Data from Emergency Medical Service Activities: A Novel Approach to Monitoring COVID-19 and Other Infectious Diseases
Abstract
1. Introduction
2. Materials and Methods
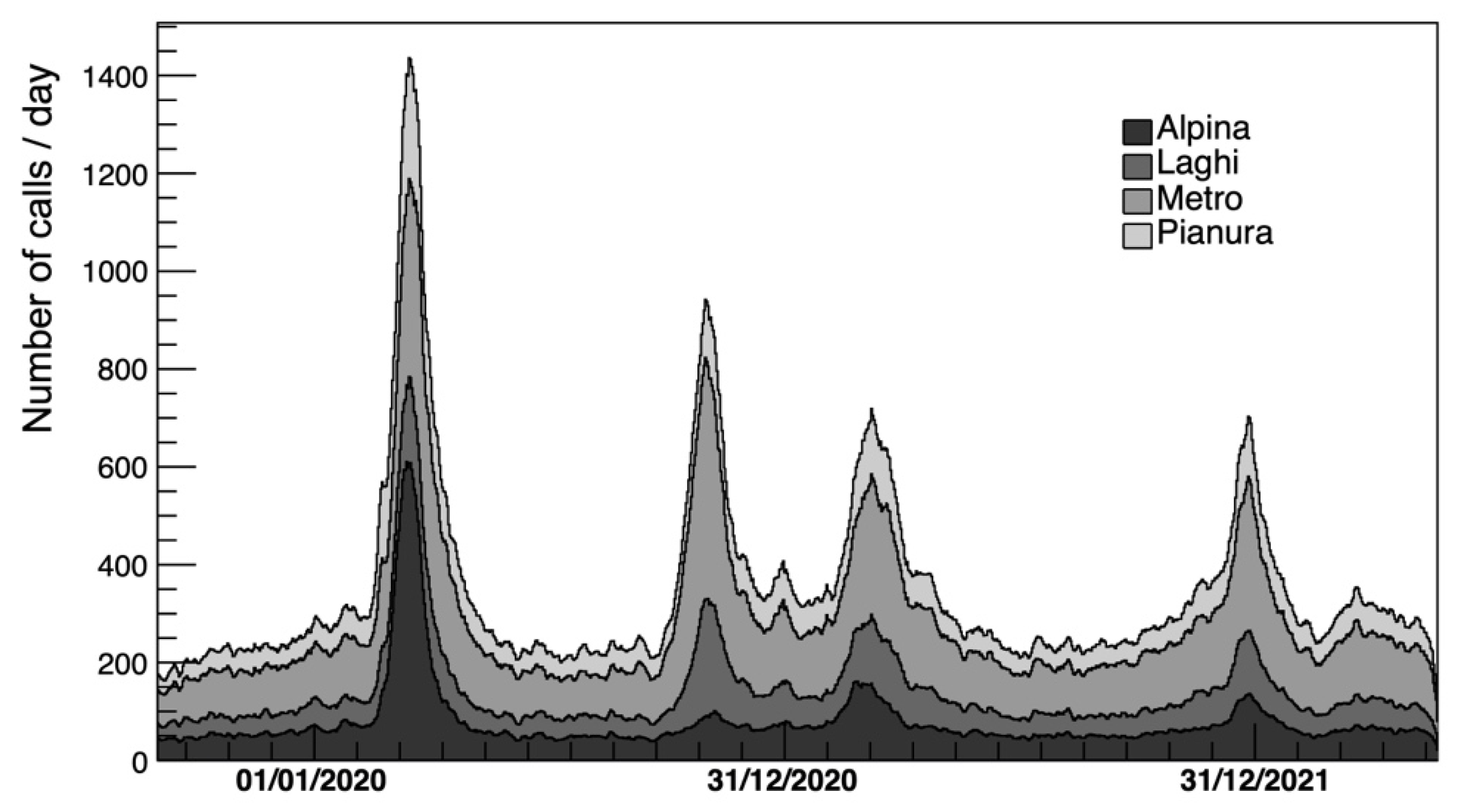
- (1)
- SOREU “Metro” (Metropolitan) in Milan;
- (2)
- SOREU “Laghi” (Lakes) in Como;
- (3)
- SOREU “Alpina” (Alpine) in Bergamo;
- (4)
- SOREU “Pianura” (Plain) in Pavia.
