AI and Interventional Radiology: A Narrative Review of Reviews on Opportunities, Challenges, and Future Directions
Abstract
:1. Introduction
1.1. The Scope and Implications of Interventional Radiology
1.1.1. Key Support in Surgery and Oncology
1.1.2. Beyond Oncology: Interventional Radiology in Medical Specialties
1.1.3. Pain Management and Contributions to Quality of Life
1.1.4. Applications in Gynecology, Urology, and Gastroenterology
1.1.5. The Importance of Vascular Access
1.2. A Continuously Evolving Future of Interventional Radiology
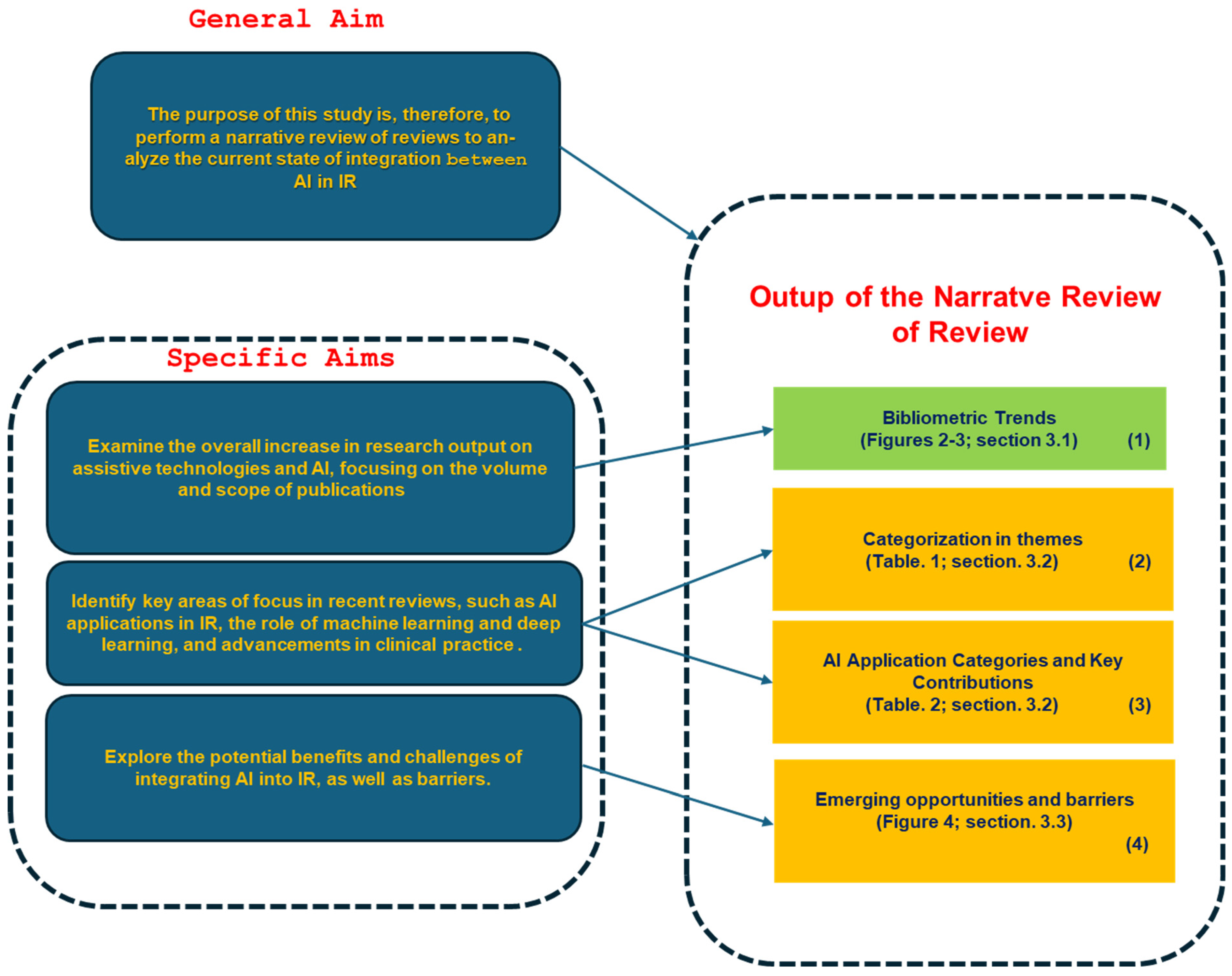
1.3. Purpose
- Analyze the overall bibliometric trends in the field: This study aims to provide a comprehensive bibliometric analysis of research output, focusing on trends and developments over time.
- Identify established themes and categories: Identify key areas of focus in reviews, such as AI applications, diagnostic accuracy, automation, decision support systems, and workflow optimization.
- Examine Opportunities and Challenges: Explore the potential benefits and challenges of integrating AI into interventional radiology, such as improving procedural precision, reducing human error, enhancing patient outcomes, and addressing issues like data privacy, regulatory concerns, and technology adoption barriers.
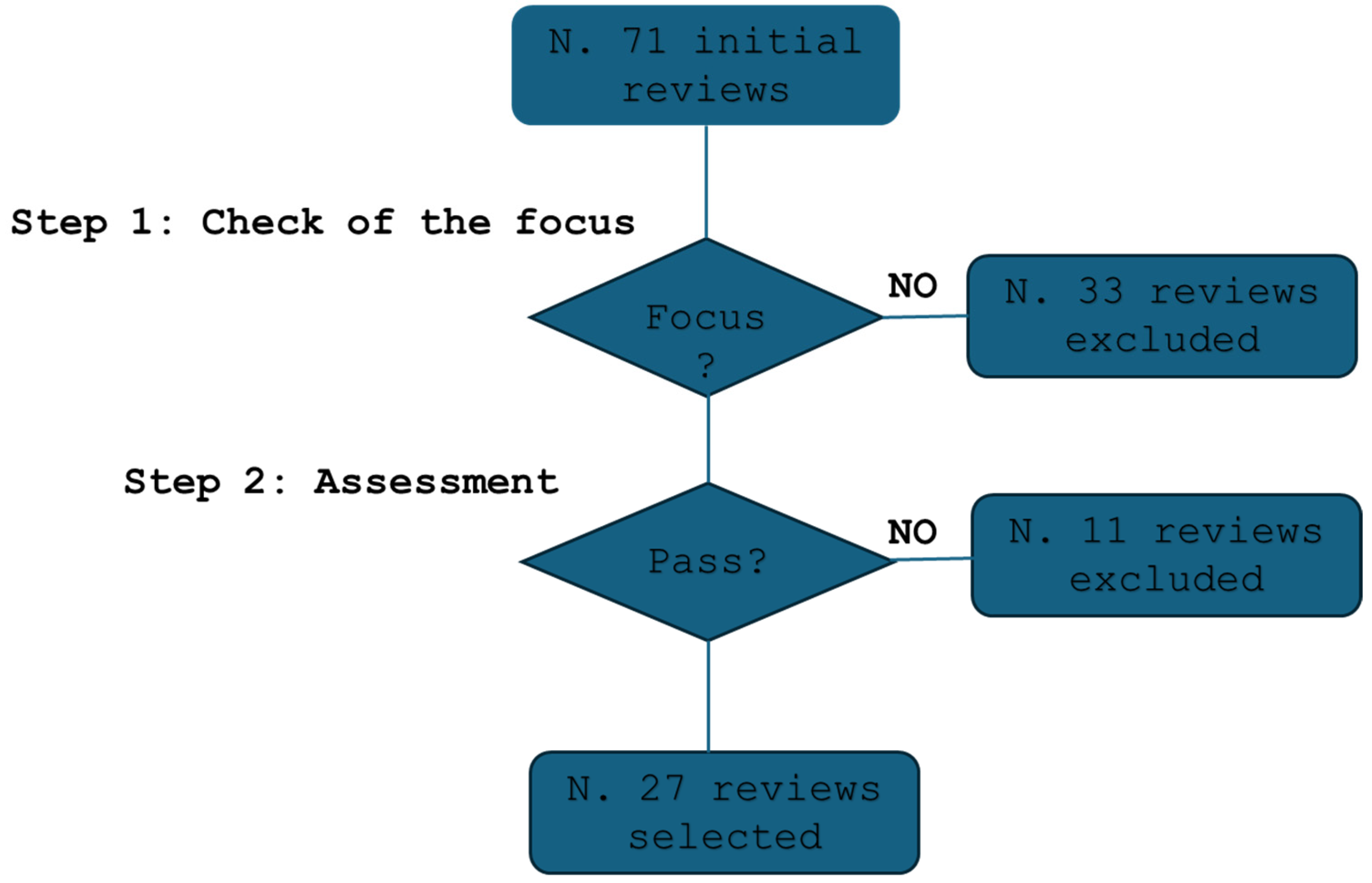
2. Methodology Overview
2.1. Narrative Review Selection and Qualification Process
2.1.1. Checklist and Qualification
| Algorithm 1: Selection Process for the NRR |
|
2.1.2. Assessment Process
2.1.3. Managing Bias in the Review
2.1.4. Selected Studies
2.2. Bibliometric Analysis Methodology
3. Results
3.1. Trends
| (interventional radiology[Title/Abstract]) (interventional radiology[Title/Abstract]) AND ((neural network[Title/Abstract]) OR (Artificial Intelligence[Title/Abstract]) OR (deep learning[Title/Abstract]) OR (ANN[Title/Abstract]) OR (GAN[Title/Abstract])) (diagnostic radiology[Title/Abstract]) AND ((neural network[Title/Abstract]) OR (Artificial Intelligence[Title/Abstract]) OR (deep learning[Title/Abstract]) OR (ANN[Title/Abstract]) OR (GAN[Title/Abstract])) |
3.2. The Application of IA in Interventional Radiology: A Comprehensive Overview
| Study | Brief Description | Focus | AI and Technology Integration |
|---|---|---|---|
| [11] Evaluation of navigation and robotic systems for percutaneous image-guided interventions: A novel metric for advanced imaging and artificial intelligence integration | This study reviews clinically validated robotic and navigation systems for percutaneous image-guided interventions, focusing on integrating AI and advanced imaging. It introduces a novel metric, LIAI2, for assessing AI and imaging integration. | The paper evaluates the extent of AI and advanced imaging integration in robotic systems for percutaneous procedures, aiming to enhance automation levels and precision. | The integration of AI aims to improve procedural accuracy and system autonomy, helping with tasks like needle placement and biopsies. This paper introduces a novel taxonomy to measure AI and imaging integration, addressing current limitations and driving future innovation in autonomous navigation. |
| [12] The Role and Future of Artificial Intelligence in Robotic Image-Guided Interventions | This review explores AI’s transformative potential in robotic-assisted interventional radiology (IR). It discusses AI’s role in handling tasks like catheter manipulation and needle placement, as well as current challenges such as limited decision-making capabilities. | The study focuses on how AI can improve robotic systems’ precision, efficiency, and reliability in IR interventions, enabling automation in complex procedures. | AI integration in robotic systems enhances precision and adaptability, particularly through reinforcement learning. While AI-driven robotics are expected to take over more tasks, human oversight remains essential to ensure safety and control during complex procedures. |
| [13] The Transformative Impact of AI, Extended Reality, and Robotics in Interventional Radiology: Current Trends and Applications | This article explores the integration of AI, robotics, and extended reality (XR) in interventional radiology, showcasing how these technologies are reshaping procedures and improving outcomes. It discusses the challenges of standardization across healthcare settings. | The paper emphasizes the synergy between AI, XR, and robotics to enhance image-guided interventions’ precision and efficiency in IR. | AI, robotics, and XR are being integrated to enhance diagnostic accuracy and procedural precision. AI is improving outcomes, while XR aids in visualizing complex anatomy, and robotics reduces human error. These technologies complement clinicians’ skills and aim to optimize patient care without replacing human expertise. |
| [14] Smartphone Technology for Applications in Image-Guided Minimally Invasive Interventional Procedures | This study investigates the use of smartphone technologies, such as augmented reality (AR), in image-guided minimally invasive procedures like biopsies and ablations. It explores how smartphones could enhance the accuracy and efficiency of needle-based interventions. | The focus is on the use of smartphones and AR to improve minimally invasive IR procedures by offering portable, real-time image guidance. | The integration of AR with smartphone sensors allows for real-time visualization of the procedural environment, offering greater precision in navigating complex anatomy. However, further research is needed to refine the technology and optimize its clinical use in IR. |
| [15] Imaging in France: 2024 Update | This article reviews recent advances in diagnostic and interventional radiology in France, particularly the integration of AI into diagnostic imaging. It highlights France’s contributions to improving diagnostic accuracy and advancing minimally invasive treatments in IR. | The paper focuses on technological advancements in AI-driven diagnostic imaging and their impact on IR, emphasizing innovations in tumor detection and advanced image fusion techniques. | AI has become central to improving diagnostic imaging in France, with applications in tumor detection, CT imaging, and image fusion. These advancements are enhancing the accuracy of diagnoses and treatment planning in IR. The study also discusses AI’s role in improving workflows and patient outcomes in interventional procedures. |
| [16] Applications of artificial intelligence in interventional oncology: An up-to-date review of the literature | This comprehensive review examines the role of AI in interventional oncology, particularly in image-guided therapies such as tumor embolization and ablation. It discusses AI tasks like tumor segmentation, outcome prediction, and recurrence detection. | The study focuses on how AI is revolutionizing interventional oncology through automation and enhanced treatment prediction. | AI in interventional oncology is being used to automate segmentation, predict outcomes, and detect recurrence after treatments. The integration of deep learning and radiomics is crucial in these tasks, improving treatment precision and patient management. More research is needed to validate these AI applications in clinical settings. |
| [17] Artificial intelligence in interventional radiology: Current concepts and future trends | This article explores the state of AI in interventional radiology, emphasizing its applications in preoperative, perioperative, and postoperative care. It highlights AI’s role in patient selection and outcome prediction. | The paper highlights both current and potential future applications of AI in IR, including image analysis, patient management, and real-time decision-making. | AI is enhancing the planning and execution of IR procedures, particularly in managing multimodal data and predicting patient outcomes. AI’s ability to support decision-making and improve robotic system capabilities is transforming procedural approaches and increasing procedural autonomy. |
