Abnormal Static Sagittal Cervical Curvatures following Motor Vehicle Collisions: A Retrospective Case Series of 41 Patients before and after a Crash Exposure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Data Collection
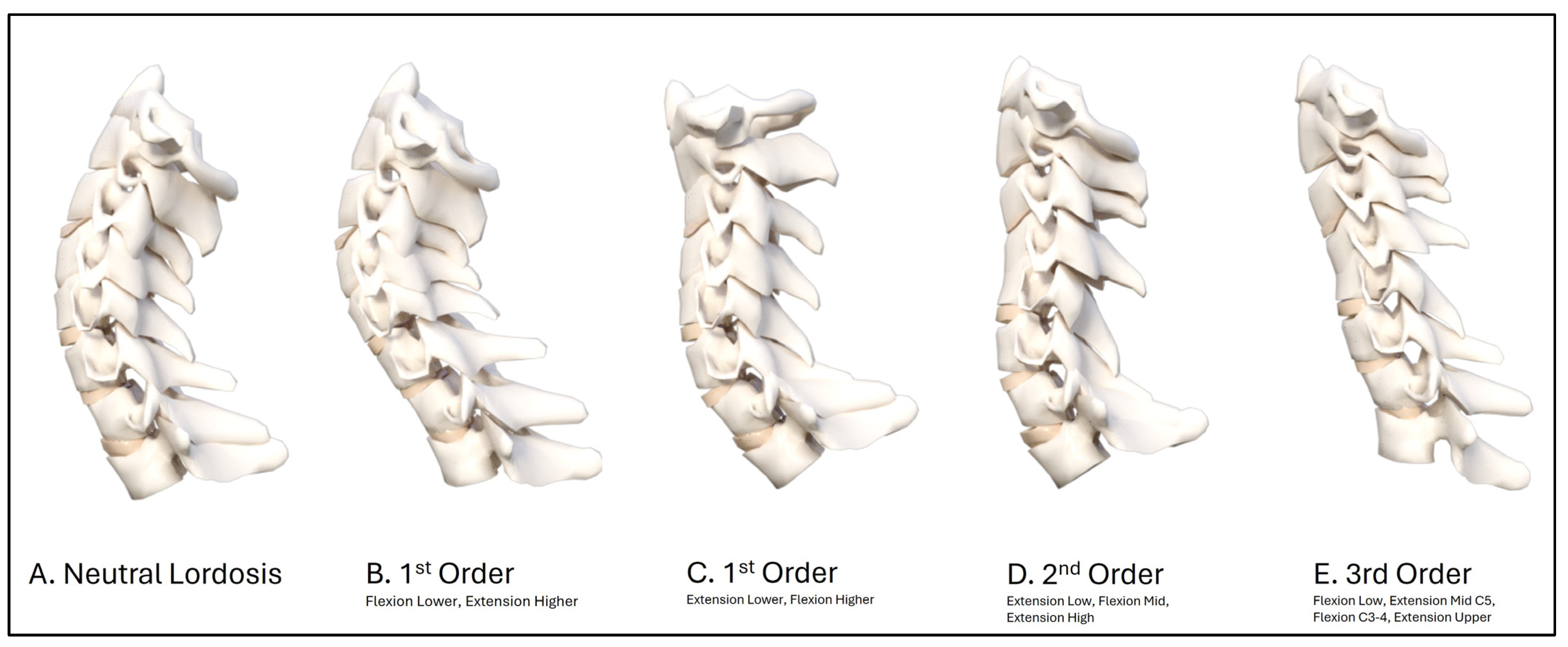
2.2. Cervical Circular and Elliptical Modeling
2.3. Radiographic Procedures and Variables
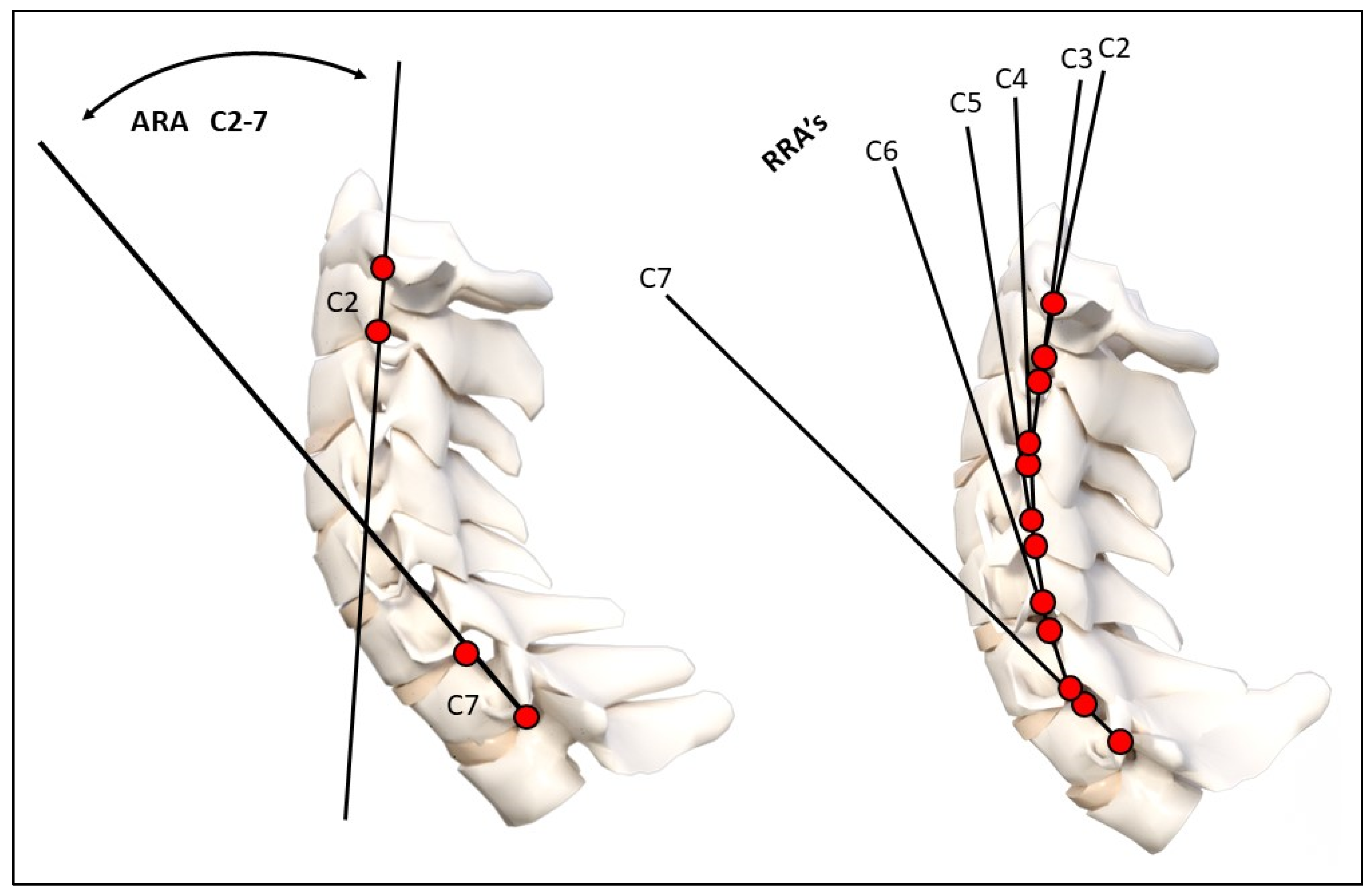
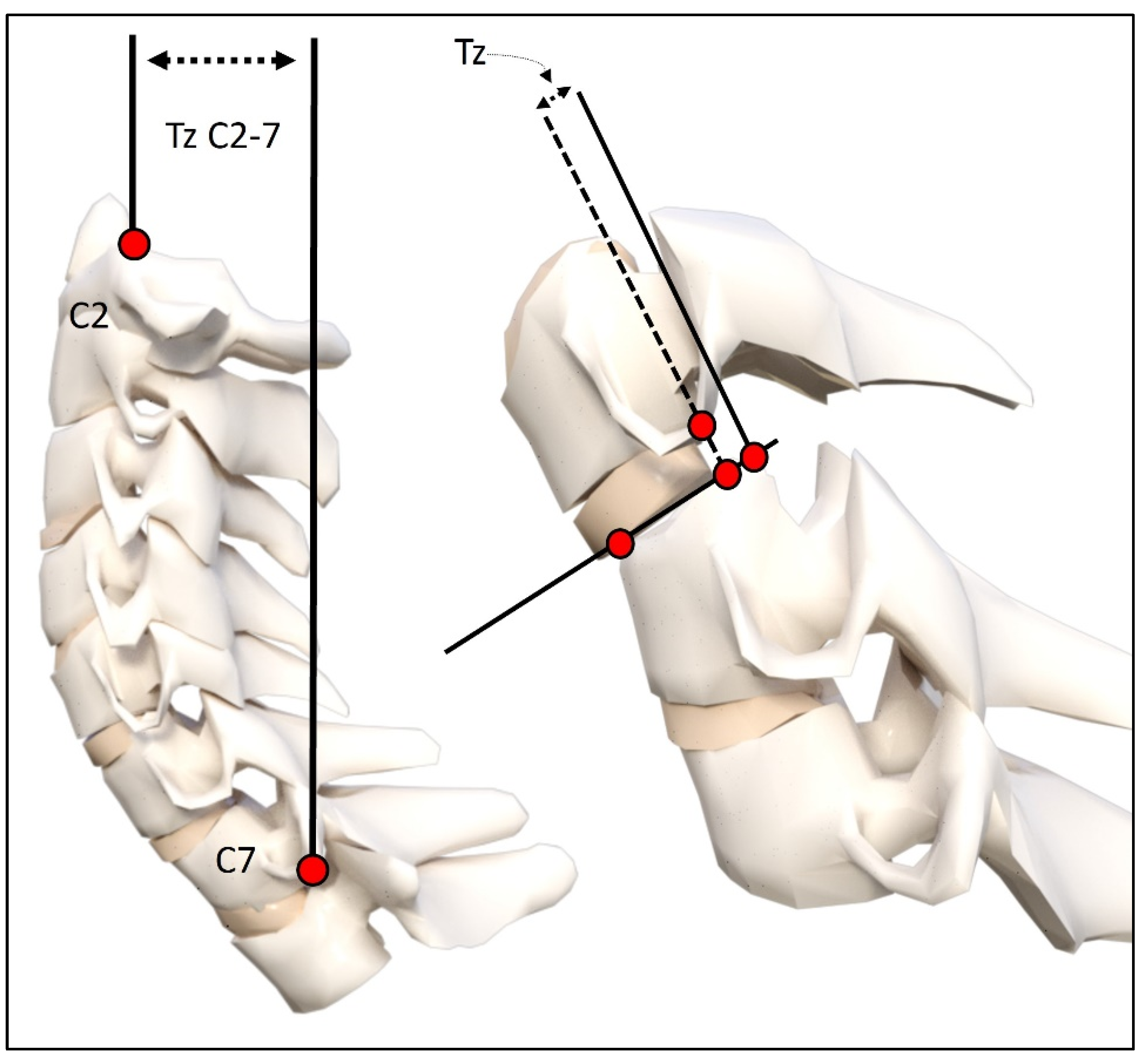
Cervical Spine Radiographic Measurement Variables
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics
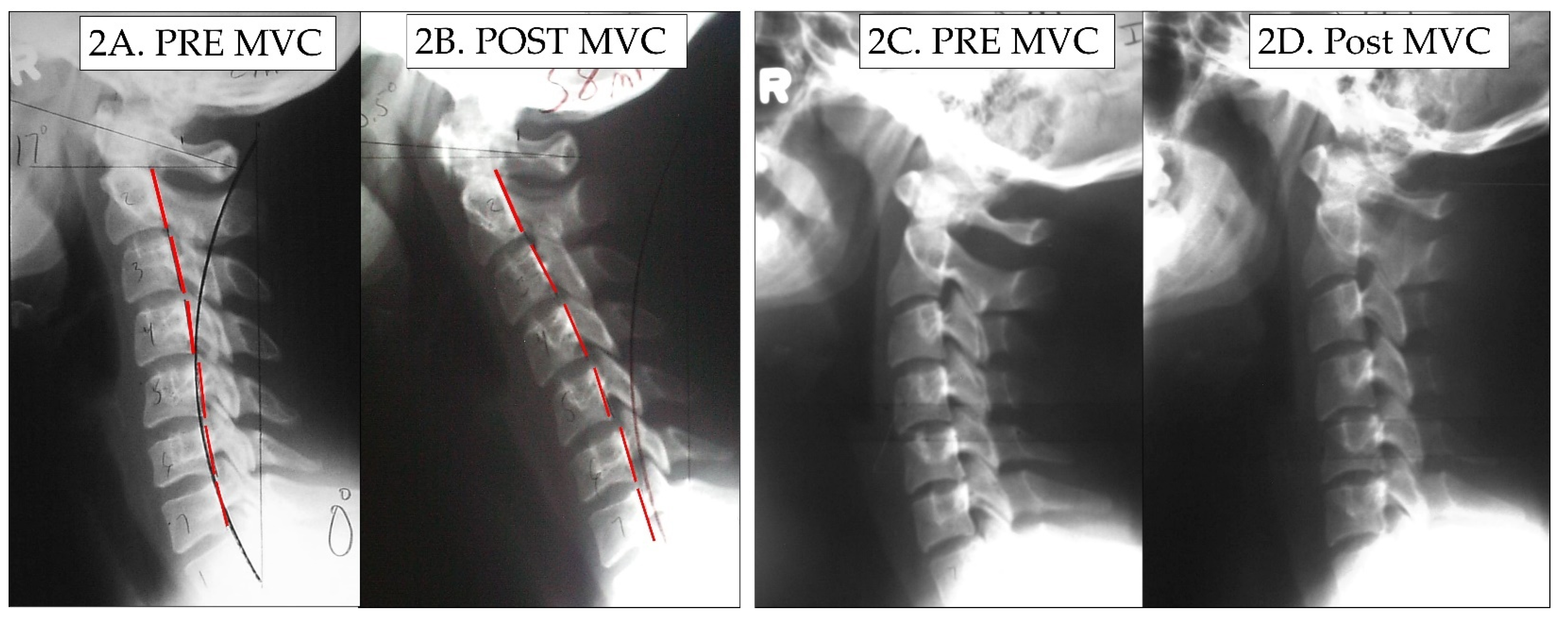
3.2. Change in Cervical Curvature from MVC
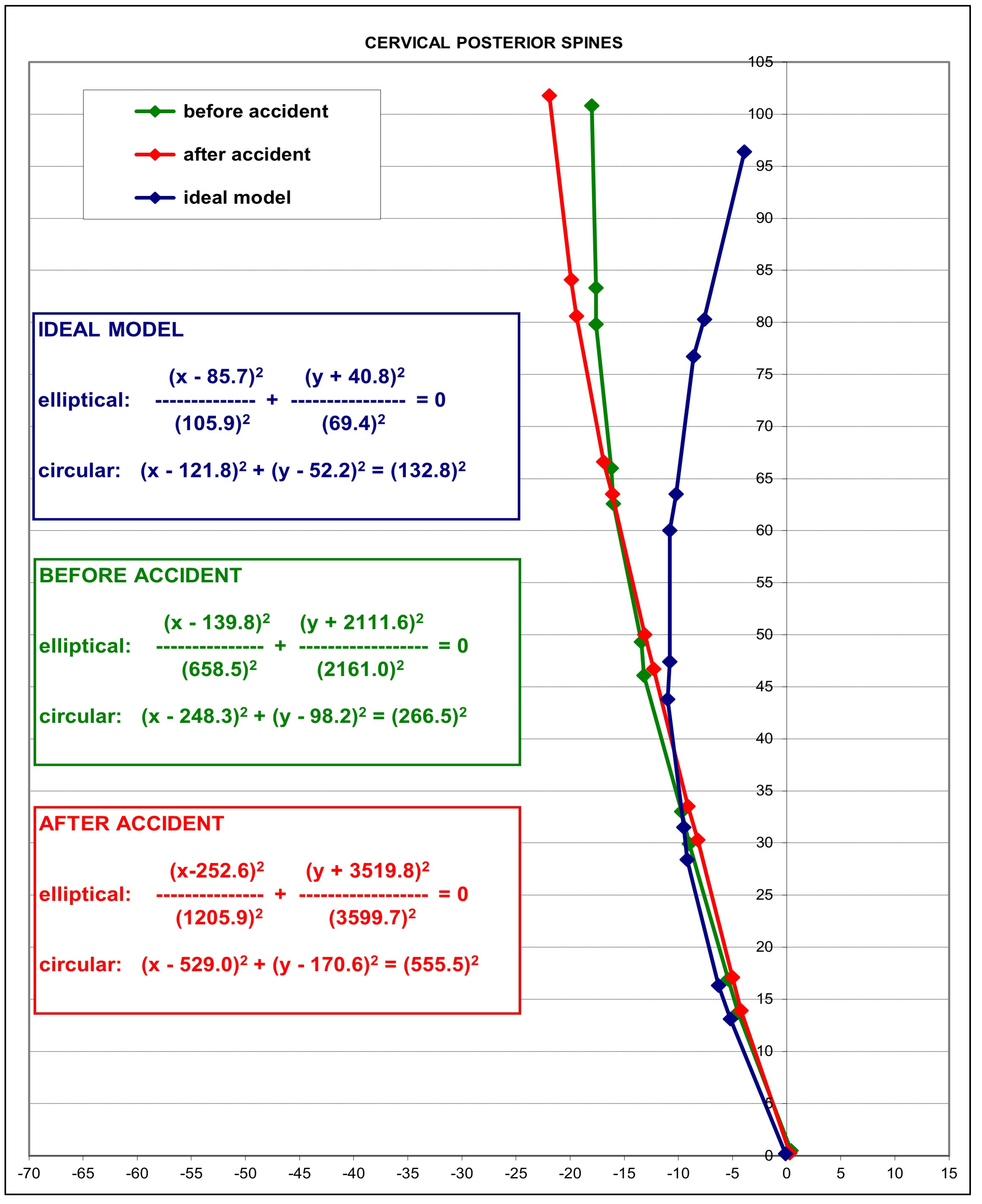
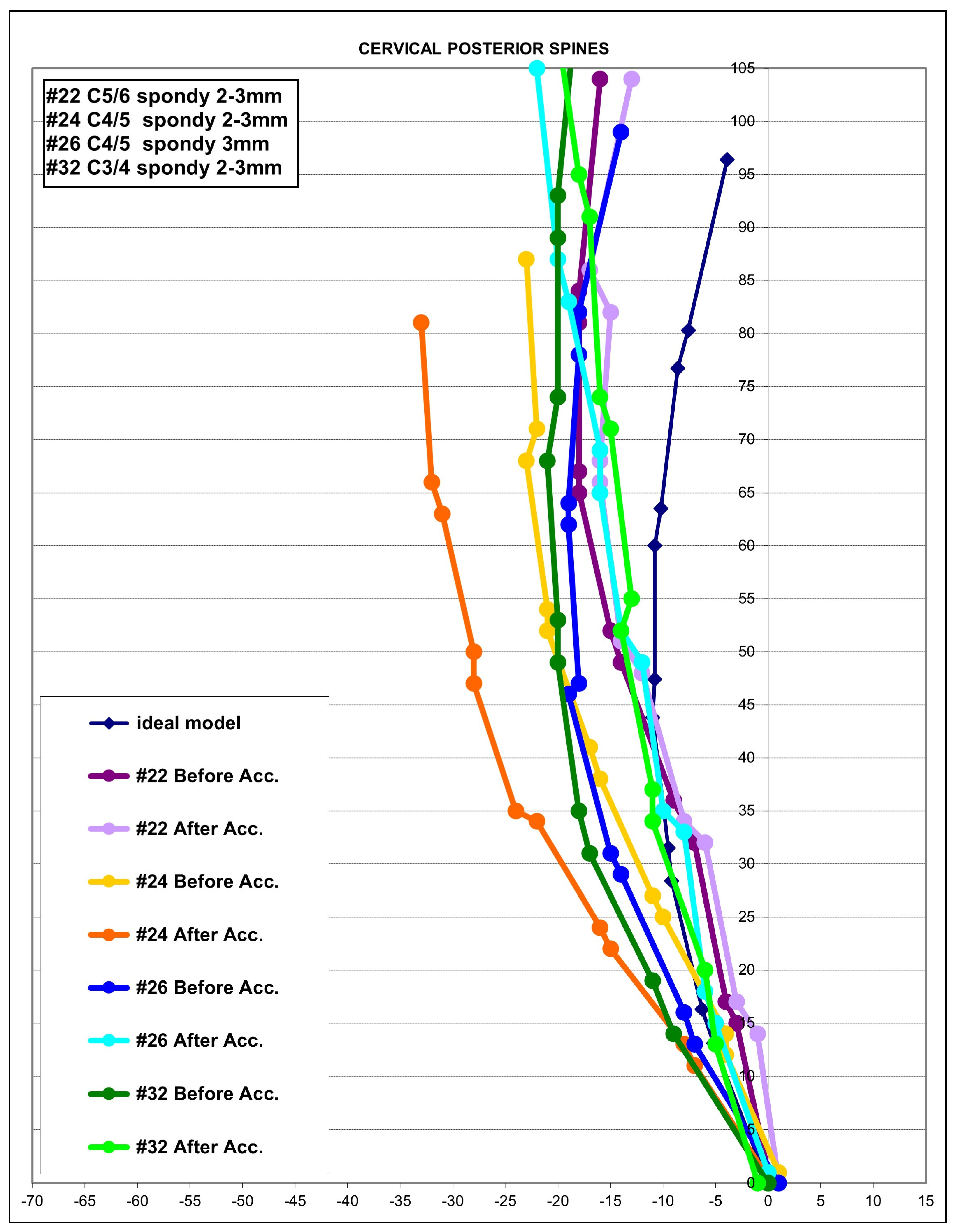
3.3. Modeling Results
4. Discussion
4.1. Loss of Lordosis in MVC Populations
4.2. Altered Sagittal Cervical Geometry as a Buckling Type Alignment
4.3. Pain Increase Post-MVC and Clinical Consideration
4.4. Safety of Radiography for MVC Patients
4.5. Study Limitations and Future Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Quinlan, K.P.; Annest, J.L.; Myers, B.; Ryan, G.; Hill, H. Neck strains and sprains among motor vehicle occupants-United States, 2000. Accid. Anal. Prev. 2004, 36, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Curatolo, M.; Bogduk, N.; Ivancic, P.C.; McLean, S.A.; Siegmund, G.P.; Winkelstein, B.A. The role of tissue damage in whiplash-associated disorders: Discussion paper 1. Spine 2011, 36 (Suppl. S25), S309–S315. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, E.J.; Scholten-Peeters, G.G.; Van der Windt, D.A.; Neeleman-van der Steen, C.W.; Oostendorp, R.A.; Verhagen, A.P. Prognostic factors for a poor recovery in acute whiplash patients. Pain 2005, 114, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; Jull, G.; Kenardy, J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain 2006, 122, 102–108. [Google Scholar] [CrossRef]
- Rebbeck, T.; Sindhusake, D.; Cameron, I.D.; Rubin, G.; Feyer, A.M.; Walsh, J.; Gold, M.; Schofield, W.N. A prospective cohort study of health outcomes following whiplash associated disorders in an Australian population. Inj. Prev. 2006, 12, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Fundaun, J.; Kolski, M.; Baskozos, G.; Dilley, A.; Sterling, M.; Schmid, A.B. Nerve pathology and neuropathic pain after whiplash injury: A systematic review and meta-analysis. Pain 2022, 163, e789–e811. [Google Scholar] [CrossRef] [PubMed]
