Prediction Models Using Decision Tree and Logistic Regression Method for Predicting Hospital Revisits in Peritoneal Dialysis Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design
2.3. Covariates and Outcomes
2.4. Statistics
3. Results
3.1. Patient Characteristics for the ER Return Study
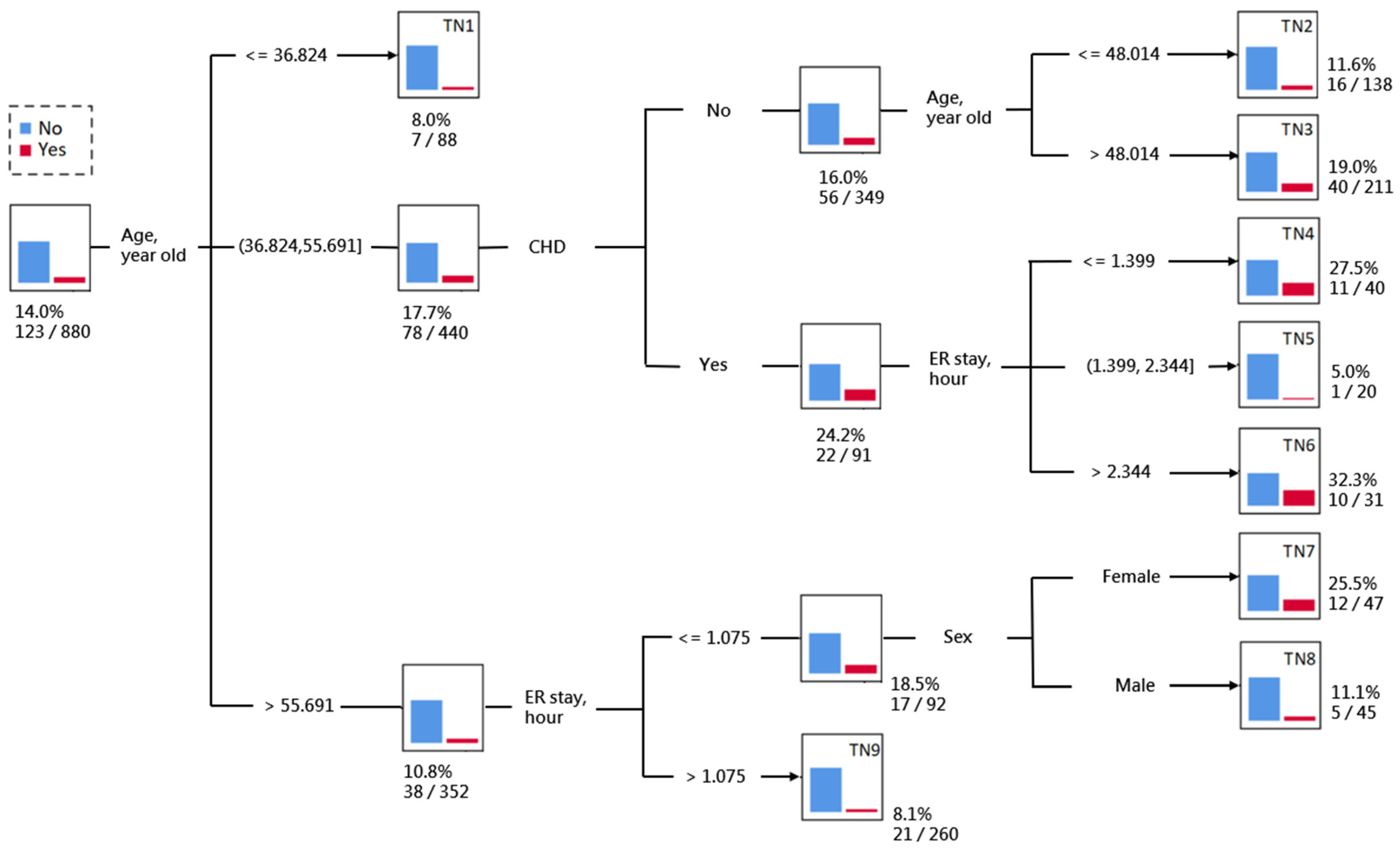
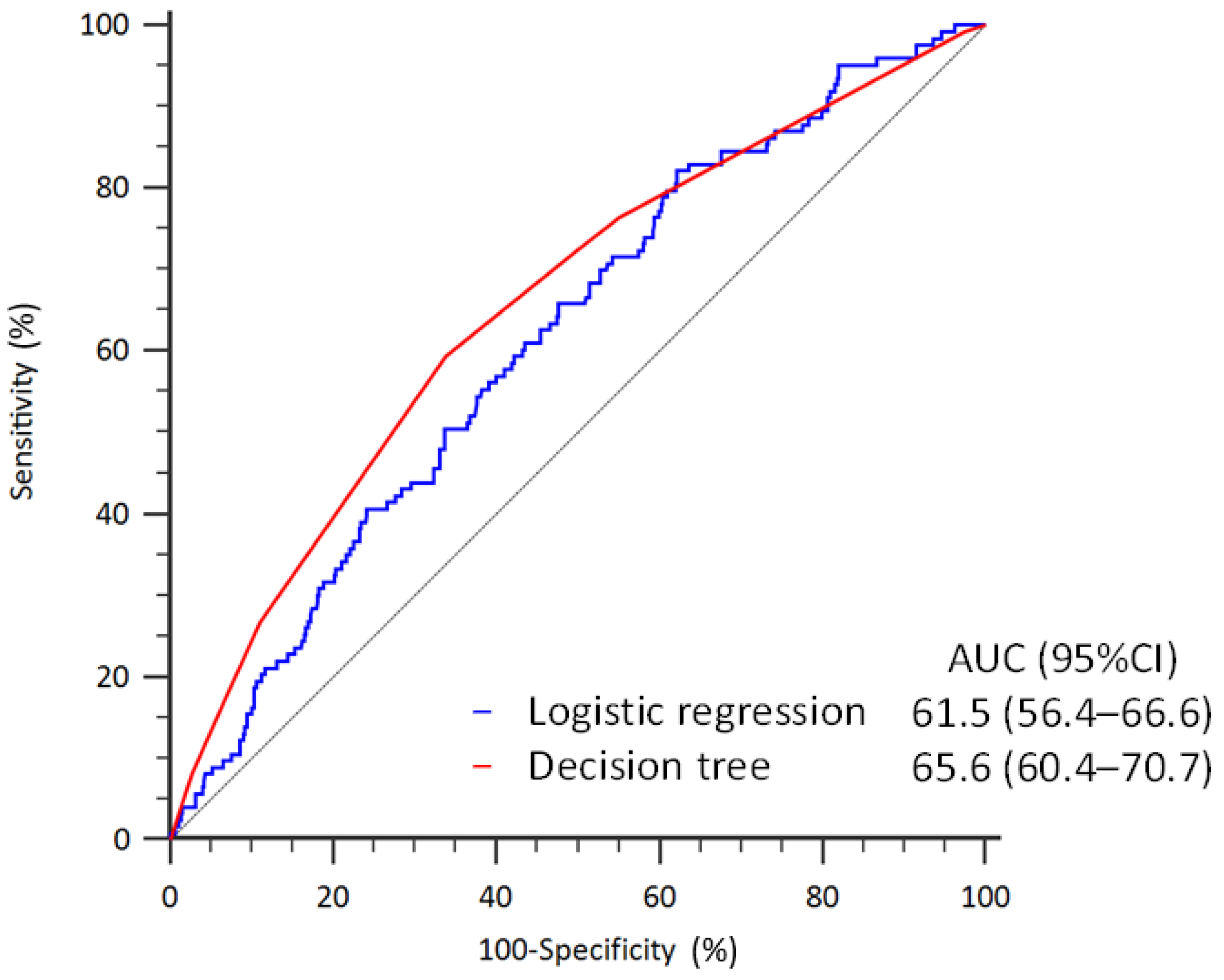
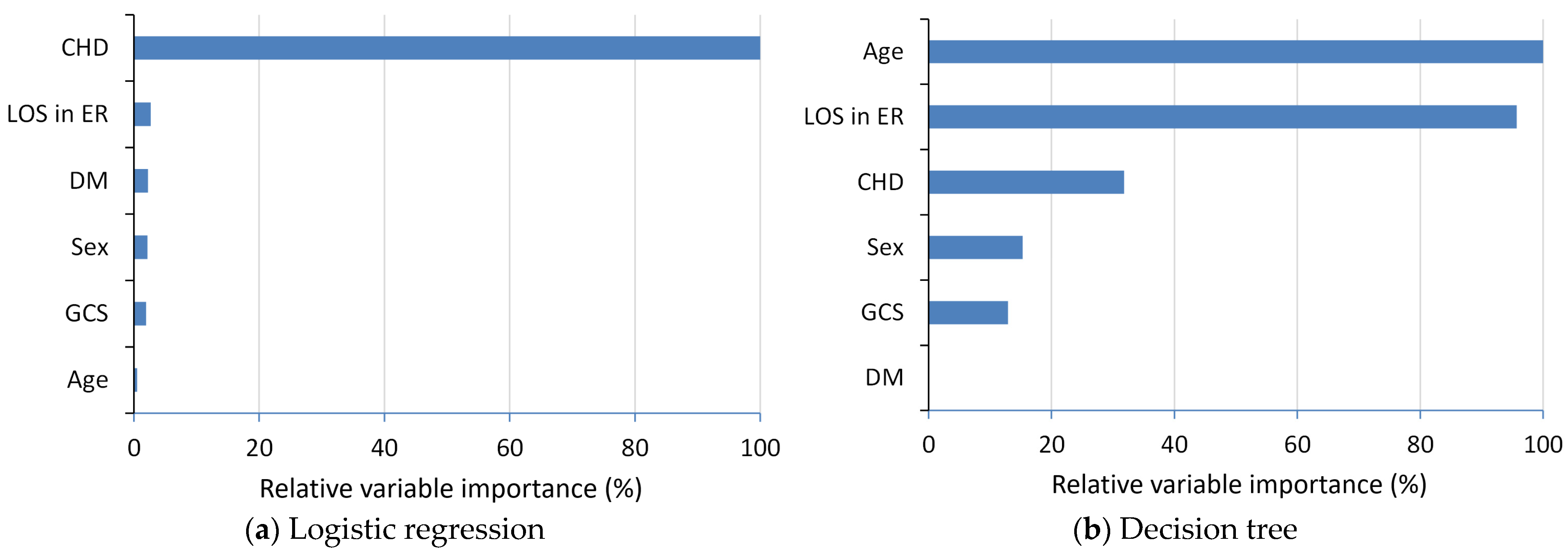
3.2. Prediction of ER Return within 72-h
3.3. Patient Characteristics for the Readmission Study
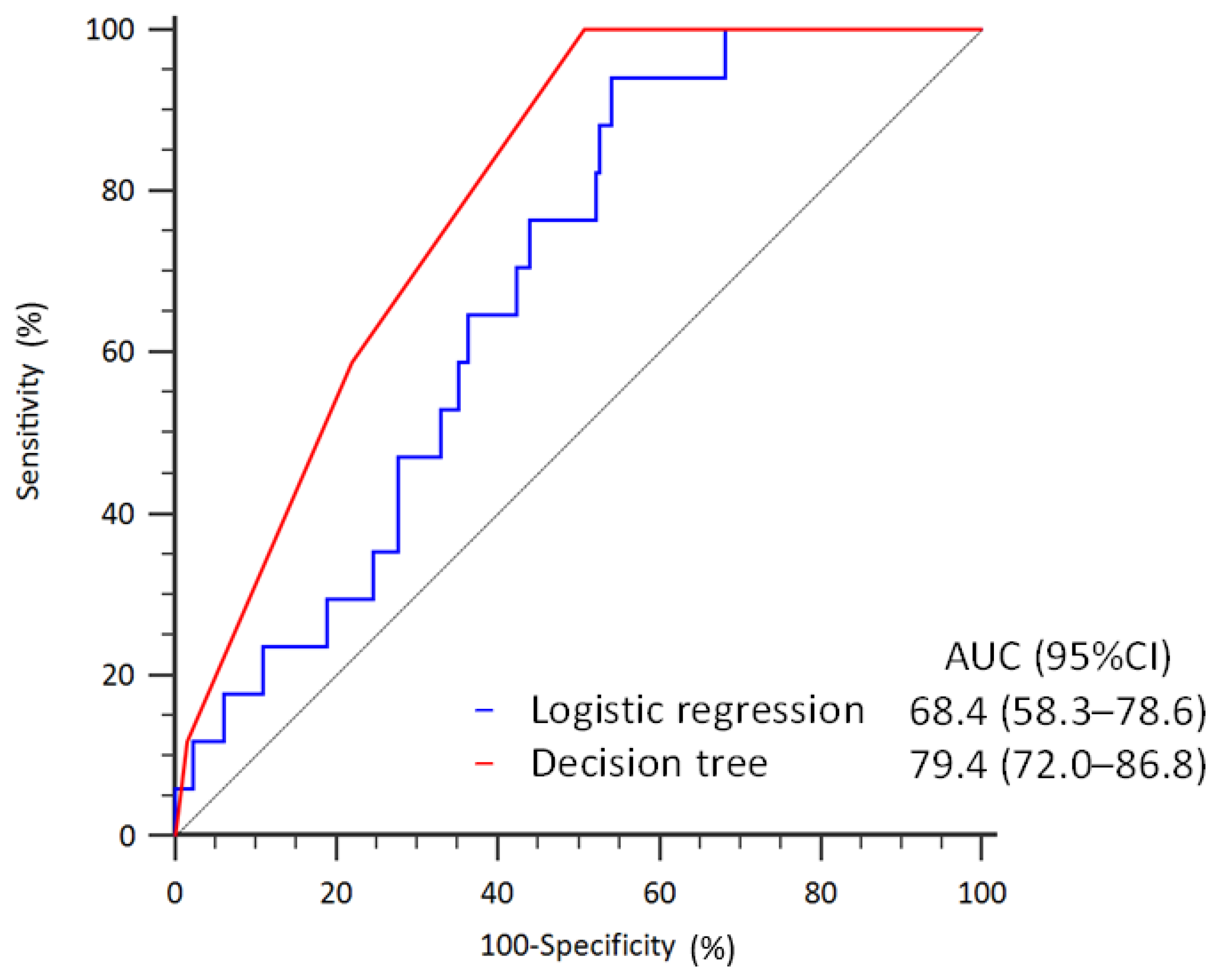
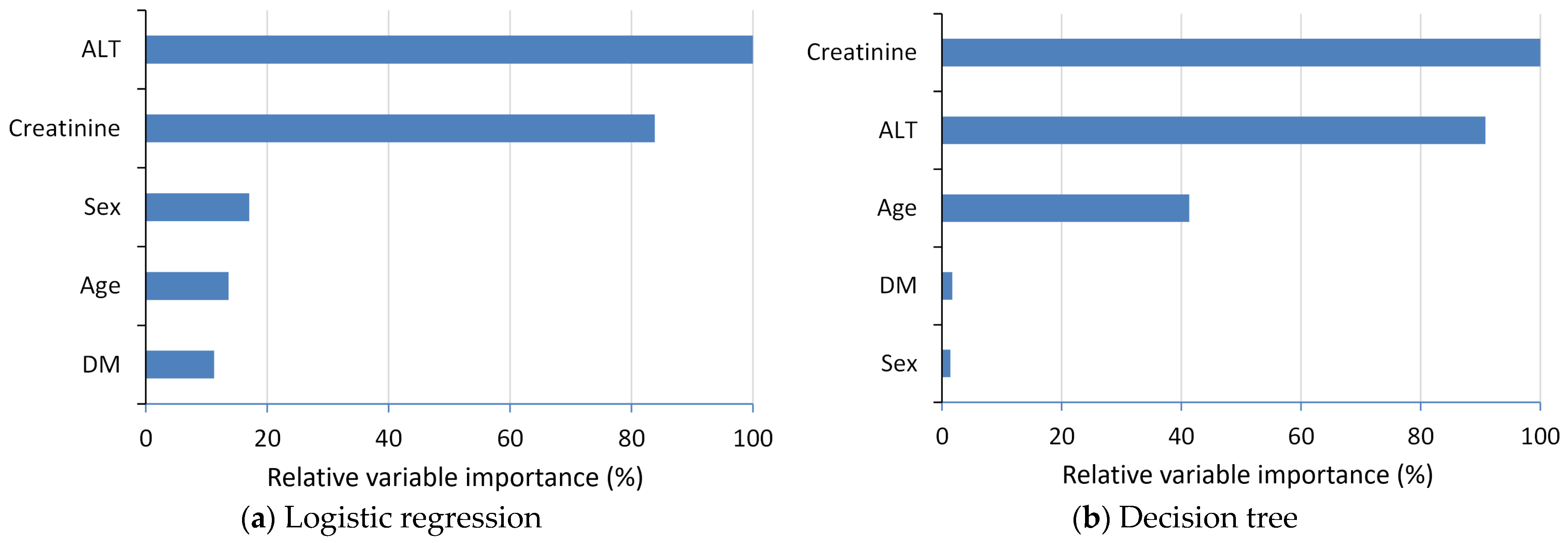
3.4. Prediction of Readmission within 14-Days
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hao, S.; Jin, B.O.; Shin, A.Y.; Zhao, Y.; Zhu, C.; Li, Z.; Hu, Z.; Fu, C.; Ji, J.; Wang, Y.; et al. Risk prediction of emergency department revisit 30 days post discharge: A prospective study. PLoS ONE 2014, 9, e112944. [Google Scholar] [CrossRef]
- Han, C.-Y.; Chen, L.-C.; Barnard, A.; Lin, C.-C.; Hsiao, Y.-C.; Liu, H.-E.; Chang, W. Early revisit to the emergency department: An integrative review. J. Emerg. Nurs. 2015, 41, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.; Lingsma, H.F.; Marang-van de Mheen, P.J.; Kringos, D.S.; Klazinga, N.S.; Steyerberg, E.W. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS ONE 2014, 9, e112282. [Google Scholar] [CrossRef]
- Yang, C.C. Explainable Artificial Intelligence for Predictive Modeling in Healthcare. J. Healthc. Inform. Res. 2022, 6, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Ehrman, R.R.; Kline, J.A. Primer on logistic regression for emergency care researchers. J. Emerg. Med. 2022, 63, 683–691. [Google Scholar] [CrossRef]
- Tanimu, J.J.; Hamada, M.; Hassan, M.; Kakudi, H.; Abiodun, J.O. A machine learning method for classification of cervical cancer. Electronics 2022, 11, 463. [Google Scholar] [CrossRef]