| [18] How AI and Robotics Will Advance Interventional Radiology: Narrative Review and Future Perspectives | This review discusses the convergence of AI and robotics in advancing interventional radiology, particularly focusing on deep learning, machine learning, and convolutional neural networks (CNNs). It examines how AI and robotics can enhance precision across different specialties in IR. | The focus is on AI and robotics’ integration to improve procedural accuracy in IR, particularly in specialties like oncology, neurology, and cardiology. | AI and robotics are improving procedural precision in IR, with deep learning and CNNs automating complex tasks and predicting patient outcomes. The review discusses the potential for AI-driven robotics in IR, highlighting challenges such as integration and the need for standardization. |
| [19] Artificial intelligence in interventional radiology: state of the art | This paper provides an overview of AI applications in interventional radiology, emphasizing how AI supports decision-making, enhances imaging quality, and improves robotic interactions. It also addresses challenges to AI adoption, such as the complexity of IR procedures and the lack of standardization. | The focus is on AI’s role in enhancing decision support, imaging, and procedural execution in IR, with a focus on its transformative potential. | AI is significantly contributing to IR by improving decision support systems, enhancing imaging technologies like fusion imaging, and enabling robotic systems to function with greater precision. AI’s role in touchless interaction and virtual biopsies is also explored, though adoption is hindered by variability in procedural practices across institutions. |
| [20] An Introductory Guide to Artificial Intelligence in Interventional Radiology: Part 2: Implementation Considerations and Harms | This article provides a comprehensive look at the risks and challenges of implementing AI in interventional radiology (IR). It discusses potential harms associated with AI deployment, including overreliance on automated systems, and offers a practical checklist for clinicians to safely integrate AI technologies into clinical practice. | The article focuses on the practical considerations necessary for AI integration in IR. It emphasizes understanding and managing the risks involved in deploying AI systems, ensuring clinicians are equipped with strategies for safe implementation. It discusses regulatory oversight and monitoring mechanisms to prevent adverse effects on patient care. | The study presents AI as a tool with significant benefits but also highlights the importance of evaluating AI technologies based on their risk potential. It stresses the need for proper risk assessment and regulatory frameworks to ensure patient safety during AI deployment in clinical settings. |
| [21] An Introductory Guide to Artificial Intelligence in Interventional Radiology: Part 1 Foundational Knowledge | This foundational guide introduces interventional radiologists to the core concepts of AI. It outlines how AI is applied across different procedural stages, including pre-procedural planning, intra-procedural guidance, and post-procedural monitoring, aiming to enhance diagnostic accuracy and workflow efficiency. | The focus of this article is on educating clinicians about the role of AI in IR, explaining how AI can be used to optimize clinical workflows and decision-making at various stages of procedures. It also introduces a classification system for AI models to help clinicians understand the complexity and suitability of different AI technologies for their practice. | AI is framed as an essential tool for improving clinical outcomes and procedural efficiency in IR. The guide emphasizes the importance of AI across all procedural stages, helping radiologists understand how AI technologies can be effectively integrated into their daily practice. |
| [22] Interventional Oncology: 2024 Update | This review examines the integration of AI in interventional oncology, focusing on its role in imaging, treatment planning, and patient care. It explores AI’s potential to enhance tumor detection and personalize treatments, ultimately aiming to improve patient outcomes in oncology. | The focus is on AI’s impact on interventional oncology, particularly in improving diagnostic accuracy and tailoring treatment strategies to individual patients. The article also discusses the evolving training requirements for clinicians to handle AI technologies in oncology and their growing importance in clinical decision-making. | AI is integrated with advanced imaging technologies to improve tumor detection and characterization. It also plays a key role in personalizing treatment plans based on genomic data, offering a more individualized approach to oncology care. |
| [23] Understanding ChatGPT for Evidence-Based Utilization in Interventional Radiology | This study explores the use of ChatGPT, a language-based AI model, to support evidence-based decision-making in interventional radiology. It discusses how this AI tool can assist with patient communication, data interpretation, and clinical decision support. | The focus is on ChatGPT’s potential to enhance communication between clinicians and patients, as well as its ability to assist in decision-making processes by providing evidence-based insights and recommendations. | ChatGPT is presented as a valuable tool for streamlining communication in IR, helping clinicians access information quickly and support clinical decision-making by interpreting data and providing relevant recommendations. |
| [24] Current Applications of Algorithmic Artificial Intelligence in Interventional Radiology: A Review of the Literature | This review provides an overview of the current uses of algorithmic AI in interventional radiology, exploring its applications across various procedural stages. It discusses how AI is used to optimize imaging, assist in decision-making, and predict procedural outcomes. | The focus is on the broad applications of AI in IR, detailing its use in improving imaging quality, selecting patients for procedures, and predicting treatment outcomes. It emphasizes the potential of AI to streamline workflows and enhance the precision of interventions. | AI is used to enhance imaging capabilities, improve diagnostic accuracy, and assist with procedural decision-making. The review highlights AI’s growing role in predicting outcomes, reducing errors, and increasing efficiency in IR procedures. |
| [25] An Interventional Radiologist’s Primer of Critical Appraisal of Artificial Intelligence Research | This primer guides interventional radiologists in evaluating AI research, providing criteria for assessing the accuracy, reliability, and clinical applicability of AI models. It helps clinicians critically analyze AI technologies to ensure they meet clinical needs. | The focus is on equipping clinicians with the skills to critically appraise AI research and products. It provides a structured approach to evaluating AI models, focusing on accuracy, data quality, and the relevance of AI applications in clinical practice. | The article highlights the importance of critically assessing AI tools before integrating them into clinical practice. It ensures that clinicians can evaluate AI models based on scientific rigor and clinical relevance, promoting informed decisions on technology adoption. |
| [26] Robotics in Interventional Radiology: Review of Current and Future Applications | This review explores the current and future applications of robotics in IR, particularly in procedures involving image-guided navigation. It examines how AI-powered robotic systems are improving the precision and safety of minimally invasive interventions. | The focus is on the integration of robotic systems in IR, with an emphasis on AI’s role in enhancing procedural accuracy. It discusses the potential for robotic systems to transform IR by improving precision, reducing human error, and facilitating complex procedures. | Robotics, combined with AI, is transforming IR by enhancing precision and safety in interventions. AI-driven systems assist in tasks like navigation and decision-making, particularly in minimally invasive procedures, leading to better outcomes and reduced procedural risks. |