- Braaf, M.M.; Rosne, R.S. Trauma of cervical spine as cause of chronic headache. J. Trauma 1975, 15, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Nagasawa, A.; Sakakibara, T.; Takahashi, A. Roentgenographic findings of the cervical spine in tension-type headache. Headache 1993, 33, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Cuadrado, M.L.; Pareja, J. Forward head posture and neck mobility in chronic tension-type headache: A blinded, controlled study. Cephalalgia 2006, 26, 314–319. [Google Scholar] [CrossRef]
- Vernon, H.; Steiman, I.; Hagino, C. Cervicogenic dysfunction in muscle contraction headache and migraine: A descriptive study. J. Manip. Physiol. Ther. 1992, 15, 418–429. [Google Scholar]
- Ferracini, G.N.; Chaves, T.C.; Dach, F.; Bevilaqua-Grossi, D.; Fernández-De-Las-Peñas, C.; Speciali, J.G. Analysis of the cranio-cervical curvatures in subjects with migraine with and without neck pain. Physiotherapy 2017, 103, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Buell, T.J.; Buchholz, A.L.; Quinn, J.C.; Shaffrey, C.I.; Smith, J.S. Importance of sagittal alignment of the cervical spine in the management of degenerative cervical myelopathy. Neurosurg. Clin. N. Am. 2018, 29, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Shamji, M.F.; Ames, C.P.; Smith, J.S.; Rhee, J.M.; Chapman, J.R.; Fehlings, M.G.M. Myelopathy and spinal deformity: Relevance of spinal alignment in planning surgical intervention for degenerative cervical myelopathy. Spine 2013, 38, S147–S148. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The relationship between forward head posture and neck pain: A systematic review and meta-analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef] [PubMed]
