic treatment outcome prediction remained unclear, due to the limitation of statistical models. Most conventional models proposed in the literature provided total critical scores calculated from the statistical formulas, rather than individual critical scores for each significant variable, considering that it was the collective effect of the variables that helped with diagnosis or prediction. In addition, the Wits appraisal was of value in terms of decision-making for tooth extraction and surgery. Recently, a ML model revealed a positive relationship between the Wits appraisal and the likelihood of the need for orthodontic extractions in patients with different types of malocclusions [29]. Notably, the result needs to be interpreted with caution as it could be affected by the study sample which included patients with Class Ⅱ malocclusion. For patients who have completed the growth stage, the Wits appraisal is a useful parameter for determining the need for orthognathic surgery through the discriminant analysis and t-test [30,31,32,33]. Among them, Sara et al. proposed that the cut-off value of the Wits appraisal is −5.8 mm, which should be taken into consideration together with the Holdaway angle when making a treatment plan [33]. Moreover, various ML models built in the previous studies identified the Wits appraisal as a critical parameter contributing to the determination of the need for Class III surgery, further verifying its significance [8,34,35].
Introduced by Chong et al. in 2004, the beta angle was a new measurement for assessing the skeletal discrepancy that combined three skeletal landmarks—point A, point B, and the center of the condyle (C) (Figure 1a) [41]. It was reported as the top contributor for treatment plan prediction, including the orthodontic extraction pattern in skeletal Class Ⅰ patients, as well as growth modulation, camouflage orthodontic treatment, and orthognathic surgery in skeletal Class Ⅱ and Class III patients of different ages based on ML algorithms [34]. However, the information on how the beta angle contributed to the orthodontic treatment plan prediction was not provided in this study.
Besides the linear and angular parameters mentioned above, the proportion of the length of the maxilla and mandible was another predictor in the sagittal dimension. It was one of the contributors that explained the variance of the Class III subtype with maxillary deficiency and a long face, while the authors did not show specific measurements to assess the dimension [12]. In terms of treatment stability prediction, a larger ratio of Co-A to Co-Gn can help to predict better stability in the occlusal correction with a threshold of 0.74 in adolescents receiving conventional orthodontic treatment by means of removable and fixed appliances (Figure 1b) [23]. The comparative parameter related to the difference between individual jaw lengths and normal values also played a role [23]. In addition, a dynamic ratio called the Growth Treatment Response Vector (GTRV) that describes the change in the sagittal position of points A and B during a period can help predict the stability of treatment outcomes in children, where patients with a GTRV ratio below 0.38 should be warned of potential worsening discrepancies [26]. As for treatment plan-making, the smaller proportion of the maxillary and mandibular length is an indicator of surgery need in adult patients through the discriminant analysis [30,31]. Further, the ratio of A-Ar to Gn-Ar was identified as the predictor for orthognathic surgical need through the ML model (Figure 1b) [8]. However, the ratio might be affected by the direction and the spatiotemporal difference in jaw growth.
In addition to the skeletal variables, the dental parameters, such as the inter-incisor angle, explained the variance of the same severe Class III facial subtype, similar to the jaw length ratio, since they depend on the compensatory inclination of the incisors in serious skeletal Class III malocclusion cases (Figure 1a) [12]. According to the discriminant analysis, the inter-incisor angle was a predictor for relapse in Class III children after receiving both retractor and chin-cup therapy, where those with a larger angle tended to relapse after the treatment [11]. For adult patients, a larger angle meant a greater likelihood of orthognathic surgery need [32]. However, no threshold value was provided in the above studies.
2.2. Radiographic Features for Vertical Inter-Maxillary Relationship
During the later stage of the growth peak, the mandibular growth witnesses a profound growth in the vertical dimension, especially in some patients with severe Class III malocclusion. Here, we summarize the parameters in the vertical dimension, including the measurements based on the mandibular plane, facial height, and Ricketts facial axis.
The vertical measurement is indivisible with a core plane, namely, the mandibular plane (MP). The angles which are formed by MP and the SN plane or the Frankfort horizontal (FH) plane have been identified as the parameters for the classification of a vertical facial type in Class III patients using the conventional method and the ML model (Figure 1a) [12,21]. In terms of Class III malocclusion treatment, the research found a larger angle formed by MP and the palatal plane (PP) or the stable basicranial line (SBL) was a negative predictor for the relapse of Class III malocclusion among children receiving early functional treatment, and for the orthognathic surgery need among adults, which could eliminate the interference from the variation of the SN and FH plane (Figure 1a) [8,36,37]. In other studies, it was the MP-AB angle that helped predict the treatment outcome in adolescents under orthopedic treatment, where a smaller MP-AB angle hinted at a greater likelihood of Class III malocclusion relapse (Figure 1a) [13,27,38]. This could be explained by the advantage of the MP-AB angle in reflecting the discrepancy both in the sagittal and vertical dimensions without being affected by any reference planes.
The facial height in the upper and lower parts, anterior and posterior parts can directly describe diverse vertical facial types. Bui et al. identified facial height as the parameter that explained the variance of the vertical facial subtype of skeletal Class III patients [12]. Besides, Yoshida et al. concluded that a longer distance of ANS-Me, which described a lower facial height (LFH), could help predict the tendency of relapse among children under maxillary protraction and chin-cup therapy (Figure 1b) [39]. However, it should be noted that the facial height in different parts needs to be considered together as its coordination affects facial aesthetics.
The Ricketts facial axis was defined as the NBa-PtGn angle (Figure 1a) [42]. It was one of the predictors supporting decision-making for orthodontic extraction in patients with different kinds of malocclusion according to the ML model [29]. The study found patients with a smaller angle were prone to receive orthodontic extraction treatment [29]. It should be noted that the study sample included patients with different types of malocclusion, which may influence the precise predictability of this angle for determining the orthodontic extraction pattern, specifically in Class III malocclusion patients.
3. Radiographic Features of Different Anatomical Structures in the Diagnosis and Treatment of Skeletal Class III Malocclusion
The parameters in different anatomical structures have their own specific patterns. We summarized the parameters for diagnosing and managing skeletal Class III malocclusion in the maxilla, mandible, cranial base, and soft tissue in Table 2 and Table 3 and Figure 2 and Figure 3.

Table 2.
Studies evaluating the association of maxilla and mandible with radiographic features on cephalograms using conventional statistical methods or machine learning approaches.

Table 3.
Studies evaluating the association of cranial base and soft tissue with radiographic features on cephalograms using conventional statistical methods or machine learning approaches.