| [27] Artificial Intelligence, Augmented Reality, and Virtual Reality Advances and Applications in Interventional Radiology | This review examines how AI, augmented reality (AR), and virtual reality (VR) are converging to enhance interventional radiology. It highlights the potential of these technologies to improve diagnostics, guide treatment planning, and assist in complex procedures. | The focus is on the intersection of AI with AR and VR, exploring how these technologies can work together to provide clinicians with enhanced visualizations, decision support, and real-time feedback during procedures. | AI, AR, and VR are integrated to provide a more immersive, accurate, and interactive approach to diagnostics and treatment planning in IR. These technologies are improving procedural outcomes by offering real-time insights and visual assistance to clinicians. |
| [28] Technological Advancements in Interventional Oncology | This article explores the transformative impact of artificial intelligence in interventional oncology, focusing on the integration of AI for the analysis of large datasets and its use in predictive modeling for treatment response. It discusses the evolution of AI applications in diagnosing and treating cancers, highlighting AI’s ability to improve precision in tumor detection and treatment planning. The review provides insights into how AI and digital health technologies are enhancing workflows in clinical settings, particularly within interventional oncology. | The paper highlights AI’s role in improving diagnostic precision in oncology by analyzing vast medical data, aiding in tumor detection, and optimizing treatment planning. It discusses AI’s potential to predict treatment responses and guide clinical decisions, transforming the approach to personalized cancer care and workflow efficiency in oncology interventions. | AI has proven transformative in interventional oncology, enhancing tumor detection and treatment precision. By leveraging data and predictive modeling, AI is improving diagnostic accuracy and clinical decision-making, although challenges remain regarding data quality and clinical adoption. |
| [29] Artificial intelligence in diagnostic and interventional radiology: Where are we now? | This article examines the current state of AI in radiology, specifically in diagnostic and interventional radiology. It explores how AI, especially in conjunction with radiomics, is revolutionizing imaging processes in both diagnostics and interventions. The paper emphasizes how AI technologies are increasingly being used to assist radiologists by providing enhanced image analysis, automating repetitive tasks, and supporting clinical decision-making. Interventional radiology is poised to benefit from AI’s ability to enhance procedural guidance, patient selection, and real-time monitoring. | The article discusses the integration of AI in improving image analysis and automating tasks, making diagnostic processes more efficient. It also explores AI’s growing role in interventional radiology, including procedural guidance, real-time decision support, and improving patient outcomes. | AI is improving efficiency in radiology by automating tasks and enhancing image analysis. In interventional radiology, AI is increasingly used for procedural guidance, real-time monitoring, and decision-making, though challenges like data quality and integration persist. |
| [30] Artificial Intelligence in Interventional Radiology | This article reviews the historical development of artificial intelligence in medicine, focusing on its applications in interventional radiology. It traces the evolution of AI from its early conceptual stages to its current role in enhancing diagnostic capabilities and procedural guidance. AI in interventional radiology is mainly being used to assist in tumor detection, automate routine tasks, and improve procedural outcomes. The article also discusses the potential future impact of AI in revolutionizing interventional radiology by enhancing workflow and diagnostic precision. | The paper outlines the historical evolution and current applications of AI in interventional radiology, focusing on its role in tumor detection, automation of routine tasks, and improving procedural outcomes. It also looks at the future potential for AI to further enhance diagnostic precision and workflow efficiency. | AI is significantly enhancing tumor detection, procedural guidance, and workflow automation in interventional radiology. The paper emphasizes the future potential of AI, particularly in supporting real-time decision-making and optimizing clinical outcomes. |
| [31] Applications and challenges of artificial intelligence in diagnostic and interventional radiology | This literature review discusses the implementation of machine learning (ML) and deep learning (DL) techniques in radiology, including their applications in interventional radiology. The paper explores how AI can enhance image analysis, support diagnosis, assist in predicting management decisions, and improve clinical outcomes. It also addresses the challenges of implementing AI in clinical settings, such as the need for accurate, representative datasets and ethical considerations. | This review focuses on the applications of machine learning and deep learning in radiology, especially in interventional radiology. It highlights AI’s potential to improve image analysis, diagnostic accuracy, and patient management decisions, while also addressing the challenges posed by data quality and ethical issues in clinical adoption. | AI, particularly machine learning and deep learning, is revolutionizing diagnostic and interventional radiology by improving image analysis and supporting clinical decisions. However, challenges like data quality, training requirements, and ethical concerns hinder widespread implementation. |
| [32] Prime Time for Artificial Intelligence in Interventional Radiology | This article highlights the growing interest in AI within interventional radiology, focusing on the integration of machine learning and radiomics. It examines the potential applications of AI to enhance procedural planning, image-guided interventions, and patient monitoring. The paper emphasizes the readiness of interventional radiology to lead AI development, given its standardized data formats and data-rich environment. The article also discusses the need for research into overcoming challenges related to limited datasets and the integration of AI into clinical workflows. | The paper discusses the promising applications of AI in procedural planning, image-guided interventions, and patient monitoring within interventional radiology. It highlights the sector’s data-rich environment and standardization as factors that could help accelerate AI adoption, though challenges such as limited datasets remain. | AI has the potential to revolutionize procedural planning and patient monitoring in interventional radiology. However, the paper stresses that overcoming challenges like limited datasets and integrating AI into clinical practice are key hurdles that need addressing. |
| [33] Challenges of Implementing Artificial Intelligence in Interventional Radiology | This paper discusses the slow pace of AI adoption in interventional radiology compared to diagnostic radiology, identifying key challenges such as regulatory hurdles, data limitations, and ethical concerns. Despite AI’s potential to transform interventional radiology by enhancing procedural efficiency and diagnostic accuracy, the article highlights how these barriers have delayed widespread implementation. It calls for continued engagement with stakeholders to define clinically relevant use cases and prioritize resources effectively. | The article examines the slow adoption of AI in interventional radiology, emphasizing the regulatory and data challenges, as well as ethical concerns. It calls for collaboration among stakeholders to address these barriers and unlock the full potential of AI in this field. | The article identifies key barriers to AI adoption in interventional radiology, including regulatory hurdles, data quality, and ethical concerns. It stresses the need for collaboration to address these challenges and expedite AI integration into clinical practice. |