- Casbas, L.; Chauffour, X.; Cau, J.; Bossavy, J.P.; Midy, D.; Baste, J.C.; Barret, A. Post-traumatic thoracic outlet syndromes. Ann. Vasc. Surg. 2005, 19, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, V.; Giuliano, C.; Pinto, F.; Scaglione, M. Soft tissue injury protocol (STIP) using motion MRI for cervical spine trauma assessment. Emerg. Radiol. 2004, 10, 241–245. [Google Scholar] [CrossRef]
- Giuliano, V.; Giuliano, C.; Pinto, F.; Scaglione, M. The use of flexion and extension MR in the evaluation of cervical spine trauma: Initial experience in 100 trauma patients compared with 100 normal subjects. Emerg. Radiol. 2002, 9, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.H.; Watt, I. The prognosis of neck injuries resulting from rear-end vehicle collisions. J. Bone Jt. Surg. Br. 1983, 65, 608–611. [Google Scholar] [CrossRef]
- Zatzkin, H.R.; Kveton, F.W. Evaluation of the cervical spine in whiplash injuries. Radiology 1960, 75, 577–583. [Google Scholar] [CrossRef]
- Hohl, M. Soft-tissue injuries of the neck in automobile accidents. J. Bone Jt. Surg. Am. 1974, 56, 1675–1682. [Google Scholar] [CrossRef]
- Kristjansson, E.; Jonsson, H., Jr. Is the Sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manip. Physiol. Ther. 2002, 25, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R. The positive findings in alleged neck injuries. Am. J. Orthop. Surg. 1964, 30, 178–187. [Google Scholar]
- Griffiths, H.J.; Olson, P.N.; Everson, L.I.; Winemiller, M. Hyperextension strain or “whiplash” injuries to the cervical spine. Skelet. Radiol. 1995, 24, 263–266. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Camacho, D.L.; Armstrong, A.J.; Robinette, J.J.; Myers, B.S. Inertial properties and loading rates affect buckling modes and injury mechanisms in the cervical spine. J. Biomech. 2000, 33, 191–197. [Google Scholar] [CrossRef]
- Chen, W.F.; Lui, E.M. Structural Instability: Theory and Implementation; Elsevier: New York, NY, USA, 1987; pp. 4–10. [Google Scholar]
- Yoganandan, N.; Pintar, F.A.; Arnold, P.; Reinartz, J.; Cusick, J.F.; Maiman, D.J.; Sances, A. Continuous motion analysis of the head-neck complex under impact. J. Spinal Disord. 1994, 7, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, R.W.; McElhaney, J.H.; Richardson, W.J.; Myers, B.S. Dynamic responses of the head and cervical spine axial impact loading. J. Biomech. 