- Lin, C.-L.; Fan, C.-L. Evaluation of CART, CHAID, and QUEST algorithms: A case study of construction defects in Taiwan. J. Asian Archit. Build. Eng. 2019, 18, 539–553. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Chu, C.-C.; Lin, C.-H.; Huang, C.-H.; Ng, C.-J.; Lin, G.-Y.; Chiou, M.-J.; Lo, H.-Y.; Chen, S.-Y. A Machine Learning Model for Predicting Unscheduled 72 h Return Visits to the Emergency Department by Patients with Abdominal Pain. Diagnostics 2022, 12, 82. [Google Scholar] [CrossRef]
- Lin, L.-T.; Lin, S.-F.; Chao, C.-C.; Lin, H.-A. Predictors of 72-h unscheduled return visits with admission in patients presenting to the emergency department with abdominal pain. Eur. J. Med. Res. 2023, 28, 288. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Chu, C.-C.; Ng, C.-J.; Lin, C.-H.; Lo, H.-Y.; Chen, S.-Y. Machine learning models for predicting unscheduled return visits of patients with abdominal pain at emergency department and validation during COVID-19 pandemic: A retrospective cohort study. Medicine 2024, 103, e37220. [Google Scholar] [CrossRef]
- Kao, C.-L.; Chuang, C.-C.; Hwang, C.-Y.; Lee, C.-H.; Huang, P.-C.; Hong, M.-Y.; Chi, C.-H. The risk factors of the 72-h unscheduled return visit admission to emergency department in adults below 50 years old. Eur. J. Med. Res. 2023, 28, 379. [Google Scholar] [CrossRef] [PubMed]
- Banshodani, M.; Kawanishi, H.; Moriishi, M.; Shintaku, S.; Tsuchiya, S. Association between dialysis modality and cardiovascular diseases: A comparison between peritoneal dialysis and hemodialysis. Blood Purif. 2020, 49, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, J.P.; Zasadil, S.; Keyser, D.J.; Peele, P.B. Using decision trees to manage hospital readmission risk for acute myocardial infarction, heart failure, and pneumonia. Appl. Health Econ. Health Policy 2014, 12, 573–585. [Google Scholar] [CrossRef] [PubMed]