| [34] Current and emerging artificial intelligence applications for pediatric interventional radiology | This review examines the potential applications of AI in pediatric interventional radiology, an area that remains underserved in terms of AI technologies. The article discusses how AI can be utilized to improve image analysis, assist in diagnosis, and enhance procedural guidance in pediatric patients. Given the unique challenges of treating children, the paper emphasizes the importance of developing AI tools tailored to the specific needs of pediatric patients. | The article explores how AI can improve diagnostic and procedural outcomes in pediatric interventional radiology. It stresses the need for AI tools tailored to the unique anatomical and treatment needs of pediatric patients. | AI in pediatric interventional radiology holds promise for improving image analysis and procedural guidance, but the article highlights the need for AI tools specifically designed to meet the unique challenges of treating children. |
| [35] Role of Machine Learning and Artificial Intelligence in Interventional Oncology | This review highlights the role of AI and machine learning in interventional oncology, emphasizing their potential to enhance image analysis, intraprocedural guidance, and diagnostic accuracy. | The study explores how AI improves cancer detection, tumor classification, and treatment selection by predicting outcomes based on clinical and radiologic data. It also discusses challenges such as data processing, model validation, workflow integration, and ethical considerations. | AI and ML contribute to procedural guidance with precise needle tracking and image fusion, minimizing damage to healthy tissue while optimizing tumor treatment. |
| [36] Interventional Radiology ex-machina: Impact of Artificial Intelligence on Practice | This article examines the role of AI in interventional radiology, focusing on its potential to improve minimally invasive treatments and procedural accuracy. | The study explores AI applications in screening, patient selection modeling, predictive treatment planning, and procedural navigation. It also discusses the impact of augmented reality, mixed reality, and virtual reality in enhancing interventional radiology workflows. | AI, ML, and deep learning improve image analysis, procedural precision, and decision-making. Augmented and virtual reality technologies assist in enhancing interventional radiology procedures. |
| [37] Artificial Intelligence in Interventional Radiology: A Literature Review and Future Perspectives | This literature review discusses AI’s impact on interventional radiology, integrating evidence-based insights and expert perspectives to highlight current applications and future directions. | The study focuses on AI’s role in lesion detection, segmentation, procedural planning, and interventional oncology. It examines AI’s ability to provide prognostic insights and enhance minimally invasive treatments. | AI-driven computational algorithms, machine learning, and artificial neural networks improve diagnostic accuracy, procedural workflows, and personalized treatment planning in interventional radiology. |
| Category | Study Range | Medical Applications | Expanded Medical Applications Description |
|---|---|---|---|
| AI in Robotic and Navigation Systems | [11,12,18,19] | Needle Insertion, Biopsy Guidance, Catheter Placement | AI integration in robotic and navigation systems enhances the precision of complex procedures like needle insertion, biopsy guidance, and catheter placement. By analyzing imaging data in real-time, AI systems help identify the most accurate path for needle insertions and biopsies, minimizing damage to healthy tissue and improving the precision of sampling. In catheter placement, AI-driven systems provide constant adjustments to ensure accurate targeting, improving both procedural outcomes and patient safety. These AI-enhanced robotic systems reduce human error, improve targeting, and optimize real-time decision-making, resulting in fewer complications and faster recovery for patients. |
| AI in Oncology Interventions | [16,20,28,31,32,35] | Tumor Ablation, Tumor Detection, Post-Treatment Monitoring | In oncology, AI contributes to improved precision in tumor treatments such as ablation and embolization. By providing advanced image processing and automatic segmentation, AI enhances the accuracy of targeting tumors while minimizing damage to surrounding healthy tissue. AI systems also aid in early tumor detection by analyzing various imaging modalities and highlighting potential malignancies. Additionally, AI tools monitor patients post treatment, detecting early signs of tumor recurrence, predicting patient outcomes, and assessing the effectiveness of treatments, thus enabling more personalized follow-up care. |
| AI in Predictive Decision Support | [17,19,23,33,37] | Outcome Prediction, Personalized Treatment, Decision-Making Support | AI in predictive decision support systems analyzes patient data to predict outcomes, suggest personalized treatments, and assist in real-time clinical decisions. This system provides clinicians with a more precise understanding of potential risks and complications, improving diagnostic accuracy and patient safety. By continuously learning from evolving patient data, AI supports clinicians in making data-driven decisions that adapt to individual patient needs. The predictive capability of AI optimizes treatment plans and allows clinicians to anticipate complications, ensuring the most effective interventions are chosen. |
| AI in Minimally Invasive Procedures | [13,14,15,25,34,35] | Biopsy, Ablation, Access Point Localization | AI significantly improves the precision and safety of minimally invasive procedures by guiding access point localization, enhancing biopsy accuracy, and improving ablation targeting. Real-time AI-driven imaging systems provide immediate feedback, helping clinicians navigate anatomical structures with greater precision, thereby reducing the risk of complications. AI-assisted procedures like biopsies and ablations benefit from increased targeting accuracy, minimizing damage to healthy tissues and leading to faster patient recovery. Additionally, AI technologies optimize pre-procedural planning, allowing for more efficient execution of interventions. |
| AI in Image Fusion and Enhancement | [11,19,22,26,27,35] | Tumor Detection, Image Integration, Imaging Precision | AI-powered image fusion and enhancement techniques integrate multiple imaging modalities (e.g., CT, MRI, ultrasound) to provide clinicians with a more comprehensive view of a patient’s condition. This integration enhances diagnostic accuracy, especially for complex cases such as tumor detection, vascular anomalies, and surgical planning. By merging different imaging sources, AI helps to create more precise, detailed images, enabling more informed decision-making. This fusion is particularly valuable when dealing with difficult-to-diagnose conditions, as it provides a clearer picture of the patient’s anatomy, guiding clinicians to the most accurate diagnosis and treatment plan. |
| AI in Workflow and Efficiency Optimization | [21,25,29,36] | Task Automation, Scheduling, Process Streamlining | AI improves the operational efficiency of interventional radiology by automating routine tasks such as scheduling, data entry, and image processing. This allows healthcare providers to focus more on patient care rather than administrative tasks. AI algorithms can also streamline procedural planning by analyzing patient data and procedural variables to select the most efficient approach, optimizing resource allocation, reducing unnecessary interventions, and ensuring timely patient care. Additionally, AI helps predict patient volume and plan staffing, ensuring better resource utilization and smoother workflow in clinical settings. |