1996, 29, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, R.W.; McElhaney, J.H.; Richardson, W.J.; Best, T.M.; Myers, B.S. Experimental impact injury to the cervical spine: Relating motion of the head and the mechanism of injury. J. Bone Jt. Surg. Am. 1996, 78, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, M.; Kaneoka, K.; Ono, K.; Sakane, M.; Ujihashi, S.; Ochiai, N. Neck injury mechanisms during direct face impact. Spine 2006, 31, 903–908. [Google Scholar] [CrossRef]
- Garcia, T.; Ravani, B. A biomechanical evaluation of whiplash using a multi-body dynamic model. J. Biomech. Eng. 2003, 125, 254–265. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M.; Pearson, A.M.; Ito, S.; Ivancic, P.C.; Wang, J.L. Cervical spine curvature during simulated whiplash. Clin. Biom. 2004, 19, 1–9. [Google Scholar] [CrossRef]
- Wang, Y.; Jiang, H.; Teo, E.C.; Gu, Y. Finite Element Analysis of Head–Neck Kinematics in Rear-End Impact Conditions with Headrest. Bioengineering 2023, 10, 1059. [Google Scholar] [CrossRef] [PubMed]
- Stemper, B.D.; Yoganandan, N.; Pintar, F.A. Effects of abnormal posture on capsular ligament elongations in a computational model subjected to whiplash loading. J. Biomech. 2005, 38, 1313–1323. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Sakou, T.; Sunahara, N.; Oonishi, T.; Maeda, S.; Nakanisi, K. Biomechanical analysis of buckling alignment of the cervical spine. Spine 1997, 22, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Lundeberg, T.; Lund, I.; Dahlin, L.; Borg, E.; Gustafsson, C.; Sandin, L.; Rosén, A.; Kowalski, J.; Eriksson, S.V. Reliability and responsiveness of three different pain assessments. J. Rehabil. Med. 2001, 33, 279–283. [Google Scholar] [CrossRef]
- Bijur, P.E.; Latimer, C.T.; Gallagher, E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad. Emerg. Med. 2003, 10, 390–392. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement properties of the neck disability index: A systematic review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef]