- Issue of the call (e.g., breathing difficulty, chest pain or heart disease, neurological disorder, musculoskeletal disease, intoxication or drug overdose, accidents and other major or minor injuries);
- Age;
- Sex;
- Severity evaluated by the triage classification in loco (ascending scale by gravity: white, green, yellow, red);
- Day of the call;
- Hour of the day of the call;
- Code evaluated by the trauma triage and scoring at the arrival of the patient in the hospital (ascending scale by gravity: white, green, yellow, red, black);
- Time passed between the ambulance’s departure from the hospital and its arrival to the patient location;
- Time passed between the ambulance arrival to the patient location and its return, i.e., its arrival to hospital.
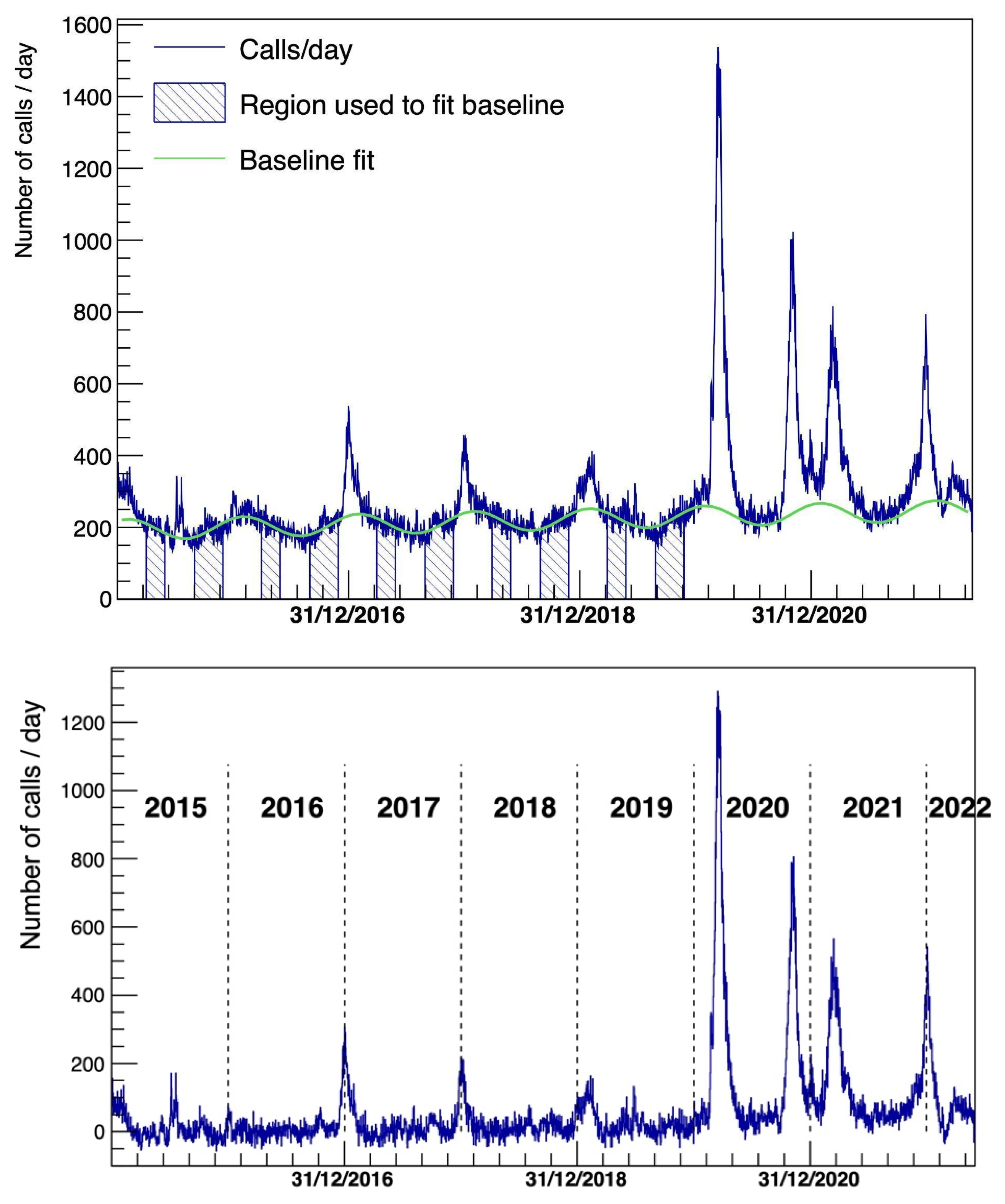
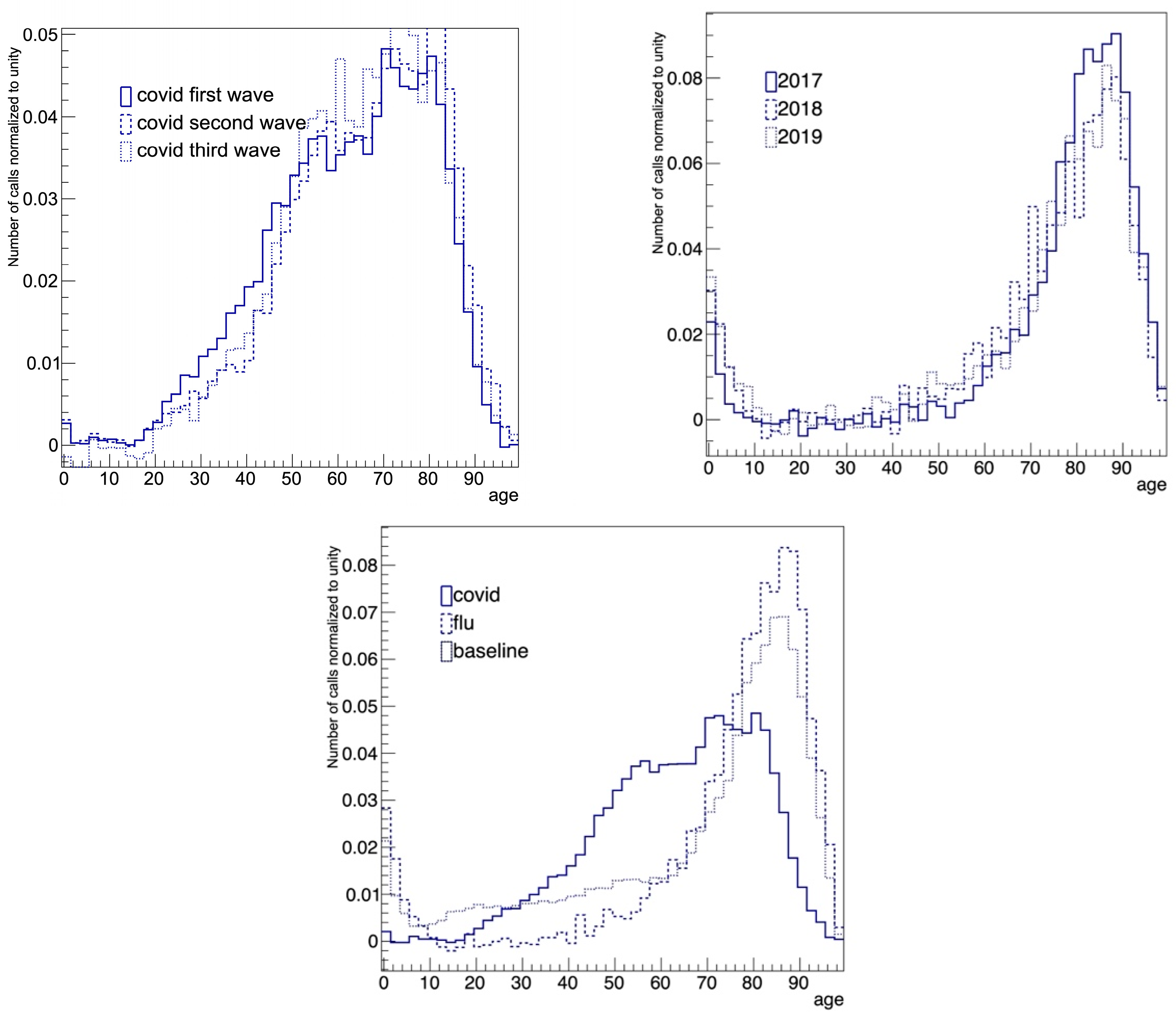
- Period 1: 1 July 2016–11 October 2016 and 10 February 2017–20 May 2017. During this period, looking at the time series, flu contribution should be negligible. This period was used to model the baseline;
- Period 2: 15 December 2016–14 February 2017. Here, the peak related to the 2017 flu was very evident;
- Period 3: 11 March 2020–31 March 2020. In this period, the first COVID-19 wave was dominant.
3. Results
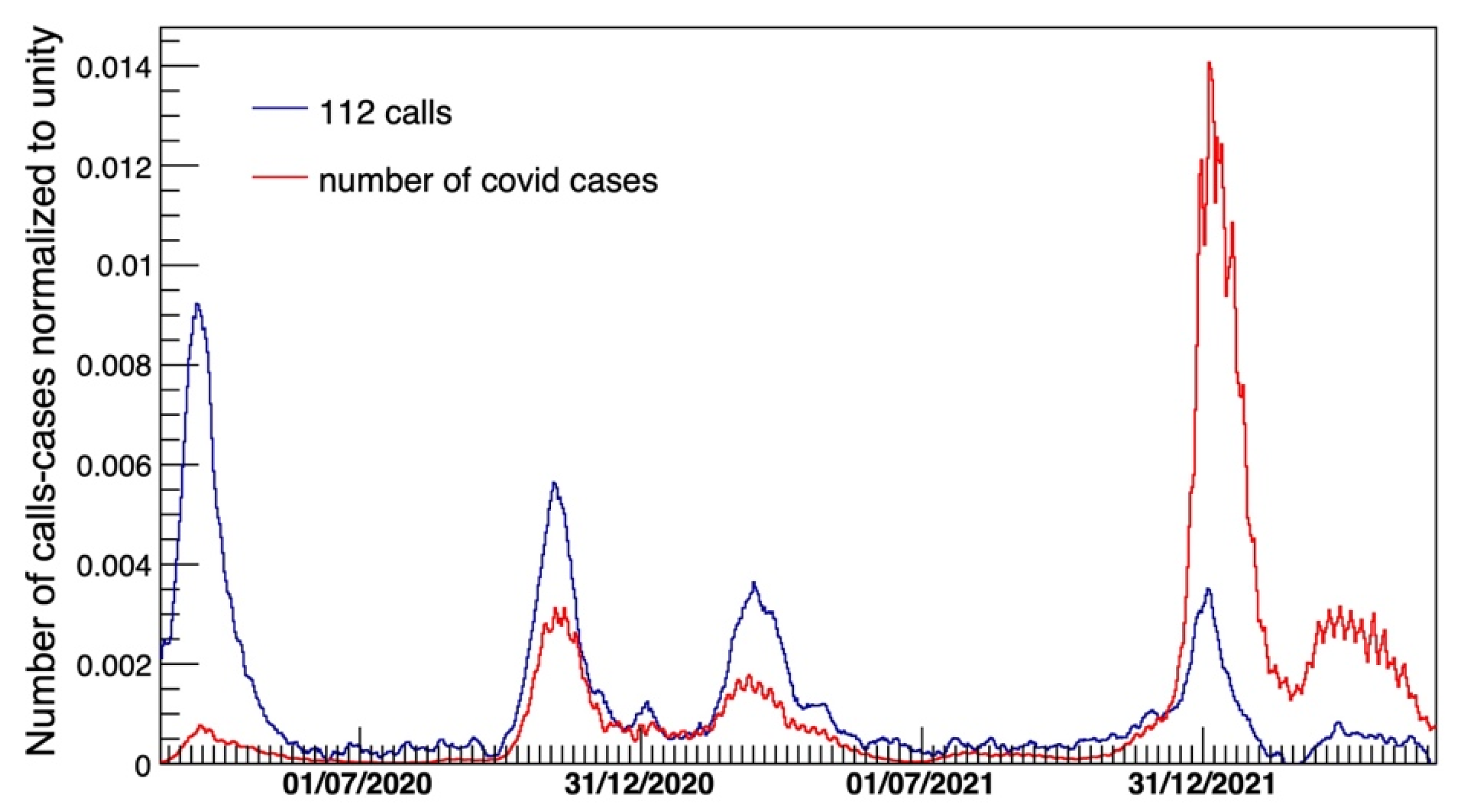
3.1. Analysis of the Time Series and Comparison with Official Data and ISTAT Mortality
3.2. Analysis of the Emergency Medical Services Variables
4. Discussion