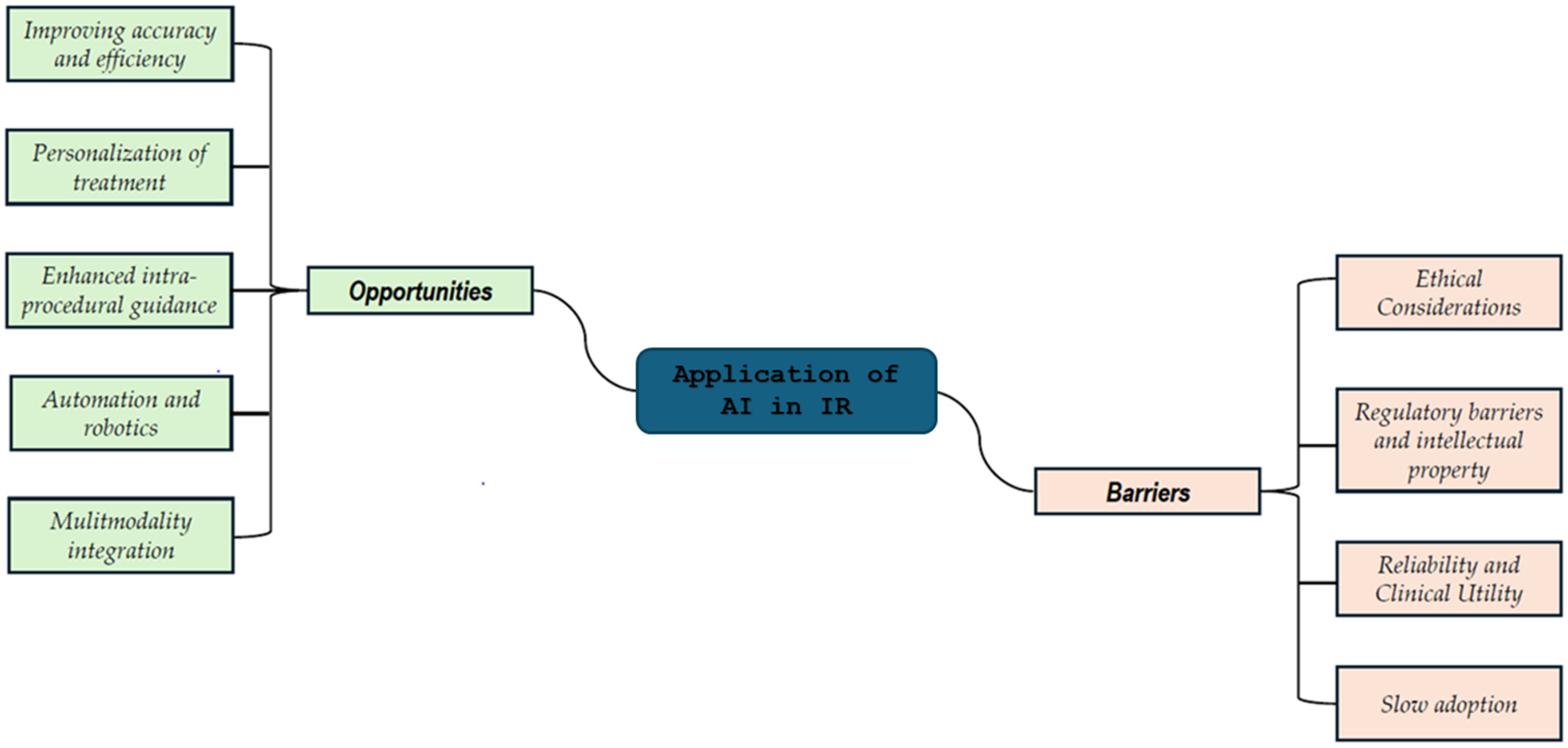
3.3. Emerging Opportunities and Challenges
4. Discussion
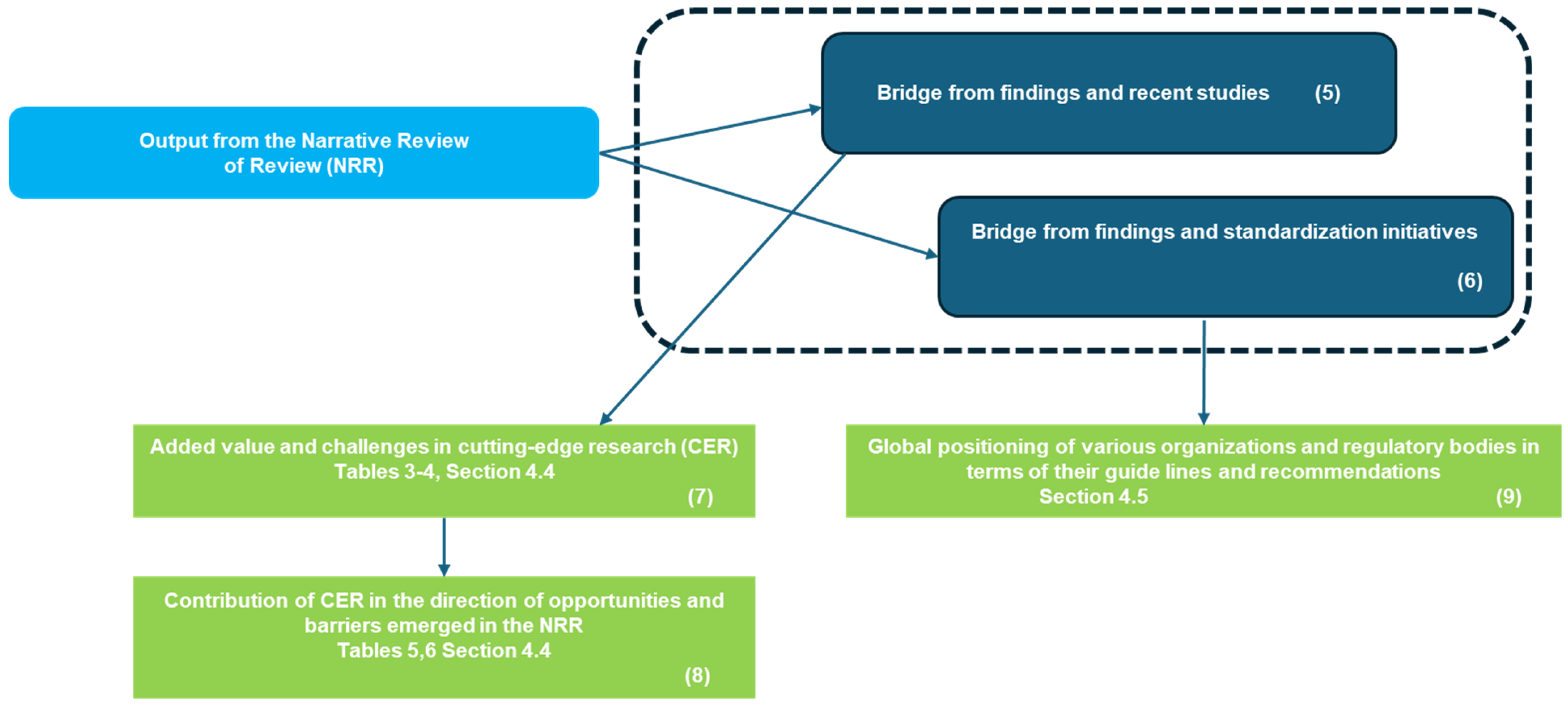
4.1. Synoptic Diagram
- Block 1: This block represents the bibliometric trends reported in Figure 2 and Figure 3 (Section 3.1). These trends were analyzed to provide an overview of the scientific production on AI applications in IR, forming the foundation for the subsequent steps of the study.
- Block 2: This block corresponds to the categorization of studies by thematic areas, as presented in Table 1 (Section 3.2). This categorization allowed for the organization of the reviewed studies according to key themes, facilitating a structured comparison.
- Block 3: Building upon the thematic categorization, this block highlights the comparative side-by-side analysis of the studies. The classification of AI applications was refined, as reported in Table 2 (Section 3.2), enabling a deeper understanding of the different ways AI is being applied across multiple domains.
- Block 4: This block synthesizes the opportunities and barriers identified in the reviewed studies, as reported in Figure 4 (Section 3.3). These findings highlight both the potential benefits of AI applications and the barriers
- Blocks 5 and 6 identify the need to bridge the gap between cutting-edge research (CER) and the current state of standardization.
- Connected to Block 5, two blocks highlight the contributions of CER in terms of added value and emerging challenges in Table 3 and Table 4 of Section 4.4 (Block 7), as well as its complementation in terms of opportunities and barriers identified in the NRR reported in Table 5 and Table 6 of Section 4.4 (Block 8)
- Connected to Block 6, Block 9 reports in Section 4.5 the global positioning of various organizations and regulatory bodies in terms of their guidelines and recommendations.
4.2. Highlights
4.3. Navigating AI in Interventional Radiology: Unique Complexities and Future Directions in Comparison to Diagnostic Radiology
4.4. AI in Interventional Radiology: Pioneering Studies Tackling Challenges, Exploring Opportunities, and Driving Key Innovations
| Advancements | Description | Related Studies |
|---|---|---|
| AI Integration for Improved Precision | AI has demonstrated significant potential in enhancing precision, optimizing patient outcomes, and revolutionizing treatment planning in IR. | [46,47,48,49,50] |
| AI in Robotic Systems | Robotic systems have shown improvements in precision and efficiency, particularly in lesion detection and path planning during CT-guided procedures. | [52] |
| AI Simplification of Radiology Reports | AI simplifies complex radiology reports, improving accessibility and readability for both clinicians and patients, but requires oversight to ensure quality. | [54] |
| AI in Parapharyngeal Space (PPS) Lesion Diagnosis | AI-assisted imaging has shown potential for precise diagnosis of PPS lesions and improved intervention planning, such as for CT-guided biopsies. | [56] |
| Advancements in Interventional Oncology (IO) | IO innovations are transforming cancer treatment, bridging diagnostic radiology and oncology, though challenges remain in integration and accuracy. | [45] |
| AI in IR Report Simplification and Accuracy | Large language models like GPT-4 and Claude-3-Opus simplify IR reports for better readability, though errors need to be minimized to ensure trust and clarity. | [57] |
| Linguistic Context Dependency | AI’s performance varies based on language and cultural context, impacting its application in liver cancer IR. | [51] |
| Deep Learning Model Refinement | While deep learning models aid anatomical identification, they face challenges in handling complex or atypical cases. | [53] |
| Automating Collimation | AI-driven collimation algorithms reduce radiation exposure and enhance image quality, but integrating them into fast-paced clinical workflows remains difficult. | [55] |
| Immunotherapy and Intratumoral Approaches | AI, through machine learning and radiomics, refines diagnosis and predicts treatment responses, optimizing personalized care in oncology. | [58] |
| Patient Education and Communication | GPT-4 aids in simplifying explanations of IR procedures, improving patient understanding and health literacy. | [59] |
| AI in Safety Data Analysis | GPT-4 categorizes and summarizes safety event data from IR devices, streamlining data analysis for improved patient safety. | [60] |
| Training and Exam Preparation | GPT-4 generates exam items for medical professionals, supporting EBIR exam preparation and training for various expertise levels. | [61] |
| Improved Imaging Techniques | AI-enhanced imaging generates synthetic contrast-enhanced images from non-contrast CT scans, improving image quality and reducing contrast agent use. | [62] |
| Challenges | Description | Related Studies |
|---|---|---|
| Data Availability | Difficulty in obtaining large datasets of labeled clinical images for AI model training, especially for fluoroscopy-guided interventions (FGIs). Synthetic data could help, but it needs rigorous validation. | [46] |
| Acceptance in Clinical Practice | AI’s ability to provide comprehensive, context-sensitive information for patient communication and informed consent remains a challenge. AI-generated outputs need more than surface-level responses. | [47] |
| Continuous Education and Training | IR professionals must keep up with rapidly evolving AI technologies, ensuring they can use these innovations effectively and ergonomically. Economic feasibility of AI adoption is also a key concern. | [48] |
| Linguistic Context Dependency | AI’s performance varies based on language and cultural context. For instance, ERNIE Bot and ChatGPT had differing performances in liver cancer IR depending on the language (Chinese vs. English). | [51] |
| Robotic Systems Integration | While robotic systems enhance precision in CT-guided procedures, challenges related to calibration, safety, and adaptability to different patients remain. | [52] |
| Radiology Report Simplification | AI can simplify radiology reports, but human oversight is often preferred by radiologists to ensure accuracy and quality, reflecting hesitance to fully trust AI. | [54] |
| Deep Learning Model Refinement | While deep learning models are useful for anatomical identification, issues persist with handling complex or atypical cases, requiring further refinement. | [53] |
| Automating Collimation | AI-driven collimation algorithms can reduce radiation exposure and improve image quality, but their integration into fast-paced clinical workflows remains challenging. | [55] |
| AI in Parapharyngeal Space (PPS) Lesions | AI shows potential in lesion diagnosis and intervention planning but needs further validation to ensure accuracy, especially in complex or rare cases. | [56] |
| Trust and Accuracy of AI Systems | While LLMs like GPT-4 and Claude-3-Opus show promise in simplifying IR reports, trust-breaking errors need to be addressed for clinical implementation. | [57] |
| Advancements in Interventional Oncology (IO) | IO innovations are transforming cancer treatment, bridging diagnostic radiology and oncology, though challenges remain in integration and accuracy. | [45] |
| Navigating Technological Change in IR | The integration of AI in IR requires leadership, collaboration, and an ongoing commitment to understanding its broader implications for patient care and clinical practice. | [50] |
| Data Quality and Consistency in Patient Education | Despite positive results in using AI for patient education, challenges remain in ensuring that AI-generated content is accurate, consistent, and suitable for all patients. | [58] |
| AI Reliability in Data Classification | AI models like GPT-4 for safety event data classification are effective, but there are concerns about the model’s reliability when handling complex or rare data. | [59] |