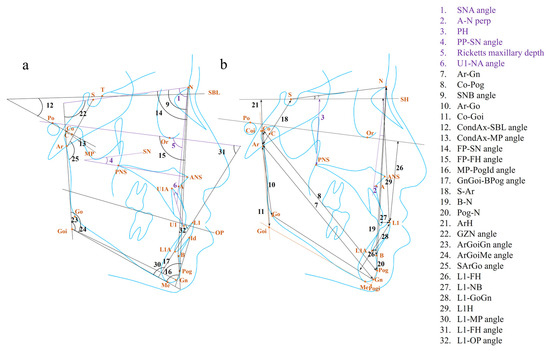
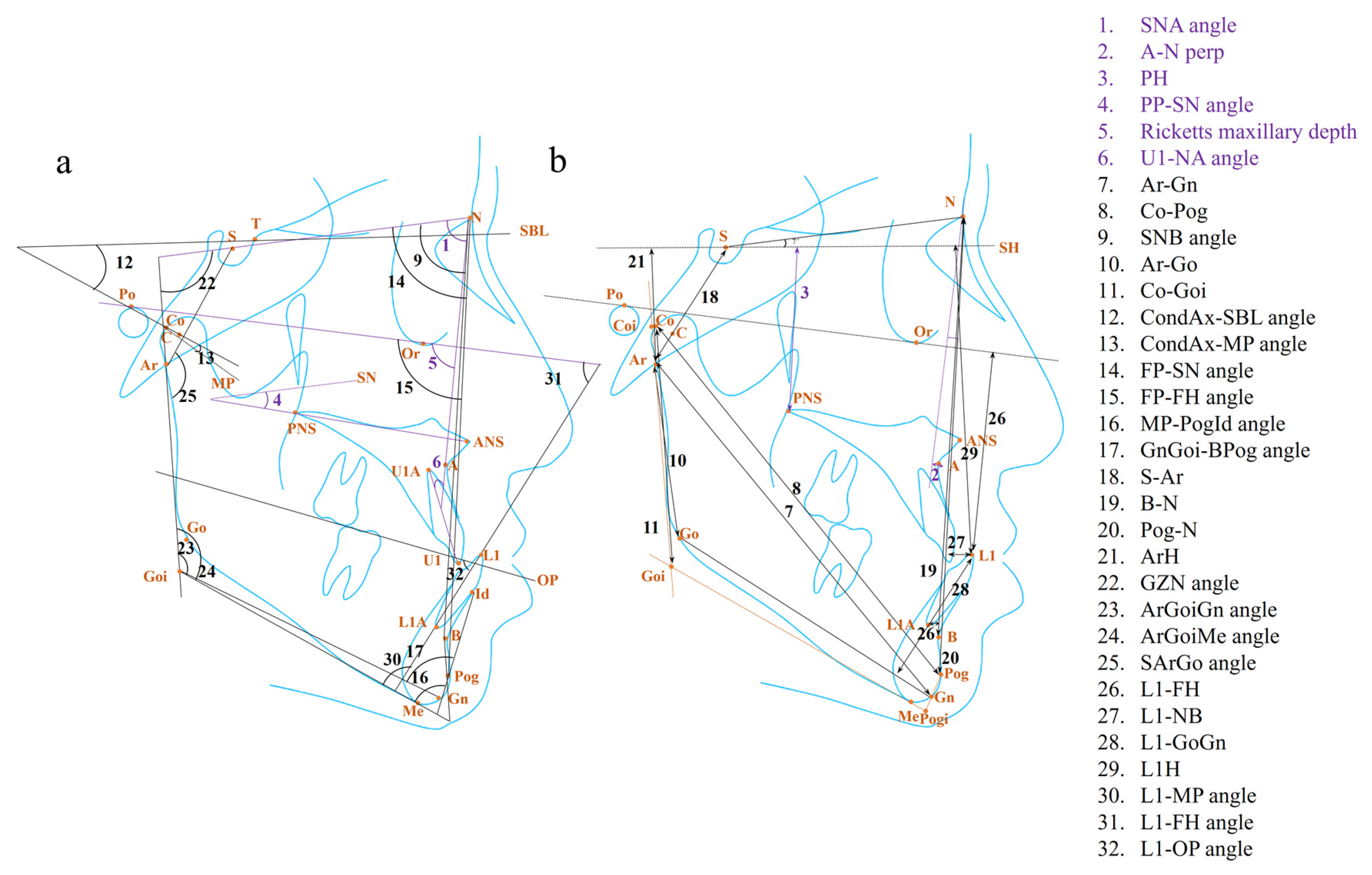
Figure 2.
The (a) angular, (b) linear, and proportional measurements in the maxillary (purple) and mandibular (black) dimension for diagnosis and treatment of skeletal Class III malocclusion in the existing literature. For the proportional values, only the involved landmark was labeled. The detailed information for the landmark, plane, and measurement is listed in Table S1.
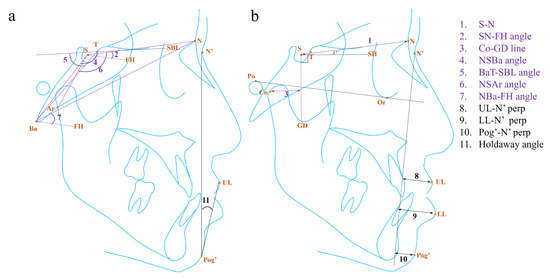
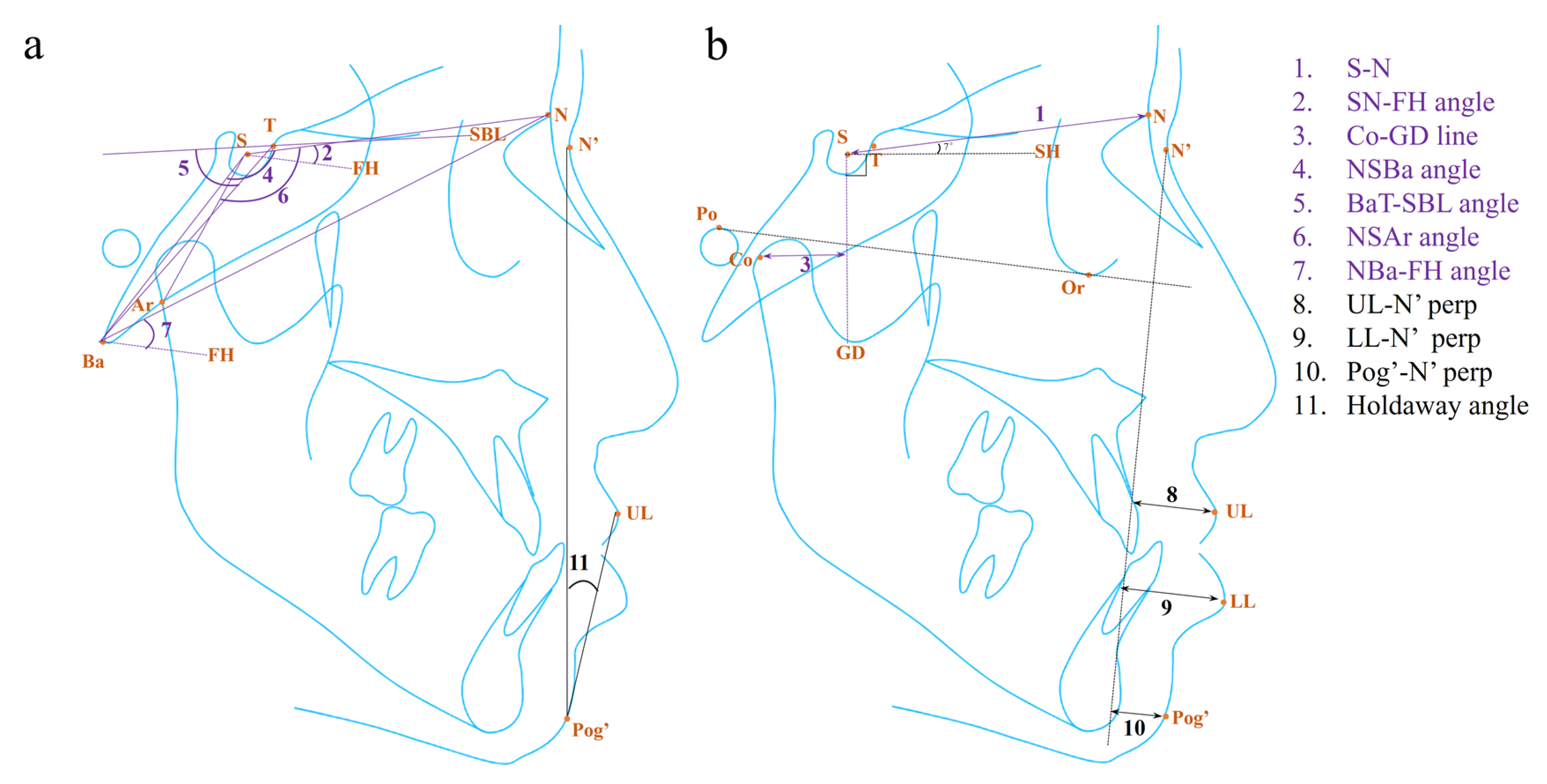
Figure 3.