- Harrison, D.D.; Harrison, D.E.; Janik, T.J.; Cailliet, R.; Haas, J.W.; Ferrantelli, J.; Holland, B. Modeling of the Sagittal Cervical Spine as a Method to Discriminate Hypo-Lordosis: Results of Elliptical and Circular Modeling in 72 Asymptomatic Subjects, 52 Acute Neck Pain Subjects, and 70 Chronic Neck Pain Subjects. Spine 2004, 29, 2485–2492. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Colloca, C.J.; Betz, J.; Janik, T.J.; Holland, B. Repeatability of Posture Overtime, X-ray Positioning, and X-ray Line Drawing: An Analysis of Six Control Groups. J. Manip. Physiol. Ther. 2003, 26, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Cailliet, R.; Troyanovich, S.J.; Janik, T.J.; Holland, B. Cobb Method or Harrison Posterior Tangent Method: Which is Better for Lateral Cervical Analysis? Spine 2000, 25, 2072–2078. [Google Scholar] [CrossRef]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef]
- Marshall, D.L. Correlation of cervical lordosis measurement with incidence of motor vehicle accidents. J Aust. Chiropr. Osteopat. 1996, 5, 79–85. [Google Scholar]
- Matsumoto, M.; Fujimura, Y.; Suzuki, N.; Toyama, Y.; Shiga, H. Cervical curvature in acute whiplash injuries: Prospective comparative study with asymptomatic subjects. Injury 1998, 29, 775–778. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.P.; Baann Liane, M.S.; Bendix, T.; Kasch, H.; Kongsted, A. Does cervical kyphosis relate to symptoms following whiplash injury? Man. Ther. 2011, 16, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Beltsios, M.; Savvidou, O.; Mitsiokapa, E.A.; Mavrogenis, A.F.; Kaspiris, A.; Efstathopoulos, N.; Papagelopoulos, P.J. Sagittal alignment of the cervical spine after neck injury. Eur. J. Orthop. Surg. Traumatol. 2013, 23 (Suppl. S1), S47–S51. [Google Scholar] [CrossRef] [PubMed]
- Linsenmaier, U.; Deak, Z.; Krtakovska, A.; Ruschi, F.; Kammer, N.; Wirth, S.; Reiser, M.; Geyer, L. Emergency radiology: Straightening of the cervical spine in MDCT after trauma—A sign of injury or normal variant? Br. J. Radiol. 2016, 89, 20150996. [Google Scholar] [CrossRef] [PubMed]
- Stemper, B.D.; Pintar, F.A.; Rao, R.D. The influence of morphology on cervical injury characteristics. Spine 2011, 36 (Suppl. S25), S180–S186. [Google Scholar] [CrossRef] [PubMed]
