Left Ventricular Diastolic Dysfunction in Type 2 Diabetes—Progress and Perspectives
Abstract
:1. Introduction
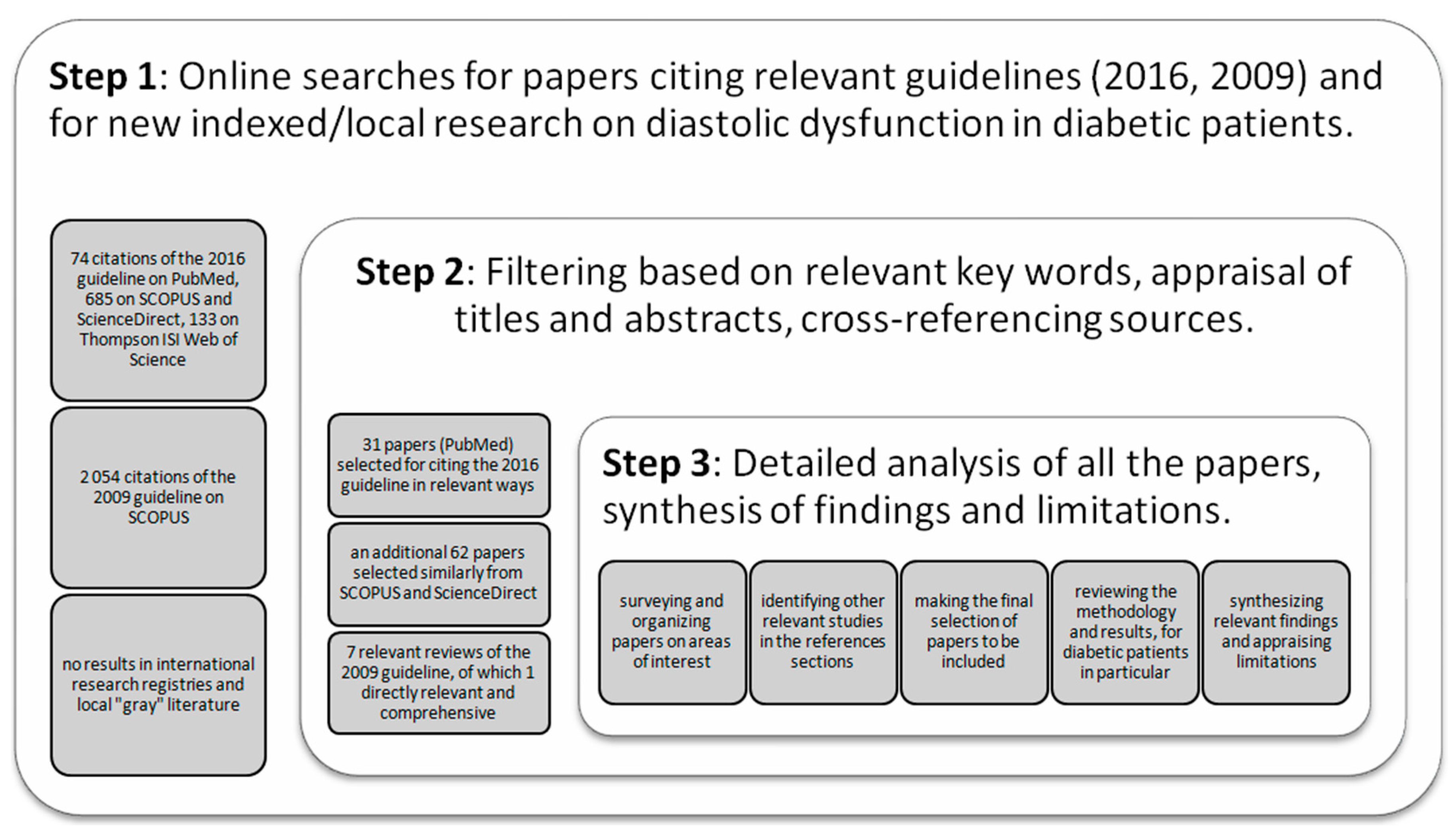
2. Materials and Methods
3. Left Ventricular Diastolic Dysfunction
3.1. Metabolic and Structural Changes
3.2. Echocardiographic Assessment Approaches
- Peak of passive filling (E wave), peak of active filling (A wave), E/A ratio, deceleration time of E wave (EDT) with pulsed Doppler (Figure 3);
- Isovolumetric relaxation time (IVRT) (Figure 4), early diastolic annular velocity E’ (septal, lateral, and average), late diastolic annular velocity A’ (septal, lateral, and average) via tissue Doppler imaging (TDI) (which measures myocardial tissue velocities during the cardiac cycle);
- Tricuspid regurgitation peak velocity (TRpV; Figure 5) with CW (continuous Doppler) on tricuspid regurgitation jet;
- S and D wave peak velocity on right superior pulmonary vein flow in pulsed Doppler (Figure 6);
- Left atrial size assessed by area or better by left atrium volume (indexed) (LAVi; Figure 7).