The (a) angular, (b) linear, and proportional measurements in the cranial base (purple) and soft tissue (black) for diagnosis and treatment of skeletal Class III malocclusion in the existing literature. For the proportional values, only the involved landmark was labeled. The detailed information for the landmark, plane, and measurement is listed in Table S1.
3.1. Radiographic Features in the Maxilla
The maxilla is one of the key components of the maxillofacial complex that grows downward and forward, with its growth ending earlier than that of the mandible [19]. In general, maxillary deficiency and proclined upper incisors could be the dentoskeletal characteristics of skeletal Class III malocclusion. The corresponding parameters are related to the skeletal and dental measurements. Notably, although the maxillary measurement has been identified in various domains, it is relatively not a decisive factor and should be considered together with the assessment of other anatomical structures, especially the mandible.
As for the maxillary skeletal parameters, the length and height of the maxilla have been identified as the variables that explained the mild and borderline Class III facial subtypes, which means the maxillary morphology may apparently impact the facial appearance in those Class III cases [12]. In growth prediction, a smaller SNA angle appeared to be a negative predictor for unfavorable growth in children with Class III malocclusion with a threshold value of 79.1 degrees (Figure 2a) [45]. A longer distance between point A and the perpendicular line through point N was identified to represent a tendency for relapse of Class III malocclusion in children receiving early orthopedic treatment, which should be taken into consideration together with a smaller AB-MP angle (Figure 2b) [13,38]. In addition, a longer distance of PH or a more inferior position of PNS was identified as a negative predictor for the growth pattern or the relapse of Class III malocclusion in children and adolescents (Figure 2b) [43,44]. In addition, the PP-SN angle describing the maxillary growth rotation was another predictor of the growth pattern or the relapse of Class III malocclusion in children, where a bigger angle would contribute to a more satisfactory prognosis (Figure 2a) [25,28]. In terms of decision-making, the maxillary dimension was recognized as a predictor for orthognathic surgery need among adult patients with Class III malocclusion based on the ML model, but the model does not provide detailed measurements [34]. Additionally, the Ricketts maxillary depth, which indicates the degree of the maxillary protrusion, was identified as the ML-based predictor for making tooth extraction decisions in patients with different kinds of malocclusions. A smaller angle indicated a greater likelihood of orthodontic extraction need (Figure 2a) [29].
In terms of dental parameters, the maxillary incisor inclination, which was measured by the U1-NA angle, was found to be a predictor of treatment outcomes in Class III children treated with a combination of upper incisor proclination and headgear, where patients with a larger angle might respond poorly to the treatment (Figure 2a) [46]. Besides, the region of maxillary teeth was identified to influence decision-making about surgery using a deep learning model [47]. However, this correlation may not be applicable to all Class III cases, particularly those with mild skeletal discrepancies that do not exhibit compensatory inclination of the upper incisors.
3.2. Radiographic Features in the Mandible
The distinct growth of the mandible in skeletal Class III malocclusion has gathered the most interest from researchers and orthodontists for its particularity in the growing pattern and potential. The mandible is displaced downward and forward during growth. Meanwhile, the mandible, along with the maxilla, undergoes complicated rotational growth—internal rotation occurring in the core of the jawbone and external rotation due to bone surface remodeling—which leads to various vertical facial types [58,59]. As early as 1997, Sugawara et al. reviewed longitudinal studies and concluded that the skeletal framework of Class III malocclusion had been established during the pre-pubertal growth period, after which, the increment of annual mandibular growth for Class III patients remained similar to those with a normal face [60]. However, after a decade, another study indicated that the duration of the mandibular growth peak lasted longer in patients with skeletal Class III malocclusion, which can partly account for the larger increment of mandibular growth of Class III patients than those with normal occlusion during growth spurts [61]. The radiographic features in the mandible were summarized, which were related to the mandibular dimension, condyle, chin, mandibular growth rotation, and lower incisors.
The abnormal mandibular dimension is the most direct characteristic in the mandible for Class III malocclusion. The ratios of Ar-Me and Go-Pog to the anterior facial height (AFH) were recognized as the indicators for facial type classification (Figure 2b) [20]. A longer distance of Ar-Gn can help to predict a worse growth pattern in children with skeletal Class III malocclusion (Figure 2b) [43]. A longer distance of Co-Pog was identified as a predictor for the relapse of Class III malocclusion in adolescents after orthopedic therapy (Figure 2b) [44,48]. In addition, a study using ML models recognized the mandibular body dimension as an indicator for decision-making for growth modulation, camouflage orthodontic treatment, or orthognathic surgery [34]. However, this should be combined with other parameters regarding the mandibular growth direction. Recently, a deep learning study has indicated that the mandible, mandibular teeth, and mandibular symphysis were the most influential regions for surgical decision-making, although the study did not provide detailed information on their roles [47]. Apart from parameters or features that directly represent the mandibular dimension, SNB, as an indirect angular parameter, was adopted for facial type classification and predicting the relapse of Class III malocclusion in children undergoing combined orthopedic therapy (Figure 2a) [20,24]. Regarding mandibular ramus height, the distance of Ar-Go was the indicator for facial type classification (Figure 2b) [12,20]. Similarly, the distance of Co-Goi was identified as the predictor for the relapse of Class III malocclusion in the children after orthopedic therapy (Figure 2b) [37,48]. However, whether a longer or shorter distance of Co-Goi can predict the risk of relapse remained controversial, as it should be considered in combination with other mandibular parameters. Another study suggested an increased ratio of Coi-Go to Pogi-Go, with a threshold value of 0.72, was a predictor for the relapse of Class III malocclusion among children after orthodontic treatment (Figure 2b) [23].