- Frechede, B.; Bertholon, N.; Saillant, G.; Lavaste, F.; WSkalli, W. Finite element model of the human neck during omni-directional impacts. Part II: Relation between cervical curvature and risk of injury. Comput. Methods Biomech. Biomed. Eng. 2006, 9, 379–386. [Google Scholar] [CrossRef]
- Fréchède, B.; Bertholon, N.; Le Coz, J.Y.; Lavaste, F.; Skalli, W. Finite element model of the human neck during omni-directional impacts. Rev. Eur. Des Éléments 2005, 14, 463–485. [Google Scholar] [CrossRef]
- Ogura, Y.; Dimar, J.R.; Djurasovic, M.; Carreon, L.Y. Etiology and treatment of cervical kyphosis: State of the art review-a narrative review. J. Spine Surg. 2021, 7, 422–433. [Google Scholar] [CrossRef]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring cervical lordosis by cervical extension traction methods in the treatment of cervical spine disorders: A systematic review of controlled trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Efficacy of Cervical Lordosis Rehabilitation for Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial with 2-Year Follow-Up. J. Clin. Med. 2022, 11, 6515. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, R. Catastrophe Theory for Scientists and Engineers; Dover Publications: New York, NY, USA, 1981. [Google Scholar]
- Pilkey, W.D.; Wunderlich, W. Mechanics of Structures: Variational and Computational Method; CRC Press: Boca Raton, FL, USA, 1994; pp. 617–635. [Google Scholar] [CrossRef]
- Juhl, J.H.; Miller, S.M.; Roberts, G.W. Roentgenographic variations in the normal cervical spine. Radiology 1962, 78, 591–597. [Google Scholar] [CrossRef]
- Clark, W.M.; Gehweiler, J.A.; Laib, R. Twelve signs of cervical spine trauma. Skeletal Radiol. 1979, 3, 201–205. [Google Scholar] [CrossRef]
- Gehweiler, J.A.; Clark, W.M.; Schaaf, R.E.; Powers, B.; Miller, M.D. Cervical spine trauma: The common combined conditions. Radiology 1979, 130, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Kettner, N.W.; Guebert, G.M. The radiology of cervical spine injury. J. Manip. Physiol. Ther. 1991, 14, 518–526. [Google Scholar]
