Air Embolism: Diagnosis, Clinical Management and Outcomes
Abstract
:1. Introduction
2. Materials and Methods
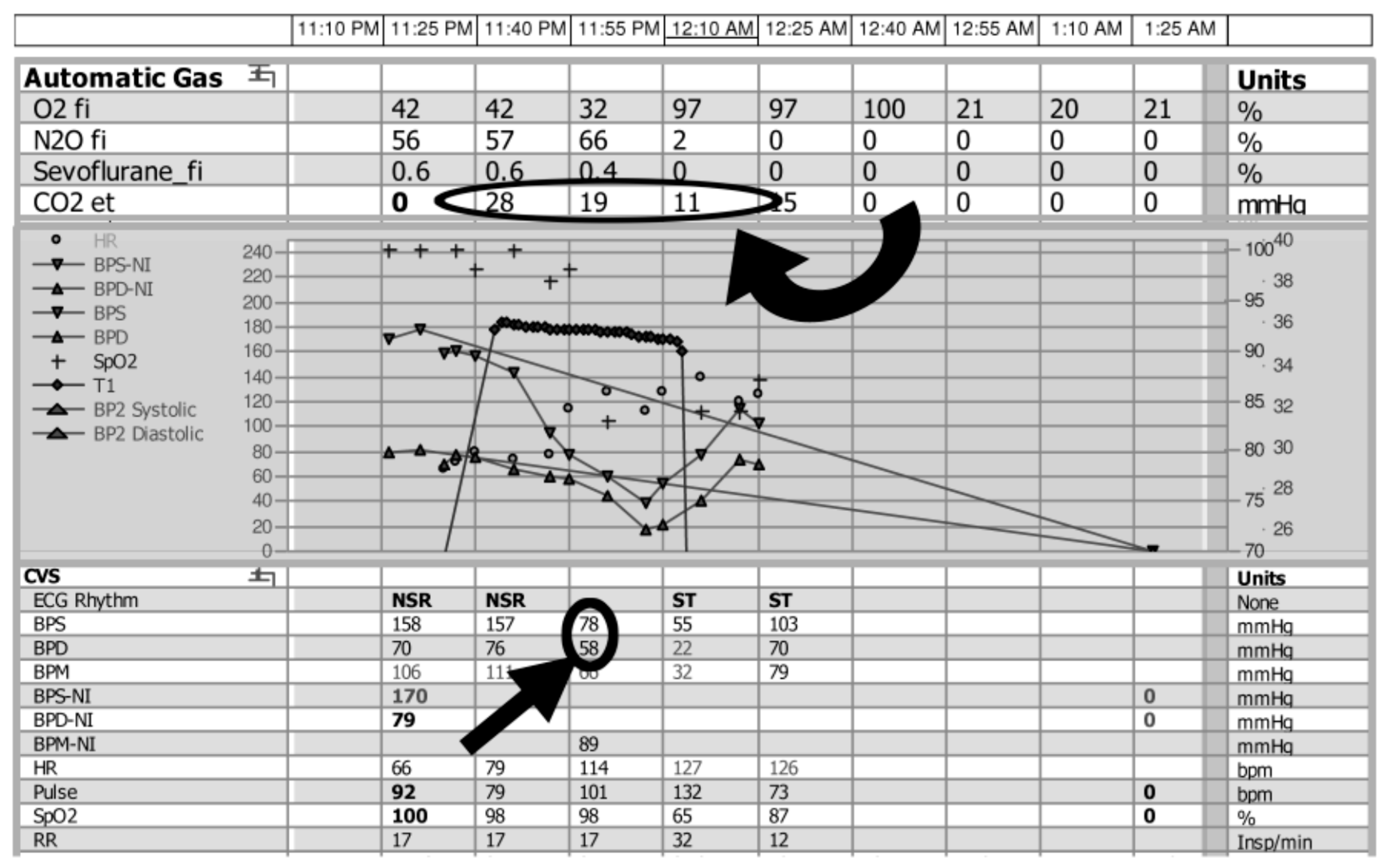
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mirski, M.A.; Lele, A.V.; Fitzsimmons, L.; Toung, T.J. Diagnosis and treatment of vascular air embolism. Anesthesiology 2007, 106, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Muth, C.M.; Shank, E.S. Gas embolism. N. Engl. J. Med. 2000, 342, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Pinho, J.; Amorim, J.M.; Araújo, J.M.; Vilaça, H.; Ribeiro, M.; Pereira, J.; Ferreira, C. Cerebral gas embolism associated with central venous catheter: Systematic review. J. Neurol. Sci. 2016, 362, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Freund, M.C.; Petersen, J.; Goder, K.C.; Bunse, T.; Wiedermann, F.; Glodny, B. Systemic air embolism during percutaneous core needle biopsy of the lung: Frequency and risk factors. BMC Pulm. Med. 2012, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Bessereau, J.; Genotelle, N.; Chabbaut, C.; Huon, A.; Tabah, A.; Aboab, J.; Chevret, S.; Annane, D. Long-term outcome of iatrogenic gas embolism. Intensiv. Care Med. 2010, 36, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Vesely, T.M. Air embolism during insertion of central venous catheters. J. Vasc. Interv. Radiol. 2001, 12, 1291–1295. [Google Scholar] [CrossRef]
- Wysoki, M.G.; Covey, A.; Pollak, J.; Rosenblatt, M.; Aruny, J.; Denbow, N. Evaluation of various maneuvers for prevention of air embolism during central venous catheter placement. J. Vasc. Interv. Radiol. 2001, 12, 764–766. [Google Scholar] [CrossRef]
- Fisher, D.C.; Fisher, E.A.; Budd, J.H.; Rosen, S.E.; Goldman, M.E. The incidence of patent foramen ovale in 1000 consecutive patients. A contrast transesophageal echocardiography study. Chest 1995, 107, 1504–1509. [Google Scholar] [CrossRef] [PubMed]
- Orebaugh, S.L. Venous air embolism: Clinical and experimental considerations. Crit. Care Med. 1992, 20, 1169–1177. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, T.; Gutierrez, G. Air embolism as a cause of the systemic inflammatory response syndrome: A case report. Crit. Care 2003, 7, R98–R100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flanagan, J.P.; Gradisar, I.A.; Gross, R.J.; Kelly, T.R. Air embolus—A lethal complication of subclavian venipuncture. N. Engl. J. Med. 1969, 281, 488–489. [Google Scholar] [CrossRef] [PubMed]
- Gale, T.; Leslie, K. Anaesthesia for neurosurgery in the sitting position. J. Clin. Neurosci. 2004, 11, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Faberowski, L.W.; Black, S.; Mickle, J.P. Incidence of venous air embolism during craniectomy for craniosynostosis repair. Anesthesiology 2000, 92, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.; Zimmerman, D.; Reintjes, F.; Courtney, M.; Klarenbach, S.; Dowling, G.; Pauly, R.P. Procedure-related serious adverse events among home hemodialysis patients: A quality assurance perspective. Am. J. Kidney Dis. 2014, 63, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.; Johnson, M.; Davies, S. Near-fatal air embolism: Fibrin sheath as the portal of air entry. South. Med. J. 2003, 96, 1036–1038. [Google Scholar] [CrossRef] [PubMed]