- Karmen, A.; Wróblewski, F.; LaDue, J.S. Transaminase activity in human blood. J. Clin. Investig. 1955, 34, 126–133. [Google Scholar] [CrossRef]
- Felig, P. The glucose-alanine cycle. Metabolism 1973, 22, 179–207. [Google Scholar] [CrossRef]
- Segev, A.; Itelman, E.; Avaky, C.; Negru, L.; Shenhav-Saltzman, G.; Grupper, A.; Wasserstrum, Y.; Segal, G. Low ALT levels associated with poor outcomes in 8700 hospitalized heart failure patients. J. Clin. Med. 2020, 9, 3185. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Kashani, K. Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients. J. Thorac. Dis. 2016, 8, E305. [Google Scholar] [CrossRef]
- Musoro, J.Z.; Zwinderman, A.H.; Puhan, M.A.; ter Riet, G.; Geskus, R.B. Validation of prediction models based on lasso regression with multiply imputed data. BMC Med. Res. Methodol. 2014, 14, 116. [Google Scholar] [CrossRef]
- Wang, S.; Chen, Y.; Cui, Z.; Lin, L.; Zong, Y. Diabetes Risk Analysis Based on Machine Learning LASSO Regression Model. J. Theory Pract. Eng. Sci. 2024, 4, 58–64. [Google Scholar]
- Allam, A.; Nagy, M.; Thoma, G.; Krauthammer, M. Neural networks versus Logistic regression for 30 days all-cause readmission prediction. Sci. Rep. 2019, 9, 9277. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Hu, J.; Szymczak, S. A review on longitudinal data analysis with random forest. Brief. Bioinform. 2023, 24, bbad002. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Mahajan, P.; Uddin, S.; Hajati, F.; Moni, M.A. Ensemble Learning for Disease Prediction: A Review. Healthcare 2023, 11, 1808. [Google Scholar] [CrossRef] [PubMed]