- The early detection of any change in incidence of communicable diseases, possibly leading to overcoming the delay between the occurrence of cases and the publication of surveillance bulletins, especially at the beginning of an outbreak.
- The public health monitoring of any big event, such as Jubilee, when many people gather together and the onset of specific health issues may evolve in a very short period, making it difficult to detect them using classical surveillance methods based on swabs or blood testing.
- Governmental analysis and monitoring of both trends in incidence of the health event and pressure on the healthcare system during outbreaks to enhance optimal resource allocation and adaptation of the healthcare services in their response to the threats (e.g., pre-alerting hospitals to a possible increase in emergency case arrivals, adapting the number of hospital beds to respond to the possible increase in patients).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Timeline of WHO’s Response to COVID-19. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 15 September 2024).
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing—5 May 2023. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing---5-may-2023 (accessed on 7 September 2024).
- Feehan, J.; Apostolopoulos, V. Is COVID-19 the Worst Pandemic? Maturitas 2021, 149, 56–58. [Google Scholar] [CrossRef] [PubMed]
- WHO. Dashboard COVID-19. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 30 October 2024).
- Presidenza del Consiglio dei Ministri. Decreto Presidenza Consiglio Dei Ministri Del 9 Marzo 2020; Gazzetta Ufficiale: Rome, Italy, 2020.