- Tellides, G.; Ugurlu, B.S.; Kim, R.W.; Hammond, G.L. Pathogenesis of systemic air embolism during bronchoscopic Nd:YAG laser operations. Ann. Thorac. Surg. 1998, 65, 930–934. [Google Scholar] [CrossRef]
- Harrison, E.A.; Mackersie, A.; McEwan, A.; Facer, E. The sitting position for neurosurgery in children: A review of 16 years’ experience. Br. J. Anaesth. 2002, 88, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, Y.; Balacumaraswami, L.; Pigott, D.W.; Matthews, P.M.; Taggart, D.P. Solid and gaseous cerebral microembolization during off-pump, on-pump, and open cardiac surgery procedures. J. Thorac. Cardiovasc. Surg. 2004, 127, 1759–1765. [Google Scholar] [CrossRef] [PubMed]
- Baerlocher, M.O.; Nikolic, B.; Silberzweig, J.E.; Kinney, T.B.; Kuo, M.D.; Rose, S.C. Society of Interventional Radiology position statement on recent change to the ASA's moderate sedation standards: Capnography. J. Vasc. Interv. Radiol. 2013, 24, 939–940. [Google Scholar] [CrossRef] [PubMed]
- Weaver, J. The latest ASA mandate: CO2 monitoring for moderate and deep sedation. Anesth. Prog. 2011, 58, 111–112. [Google Scholar] [CrossRef] [PubMed]
- Beitz, A.; Riphaus, A.; Meining, A.; Kronshage, T.; Geist, C.; Wagenpfeil, S.; Weber, A.; Jung, A.; Bajbouj, M.; Pox, C.; et al. Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: A randomized, controlled study (ColoCap Study). Am. J. Gastroenterol. 2012, 107, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, K.; Asirvatham, S.; Kamath, S.; Peck, S.; Liu, X. Successful interventional management of catastrophic coronary arterial air embolism during atrial fibrillation ablation. Heart Rhythm Case Rep. 2016, 2, 153–156. [Google Scholar] [CrossRef]
- Durant, T.M.; Long, J.; Oppenheimer, M.J. Pulmonary (venous) air embolism. Am. Heart J. 1947, 33, 269–281. [Google Scholar] [CrossRef]
- Murphy, B.P.; Harford, F.J.; Cramer, F.S. Cerebral air embolism resulting from invasive medical procedures. Treatment with hyperbaric oxygen. Ann. Surg. 1985, 201, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Brockmeyer, J.; Simon, T.; Seery, J.; Johnson, E.; Armstrong, P. Cerebral air embolism following removal of central venous catheter. Mil. Med. 2009, 174, 878–881. [Google Scholar] [CrossRef] [PubMed]
- Moon, R.; Butler, F.K. RE: Cerebral air embolism following removal of central venous catheter, published in [Mil Med 2009: 174(8): 878–881]. Mil. Med. 2010, 175, xvi. [Google Scholar] [PubMed]