- McLeish, E.; Slater, N.; Mastaglia, F.L.; Needham, M.; Coudert, J.D. From data to diagnosis: How machine learning is revolutionizing biomarker discovery in idiopathic inflammatory myopathies. Brief. Bioinform. 2024, 25, bbad514. [Google Scholar] [CrossRef]

| Return to ER within 72-h | |||||
|---|---|---|---|---|---|
| Variable | Valid N | Total (n = 880) | Yes (n = 123) | No (n = 757) | p Value |
| Male | 880 | 475 (54.0) | 63 (51.2) | 412 (54.4) | 0.737 |
| Age, year | 880 | 54.5 ± 13.2 | 54.5 ± 11.8 | 54.5 ± 13.4 | 0.981 |
| Taiwan triage and acuity scale | 880 | 0.433 | |||
| Level I: Resuscitation | 42 (4.8) | 6 (4.9) | 36 (4.8) | ||
| Level II: Emergency | 172 (19.5) | 26 (21.1) | 146 (19.3) | ||
| Level III: Urgency | 527 (59.9) | 74 (60.2) | 453 (59.8) | ||
| Level IV: Less urgency | 122 (13.9) | 17 (13.8) | 105 (13.9) | ||
| Level V: Non urgency | 17 (1.9) | 0 (0.0) | 17 (2.2) | ||
| Glasgow Coma Scale | 878 | 14.8 ± 0.94 | 15.0 ± 0.09 | 14.8 ± 1.01 | <0.001 |
| Comorbidity | |||||
| Coronary heart disease | 880 | 120 (13.6) | 25 (20.3) | 95 (12.5) | 0.006 |
| Hypertension | 880 | 861 (97.8) | 121 (98.4) | 740 (97.8) | 0.872 |
| Diabetes mellitus | 880 | 401 (45.6) | 54 (43.9) | 347 (45.8) | 0.684 |
| Stroke | 880 | 197 (22.4) | 30 (24.4) | 167 (22.1) | 0.813 |
| Chronic obstruction pulmonary disease | 880 | 105 (11.9) | 11 (8.9) | 94 (12.4) | 0.287 |
| Peripheral arterial disease | 880 | 111 (12.6) | 8 (6.5) | 103 (13.6) | 0.115 |
| Hyperkalemia | 880 | 267 (30.3) | 38 (30.9) | 229 (30.3) | 0.690 |
| Acute pulmonary edema | 880 | 197 (22.4) | 35 (28.5) | 162 (21.4) | 0.135 |
| Acidosis | 880 | 64 (7.3) | 9 (7.3) | 55 (7.3) | 0.837 |
| Heart failure | 880 | 174 (19.8) | 26 (21.1) | 148 (19.6) | 0.867 |
| Vital signs | |||||
| Systolic blood pressure, mmHg | 535 | 144.0 ± 35.0 | 140.5 ± 33.6 | 144.6 ± 35.2 | 0.300 |