The condyle is considered a growth site that largely determines the greatest postnatal growth potential in the mandible [62]. The condylar inclination is critical to the treatment of Class III malocclusion. A larger condylar axis (CondAx)-SBL angle has been associated with the increased stability of treatment outcomes in patients who received removable mandibular retractor therapy (Figure 2a) [36]. It could be explained by a recent study that a larger CondAx-SBL angle may represent an upward-forward inclination of the condyle which is in accordance with the expected change induced by the functional treatment [63]. In addition, the CondAx-MP angle is another predictor for the treatment outcome, where a bigger angle hinted at a larger possibility of relapse in children under rapid maxillary expansion followed by maxillary protraction with a facemask with a cut-off point at 147.8 degrees (Figure 2a) [50]. However, on the contrary, another study found that a smaller CondAx-MP angle may represent poorer treatment stability [5]. The inconsistency between the two studies might be related to the variations in the facial subtypes included.
In terms of the chin, the FP-SN angle and FP-FH angle were identified as the variables for the severe mandibular prognathic facial subtype (Figure 2a) [12]. The chin morphology measured by the MP-PogId angle was recognized for facial type classification, and a smaller GnGoi-BPog angle was a negative predictor for the relapse among adolescents receiving orthopedic treatment (Figure 2a) [11,20].
As one of the mechanisms of mandibular growth patterns mentioned above, internal rotation is one type of mandibular growth rotation. The internal rotation is composed of matrix rotation occurring around the center of the condyle, as well as intra-matrix rotation around the center inside the mandible [59]. As for the matrix rotation-related parameters, the distances of S-Ar, B-N, and Pog-N have been identified as the indicators for the classification of severe and mild Class III facial subtypes (Figure 2b) [12]. A larger distance of ArH was a negative predictor for the deterioration of Class III malocclusion during growth (Figure 2b) [43]. Additionally, a smaller GZN angle, defined by the angle between the ramus plane and the SN plane, together with a superiorly positioned Go, can help to predict a larger possibility of relapse of Class III malocclusion in children after early orthopedic treatment (Figure 2a) [24,44,51]. In the measurement for the intra-matrix rotation, a larger gonial angle was a significant parameter for a greater likelihood of relapse in children receiving combined orthopedic therapy (Figure 2a) [11,22,23,39,48,51]. A larger lower gonial angle which is divided by the N-Go line, was identified as an indicator of surgical need in adult patients [30]. Notably, the articular angle, the SArGo angle, was the parameter that described both the matrix and intra-matrix rotation (Figure 2a). It was identified as the variable explaining the treatment outcome of Class III children under the facemask treatment, where children with a smaller angle tended to experience Class III malocclusion relapse [27]. Considering mandibular rotation, Class III patients with prognathic mandibles and long faces are more likely to be treated with orthognathic surgery according to the ML model [53].
In the measurement of lower incisors, the distances of L1-FH, L1-NB, and L1-GoGn were the variables that explained the maxillary deficiency and high-angle subtype where there was apparently a compensatory inclination of the lower incisors (Figure 2b) [12]. A longer distance of L1H could predict the growth worsening in children with Class III malocclusion (Figure 2b) [43]. For the treatment, a smaller L1-MP angle and a larger L1-FH angle and L1-OP angle could assist in predicting Class III malocclusion relapse in children after various orthopedic therapies (Figure 2a) [25,49,51]. In addition, the distance of L1-NB was found to account for decision-making about tooth extraction according to the ML model. However, the study did not provide detailed information about how the distance predicted the orthodontic extraction mode due to the limitation of the ML model (Figure 2b) [52]. The lower incisor inclination also played a role in predicting the need for orthognathic surgery. A smaller L1-MP angle was the indicator for orthognathic surgical need in adult patients (Figure 2a) [32,35]. As for the treatment plan for the surgery, Chen et al. found that orthognathic surgery patients with a smaller L1-MP angle had a higher tendency to undergo the surgery-first approach with a threshold value of 76.1 degrees (Figure 2a) [54]. The authors supposed that the characteristic appeared more in Class III patients with a high angle, who generally had less dental crowding and compensation. Recently, Zhang et al. found that the angle between the axis of the mandibular symphysis and L1 should be taken into consideration during tooth decompensation treatment before orthognathic surgery, in case the tooth root came out of the alveolar bone [55].
3.3. Radiographic Features in the Cranial Base
As the “engine” of maxillary growth, the cranial base matures quite earlier compared with other maxillofacial bones, indirectly determining the shape and position of the maxillomandibular complex [64]. The parameters identified in this region mainly consist of the cranial base length and deflection.
The anterior cranial base length has been found to decrease in patients with Class III malocclusion, especially in Japanese and Chinese patients compared with British Caucasian patients due to their own genetic characteristics [65,66]. Then, the reduction of the anterior cranial base length may impact maxillary position, leading to maxillary deficiency [67]. In the diagnostic application, the anterior cranial base, i.e., the distance of S-N, was one of the variables for the mildly mandibular prognathic subtype in Class III patients (Figure 3b) [12]. In addition, it was also identified in relation to surgical decision-making, where the decreased length represented a greater demand for orthognathic surgery among Class III adult patients [30].
The cranial base deflection can be measured by the angles formed by the anterior or posterior cranial base and other reference planes. The SN-FH angle was identified as an indicator for the borderline Class III malocclusion subtype (Figure 3a) [12]. However, as nasion is not part of the cranial base, Seetala et al. proposed that the point of sphenoidale (Se), the intersection point between the sphenoid and ethmoid bones in the lateral cephalograms, played a role in measuring the anterior cranial base inclination [67]. Meanwhile, they observed a smaller cranial base angle (NSBa angle and SeSBa angle) and posterior cranial–base inclination (FH-SBa angle) in patients with Class III malocclusion, which means that the point of Ba was located more anteriorly in Class III patients [67]. It will then give rise to a more anterior position of the points of Co, Ar and even the whole mandible, leading to the deterioration of the discrepancy in the jaw relationship [31,48]. Similarly, studies identified a shorter distance between Co and a vertical line through S (GD line), a smaller NSBa angle, and a larger BaT-SBL angle as the predictors for the relapse of Class III malocclusion in children under orthopedic treatment (Figure 3a,b) [11,37,48]. Additionally, a smaller NSAr angle and a greater NBa-FH angle were found to be associated with a higher need for orthognathic surgery in Class III adult patients through discriminant analysis and the ML model (Figure 3a) [8,31].
3.4. Radiographic Features in the Soft Tissue
The soft tissues, such as the tongue and masticatory muscles, are closely related to the maxillofacial skeleton [68]. Although the radiographic features of bony tissues are significant for the diagnosis and treatment of malocclusion, the attention of orthodontists should not be completely shifted from the facial soft tissue to the skeletal structure, as facial soft tissue harmony is one of the goals of orthodontic treatment [69]. The parameters identified in this domain are mainly related to the position of the lips and the Holdaway angle.
The identified parameters describing the lip position mainly involved the sagittal position of the upper and lower lips. The distance between the point of UL and the perpendicular line through the point of N’ (N’ perp) was identified as the parameter explaining the borderline Class III malocclusion subtype, probably due to its availability for the detection of a mildly concave mid-face (Figure 3b) [12]. Besides, the distances of N’ perp-LL and N’ perp-Pog’ were the indicators explaining the variance of the subtypes of mandibular prognathism and a long face (Figure 3b) [12].