- McCrary, B.F. RE: Cerebral air embolism following removal of central venous catheter, published in [Mil Med 2009: 174(8): 878–881]. Mil. Med. 2009, 174, xii–xiii. [Google Scholar] [PubMed]
- Brockmeyer, J.; Johnson, E.K. Cerebral air embolism following removal of central venous catheter. Mil. Med. 2011, 9, i. [Google Scholar] [CrossRef]
- Leach, R.M.; Rees, P.J.; Wilmshurst, P. Hyperbaric oxygen therapy. BMJ 1998, 317, 1140–1143. [Google Scholar] [CrossRef] [PubMed]
- Closon, M.; Vivier, E.; Breynaert, C.; Duperret, S.; Branche, P.; Coulon, A.; De La Roche, E.; Delafosse, B. Air embolism during an aircraft flight in a passenger with a pulmonary cyst: A favorable outcome with hyperbaric therapy. Anesthesiology 2004, 101, 539–542. [Google Scholar] [CrossRef] [PubMed]
- Blanc, P.; Boussuges, A.; Henriette, K.; Sainty, J.; Deleflie, M. Iatrogenic cerebral air embolism: Importance of an early hyperbaric oxygenation. Intensiv. Care Med. 2002, 28, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Armon, C.; Deschamps, C.; Adkinson, C.; Fealey, R.D.; Orszulak, T.A. Hyperbaric treatment of cerebral air embolism sustained during an open-heart surgical procedure. Mayo Clin. Proc. 1991, 66, 565–571. [Google Scholar] [CrossRef]
- Bothma, P.A.; Schlimp, C.J., II. Retrograde cerebral venous gas embolism: Are we missing too many cases? Br. J. Anaesth. 2014, 112, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.M.; Ling, E. Systemic air embolism after lung trauma. Anesthesiology 1999, 90, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, N.; Ummunisa, F. Acute management of vascular air embolism. J. Emerg. Trauma Shock 2009, 2, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, J.A.; Gottlieb, J.D.; Sweet, R.B. Closed-Chest Cardiac Massage in the Treatment of Venous Air Embolism. N. Engl. J. Med. 1964, 270, 1353–1354. [Google Scholar] [CrossRef] [PubMed]
- Ziewacz, J.E.; Arriaga, A.F.; Bader, A.M.; Berry, W.R.; Edmondson, L.; Wong, J.M.; Lipsitz, S.R.; Hepner, D.L.; Peyre, S.; Nelson, S.; et al. Crisis checklists for the operating room: Development and pilot testing. J. Am. Coll. Surg. 2011, 213, 212–217.e10. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.J.; Behravesh, S.; Naidu, S.G.; Oklu, R. Air Embolism: Practical Tips for Prevention and Treatment. J. Clin. Med. 2016, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Feil, M. Preventing central line air embolism. Am. J. Nurs. 2015, 115, 64–69. [Google Scholar] [CrossRef] [PubMed]


| Location of Event | Number of Patients |
|---|---|
| Community | 4 |
| Dialysis | 2 |
| Floor/ICU (intensive care unit) | 11 |
| Intraoperative (including interventional radiology) | 48 |
| Peri-operative | 1 |
| Radiology (excluding interventional radiology) | 1 |
| Procedure | Number |
|---|---|
| Abdominal aortic aneurysm repair | 1 |
| Abdominoperineal resection | 1 |
| Atrial septal defect closure | 2 |
| Bronchoscopy | 1 |
| Coronary artery bypass grafting | 2 |