| Diastolic blood pressure, mmHg | 534 | 83.0 ± 19.0 | 82.7 ± 16.5 | 83.3 ± 19.0 | 0.791 |
| Body temperature, °C | 330 | 36.5 ± 0.7 | 36.6 ± 0.7 | 36.4 ± 0.7 | 0.217 |
| Heart rate, beat/min | 529 | 82.2 ± 15.3 | 82.6 ± 14.2 | 82.1 ± 15.5 | 0.773 |
| Respiratory rate, beat/min | 163 | 21.6 ± 12.3 | 20.1 ± 0.4 | 21.9 ± 13.7 | 0.449 |
| Peritonitis | 880 | 38 (4.3) | 7 (5.7) | 31 (4.1) | 0.423 |
| Lab data | |||||
| Leukocyte, 1000/μL | 522 | 7.3 (5.4, 9.7) | 6.8 (4.9, 9.6) | 7.3 (5.5, 9.7) | 0.195 |
| Hemoglobin, g/dL | 534 | 10.0 (8.7, 11.3) | 10.0 (8.5, 11.2) | 9.9 (8.8, 11.3) | 0.538 |
| Alanine aminotransferase, U/L | 409 | 20.0 (15.0, 28.0) | 20.0 (16.0, 26.0) | 20.0 (15.0, 28.0) | 0.929 |
| BUN, mg/dL | 288 | 61.7 (42.2, 79.0) | 62.6 (39.5, 77.8) | 61.4 (42.5, 79.1) | 0.735 |
| Creatinine, mg/dL | 293 | 10.1 (7.4, 12.9) | 10.4 (8.8, 14.3) | 10.0 (7.2, 12.9) | 0.120 |
| Sodium, mg/dL | 493 | 134.6 (131.0, 137.2) | 135.0 (130.8, 137.8) | 134.3 (131.1, 137.1) | 0.791 |
| Potassium, mg/dL | 506 | 3.8 (3.2, 4.3) | 3.8 (3.1, 4.3) | 3.8 (3.2, 4.3) | 0.624 |
| C-reactive protein, mg/dL | 211 | 10.0 (5.0, 28.9) | 12.8 (5.0, 45.2) | 9.6 (5.0, 25.4) | 0.076 |
| Calcium, mg/dL | 254 | 9.8 (9.2, 10.5) | 9.9 (9.3, 10.6) | 9.8 (9.1, 10.4) | 0.191 |
| Phosphates, mg/dL | 201 | 4.8 (3.9, 5.7) | 5.0 (4.2, 5.8) | 4.8 (3.9, 5.7) | 0.276 |
| Platelet, 1000/μL | 515 | 188.0 (151.0, 229.0) | 189.5 (151.5, 229.5) | 188.0 (149.0, 229.0) | 0.750 |
| Neutrophil, % | 495 | 70.8 (62.0, 78.8) | 71.0 (60.5, 79.0) | 70.6 (63.0, 78.4) | 0.754 |
| Emergency room stay, h | 880 | 1.7 (0.9, 5.2) | 1.6 (0.6, 3.7) | 1.8 (1.0, 5.4) | 0.017 |
| Death in emergency room | 871 | 2 (0.2) | 0 (0.0) | 2 (0.3) | 0.604 |
| Predictor | OR (95% CI) | p Value |
|---|---|---|
| Male | 0.75 (0.49–1.15) | 0.185 |
| Age, year | 1.00 (0.99–1.02) | 0.773 |