3.3. Diastolic Dysfunction—Where Are We Now?
3.4. Additional Remarks
3.4.1. General Patient Information
3.4.2. Alternative Diagnostic Methods
3.4.3. Treatment Spin-Offs
4. Limitations of The Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kenny, H.; Abel, E. Heart Failure in Type 2 Diabetes Mellitus. Circ. Res. 2019, 124, 121–141. [Google Scholar] [CrossRef]
- Newman, J.; Schwartzbard, A.; Weintraub, H.; Goldberg, I.; Berger, J. Primary Prevention of Cardiovascular Disease in Diabetes Mellitus. J. Am. Coll. Cardiol. 2017, 70, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.; Acs, A.; Ludwig, C.; Panton, U. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [PubMed]
- Schernthaner, G.; Lotan, C.; Baltadzhieva-Trendafilova, E.; Ceponis, J.; Clodi, M.; Ducena, K.; Goncalvesova, E.; Guja, C.; Honka, M.; Janež, A.; et al. Unrecognised cardiovascular disease in type 2 diabetes: Is it time to act earlier? Cardiovasc. Diabetol. 2018, 17, 145. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.; Golden, S.; Anderson, C.; Bray, G.; Burke, L.; de Boer, I.; Deedwania, P.; Eckel, R.; Ershow, A.; Fradkin, J.; et al. Update on Prevention of Cardiovascular Disease in Adults with Type 2 Diabetes Mellitus in Light of Recent Evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association. Diabetes Care 2015, 38, 1777–1803. [Google Scholar] [CrossRef]
- American Diabetes Association. 10. Cardiovascular disease and risk management: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019, 42 (Suppl. 1), S103–S123. [Google Scholar] [CrossRef] [PubMed]
- Atherton, J.; Sindone, A.; De Pasquale, C.; Driscoll, A.; MacDonald, P.; Hopper, I.; Kistler, P.; Briffa, T.; Wong, J.; Abhayaratna, W.; et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Guidelines for the Prevention, Detection, and Management of Heart Failure in Australia 2018. Heart Lung Circ. 2018, 27, 1123–1208. [Google Scholar] [CrossRef] [Green Version]
- Makrilakis, K.; Liatis, S. Cardiovascular Screening for the Asymptomatic Patient with Diabetes: More Cons Than Pros. J. Diabetes Res. 2017, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.; Appleton, C.; Gillebert, T.; Marino, P.; Oh, J.; Smiseth, O.; Waggoner, A.; Flachskampf, F.; Pellikka, P.; Evangelista, A. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography. J. Am. Soc. Echocardiogr. 2009, 22, 107–133. [Google Scholar] [CrossRef] [Green Version]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [Green Version]
- Lang, T.A.; Secic, M. Synthesizing the Results of Related Studies. In How to Report Statistics in Medicine, 2nd ed.; Lang, T.A., Secic, M., Eds.; American College of Physicians: Philadelphia, PA, USA, 2006; pp. 255–280. [Google Scholar]
- Zoppini, G.; Bergamini, C.; Mantovani, A.; Dauriz, M.; Targher, G.; Rossi, A.; Bonora, E. The E/e’ ratio difference between subjects with type 2 diabetes and controls. A meta-analysis of clinical studies. PLoS ONE 2018, 13, e0209794. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.; Fontes-Carvalho, R.; Sampaio, F.; Ribeiro, J.; Bettencourt, P.; Flachskampf, F.; Leite-Moreira, A.; Azevedo, A. Impact of the 2016 ASE/EACVI recommendations on the prevalence of diastolic dysfunction in the general population. Eur. Heart J. Cardiovasc. Imaging 2017, 19, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ISRCTN Registry. Available online: http://www.isrctn.com/ (accessed on 15 March 2019).
- Research Registry. Available online: https://www.researchregistry.com/ (accessed on 15 March 2019).