| AI Integration into Medical Education | AI’s role in medical exam preparation is promising, yet further validation is required to ensure that AI-generated questions are clinically relevant and effective for training purposes. | [60] |
| Image Quality and Safety in Advanced Imaging | While AI can generate synthetic contrast-enhanced images, ensuring their quality and clinical validity without causing patient harm remains a significant challenge. | [61] |
| Safety and Efficacy of AI in High-Stakes Procedures | AI models for synthetic contrast imaging are beneficial, but there is a need to address concerns about safety, accuracy, and clinical efficacy in high-stakes procedures like renal cancer treatments. | [62] |
| Opportunities form NRR | Description of Contribution from CER | References |
|---|---|---|
| 1. Improving Accuracy and Efficiency | AI plays a key role in enhancing diagnostic accuracy and operational efficiency within interventional radiology (IR). Deep learning models, for example, have been shown to improve the accuracy of anatomical location classification in imaging techniques like digital subtraction angiography (DSA). Additionally, the integration of AI into robotic systems for lesion detection and path planning helps ensure more precise targeting, reducing errors, and increasing procedural success rates. These advancements collectively improve patient outcomes and workflow efficiency. | [52,53] |
| 2. Personalization of Treatment | AI is significantly advancing personalized treatment planning, particularly in interventional oncology (IO). AI’s ability to improve tumor segmentation and detect lymph node metastasis allows for more tailored and accurate treatment strategies that are customized to individual patient profiles. For instance, AI is used to refine treatment planning for procedures like CT-guided biopsies, ensuring better-targeted interventions that align with the patient’s specific condition. This approach is vital for enhancing patient care and improving outcomes, especially in complex or rare cases. | [56] |
| 3. Enhanced Intra-Procedural Guidance | AI is crucial for improving intra-procedural guidance in IR. For example, robotic systems used in procedures like CT-guided interventions have shown improvements in precision and accuracy, enabling real-time decision-making and guidance. AI algorithms that automatically control collimation during procedures also contribute by reducing radiation exposure while maintaining high image quality. This capability is crucial for ensuring both patient safety and procedural success, making AI an essential tool in modern IR workflows. | [52,55] |
| 4. Automation and Robotics | The integration of AI-driven automation and robotic systems significantly enhances the accuracy, efficiency, and precision of interventional procedures. Robotic assistance not only improves procedural accuracy but also reduces clinician fatigue, particularly when performing repetitive or complex tasks. Moreover, AI’s role in automating tasks like report generation or collimation streamlines workflows, allowing healthcare professionals to allocate more time for critical decision-making and patient care. These advancements support the optimization of clinical outcomes in IR. | [52] |
| 5. Multimodal Integration | AI’s capacity to integrate different modalities, such as imaging, robotics, and real-time data analysis, is revolutionizing IR. Recent innovations, such as generating synthetic contrast-enhanced images from non-contrast CT scans, reduce reliance on contrast agents while maintaining high diagnostic quality. By improving imaging accuracy and optimizing procedural planning, AI-driven multimodal integration enhances treatment strategies and reduces patient exposure to harmful substances, making it a game-changer in the field. | [62] |
| Barriers from NRR | Description of Contribution of CER | References |
|---|---|---|
| 1. Ethical Considerations | Ethical challenges are a major barrier to AI adoption in IR. Concerns around data privacy, patient consent, and potential biases in AI models must be addressed to ensure that AI systems are ethically deployed. Additionally, the use of AI tools for tasks such as explaining procedures or risks to patients raises questions about whether these systems can provide contextually accurate and sensitive information. Clinicians may hesitate to fully rely on AI, especially when it comes to explaining complex medical situations to patients. | [47] |
| 2. Regulatory Barriers and Intellectual Property | Regulatory hurdles pose significant challenges to the integration of AI in clinical practice. AI technologies require rigorous validation and approval processes to ensure their safety and effectiveness. However, the rapid pace of AI development often outstrips existing regulatory frameworks, causing delays in clinical adoption. Furthermore, intellectual property issues related to AI models and the sharing of new technologies complicate collaboration and innovation in healthcare. These obstacles must be addressed to facilitate the broader use of AI in interventional radiology. | [46] |
| 3. Reliability and Clinical Utility | The reliability and clinical utility of AI systems remain significant barriers to their widespread adoption. While AI models have demonstrated promising results in controlled environments, their real-world performance may be inconsistent due to variations in data quality, model training, and the complexity of clinical cases. For example, AI models trained on synthetic data may not perform as effectively in real-world clinical scenarios, particularly in atypical or complex cases. This raises concerns among clinicians, who may be reluctant to trust AI outputs without human oversight, especially in critical applications like interventional procedures. | [46,54] |
| 4. Slow Adoption | Slow adoption of AI technologies remains a key barrier in interventional radiology. While there is significant interest in AI’s potential, many professionals are hesitant to integrate it into their practices. Concerns about the clinical utility of AI, the need for continuous training, and the disruption of established workflows all contribute to this resistance. Additionally, the financial and logistical challenges involved in adopting AI technologies, such as the cost of new equipment and system integration, hinder the widespread implementation of AI in clinical settings. | [48] |
4.5. Emerging Directions in Interventional Radiology: AI Integration and the Path to Global Harmonization
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: https://www.collinsdictionary.com/dictionary/english/interventional-radiology (accessed on 23 February 2025).
- Available online: https://www.oxfordreference.com/display/10.1093/oi/authority.20110803100008707?p=emailAMeeGkkfeJyEM&d=/10.1093/oi/authority.20110803100008707 (accessed on 23 February 2025).
- Chand, R.; Eltorai, A.E.; Healey, T.; Ahn, S. (Eds.) Essential Interventional Radiology Review A Question and Answer Guide; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Neri, E.; Erba, P.A. (Eds.) Multimodality Imaging and Intervention in Oncology; Sringer: Berlin/Heidelberg, Germany, 2023. [Google Scholar]
- Kini, A.; Sharma, S.K. (Eds.) Practical Manual of Interventional Cardiology; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Patel, A.; Petrone, B.; Carter, K.R. Percutaneous Vertebroplasty and Kyphoplasty. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK525963/ (accessed on 23 February 2025).
- Pinto, A.; Giurazza, F.; Califano, T.; Rea, G.; Valente, T.; Niola, R.; Caranci, F. Interventional radiology in gynecology and obstetric practice: Safety issues. In Seminars in Ultrasound, CT and MRI; WB Saunders: Philadelphia, PA, USA, 2021; Volume 42, pp. 104–112. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Montanarella, M.J.; Agarwal, A.; Moon, B. Peripherally Inserted Central Catheter (PICC) Line Placement. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK573064/ (accessed on 23 February 2025).