| Coronary heart disease | 2.36 (1.31–4.25) | 0.004 |
| Diabetes mellitus | 0.73 (0.47–1.15) | 0.177 |
| Emergency room stay, hour | 0.99 (0.97–1.01) | 0.148 |
| Glasgow Coma Scale | 3.01 (0.55–16.46) | 0.204 |
| Readmission within 14 Days | |||||
|---|---|---|---|---|---|
| Variable | Valid N | Total (n = 493) | Yes (n = 30) | No (n = 463) | p Value |
| Male | 493 | 232 (47.1) | 15 (50.0) | 217 (46.9) | 0.739 |
| Age, year | 493 | 59.0 ± 13.4 | 57.8 ± 12.7 | 59.0 ± 13.4 | 0.613 |
| Taiwan triage and acuity scale | 493 | 0.771 | |||
| Level I: Resuscitation | 55 (10.6) | 2 (6.7) | 44 (9.5) | ||
| Level II: Emergency | 149 (28.8) | 6 (20.0) | 134 (28.9) | ||
| Level III: Urgency | 296 (57.1) | 21 (70.0) | 268 (57.9) | ||
| Level IV: Less urgency | 17 (3.3) | 1 (3.3) | 16 (3.5) | ||
| Level V: Non urgency | 1 (0.2) | 0 (0.0) | 1 (0.2) | ||
| Glasgow Coma Scale | 493 | 14.48 ± 1.66 | 14.37 ± 2.01 | 14.48 ± 1.64 | 0.709 |
| Eye opening | 488 | 3.95 ± 0.32 | 3.90 ± 0.55 | 3.95 ± 0.30 | 0.365 |
| Verbal response | 489 | 4.78 ± 0.73 | 4.63 ± 1.03 | 4.79 ± 0.70 | 0.411 |
| Motor response | 489 | 5.89 ± 0.47 | 5.73 ± 0.98 | 5.90 ± 0.41 | 0.369 |
| Comorbidity | |||||
| Coronary heart disease | 493 | 40 (8.1) | 3 (10.0) | 37 (8.0) | 0.696 |
| Hypertension | 493 | 479 (97.2) | 30 (100.0) | 449 (97.0) | 0.334 |
| Diabetes mellitus | 493 | 228 (46.2) | 15 (50.0) | 213 (46.0) | 0.671 |
| Stroke | 493 | 102 (20.7) | 5 (16.7) | 97 (21.0) | 0.575 |
| Chronic obstruction pulmonary disease | 493 | 74 (15.0) | 5 (16.7) | 69 (14.9) | 0.793 |
| Peripheral arterial disease | 493 | 56 (11.4) | 3 (10.0) | 53 (11.4) | 0.809 |
| Hyperkalemia | 493 | 143 (29.0) | 9 (30.0) | 134 (28.9) | 0.901 |
| Acute pulmonary edema | 493 | 62 (12.6) | 1 (3.3) | 61 (13.2) | 0.115 |
| Acidosis | 493 | 53 (10.8) | 1 (3.3) | 52 (11.2) | 0.176 |