- Ponikowski, P.; Voors, A.; Anker, S.; Bueno, H.; Cleland, J.; Coats, A.; Falk, V.; González-Juanatey, J.; Harjola, V.; Jankowska, E.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Paulus, W.J. Heart Failure with Presearved Ejection Fraction: Pathophysiology, Diagnostic, and Treatment. Eur. Heart J. 2011, 32, 670–679. [Google Scholar] [CrossRef]
- Frati, G.; Schirone, L.; Chimenti, I.; Yee, D.; Biondi-Zoccai, G.; Volpe, M.; Sciarretta, S. An overview of the inflammatory signalling mechanisms in the myocardium underlying the development of diabetic cardiomyopathy. Cardiovasc. Res. 2017, 113, 378–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, G.; DeMarco, V.; Sowers, J. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat. Rev. Endocrinol. 2016, 12, 144–153. [Google Scholar] [CrossRef]
- Mandavia, C.; Aroor, A.; DeMarco, V.; Sowers, J. Molecular and metabolic mechanisms of cardiac dysfunction in diabetes. Life Sci. 2013, 92, 601–608. [Google Scholar] [CrossRef]
- Seferović, P.; Petrie, M.; Filippatos, G.; Anker, S.; Rosano, G.; Bauersachs, J.; Paulus, W.; Komajda, M.; Cosentino, F.; de Boer, R.; et al. Type 2 diabetes mellitus and heart failure: A position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 853–872. [Google Scholar] [CrossRef]
- Guja, C.; Dănciulescu Miulescu, S. Heart failure in type 2 diabetes – the forgotten complication. Rom. J. Diabetes Nutr. Metab. Dis. 2018, 25, 123–130. [Google Scholar] [CrossRef]
- Chavali, V.; Tyagi, S.C.; Mishra, P. Predictors and prevention of diabetic cardiomyopathy. Diabetes Metab Syndr. Obes. Targets Ther. 2013, 6, 151–160. [Google Scholar] [CrossRef]
- Maack, C.; Lehrke, M.; Backs, J.; Heinzel, F.; Hulot, J.; Marx, N.; Paulus, W.; Rossignol, P.; Taegtmeyer, H.; Bauersachs, J.; et al. Heart failure and diabetes: Metabolic alterations and therapeutic interventions: A state-of-the-art review from the Translational Research Committee of the Heart Failure Association–European Society of Cardiology. Eur. Heart J. 2018, 39, 4243–4254. [Google Scholar] [CrossRef] [PubMed]
- Pappachan, J.; Varughese, G.; Sriraman, R.; Arunagirinathan, G. Diabetic cardiomyopathy: Pathophysiology, diagnostic evaluation and management. World J. Diabetes 2013, 4, 177. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Refaat, M.; Mohammedi, K.; Jayyousi, A.; Al Suwaidi, J.; Abi Khalil, C. Macrovascular Complications in Patients with Diabetes and Prediabetes. Biomed. Res. Int. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sardu, C.; De Lucia, C.; Wallner, M.; Santulli, G. Diabetes Mellitus and Its Cardiovascular Complications: New Insights into an Old Disease. J. Diabetes Res. 2019, 1–2. [Google Scholar] [CrossRef] [PubMed]
- de Mattos Matheus, A.S.; Tannus, L.R.; Cobas, R.A.; Palma, C.C.; Negrato, C.A.; de Brito Gomes, M. Impact of Diabetes on Cardiovascular Disease: An Update. Int J. Hypertens 2013, 653789. [Google Scholar] [CrossRef]
- Riehle, C.; Bauersachs, J. Of mice and men: Models and mechanisms of diabetic cardiomyopathy. Basic Res. Cardiol. 2019, 114, 2. [Google Scholar] [CrossRef] [PubMed]
- Wan, S.; Vogel, M.; Chen, H. Pre-Clinical Diastolic Dysfunction. JACC 2014, 63, 407–416. [Google Scholar] [CrossRef]
- Low Wang, C.; Hess, C.; Hiatt, W.; Goldfine, A. Clinical Update: Cardiovascular Disease in Diabetes Mellitus. Circulation 2016, 133, 2459–2502. [Google Scholar] [CrossRef]
- Gilca, G.; Stefanescu, G.; Badulescu, O.; Tanase, D.; Bararu, I.; Ciocoiu, M. Diabetic Cardiomyopathy: Current Approach and Potential Diagnostic and Therapeutic Targets. J. Diabetes Res. 2017, 2017, 1–7. [Google Scholar] [CrossRef]
- Soares Felício, J.; Cavalcante Koury, C.; Tavares Carvalho, C.; Felício Abrahão Neto, J.; Barbosa Miléo, K.; Pontes Arbage, T.; Dias Silva, D.; Ferreira de Oliveira, A.; Soares Peixoto, A.; Bentes Figueiredo, A.; et al. Present Insights on Cardiomyopathy in Diabetic Patients. Curr. Diabetes Rev. 2016, 12, 384–395. [Google Scholar] [CrossRef] [Green Version]