- Bezzini, D.; Schiavetti, I.; Manacorda, T.; Franzone, G.; Battaglia, M.A. First Wave of COVID-19 Pandemic in Italy: Data and Evidence. In Coronavirus Therapeutics—Volume II. Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2021; pp. 91–113. [Google Scholar]
- Porcu, G.; Chen, Y.X.; Bonaugurio, A.S.; Villa, S.; Riva, L.; Messina, V.; Bagarella, G.; Maistrello, M.; Leoni, O.; Cereda, D.; et al. Web-Based Surveillance of Respiratory Infection Outbreaks: Retrospective Analysis of Italian COVID-19 Epidemic Waves Using Google Trends. Front. Public Health 2023, 11, 1141688. [Google Scholar] [CrossRef] [PubMed]
- García-Basteiro, A.L.; Chaccour, C.; Guinovart, C.; Llupià, A.; Brew, J.; Trilla, A.; Plasencia, A. Monitoring the COVID-19 Epidemic in the Context of Widespread Local Transmission. Lancet Respir. Med. 2020, 8, 440–442. [Google Scholar] [CrossRef]
- Mazick, A. Workshop on mortality monitoring in Europe Monitoring Excess Mortality for Public Health Action: Potential for a Future European Network. Eurosurveillance 2007, 12, E070104.1. [Google Scholar] [PubMed]
- Nielsen, J.; Krause, T.G.; Mølbak, K. Influenza-associated Mortality Determined from All-cause Mortality, Denmark 2010/11–2016/17: The FluMOMO Model. Influenza Other Respir. Viruses 2018, 12, 591–604. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J.; Vestergaard, L.S.; Richter, L.; Schmid, D.; Bustos, N.; Asikainen, T.; Trebbien, R.; Denissov, G.; Innos, K.; Virtanen, M.J.; et al. European All-Cause Excess and Influenza-Attributable Mortality in the 2017/18 Season: Should the Burden of Influenza B Be Reconsidered? Clin. Microbiol. Infect. 2019, 25, 1266–1276. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, E.; Minelli, G.; Egidi, V.; Jona Lasinio, G. Assessment of Excess Mortality in Italy in 2020–2021 as a Function of Selected Macro-Factors. Int. J. Environ. Res. Public Health 2023, 20, 2812. [Google Scholar] [CrossRef] [PubMed]
- Odone, A.; Delmonte, D.; Gaetti, G.; Signorelli, C. Doubled Mortality Rate during the COVID-19 Pandemic in Italy: Quantifying What Is Not Captured by Surveillance. Public Health 2021, 190, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Michelozzi, P.; de’Donato, F.; Scortichini, M.; Pezzotti, P.; Stafoggia, M.; De Sario, M.; Costa, G.; Noccioli, F.; Riccardo, F.; Bella, A.; et al. Temporal Dynamics in Total Excess Mortality and COVID-19 Deaths in Italian Cities. BMC Public Health 2020, 20, 1238. [Google Scholar] [CrossRef] [PubMed]
- Fior, M.; Mpampatsikos, V. COVID-19 and Estimates of Actual Deaths in Italy. Scenarios for Urban Planning in Lombardy. J. Urban Manag. 2021, 10, 275–301. [Google Scholar] [CrossRef]
- Scortichini, M.; Schneider dos Santos, R.; De’ Donato, F.; De Sario, M.; Michelozzi, P.; Davoli, M.; Masselot, P.; Sera, F.; Gasparrini, A. Excess Mortality during the COVID-19 Outbreak in Italy: A Two-Stage Interrupted Time-Series Analysis. Int. J. Epidemiol. 2021, 49, 1909–1917. [Google Scholar] [CrossRef] [PubMed]
- Kulu, H.; Dorey, P. Infection Rates from COVID-19 in Great Britain by Geographical Units: A Model-Based Estimation from Mortality Data. Health Place 2021, 67, 102460. [Google Scholar] [CrossRef] [PubMed]
- Kontis, V.; Bennett, J.E.; Rashid, T.; Parks, R.M.; Pearson-Stuttard, J.; Guillot, M.; Asaria, P.; Zhou, B.; Battaglini, M.; Corsetti, G.; et al. Magnitude, Demographics and Dynamics of the Effect of the First Wave of the COVID-19 Pandemic on All-Cause Mortality in 21 Industrialized Countries. Nat. Med. 2020, 26, 1919–1928. [Google Scholar] [CrossRef] [PubMed]