| Heart failure | 493 | 87 (17.6) | 4 (13.3) | 83 (17.9) | 0.522 |
| Vital signs | |||||
| Systolic blood pressure, mmHg | 492 | 144.2 ± 34.9 | 146 ± 31 | 144.1 ± 35.2 | 0.740 |
| Diastolic blood pressure, mmHg | 492 | 80.5 ± 17.2 | 84.0 ± 13 | 80.3 ± 17.5 | 0.150 |
| Body temperature, °C | 493 | 36.8 ± 0.9 | 36.7 ± 0.8 | 36.8 ± 0.9 | 0.547 |
| Heart rate, beat/min | 492 | 86.9 ± 16.8 | 89.9 ± 15.4 | 86.7 ± 16.9 | 0.310 |
| Respiratory rate, beat/min | 373 | 21.4 ± 7.2 | 20.0 ± 1.0 | 21.4 ± 7.5 | 0.492 |
| Peritonitis | 493 | 159 (32.3) | 13 (43.3) | 146 (31.5) | 0.180 |
| Lab data | |||||
| Leukocyte, 1000/μL | 485 | 9.6 (6.6, 13.0) | 9.3 (7.0, 12.5) | 9.6 (6.5, 13.0) | 0.788 |
| Hemoglobin, g/dL | 483 | 9.6 (8.4, 10.8) | 9.3 (8.3, 10.3) | 9.6 (8.4, 10.8) | 0.377 |
| Alanine aminotransferase, U/L | 415 | 20 (14, 32) | 14 (8, 26) | 21 (14, 32) | 0.016 |
| Albumin, g/dL | 179 | 2.9 (2.3, 3.4) | 2.6 (2.1, 3.1) | 2.9 (2.4, 3.4) | 0.161 |
| BUN, mg/dL | 306 | 57.2 (35.2, 77.3) | 40.1 (30.5, 87.0) | 57.9 (37.0, 77.3) | 0.369 |
| Creatinine, mg/dL | 312 | 8.8 (6.4, 11.2) | 7.0 (3.4, 9.5) | 8.9 (6.5, 11.7) | 0.025 |
| Sodium, mg/dL | 470 | 133 (130, 136) | 134 (131, 136) | 133 (130, 136) | 0.465 |
| Potassium, mg/dL | 472 | 3.5 (2.9, 4.2) | 3.8 (3.4, 4.4) | 3.5 (2.9, 4.2) | 0.061 |
| C-reactive protein, mg/dL | 233 | 40.7 (13.4, 96.2) | 53.0 (34.3, 68.9) | 39.3 (12.7, 100.8) | 0.194 |
| Calcium, mg/dL | 266 | 9.3 (8.5, 10.0) | 9.1 (8.3, 10.0) | 9.3 (8.5, 10.0) | 0.638 |
| Phosphates, mg/dL | 240 | 4.2 (3.1, 5.3) | 3.3 (2.9, 4.6) | 4.3 (3.1, 5.3) | 0.310 |
| Platelet, 1000/μL | 481 | 200 (154, 253) | 215 (149, 289) | 200 (155, 252) | 0.520 |
| Neutrophil, % | 480 | 78.7 (70.2, 85.0) | 83.0 (75.7, 85.0) | 78.5 (70.0, 85.0) | 0.088 |
| Admission days | 493 | 6.9 (4.0, 13.9) | 10.2 (6.7, 15.8) | 6.8 (4.0, 13.9) | 0.146 |