The Holdaway angle is a significant parameter, especially for decision-making regarding orthognathic surgery. Proposed by Holdaway in 1983, it refers to the angle formed by the harmony line (H line) and N’-Pog’ in order to measure the prominence of the upper lip and chin (Figure 3a) [70]. Some researchers believed that this soft tissue parameter could be more helpful in assisting treatment planning than the bony ones, especially in borderline Class III malocclusion cases where the facial aesthetics might be more critical than the skeletal discrepancy [33]. A smaller Holdaway angle was identified as an indicator for the need for orthognathic surgery in adult patients with Class III malocclusion, with the cut-off value ranging from 7.2 to 12 degrees in different studies [33,56,57]. The variation could be due to diverse races and inclusion criteria for Class III malocclusion. Additionally, it was also verified by the ML model as an indicator for surgical decision-making [35].
4. Radiographic Features in 3D Images of Skeletal Class III Malocclusion
Given the irregular shape and the intricate anatomical structure of the maxillofacial skeleton, three-dimensional (3D) imaging tends to be a more satisfactory approach for detecting oral and maxillofacial diseases, as well as the discrepancies in dental alignment and/or the jaws. However, with the relatively late emergence of 3D imaging technologies, only a few radiological features have been observed in Class III malocclusion cases based on CBCT and MRI until now, in contrast to numerous parameters identified in traditional 2D images. As 3D imaging technologies continue to advance, it is expected that more comprehensive and accurate parameters will be discovered, leading to the improved diagnosis and treatment of Class III malocclusion. We have summarized the representative features for Class III malocclusion in 3D images to provide a reference for future research (Table 4).

Table 4.
Studies evaluating the radiographic features on CBCT and MRI.
4.1. Radiographic Features in CBCT
The different locations of the mandibular canal (MC) in relation to the mandible in patients with Class III malocclusion have been preliminary studied. Huang et al. measured the position of MC in the inner and mid-posterior dimensions and did not observe significant differences in patients with various kinds of dentofacial relationships [71]. Nevertheless, F. Kalabalik later measured the 3D location of MC and found a more buccal, superior and forward position of MC in patients with Class III malocclusion compared with those with Class Ⅰ malocclusion. This may serve as a reference to reduce the risk of neurosensory disturbance during the orthognathic surgery [73].
Research has also focused on the specific features of condyles. Petra et al. demonstrated that Class III subjects had longer and larger condyles with higher antero–posterior and medio–lateral inclination angles based on CBCT [63]. The hyperdivergent subjects had smaller condyles with higher antero–posterior inclination angles, which further illustrates a strong association between the shape and the growth direction of condyles and the whole mandible [63]. Additionally, Kim et al. measured condylar bone densities in adolescents with different types of malocclusions and observed that the cortical, cancellous, and total bone densities increased as the ANB angle increased and the postero–anterior facial height ratio decreased [72]. It hinted that condylar bone densities could be candidate predictors for growth patterns in patients with different kinds of malocclusion.
Although CBCT is expected to aid in the diagnosis and treatment of malocclusion, the radiation protection of CBCT should be seriously taken into consideration in clinical practice. As described in the previous study, the radiation dose of a CBCT is about 3–6 times a panoramic radiograph (OPG), 8–14 times a postero–anterior cephalogram (PA), and 15–26 times a lateral cephalogram [78]. Hence, the ALARA (As Low As Reasonably Achievable) principle should always be followed by orthodontists and radiologists [79].
4.2. Radiographic Features in MRI
Studies have suggested that the temporomandibular joint (TMJ) disk and tongue may show some adaptive or even pathological changes in relation to the Class III malocclusion, which could be detected using MRI. It was reported that the displacement and abnormal shape of the TMJ disk were more common in patients with Class III malocclusion compared with those with Class Ⅰ malocclusion, while whether the vertical facial type was related to TMJ disk displacement remained controversial [75,76,77]. Additionally, in accordance with the growth pattern of the maxillofacial skeleton in Class III malocclusion cases, the posterior portion of the dorsal tongue and the tip of the tongue were reported to be positioned more inferiorly and anteriorly, respectively [74]. The tongue movement during the deglutition stage was also found to be different in patients with skeletal Class III malocclusion [74]. Future research should take advantage of MRI’s ability to detect dynamic changes in soft tissue to better elucidate their relationship with the maxillofacial skeleton and soft tissue in the context of skeletal Class III malocclusion.
5. Current States and Future Prospects
The development of radiology has greatly contributed to the diagnosis and treatment of skeletal Class III malocclusion. In this review, we provided a comprehensive summary of the significant parameters on 2D cephalograms for inter-maxillary relationship and various anatomical structures. Additionally, we synthesize the characteristics related to skeletal Class III malocclusion in 3D images based on the limited number of studies available. These radiographic features have the potential to assist in classifying facial type, predicting growth, making decisions regarding tooth extraction or orthognathic surgery, and guiding clinical practices. However, several limitations in current research still exist that may hinder the practical application of these features in diagnosing or treating Class III malocclusion.
In addition to the lateral cephaolograms, CBCT and MRI images, the OPG, and PA are commonly used in orthodontic clinical practice. Nevertheless, since the OPG provides a panoramic image of the teeth, mandible, and maxilla, and the PA is the cephalogram taken from the frontal view, both of them are not sensitive to detect the Class III malocclusion subtype which is characterized by the sagittal discrepancy. Up to now, no predictors for the diagnosis and treatment of skeletal Class III malocclusion have been identified in the OPG and PA.
The significant parameters identified in different studies often share little similarity, which may undermine their value in clinical application and generalization. This discrepancy might be associated with the following aspects. First, many studies had an insufficient sample size, especially longitudinal studies for growth prediction. Second, the standards for evaluating growth patterns or treatment outcomes differed among studies. In the cases of decision-making for tooth extraction or orthognathic surgery, it was the experts’ opinions that served as the grouping standards, potentially introducing bias. Third, variations in the quantity and the types of input values across studies, together with potential examiner measurement errors, could affect the power of identifying the significant parameters. Finally, the conventional statistical models or the ML algorithms performed in each study were not always consistent. These reasons make it difficult to objectively compare and apply those significant variables from various studies.
Despite plenty of identified parameters for the diagnosis and treatment of Class III malocclusion, the weight or priority of each variable in different structures remains unclear. Each parameter has its own advantage and disadvantage, making it difficult to select valuable indicators or a complete variable set from the candidate parameters to assist in the precise diagnosis or the treatment outcome prediction. In addition, the performance of the models in the diagnosis or treatment of Class III malocclusion was not always satisfactory, especially in borderline Class III cases [52]. Thus, the constructed models may not completely assist less-experienced orthodontists in practice.
Several ML models have been developed in orthodontics to identify relevant variables with greater accuracy compared to conventional statistical models [17,80,81,82]. Recently, two studies have developed deep learning models to predict the need for orthognathic surgery using lateral cephalograms [47,83]. Although these deep learning models obtained favorable prediction accuracy, interpreting their prediction outcomes is challenging due to their “black box” nature, making the decision-making process difficult to explain [17]. Most recently, it has been raised that quantitative textural imaging analysis could be utilized to predict the growth of specific organs or the progression of lesions [84,85]. The integration of ML and quantitative imaging feature analysis (i.e., radiomics) may potentially advance the personalized diagnosis and treatment of Class III malocclusion, enhancing the understanding of the underlying mechanisms of maxillofacial growth.