| Cardiac ablation | 1 |
| Cardiac catheterization | 3 |
| Inadvertent air bolus via IV line | 1 |
| Central vascular access | 9 |
| Endoscopic Retrograde Cholangio-Pancreatography (ERCP) | 1 |
| Hysteroscopy | 1 |
| Laparoscopic liver resection | 2 |
| Necrotic bowel resection | 1 |
| Endovascular neurointervention | 2 |
| Neurosurgery (open procedures) | 11 |
| Pacemaker placement | 1 |
| Spinal surgery | 2 |
| Transarterial chemoembolization (TACE) | 1 |
| Cardiac valve replacement | 4 |
| Varicose vein injection | 2 |
| Central Vascular Access | Number | Total |
|---|---|---|
| Central line before hip surgery | 1 | 9 |
| Dialysis catheter placement | 4 | |
| Hickman placement | 1 | |
| Central line placement during management of polytrauma | 1 | |
| Port placement | 2 | |
| Central line removal | ||
| Removal of internal jugular line | 5 | 7 |
| Removal of pulmonary arterial line | 1 | |
| Removal of subclavian line | 1 | |
| Other line-related | ||
| Patient absconded from hospital and removed central line at home | 1 | 6 |
| Inadvertent bolus of air via venous access device | 2 | |
| Patient removed hubs from peripherally inserted central catheter (PICC) at home | 1 | |
| Peripheral IV line placement | 2 |
| Anatomical Location | Number |
|---|---|
| Coronary artery | 8 |
| Lower extremity | 1 |
| Pulmonary artery/right heart | 36 |
| Cerebral | 21 |
| Pulmonary artery/right heart and cerebral arteries | 1 |
| Immediate Clinical Signs/Symptoms | Number |
|---|---|
| Acute myocardial infarct | 1 |
| Bradycardia, hypotension, unresponsive | 1 |
| Cardiac arrest | 13 |
| Desaturation | 5 |
| Desaturation and hypotension | 3 |
| Desaturation and neurological signs/symptoms | 3 |
| Desaturation, reduced end tidal carbon dioxide (ETCO2) | 6 |
| Desaturation, reduced ETCO2, and hypotension | 6 |
| Neurological signs/symptoms, without seizure | 16 |
| None observed clinically or seen on imaging * | 10 |
| Seizure | 3 |
| Time to Death | Number |
|---|---|
| <24 h | 5 |
| 24–48 h | 6 |
| 3–7 days | 2 |
| >7 days * | 1 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCarthy, C.J.; Behravesh, S.; Naidu, S.G.; Oklu, R. Air Embolism: Diagnosis, Clinical Management and Outcomes. Diagnostics 2017, 7, 5. https://doi.org/10.3390/diagnostics7010005
McCarthy CJ, Behravesh S, Naidu SG, Oklu R. Air Embolism: Diagnosis, Clinical Management and Outcomes. Diagnostics. 2017; 7(1):5. https://doi.org/10.3390/diagnostics7010005
Chicago/Turabian StyleMcCarthy, Colin J., Sasan Behravesh, Sailendra G. Naidu, and Rahmi Oklu. 2017. "Air Embolism: Diagnosis, Clinical Management and Outcomes" Diagnostics 7, no. 1: 5. https://doi.org/10.3390/diagnostics7010005
APA StyleMcCarthy, C. J., Behravesh, S., Naidu, S. G., & Oklu, R. (2017). Air Embolism: Diagnosis, Clinical Management and Outcomes. Diagnostics, 7(1), 5. https://doi.org/10.3390/diagnostics7010005