| Transferred to ICU | 493 | 49 (9.9) | 3 (10.0) | 46 (9.9) | 0.991 |
| Removal of PD catheter during hospitalization | 493 | 28 (5.7) | 3 (10.0) | 25 (5.4) | 0.291 |
| Medical expenditure, ×103 NTD | 444 | 30.4 (15.3, 82.4) | 59.4 (34.6, 118.8) | 29.0 (15.0, 80.5) | 0.828 |
| Predictor | OR (95% CI) | p Value |
|---|---|---|
| Male | 0.67 (0.22–2.07) | 0.487 |
| Age, year | 0.99 (0.95–1.03) | 0.608 |
| Diabetes mellitus | 1.22 (0.39–3.81) | 0.737 |
| Alanine aminotransferase, U/L | 0.96 (0.93–1.01) | 0.083 |
| Creatinine, mg/dL | 0.89 (0.77–1.02) | 0.099 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, S.-J.; Liu, C.-C.; Tsai, D.M.T.; Shih, Y.-H.; Lin, C.-L.; Hsu, Y.-C. Prediction Models Using Decision Tree and Logistic Regression Method for Predicting Hospital Revisits in Peritoneal Dialysis Patients. Diagnostics 2024, 14, 620. https://doi.org/10.3390/diagnostics14060620
Lin S-J, Liu C-C, Tsai DMT, Shih Y-H, Lin C-L, Hsu Y-C. Prediction Models Using Decision Tree and Logistic Regression Method for Predicting Hospital Revisits in Peritoneal Dialysis Patients. Diagnostics. 2024; 14(6):620. https://doi.org/10.3390/diagnostics14060620
Chicago/Turabian StyleLin, Shih-Jiun, Cheng-Chi Liu, David Ming Then Tsai, Ya-Hsueh Shih, Chun-Liang Lin, and Yung-Chien Hsu. 2024. "Prediction Models Using Decision Tree and Logistic Regression Method for Predicting Hospital Revisits in Peritoneal Dialysis Patients" Diagnostics 14, no. 6: 620. https://doi.org/10.3390/diagnostics14060620
APA StyleLin, S.-J., Liu, C.-C., Tsai, D. M. T., Shih, Y.-H., Lin, C.-L., & Hsu, Y.-C. (2024). Prediction Models Using Decision Tree and Logistic Regression Method for Predicting Hospital Revisits in Peritoneal Dialysis Patients. Diagnostics, 14(6), 620. https://doi.org/10.3390/diagnostics14060620