6. Conclusions
Radiographic features in 2D and 3D radiographic images provide valuable insight for the diagnosis and treatment of skeletal Class III malocclusion. Various parameters related to the inter-maxillary relationship and different anatomical structures contribute to the accurate diagnosis and prediction of facial growth or treatment outcomes, decision-making for tooth extraction and surgery, and guiding clinical practices. However, there are still some challenges to adopting these parameters into clinical practices due to their high diversity. With the improvement in generalizability and analytic approaches, including ML and radiomics, the significant radiographic features may become more informative for orthodontists to provide precise and personalized dental services.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics14050544/s1, Table S1: Description of the critical landmark, plane, and measurement on radiograms.
Author Contributions
Conceptualization, Z.-Y.L. and Z.-Y.S.; writing—original draft preparation, Z.-Y.L.; writing—review and editing, K.-F.H., Q.Y.H.A., M.G., Y.-X.S., and Z.-Y.S.; supervision, Z.-Y.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Angle, E.H. Classification of malocclusion. Dent. Cosmos 1899, 41, 350–357. [Google Scholar]
- Hardy, D.K.; Cubas, Y.P.; Orellana, M.F. Prevalence of angle class III malocclusion: A systematic review and meta-analysis. Open J. Epidemiol. 2012, 2, 75–82. [Google Scholar] [CrossRef]
- Ribeiro, L.G.; Antunes, L.S.; Küchler, E.C.; Baratto-Filho, F.; Kirschneck, C.; Guimarães, L.S.; Antunes, L.A.A. Impact of malocclusion treatments on Oral Health-Related Quality of Life: An overview of systematic reviews. Clin. Oral Investig. 2023, 27, 907–932. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, F.; Masalehi, H.; Golshah, A.; Imani, M.M. Oral health related quality of life of patients with class III skeletal malocclusion before and after orthognathic surgery. BMC Oral Health 2019, 19, 289. [Google Scholar] [CrossRef] [PubMed]
- Nardoni, D.N.; Siqueira, D.F.; Cardoso Mde, A.; Capelozza Filho, L. Cephalometric variables used to predict the success of interceptive treatment with rapid maxillary expansion and face mask. A longitudinal study. Dent. Press J. Orthod. 2015, 20, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Almashraqi, A.A.; Khadhi, A.H.; Arishi, K.A.; Alamir, A.A.; Beleges, E.M.; Halboub, E. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: A systematic review. Clin. Oral Investig. 2022, 26, 6443–6455. [Google Scholar] [CrossRef]
- Taraji, S.; Atici, S.F.; Viana, G.; Kusnoto, B.; Allareddy, V.S.; Miloro, M.; Elnagar, M.H. Novel Machine Learning Algorithms for Prediction of Treatment Decisions in Adult Patients with Class III Malocclusion. J. Oral Maxillofac. Surg. 2023, 81, 1391–1402. [Google Scholar] [CrossRef]
- Schulhof, R.J.; Nakamura, S.; Williamson, W.V. Prediction of abnormal growth in class III malocclusions. Am. J. Orthod. 1977, 71, 421–430. [Google Scholar] [CrossRef]
- Zentner, A.; Doll, G.M. Size discrepancy of apical bases and treatment success in angle Class III malocclusion. J. Orofac. Orthop. 2001, 62, 97–106. [Google Scholar] [CrossRef]
- Stensland, A.; Wisth, P.J.; Böe, O.E. Dentofacial changes in children with negative overjet treated by a combined orthodontic and orthopaedic approach. Eur. J. Orthod. 1988, 10, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Bui, C.; King, T.; Proffit, W.; Frazier-Bowers, S. Phenotypic characterization of Class III patients. Angle Orthod. 2006, 76, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.M.; Kang, B.Y.; Kim, H.G.; Baek, S.H. Prognosis prediction for Class III malocclusion treatment by feature wrapping method. Angle Orthod. 2009, 79, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhang, C.; Shan, Z. Application of Artificial Intelligence in Orthodontics: Current State and Future Perspectives. Healthcare 2023, 11, 2760. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.L.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Tortora, M.; Gemini, L.; Scaravilli, A.; Ugga, L.; Ponsiglione, A.; Stanzione, A.; D’arco, F.; D’anna, G.; Cuocolo, R. Radiomics Applications in Head and Neck Tumor Imaging: A Narrative Review. Cancers 2023, 15, 1174. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.F.; Ai, Q.Y.H.; Wong, L.M.; Yeung, A.W.K.; Li, D.T.S.; Leung, Y.Y. Current Applications of Deep Learning and Radiomics on CT and CBCT for Maxillofacial Diseases. Diagnostics 2022, 13, 110. [Google Scholar] [CrossRef]
- Fudalej, P.; Dragan, M.; Wedrychowska-Szulc, B. Prediction of the outcome of orthodontic treatment of Class III malocclusions—A systematic review. Eur. J. Orthod. 2011, 33, 190–197. [Google Scholar] [CrossRef]
- Manlove, A.E.; Romeo, G.; Venugopalan, S.R. Craniofacial Growth: Current Theories and Influence on Management. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 167–175. [Google Scholar] [CrossRef]
- Kim, C.; Ishikawa, H. Multivariate analysis of the effects of chin cap therapy. Hokkaido J. Dent. Sci. 1995, 16, 149–165. Available online: https://jglobal.jst.go.jp/en/detail?JGLOBAL_ID=200902180218977103 (accessed on 10 January 2024).