- Rechtman, A.M.; Borden, A.G.; Gershon-Cohen, J. The lordotic curve of the cervical spine. Clin. Orthop. 1961, 20, 208–216. [Google Scholar]
- Helliwell, P.S.; Evans, P.F.; Wright, V. The straight cervical spine: Does it indicate muscle spasm? J. Bone Jt. Surg. 1994, 76, 103–106. [Google Scholar] [CrossRef]
- Fedorchuk, C.A.; McCoy, M.; Lightstone, D.F.; Bak, D.A.; Moser, J.; Kubricht, B.; Packer, J.; Walton, D.; Binongo, J. Impact of Isometric Contraction of Anterior Cervical Muscles on Cervical Lordosis. J. Radiol. Case Rep. 2016, 10, 13–25. [Google Scholar] [CrossRef]
- Nightingale, R.W.; Sganga, J.; Cutcliffe, H.; Bass, C.R. Impact responses of the cervical spine: A computational study of the effects of muscle activity, torso constraint, and pre-flexion. J. Biomech. 2016, 49, 558–564. [Google Scholar] [CrossRef] [PubMed]
- McAviney, J.; Schulz, D.; Bock, R.; Harrison, D.E.; Holland, B. Determining the relationship between cervical lordosis and neck complaints. J. Manip. Physiol. Ther. 2005, 28, 187–193. [Google Scholar] [CrossRef]
- Fejer, R.; Jordan, A.; Hartvigsen, J. Categorizing the severity of neck pain: Establishment of cut-points for use in clinical and epidemiological research. Pain 2005, 119, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Shin, J.I.; Koyanagi, A.; Jacob, L.; Smith, L.; Lee, H.; Chang, Y.; Song, T.J. Global, regional, and national neck pain burden in the general population, 1990-2019: An analysis of the global burden of disease study 2019. Front. Neurol. 2022, 13, 955367. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; Aris, I.M.; Snyder, B.D.; Harris, M.B.; Kang, J.D.; Murray, M.; Rodriguez, E.K.; Nazarian, A. Musculoskeletal health: An ecological study assessing disease burden and research funding. Lancet Reg. Health Am. 2024, 29, 100661. [Google Scholar] [CrossRef] [PubMed]
- Werndle, M.C.; Myers, J.; Mortimer, A. Missed cervical spine injuries: Aim for the top. Emerg Radiol. 2022, 29, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Preuss, C.V.; Kalava, A.; King, K.C. Prescription of Controlled Substances: Benefits and Risks. [Updated 2023 Apr 29]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537318/ (accessed on 13 February 2024).