- Vanella, P.; Basellini, U.; Lange, B. Assessing Excess Mortality in Times of Pandemics Based on Principal Component Analysis of Weekly Mortality Data—The Case of COVID-19. Genus 2021, 77, 16. [Google Scholar] [CrossRef]
- Modi, C.; Böhm, V.; Ferraro, S.; Stein, G.; Seljak, U. Estimating COVID-19 Mortality in Italy Early in the COVID-19 Pandemic. Nat. Commun. 2021, 12, 2729. [Google Scholar] [CrossRef]
- Gil-Jardiné, C.; Chenais, G.; Pradeau, C.; Tentillier, E.; Revel, P.; Combes, X.; Galinski, M.; Tellier, E.; Lagarde, E. Trends in Reasons for Emergency Calls during the COVID-19 Crisis in the Department of Gironde, France Using Artificial Neural Network for Natural Language Classification. Scand. J. Trauma. Resusc. Emerg. Med. 2021, 29, 55. [Google Scholar] [CrossRef] [PubMed]
- Valent, F.; Licata, S. Emergency Medical Services Calls During Italy’s COVID-19 Lockdown. Ann. Emerg. Med. 2020, 76, 812–814. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, E.; Sonkin, R.; Strugo, R.; Zerath, E. Evolution of Emergency Medical Calls during a Pandemic—An Emergency Medical Service during the COVID-19 Outbreak. Am. J. Emerg. Med. 2021, 43, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Castro Delgado, R.; Delgado Sánchez, R.; Duque Del Río, M.D.C.; Arcos González, P. Potential Capacity of an Emergency Dispatch Center to Predict COVID-19-Related Hospital and Intensive Care Unit Admissions. Emergencias 2021, 33, 368–373. [Google Scholar] [PubMed]
- Scquizzato, T.; Landoni, G.; Ristagno, G.; Pruna, A.; Zangrillo, A. Emergency Calls as an Early Indicator of Intensive Care Unit Demand for Coronavirus Disease 2019. Eur. J. Emerg. Med. 2023, 30, 47–48. [Google Scholar] [CrossRef]
- del Re, D.; Palla, L.; Meridiani, P.; Soffi, L.; Loiudice, M.T.; Antinozzi, M.; Cattaruzza, M.S. The Spread in Time and Space of COVID-19 Pandemic Waves: The Italian Experience from Mortality Data Analyses. Front. Public. Health 2024, 12, 1324033. [Google Scholar] [CrossRef]
- Areu Lombardia—Soreu. Available online: https://www.areu.lombardia.it/web/home/soreu (accessed on 10 July 2024).
- Fagoni, N.; Bellini, L.; Bonora, R.; Botteri, M.; Migliari, M.; Pagliosa, A.; Sechi, G.M.; Signorelli, C.; Zoli, A.; Stirparo, G. Changing the Stroke Network during Pandemic Scenarios Does Not Affect the Management of Patients with a Positive Cincinnati Prehospital Stroke Scale. Neurol. Sci. 2024, 45, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Stirparo, G.; Bellini, L.; Ristagno, G.; Bonora, R.; Pagliosa, A.; Migliari, M.; Andreassi, A.; Signorelli, C.; Sechi, G.M.; Fagoni, N. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network—A Three-Year Study. J. Clin. Med. 2022, 11, 5718. [Google Scholar] [CrossRef]
- ISTAT—Mortalità. Available online: https://www.istat.it/notizia/dati-di-mortalita-cosa-produce-listat/ (accessed on 30 July 2024).
- ROOT—Cern. Available online: https://root.cern/ (accessed on 10 July 2024).
- Brun, R.; Rademakers, F. ROOT—An Object Oriented Data Analysis Framework. Nucl. Instrum. Methods Phys. Res. A 1997, 389, 81–86. [Google Scholar] [CrossRef]
- Glasziou, P.P.; Sanders, S.; Hoffmann, T. Waste in COVID-19 Research. BMJ 2020, 369, m1847. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Khosrawipour, T.; Kocbach, P.; Ichii, H.; Bania, J.; Khosrawipour, V. Evaluating the Massive Underreporting and Undertesting of COVID-19 Cases in Multiple Global Epicenters. Pulmonology 2021, 27, 110–115. [Google Scholar] [CrossRef]
- Istituto Superiore Di Sanità. Dati Della Sorveglianza Integrata COVID-19 in Italia. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard (accessed on 30 July 2024).