- Ueda, A.; Tussie, C.; Kim, S.; Kuwajima, Y.; Matsumoto, S.; Kim, G.; Satoh, K.; Nagai, S. Classification of Maxillofacial Morphology by Artificial Intelligence Using Cephalometric Analysis Measurements. Diagnostics 2023, 13, 2134. [Google Scholar] [CrossRef] [PubMed]
- Tahmina, K.; Tanaka, E.; Tanne, K. Craniofacial morphology in orthodontically treated patients of class III malocclusion with stable and unstable treatment outcomes. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 681–690. [Google Scholar] [CrossRef]
- Zentner, A.; Doll, G.M.; Peylo, S.M. Morphological parameters as predictors of successful correction of Class III malocclusion. Eur. J. Orthod. 2001, 23, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Ferro, A.; Nucci, L.P.; Ferro, F.; Gallo, C. Long-term stability of skeletal Class III patients treated with splints, Class III elastics, and chincup. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Schuster, G.; Lux, C.J.; Stellzig-Eisenhauer, A. Children with class III malocclusion: Development of multivariate statistical models to predict future need for orthognathic surgery. Angle Orthod. 2003, 73, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.; Wei, S.H.-Y. Early treatment of Class III patients to improve facial aesthetics and predict future growth. Hong Kong Dent. J. 2004, 1, 24–30. [Google Scholar]
- Choi, Y.J.; Chang, J.E.; Chung, C.J.; Tahk, J.H.; Kim, K.H. Prediction of long-term success of orthopedic treatment in skeletal Class III malocclusions. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 193–203. [Google Scholar] [CrossRef]
- Auconi, P.; Ottaviani, E.; Barelli, E.; Giuntini, V.; McNamara, J.A.; Franchi, L. Prognostic approach to Class III malocclusion through case-based reasoning. Orthod. Craniofac. Res. 2021, 24 (Suppl. 2), 163–171. [Google Scholar] [CrossRef]
- Real, A.D.; Real, O.D.; Sardina, S.; Oyonarte, R. Use of automated artificial intelligence to predict the need for orthodontic extractions. Korean J. Orthod. 2022, 52, 102–111. [Google Scholar] [CrossRef]
- Stellzig-Eisenhauer, A.; Lux, C.J.; Schuster, G. Treatment decision in adult patients with Class III malocclusion: Orthodontic therapy or orthognathic surgery? Am. J. Orthod. Dentofac. Orthop. 2002, 122, 27–37, discussion 37–38. [Google Scholar] [CrossRef]
- Kochel, J.; Emmerich, S.; Meyer-Marcotty, P.; Stellzig-Eisenhauer, A. New model for surgical and nonsurgical therapy in adults with Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e165–e174. [Google Scholar] [CrossRef] [PubMed]
- Martinez, P.; Bellot-Arcís, C.; Llamas, J.M.; Cibrian, R.; Gandia, J.L.; Paredes-Gallardo, V. Orthodontic camouflage versus orthognathic surgery for class III deformity: Comparative cephalometric analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 490–495. [Google Scholar] [CrossRef]
- Eslami, S.; Faber, J.; Fateh, A.; Sheikholaemmeh, F.; Grassia, V.; Jamilian, A. Treatment decision in adult patients with class III malocclusion: Surgery versus orthodontics. Prog. Orthod. 2018, 19, 28. [Google Scholar] [CrossRef] [PubMed]
- Prasad, J.; Mallikarjunaiah, D.R.; Shetty, A.; Gandedkar, N.; Chikkamuniswamy, A.B.; Shivashankar, P.C. Machine Learning Predictive Model as Clinical Decision Support System in Orthodontic Treatment Planning. Dent. J. 2022, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Ahmad, S.; Frazier, M.; Dundar, M.M.; Turkkahraman, H. A novel machine learning model for class III surgery decision. J. Orofac. Orthop. 2022. [Google Scholar] [CrossRef] [PubMed]
- Franchi, L.; Baccetti, T.; Tollaro, I. Predictive variables for the outcome of early functional treatment of Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. Cephalometric variables predicting the long-term success or failure of combined rapid maxillary expansion and facial mask therapy. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 16–22. [Google Scholar] [CrossRef]
- Moon, Y.M.; Ahn, S.J.; Chang, Y.I. Cephalometric predictors of long-term stability in the early treatment of Class III malocclusion. Angle Orthod. 2005, 75, 747–753. [Google Scholar] [CrossRef]
- Yoshida, I.; Yamaguchi, N.; Mizoguchi, I. Prediction of post-treatment outcome after combined treatment with maxillary protraction and chincap appliances. Eur. J. Orthod. 2006, 28, 89–96. [Google Scholar] [CrossRef]
- Jacobson, A. Update on the Wits appraisal. Angle Orthod. 1988, 58, 205–219. [Google Scholar] [CrossRef]
- Baik, C.Y.; Ververidou, M. A new approach of assessing sagittal discrepancies: The Beta angle. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, M.; Higurashi, N.; Miyazaki, S.; Itasaka, Y.; Chiba, S.; Nezu, H. Facial pattern categories of sleep breathing-disordered children using Ricketts analysis. Psychiatry Clin. Neurosci. 2002, 56, 329–330. [Google Scholar] [CrossRef] [PubMed]
- Abu Alhaija, E.S.; Richardson, A. Growth prediction in Class III patients using cluster and discriminant function analysis. Eur. J. Orthod. 2003, 25, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Wells, A.P.; Sarver, D.M.; Proffit, W.R. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006, 76, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Auconi, P.; Scazzocchio, M.; Caldarelli, G.; Nieri, M.; McNamara, J.A.; Franchi, L. Understanding interactions among cephalometrics variables during growth in untreated Class III subjects. Eur. J. Orthod. 2017, 39, 395–401. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Blagitz, M.N.; Almeida, G.A.; Normando, D. Factors associated with the stability of compensatory orthodontic treatment of Class III malocclusion in the permanent dentition. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e63–e72. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Ryu, J.-J.; Jang, H.S.; Lee, D.-Y.; Jung, S.-K. Deep convolutional neural networks based analysis of cephalometric radiographs for differential diagnosis of orthognathic surgery indications. Appl. Sci. 2020, 10, 2124. [Google Scholar] [CrossRef]
- Ghiz, M.A.; Ngan, P.; Gunel, E. Cephalometric variables to predict future success of early orthopedic Class III treatment. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 301–306. [Google Scholar] [CrossRef]
- Ko, Y.I.; Baek, S.H.; Mah, J.; Yang, W.S. Determinants of successful chincup therapy in skeletal class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 33–41. [Google Scholar] [CrossRef]
- Souki, B.Q.; Nieri, M.; Pavoni, C.; Pavan Barros, H.M.; Junqueira Pereira, T.; Giuntini, V.; Cozza, P.; Franchi, L. Development and validation of a prediction model for long-term unsuccess of early treatment of Class III malocclusion. Eur. J. Orthod. 2020, 42, 200–205. [Google Scholar] [CrossRef]
- Inoue, Y.; Deguchi, T.; Hartsfield, J.K., Jr.; Tome, W.; Kitai, N. Analysis of pretreatment factors associated with stability in early class III treatment. Prog. Orthod. 2021, 22, 23. [Google Scholar] [CrossRef] [PubMed]
- Etemad, L.; Wu, T.H.; Heiner, P.; Liu, J.; Lee, S.; Chao, W.L.; Zaytoun, M.L.; Guez, C.; Lin, F.; Jackson, C.B.; et al. Machine learning from clinical data sets of a contemporary decision for orthodontic tooth extraction. Orthod. Craniofac. Res. 2021, 24 (Suppl. 2), 193–200. [Google Scholar] [CrossRef] [PubMed]