- Beaudoin, F.L.; Gutman, R.; Merchant, R.C.; Clark, M.A.; Swor, R.A.; Jones, J.S.; Lee, D.C.; Peak, D.A.; Domeier, R.M.; Rathlev, N.K.; et al. Persistent pain after motor vehicle collision: Comparative effectiveness of opioids vs nonsteroidal antiinflammatory drugs prescribed from the emergency department-a propensity matched analysis. Pain 2017, 158, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, E.J.; Agathokleous, E.; Giordano, J.; Selby, P.B. Manhattan Project genetic studies: Flawed research discredits LNT recommendations. Environ. Pollut. 2023, 319, 120902. [Google Scholar] [CrossRef]
- Wijetunga, C.; Brady, Z.; Varma, D.K. Responsible use of advanced imaging technology. How well are risks and benefits of radiation recognised? Injury 2018, 49, 883–884. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.E. Radiophobia: 7 Reasons Why Radiography Used in Spine and Posture Rehabilitation Should Not Be Feared or Avoided. Dose Response 2018, 16, 1–10. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.E. X-ray Hesitancy: Patients’ Radiophobic Concerns Over Medical X-rays. Dose Response 2020, 18, 1559325820959542. [Google Scholar] [CrossRef]
- Norton, T.C.; Oakley, P.A.; Haas, J.W.; Harrison, D.E. Positive Outcomes Following Cervical Acceleration-Deceleration (CAD) Injury Using Chiropractic BioPhysics® Methods: A Pre-Auto Injury and Post-Auto Injury Case Series. J. Clin. Med. 2023, 12, 6414. [Google Scholar] [CrossRef]
- Gore, D.R. Roentgenographic findings in the cervical spine in asymptomatic persons: A 10 year follow-up. Spine 2001, 26, 2463–2466. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-M.; Song, K.-S.; Park, S.-H.; Kang, H.; Riew, K.D. Does whole-spine lateral radiograph with clavicle positioning reflect the correct cervical sagittal alignment? Eur. Spine J. 2015, 24, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.E.; Harrison, D.D.; Janik, T.J.; Holland, B.; Siskin, L.A. Slight head extension: Does it change the sagittal cervical curve? Eur. Spine J. 2001, 10, 149–153. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD | Location in Vehicle | Collision Type | Pre NRS | Post NRS | Cohen’s d for NRS | p Value * Change |
|---|---|---|---|---|---|---|---|
| Height | 159 ± 43.5 | FD = 28 FP = 10 RP = 3 | Rear = 30 Front = 2 Side = 7 Oblique = 2 | 2.7 ± 2.5 | 5.0 ± 2.4 | 0.939 | p < 0.001 |
| Weight | 65.1 ± 4.5 | Pre NDI ** | Post NDI ** | Cohen’s d for NDI | p Value * Change | ||
| Sex | M = 15 F = 26 | 15.7 ± 15.1 | 32.8 ± 15.4 | 1.121 | p < 0.001 | ||
| Age | 33.9 ± 16.9 8–65 years |
| Variable | Initial Lateral Cervical Radiograph | Post Lateral Cervical Radiograph | Cohen’s d | p Value ** Change | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Maximum Value | Minimum Value | Mean ± SD | Maximum Value | Minimum Value | |||
| Tz C2–C7 (mm) | 19.6 ± 9.8 | 47 | 2 | 22.0 ± 12.5 | 58 | −3 | 0.215 | p < 0.05 |
| Chamberlains (°) | −2.4 ± 6.7 | 12 | −19 | −0.96 ± 6.6 | 14 | −12 | 0.217 | p < 0.05 |
| ARA C2–C7 (°) | −17.1 ± 13.9 | 26 | −45 | −9.52 ± 12.2 | 20 | −29 | 0.581 | p < 0.001 |
| Circular Radii * (mm2) | 265.5 | 555.5 | p < 0.001 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haas, J.W.; Oakley, P.A.; Ferrantelli, J.R.; Katz, E.A.; Moustafa, I.M.; Harrison, D.E. Abnormal Static Sagittal Cervical Curvatures following Motor Vehicle Collisions: A Retrospective Case Series of 41 Patients before and after a Crash Exposure. Diagnostics 2024, 14, 957. https://doi.org/10.3390/diagnostics14090957
Haas JW, Oakley PA, Ferrantelli JR, Katz EA, Moustafa IM, Harrison DE. Abnormal Static Sagittal Cervical Curvatures following Motor Vehicle Collisions: A Retrospective Case Series of 41 Patients before and after a Crash Exposure. Diagnostics. 2024; 14(9):957. https://doi.org/10.3390/diagnostics14090957
Chicago/Turabian StyleHaas, Jason W., Paul A. Oakley, Joseph R. Ferrantelli, Evan A. Katz, Ibrahim M. Moustafa, and Deed E. Harrison. 2024. "Abnormal Static Sagittal Cervical Curvatures following Motor Vehicle Collisions: A Retrospective Case Series of 41 Patients before and after a Crash Exposure" Diagnostics 14, no. 9: 957. https://doi.org/10.3390/diagnostics14090957
APA StyleHaas, J. W., Oakley, P. A., Ferrantelli, J. R., Katz, E. A., Moustafa, I. M., & Harrison, D. E. (2024). Abnormal Static Sagittal Cervical Curvatures following Motor Vehicle Collisions: A Retrospective Case Series of 41 Patients before and after a Crash Exposure. Diagnostics, 14(9), 957. https://doi.org/10.3390/diagnostics14090957