- Alamo, T.; Reina, D.; Mammarella, M.; Abella, A. COVID-19: Open-Data Resources for Monitoring, Modeling, and Forecasting the Epidemic. Electronics 2020, 9, 827. [Google Scholar] [CrossRef]
- Rizzo, M.; Foresti, L.; Montano, N. Comparison of Reported Deaths From COVID-19 and Increase in Total Mortality in Italy. JAMA Intern. Med. 2020, 180, 1250. [Google Scholar] [CrossRef]
- Mannucci, E.; Nreu, B.; Monami, M. Factors Associated with Increased All-Cause Mortality during the COVID-19 Pandemic in Italy. Int. J. Infect. Dis. 2020, 98, 121–124. [Google Scholar] [CrossRef]
- Brainard, J.; Lake, I.R.; Morbey, R.A.; Jones, N.R.; Elliot, A.J.; Hunter, P.R. Comparison of Surveillance Systems for Monitoring COVID-19 in England: A Retrospective Observational Study. Lancet Public Health 2023, 8, e850–e858. [Google Scholar] [CrossRef]
- Fattore, G.; Pongiglione, B.; Vezzosi, L. Excess Hospitalizations and In-Hospital Mortality Associated with Seasonal Influenza in Italy: A 11-Year Retrospective Study. BMC Infect. Dis. 2024, 24, 227. [Google Scholar] [CrossRef]
- Rosano, A.; Bella, A.; Gesualdo, F.; Acampora, A.; Pezzotti, P.; Marchetti, S.; Ricciardi, W.; Rizzo, C. Investigating the Impact of Influenza on Excess Mortality in All Ages in Italy during Recent Seasons (2013/14–2016/17 Seasons). Int. J. Infect. Dis. 2019, 88, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Vinci, A.; Pasquarella, A.; Corradi, M.P.; Chatzichristou, P.; D’Agostino, G.; Iannazzo, S.; Trani, N.; Parafati, M.A.; Palombi, L.; Ientile, D.A. Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy. Int. J. Environ. Res. Public Health 2022, 19, 5951. [Google Scholar] [CrossRef]
- Rivieccio, B.A.; Micheletti, A.; Maffeo, M.; Zignani, M.; Comunian, A.; Nicolussi, F.; Salini, S.; Manzi, G.; Auxilia, F.; Giudici, M.; et al. COVID-19, Learning from the Past: A Wavelet and Cross-Correlation Analysis of the Epidemic Dynamics Looking to Emergency Calls and Twitter Trends in Italian Lombardy Region. PLoS ONE 2021, 16, e0247854. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
del Re, D.; Palla, L.; Meridiani, P.; Soffi, L.; Loiudice, M.T.; Antinozzi, M.; Cattaruzza, M.S. Data from Emergency Medical Service Activities: A Novel Approach to Monitoring COVID-19 and Other Infectious Diseases. Diagnostics 2025, 15, 181. https://doi.org/10.3390/diagnostics15020181
del Re D, Palla L, Meridiani P, Soffi L, Loiudice MT, Antinozzi M, Cattaruzza MS. Data from Emergency Medical Service Activities: A Novel Approach to Monitoring COVID-19 and Other Infectious Diseases. Diagnostics. 2025; 15(2):181. https://doi.org/10.3390/diagnostics15020181
Chicago/Turabian Styledel Re, Daniele, Luigi Palla, Paolo Meridiani, Livia Soffi, Michele Tancredi Loiudice, Martina Antinozzi, and Maria Sofia Cattaruzza. 2025. "Data from Emergency Medical Service Activities: A Novel Approach to Monitoring COVID-19 and Other Infectious Diseases" Diagnostics 15, no. 2: 181. https://doi.org/10.3390/diagnostics15020181
APA Styledel Re, D., Palla, L., Meridiani, P., Soffi, L., Loiudice, M. T., Antinozzi, M., & Cattaruzza, M. S. (2025). Data from Emergency Medical Service Activities: A Novel Approach to Monitoring COVID-19 and Other Infectious Diseases. Diagnostics, 15(2), 181. https://doi.org/10.3390/diagnostics15020181