- Giurazza, F.; Niola, R. Interventional radiology in the 3rd millennium: Past, present and future perspectives. Radiol. Med. 2024, 129, 1429–1430. [Google Scholar] [CrossRef] [PubMed]
- Brady, A.P.; Allen, B.; Chong, J.; Kotter, E.; Kottler, N.; Mongan, J.; Oakden-Rayner, L.; Pin-to Dos Santos, D.; Tang, A.; Wald, C.; et al. Developing, purchasing, implementing and monitoring AI tools in radiology: Practical considerations. A multi-society statement from the ACR, CAR, ESR, RANZCR & RSNA. J. Med. Imaging Radiat. Oncol. 2024, 68, 7–26. [Google Scholar] [CrossRef] [PubMed]
- Cornelis, F.H.; Filippiadis, D.K.; Wiggermann, P.; Solomon, S.B.; Madoff, D.C.; Milot, L.; Bodard, S. Evaluation of navigation and robotic systems for percutaneous image-guided interventions: A novel metric for advanced imaging and artificial intelligence integration. Diagn. Interv. Imaging, 2025; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Boeken, T.; Lim, H.D.; Cohen, E.I. The Role and Future of Artificial Intelligence in Robotic Image-Guided Interventions. Tech. Vasc. Interv. Radiol. 2024, 27, 101001. [Google Scholar] [CrossRef] [PubMed]
- Vlastaris, K.; Alrez, A.; Friedland, S.; Randazzo, A.; Abboud, R.; Martin, C. The Transformative Impact of AI, Extended Reality, and Robotics in Interventional Radiology: Current Trends and Applications. Tech. Vasc. Interv. Radiol. 2024, 27, 101003. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Muniyandi, P.; Li, M.; Saccenti, L.; Christou, A.; Xu, S.; Wood, B.J. Smartphone Technology for Applications in Image-Guided Minimally Invasive Interventional Procedures. Cardiovasc. Interv. Radiol. 2025, 48, 142–156. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barat, M.; Crombé, A.; Boeken, T.; Dacher, J.N.; Si-Mohamed, S.; Dohan, A.; Chassagnon, G.; Lecler, A.; Greffier, J.; Nougaret, S.; et al. Imaging in France: 2024 Update. Can. Assoc. Radiol. J. 2024; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Matsui, Y.; Ueda, D.; Fujita, S.; Fushimi, Y.; Tsuboyama, T.; Kamagata, K.; Ito, R.; Yanagawa, M.; Yamada, A.; Kawamura, M.; et al. Applications of artificial intelligence in interventional oncology: An up-to-date review of the literature. Jpn. J. Radiol. 2025, 43, 164–176. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lesaunier, A.; Khlaut, J.; Dancette, C.; Tselikas, L.; Bonnet, B.; Boeken, T. Artificial intelligence in interventional radiology: Current concepts and future trends. Diagn. Interv. Imaging 2025, 106, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Fang, J.; Xu, Y.; Si, G. How AI and Robotics Will Advance Interventional Radiology: Narrative Review and Future Perspectives. Diagnostics 2024, 14, 1393. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Glielmo, P.; Fusco, S.; Gitto, S.; Zantonelli, G.; Albano, D.; Messina, C.; Sconfienza, L.M.; Mauri, G. Artificial intelligence in interventional radiology: State of the art. Eur. Radiol. Exp. 2024, 8, 62. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Warren, B.E.; Bilbily, A.; Gichoya, J.W.; Chartier, L.B.; Fawzy, A.; Barragán, C.; Jaberi, A.; Mafeld, S. An Introductory Guide to Artificial Intelligence in Interventional Radiology: Part 2: Implementation Considerations and Harms. Can. Assoc. Radiol. J. 2024, 75, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Warren, B.E.; Bilbily, A.; Gichoya, J.W.; Conway, A.; Li, B.; Fawzy, A.; Barragán, C.; Jaberi, A.; Mafeld, S. An Introductory Guide to Artificial Intelligence in Interventional Radiology: Part 1 Foundational Knowledge. Can. Assoc. Radiol. J. 2024, 75, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Geevarghese, R.; Bodard, S.; Razakamanantsoa, L.; Marcelin, C.; Petre, E.N.; Dohan, A.; Kastler, A.; Frandon, J.; Barral, M.; Soyer, P.; et al. Interventional Oncology: 2024 Update. Can. Assoc. Radiol. J. 2024, 75, 658–670. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.A., IV; Chick, J.F.B.; Shin, D.; Makary, M.S. Understanding ChatGPT for evidence-based utilization in interventional radiology. Clin. Imaging 2024, 108, 110098. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, A.J.; Vrazas, J.I.; Clements, W. Current applications of algorithmic artificial intelligence in interventional radiology: A review of the literature. J. Med. Imaging Radiat. Oncol. 2024, 68, 194–207. [Google Scholar] [CrossRef] [PubMed]
- Gaddum, O.; Chapiro, J. An Interventional Radiologist’s Primer of Critical Appraisal of Artificial Intelligence Research. J. Vasc. Interv. Radiol. 2024, 35, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Lanza, C.; Carriero, S.; Buijs, E.F.M.; Mortellaro, S.; Pizzi, C.; Sciacqua, L.V.; Biondetti, P.; Angileri, S.A.; Ianniello, A.A.; Ierardi, A.M.; et al. Robotics in Interventional Radiology: Review of Current and Future Applications. Technol. Cancer Res. Treat. 2023, 22, 15330338231152084. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- von Ende, E.; Ryan, S.; Crain, M.A.; Makary, M.S. Artificial Intelligence, Augmented Reality, and Virtual Reality Advances and Applications in Interventional Radiology. Diagnostics 2023, 13, 892. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Posa, A.; Barbieri, P.; Mazza, G.; Tanzilli, A.; Natale, L.; Sala, E.; Iezzi, R. Technological Advancements in Interventional Oncology. Diagnostics 2023, 13, 228. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boeken, T.; Feydy, J.; Lecler, A.; Soyer, P.; Feydy, A.; Barat, M.; Duron, L. Artificial intelligence in diagnostic and interventional radiology: Where are we now? Diagn. Interv. Imaging 2023, 104, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Kallini, J.R.; Moriarty, J.M. Artificial Intelligence in Interventional Radiology. Semin. Interv. Radiol. 2022, 39, 341–347. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Waller, J.; O’Connor, A.; Rafaat, E.; Amireh, A.; Dempsey, J.; Martin, C.; Umair, M. Applications and challenges of artificial intelligence in diagnostic and interventional radiology. Pol. J. Radiol. 2022, 87, e113–e117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seah, J.; Boeken, T.; Sapoval, M.; Goh, G.S. Prime Time for Artificial Intelligence in Interventional Radiology. Cardiovasc. Interv. Radiol. 2022, 45, 283–289. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazaheri, S.; Loya, M.F.; Newsome, J.; Lungren, M.; Gichoya, J.W. Challenges of Implementing Artificial Intelligence in Interventional Radiology. Semin. Interv. Radiol. 2021, 38, 554–559. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Desai, S.B.; Pareek, A.; Lungren, M.P. Current and emerging artificial intelligence applications for pediatric interventional radiology. Pediatr. Radiol. 2022, 52, 2173–2177. [Google Scholar] [CrossRef] [PubMed]
- D’Amore, B.; Smolinski-Zhao, S.; Daye, D.; Uppot, R.N. Role of Machine Learning and Artificial Intelligence in Interventional Oncology. Curr. Oncol. Rep. 2021, 23, 70. [Google Scholar] [CrossRef] [PubMed]
- Gurgitano, M.; Angileri, S.A.; Rodà, G.M.; Liguori, A.; Pandolfi, M.; Ierardi, A.M.; Wood, B.J.; Carrafiello, G. Interventional Radiology ex-machina: Impact of Artificial Intelligence on practice. Radiol. Med. 2021, 126, 998–1006. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iezzi, R.; Goldberg, S.N.; Merlino, B.; Posa, A.; Valentini, V.; Manfredi, R. Artificial Intelligence in Interventional Radiology: A Literature Review and Future Perspectives. J. Oncol. 2019, 2019, 6153041. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giansanti, D. AI in Cytopathology: A Narrative Umbrella Review on Innovations, Challenges, and Future Directions. J. Clin. Med. 2024, 13, 6745. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pirrera, A.; Giansanti, D. Human-Machine Collaboration in Diagnostics: Exploring the Synergy in Clinical Imaging with Artificial Intelligence. Diagnostics 2023, 13, 2162. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Auloge, P.; Garnon, J.; Robinson, J.M.; Dbouk, S.; Sibilia, J.; Braun, M.; Vanpee, D.; Koch, G.; Cazzato, R.L.; Gangi, A. Interventional radiology and artificial intelligence in radiology: Is it time to enhance the vision of our medical students? Insights Into Imaging 2020, 11, 127. [Google Scholar] [CrossRef]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=%28diagnostic+radiology%5BTitle%2FAbstract%5D%29+AND+%28%28neural+network%5BTitle%2FAbstract%5D%29+OR+%28Artificial+Intelligence%5BTitle%2FAbstract%5D%29+OR+%28deep+learning%5BTitle%2FAbstract%5D%29+OR+%28ANN%5BTitle%2FAbstract%5D%29+OR+%28GAN%5BTitle%2FAbstract%5D%29+%29&sort=date&size=50 (accessed on 23 February 2025).