- Khosravi-Kamrani, P.; Qiao, X.; Zanardi, G.; Wiesen, C.A.; Slade, G.; Frazier-Bowers, S.A. A machine learning approach to determine the prognosis of patients with Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2022, 161, e1–e11. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Chen, C.Y.; Chen, M.C.; Ko, E.W.; Lin, C.H. Dental Occlusion Characteristics for Treatment Decision-Making Regarding Surgery-First Approach in Orthodontics. J. Clin. Med. 2023, 12, 6029. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liang, Y.; Chen, R.; Chen, S.; Lin, J.; Han, B.; Liu, X. Inclination of mandibular incisors and symphysis in severe skeletal class III malocclusion. Head Face Med. 2023, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Rabie, A.B.; Wong, R.W.; Min, G.U. Treatment in Borderline Class III Malocclusion: Orthodontic Camouflage (Extraction) Versus Orthognathic Surgery. Open Dent. J. 2008, 2, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Benyahia, H.; Azaroual, M.F.; Garcia, C.; Hamou, E.; Abouqal, R.; Zaoui, F. Treatment of skeletal Class III malocclusions: Orthognathic surgery or orthodontic camouflage? How to decide. Int. Orthod. 2011, 9, 196–209. [Google Scholar] [CrossRef] [PubMed]
- Mosca, G.; Grippaudo, C.; Marchionni, P.; Deli, R. Class III dento-skeletal anomalies: Rotational growth and treatment timing. Eur. J. Paediatr. Dent. 2006, 7, 23–28. [Google Scholar]
- Kim, J.H.; Kim, Y.H.; Kim, S.J.; Sung, J.; Song, Y.M.; Shin, J.W.; Park, J.H.; Chae, H.S. Twin study-genetic comparison of matrix versus intramatrix rotation in the mandible and three different occlusal planes. Prog. Orthod. 2020, 21, 44. [Google Scholar] [CrossRef]
- Sugawara, J.; Mitani, H. Facial growth of skeletal Class III malocclusion and the effects, limitations, and long-term dentofacial adaptations to chincap therapy. Semin. Orthod. 1997, 3, 244–254. [Google Scholar] [CrossRef]
- Baccetti, T.; Reyes, B.C.; McNamara, J.A., Jr. Craniofacial changes in Class III malocclusion as related to skeletal and dental maturation. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 171.e1–171.e12. [Google Scholar] [CrossRef] [PubMed]
- Lemes, C.R.; Tozzi, C.F.; Gribel, S.; Gribel, B.F.; Venezian, G.C.; do Carmo Menezes, C.; Custodio, W. Mandibular ramus height and condyle distance asymmetries in individuals with different facial growth patterns: A cone-beam computed tomography study. Surg. Radiol. Anat. 2021, 43, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Santander, P.; Quast, A.; Olbrisch, C.; Rose, M.; Moser, N.; Schliephake, H.; Meyer-Marcotty, P. Comprehensive 3D analysis of condylar morphology in adults with different skeletal patterns—A cross-sectional study. Head Face Med. 2020, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Vora, S.R. Mouse models for the study of cranial base growth and anomalies. Orthod. Craniofac. Res. 2017, 20 (Suppl. 1), 18–25. [Google Scholar] [CrossRef] [PubMed]
- Ishii, N.; Deguchi, T.; Hunt, N.P. Craniofacial differences between Japanese and British Caucasian females with a skeletal Class III malocclusion. Eur. J. Orthod. 2002, 24, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Proff, P.; Will, F.; Bokan, I.; Fanghänel, J.; Gedrange, T. Cranial base features in skeletal Class III patients. Angle Orthod. 2008, 78, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Sanggarnjanavanich, S.; Sekiya, T.; Nomura, Y.; Nakayama, T.; Hanada, N.; Nakamura, Y. Cranial-base morphology in adults with skeletal Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 82–91. [Google Scholar] [CrossRef]
- Buvinic, S.; Balanta-Melo, J.; Kupczik, K.; Vásquez, W.; Beato, C.; Toro-Ibacache, V. Muscle-Bone Crosstalk in the Masticatory System: From Biomechanical to Molecular Interactions. Front. Endocrinol. 2020, 11, 606947. [Google Scholar] [CrossRef]
- Nanda, R.S.; Ghosh, J. Facial soft tissue harmony and growth in orthodontic treatment. Semin. Orthod. 1995, 1, 67–81. [Google Scholar] [CrossRef]
- Holdaway, R.A. A soft-tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am. J. Orthod. 1983, 84, 1–28. [Google Scholar] [CrossRef]
- Huang, C.Y.; Liao, Y.F. Anatomical position of the mandibular canal in relation to the buccal cortical bone in Chinese patients with different dentofacial relationships. J. Formos. Med. Assoc. 2016, 115, 981–990. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J.; Park, J.H.; Bay, R.C.; Lee, M.Y.; Chang, N.Y.; Chae, J.M. Mandibular condyle bone density in adolescents with varying skeletal patterns evaluated using cone-beam computed tomography: A potential predictive tool. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Kalabalik, F.; Akçay, H.; Tatar, B. Morphometric analysis of mandibular corpus relevance to sagittal split osteotomy: Comparison of dentoskeletal Class I and Class III patients. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Görgülü, S.; Sağdıç, D.; Akin, E.; Karaçay, S.; Bulakbası, N. Tongue movements in patients with skeletal Class III malocclusions evaluated with real-time balanced turbo field echo cine magnetic resonance imaging. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e405–e414. [Google Scholar] [CrossRef] [PubMed]
- Jung, W.S.; Kim, H.; Jeon, D.M.; Mah, S.J.; Ahn, S.J. Magnetic resonance imaging-verified temporomandibular joint disk displacement in relation to sagittal and vertical jaw deformities. Int. J. Oral Maxillofac. Surg. 2013, 42, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Gökalp, H. Disc position in clinically asymptomatic, pretreatment adolescents with Class I, II, or III malocclusion: A retrospective magnetic resonance imaging study. J. Orofac. Orthop. 2016, 77, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Tagawa, D.T.; Franco, A.A.; Puchnick, A.; Wolosker, A.M.B.; Florez, B.M.; Dominguez, G.C.; Yamashita, H.K.; Cevidanes, L.H.S.; Aidar, L.A.d.A.; Junior, H.C. Temporomandibular joint articular disc position and shape in skeletal Class III. Orthod. Craniofac. Res. 2023, 26, 185–196. [Google Scholar] [CrossRef]
- Signorelli, L.; Patcas, R.; Peltomäki, T.; Schätzle, M. Radiation dose of cone-beam computed tomography compared to conventional radiographs in orthodontics. J. Orofac. Orthop. 2016, 77, 9–15. [Google Scholar] [CrossRef]
- Staderini, E.; Guglielmi, F.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: A novel method. Orthod. Craniofac. Res. 2019, 22, 16–23. [Google Scholar] [CrossRef]
- Hung, K.F.; Yeung, A.W.K.; Bornstein, M.M.; Schwendicke, F. Personalized dental medicine, artificial intelligence, and their relevance for dentomaxillofacial imaging. Dentomaxillofac. Radiol. 2023, 52, 20220335. [Google Scholar] [CrossRef]
- Hung, K.F.; Ai, Q.Y.H.; Leung, Y.Y.; Yeung, A.W.K. Potential and impact of artificial intelligence algorithms in dento-maxillofacial radiology. Clin. Oral Investig. 2022, 26, 5535–5555. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.; Montalvao, C.; Tanaka, R.; Kawai, T.; Bornstein, M.M. The use and performance of artificial intelligence applications in dental and maxillofacial radiology: A systematic review. Dentomaxillofac. Radiol. 2020, 49, 20190107. [Google Scholar] [CrossRef]
- Shin, W.; Yeom, H.G.; Lee, G.H.; Yun, J.P.; Jeong, S.H.; Lee, J.H.; Kim, H.K.; Kim, B.C. Deep learning based prediction of necessity for orthognathic surgery of skeletal malocclusion using cephalogram in Korean individuals. BMC Oral Health 2021, 21, 130. [Google Scholar] [CrossRef] [PubMed]
- Caloro, E.; Cè, M.; Gibelli, D.; Palamenghi, A.; Martinenghi, C.; Oliva, G.; Cellina, M. Artificial Intelligence (AI)-Based Systems for Automatic Skeletal Maturity Assessment through Bone and Teeth Analysis: A Revolution in the Radiological Workflow? Appl. Sci. 2023, 13, 3860. [Google Scholar] [CrossRef]
- Nardone, V.; Reginelli, A.; Grassi, R.; Boldrini, L.; Vacca, G.; D’Ippolito, E.; Annunziata, S.; Farchione, A.; Belfiore, M.P.; Desideri, I.; et al. Delta radiomics: A systematic review. Radiol. Med. 2021, 126, 1571–1583. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).