- Trivedi, P.; Young, S. The Evolution of Interventional Radiology: How Far Will the Apple Land From the Tree? J. Am. Coll. Radiol. 2024, 21, 701–703. [Google Scholar] [CrossRef]
- Majid, A.S.; White, S.B. The future of interventional radiology should be continued alignment with diagnostic radiology. J. Am. Coll. Radiol. 2024, 21, 704–705. [Google Scholar] [CrossRef] [PubMed]
- Ryu, R.K. The future of interventional radiology is independent of diagnostic radiology. J. Am. Coll. Radiol. 2024, 21, 706–707. [Google Scholar] [PubMed]
- Newbury, A.; Ferguson, C.; Valero, D.A.; Kutcher-Diaz, R.; McIntosh, L.; Karamanian, A.; Harman, A. Interventional oncology update. Eur. J. Radiol. Open 2022, 9, 100430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fum, W.K.S.; Md Shah, M.N.; Raja Aman, R.R.A.; Abd Kadir, K.A.; Wen, D.W.; Leong, S.; Tan, L.K. Generation of fluoroscopy-alike radiographs as alternative datasets for deep learning in interventional radiology. Phys. Eng. Sci. Med. 2023, 46, 1535–1552. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, H.L.; Vairavamurthy, J. Large language model doctor: Assessing the ability of ChatGPT-4 to deliver interventional radiology procedural information to patients during the consent process. CVIR Endovasc. 2024, 7, 83. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cornelis, F.H.; Soyer, P.; Patlas, M.N. Interventional Radiology is Now at the Confluence of Expertise, Innovation, and Artificial Intelligence. Can. Assoc. Radiol. J. 2024, 75, 456–457. [Google Scholar] [CrossRef] [PubMed]
- Najafi, A.; Cazzato, R.L.; Meyer, B.C.; Pereira, P.L.; Alberich, A.; López, A.; Ronot, M.; Fritz, J.; Maas, M.; Benson, S.; et al. CIRSE Position Paper on Artificial Intelligence in Interventional Radiology. Cardiovasc. Interv. Radiol. 2023, 46, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, B.; Tselikas, L. Available online: https://www.sciencedirect.com/science/article/abs/pii/S2211568425000075?via%3Dihub (accessed on 23 February 2025).
- Yuan, X.T.; Shao, C.Y.; Zhang, Z.Z.; Qian, D. Comparing the performance of ChatGPT and ERNIE Bot in answering questions regarding liver cancer interventional radiology in Chinese and English contexts: A comparative study. Digit. Health 2025, 11, 20552076251315511. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sato, T.; Kawai, T.; Shimohira, M.; Ohta, K.; Suzuki, K.; Nakayama, K.; Takikawa, J.; Kawaguchi, T.; Urano, M.; Ng, K.W.; et al. Robot-Assisted CT-guided Biopsy with an Artificial Intelligence-Based Needle-Path Generator: An Experimental Evaluation Using a Phantom Model. J. Vasc. Interv. Radiol. 2025, S1051-0443(25)00040-5. [Google Scholar] [CrossRef] [PubMed]
- Taghavi, R.M.; Shah, A.; Filkov, V.; Goldman, R.E. Deep Learning Models for Automatic Classification of Anatomic Location in Abdominopelvic Digital Subtraction Angiography. J. Imaging Inform. Med. 2025; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Amin, K.S.; Davis, M.A.; Naderi, A.; Forman, H.P. Release of complex imaging reports to patients, do radiologists trust AI to help? Curr. Probl. Diagn. Radiol. 2025, 54, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.C.; Rijhwani, D.; Lang, S.; van Oorde-Grainger, S.; Haak, A.; Bleise, C.; Lylyk, P.; Ruijters, D.; Sinha, A. Tunable and real-time automatic interventional x-ray collimation from semi-supervised deep feature extraction. Med. Phys. 2024; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Vogl, T.J.; Burck, I.; Stöver, T.; Helal, R. Parapharyngeal Space: Diagnostic Imaging and Intervention. In RöFo-Fortschritte auf dem Gebiet der Röntgenstrahlen und der Bildgebenden Verfahren; Georg Thieme Verlag KG: Stuttgart, Germany, 2024. [Google Scholar] [CrossRef] [PubMed]
- Can, E.; Uller, W.; Vogt, K.; Doppler, M.C.; Busch, F.; Bayerl, N.; Ellmann, S.; Kader, A.; Elkilany, A.; Makowski, M.R.; et al. Large Language Models for Simplified Interventional Radiology Reports: A Comparative Analysis. Acad. Radiol. 2025, 32, 888–898. [Google Scholar] [CrossRef] [PubMed]
- Sajan, A.; Lamane, A.; Baig, A.; Floch, K.L.; Dercle, L. The emerging role of AI in enhancing intratumoral immunotherapy care. Oncotarget 2024, 15, 635–637. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elhakim, T.; Brea, A.R.; Fidelis, W.; Paravastu, S.S.; Malavia, M.; Omer, M.; Mort, A.; Ramasamy, S.K.; Tripathi, S.; Dezube, M.; et al. Enhanced PROcedural Information READability for Patient-Centered Care in Interventional Radiology With Large Language Models (PRO-READ IR). J. Am. Coll. Radiol. 2025, 22, 84–97. [Google Scholar] [CrossRef] [PubMed]
- Warren, B.E.; Alkhalifah, F.; Ahrari, A.; Min, A.; Fawzy, A.; Annamalai, G.; Jaberi, A.; Beecroft, R.; Kachura, J.R.; Mafeld, S.C. Feasibility of Artificial Intelligence Powered Adverse Event Analysis: Using a Large Language Model to Analyze Microwave Ablation Malfunction Data. Can. Assoc. Radiol. J. 2025, 76, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Ebel, S.; Ehrengut, C.; Denecke, T.; Gößmann, H.; Beeskow, A.B. GPT-4o’s competency in answering the simulated written European Board of Interventional Radiology exam compared to a medical student and experts in Germany and its ability to generate exam items on interventional radiology: A descriptive study. J. Educ. Eval. Health Prof. 2024, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, M.A.; Hu, Y.; Bandula, S.; Barratt, D.C. Time conditioning for arbitrary contrast phase generation in interventional computed tomography. Phys. Med. Biol. 2024, 69, 115010. [Google Scholar]
- Available online: https://pubs.rsna.org/page/ai/claim (accessed on 23 February 2025).
- Available online: https://www.acr.org/News-and-Publications/Joint-Radiological-Society-Paper-Guides-Implementation-and-Use-of-AI-Tools-in-Radiology (accessed on 23 February 2025).
- Available online: https://www.sor.org/learning-advice/professional-body-guidance-and-publications/documents-and-publications/policy-guidance-document-library/artificial-intelligence-guidance-for-clinical-imag (accessed on 23 February 2025).
- Available online: https://www.rcr.ac.uk/our-services/all-our-publications/clinical-radiology-publications/integrating-artificial-intelligence-with-the-radiology-reporting-workflows-ris-and-pacs/ (accessed on 23 February 2025).
- Available online: https://www.fda.gov/media/184856/download (accessed on 23 February 2025).
- Available online: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device (accessed on 23 February 2025).
- Available online: https://radiologybusiness.com/topics/healthcare-management/healthcare-policy/fda-clears-ai-software-aiding-interventional-radiologists-during-image-guided-procedures (accessed on 23 February 2025).
- Available online: https://www.fda.gov/media/184830/download (accessed on 23 February 2025).
- Available online: https://www.europarl.europa.eu/doceo/document/TA-9-2024-0138_EN.pdf (accessed on 23 February 2025).
- Kotter, E.; D’antonoli, T.A.; Cuocolo, R.; Hierath, M.; Huisman, M.; Klontzas, M.E.; Martí-Bonmatí, L.; May, M.S.; Neri, E.; Nikolaou, K.; et al. Guiding AI in radiology: ESR’s recommendations for effective imple-mentation of the European AI Act. Insights Imaging 2025, 16, 33. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lastrucci, A.; Iosca, N.; Wandael, Y.; Barra, A.; Lepri, G.; Forini, N.; Ricci, R.; Miele, V.; Giansanti, D. AI and Interventional Radiology: A Narrative Review of Reviews on Opportunities, Challenges, and Future Directions. Diagnostics 2025, 15, 893. https://doi.org/10.3390/diagnostics15070893
Lastrucci A, Iosca N, Wandael Y, Barra A, Lepri G, Forini N, Ricci R, Miele V, Giansanti D. AI and Interventional Radiology: A Narrative Review of Reviews on Opportunities, Challenges, and Future Directions. Diagnostics. 2025; 15(7):893. https://doi.org/10.3390/diagnostics15070893
Chicago/Turabian StyleLastrucci, Andrea, Nicola Iosca, Yannick Wandael, Angelo Barra, Graziano Lepri, Nevio Forini, Renzo Ricci, Vittorio Miele, and Daniele Giansanti. 2025. "AI and Interventional Radiology: A Narrative Review of Reviews on Opportunities, Challenges, and Future Directions" Diagnostics 15, no. 7: 893. https://doi.org/10.3390/diagnostics15070893
APA StyleLastrucci, A., Iosca, N., Wandael, Y., Barra, A., Lepri, G., Forini, N., Ricci, R., Miele, V., & Giansanti, D. (2025). AI and Interventional Radiology: A Narrative Review of Reviews on Opportunities, Challenges, and Future Directions. Diagnostics, 15(7), 893. https://doi.org/10.3390/diagnostics15070893