- Mizamtsidi, M.; Paschou, S.; Grapsa, J.; Vryonidou, A. Diabetic cardiomyopathy: A clinical entity or a cluster of molecular heart changes? Eur. J. Clin. Investig. 2016, 46, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Almorós, A.; Tuñón, J.; Orejas, M.; Cortés, M.; Egido, J.; Lorenzo, Ó. Diagnostic approaches for diabetic cardiomyopathy. Cardiovasc. Diabetol. 2017, 16. [Google Scholar] [CrossRef] [PubMed]
- Maisch, B.; Alter, P.; Pankuweit, S. Diabetic cardiomyopathy—fact or fiction? Herz 2011, 36, 102–115. [Google Scholar] [CrossRef]
- Gajardo, A.; Llancaqueo, M. Circulating biomarkers of left ventricular diastolic function and dysfunction: Filling the research gap under high pressure. Eur. J. Prev. Cardiol. 2018, 26, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Whaley-Connell, A.; Sowers, J. Diabetic cardiomyopathy: A hyperglycaemia- and insulin-resistance-induced heart disease. Diabetologia 2018, 61, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Bugger, H.; Abel, E. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia 2014, 57, 660–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishida, K.; Otsu, K. Inflammation and metabolic cardiomyopathy. Cardiovasc. Res. 2017, 113, 389–398. [Google Scholar] [CrossRef] [Green Version]
- Sardu, C.; Pieretti, G.; D’Onofrio, N.; Ciccarelli, F.; Paolisso, P.; Passavanti, M.; Marfella, R.; Cioffi, M.; Mone, P.; Dalise, A.; et al. Inflammatory Cytokines and SIRT1 Levels in Subcutaneous Abdominal Fat: Relationship with Cardiac Performance in Overweight Pre-diabetics Patients. Front. Physiol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, N.; Pieretti, G.; Ciccarelli, F.; Gambardella, A.; Passariello, N.; Rizzo, M.; Barbieri, M.; Marfella, R.; Nicoletti, G.; Balestrieri, M.; et al. Abdominal Fat SIRT6 Expression and Its Relationship with Inflammatory and Metabolic Pathways in Pre-Diabetic Overweight Patients. Int. J. Mol. Sci. 2019, 20, 1153. [Google Scholar] [CrossRef] [PubMed]
- Seferović, P.; Paulus, W. Clinical diabetic cardiomyopathy: A two-faced disease with restrictive and dilated phenotypes. Eur. Heart J. 2015, 36, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Hölscher, M.; Bode, C.; Bugger, H. Diabetic Cardiomyopathy: Does the Type of Diabetes Matter? Int. J. Mol. Sci. 2016, 17, 2136. [Google Scholar] [CrossRef] [PubMed]
- Smiseth, O. Evaluation of left ventricular diastolic function: State of the art after 35 years with Doppler assessment. J. Echocardiogr. 2017, 16, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Silbiger, J. Pathophysiology and Echocardiographic Diagnosis of Left Ventricular Diastolic Dysfunction. J. Am. Soc. Echocardiogr. 2019, 32, 216–232. [Google Scholar] [CrossRef] [PubMed]
- Mitter, S.; Shah, S.; Thomas, J. A Test in Context. J. Am. Coll Cardiol 2017, 69, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Lang, M.R.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc Echocardiogr 2015, 28, 1–39. [Google Scholar] [CrossRef] [PubMed]
- Kossaify, A.; Nasr, M. Diastolic Dysfunction and the New Recommendations for Echocardiographic Assessment of Left Ventricular Diastolic Function: Summary of Guidelines and Novelties in Diagnosis and Grading. JDMS 2019, 35, 317–325. [Google Scholar] [CrossRef]
- Sanchis, L.; Andrea, R.; Falces, C.; Poyatos, S.; Vidal, B.; Sitges, M. Differential Clinical Implications of Current Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography. J. Am. Soc. Echocardiogr. 2018, 31, 1203–1208. [Google Scholar] [CrossRef]
- Gottbrecht, M.; Salerno, M.; Aurigemma, G. Evolution of diastolic function algorithms: Implications for clinical practice. Echocardiography 2017, 35, 39–46. [Google Scholar] [CrossRef]
- Fabiani, I.; Pugliese, N.; La Carrubba, S.; Conte, L.; Colonna, P.; Caso, P.; Benedetto, F.; Antonini-Canterin, F.; Citro, R.; Dini, F.; et al. Interactive role of diastolic dysfunction and ventricular remodeling in asymptomatic subjects at increased risk of heart failure. Int. J. Cardiovasc. Imaging 2019. [Google Scholar] [CrossRef]
- Alonso-Gómez, A.; Tojal Sierra, L.; Fortuny Frau, E.; Goicolea Güemez, L.; Aboitiz Uribarri, A.; Portillo, M.; Toledo, E.; Schröder, H.; Salas-Salvadó, J.; Arós Borau, F. Diastolic dysfunction and exercise capacity in patients with metabolic syndrome and overweight/obesity. Int J. Cardiol Heart Vasc 2019, 22, 67–72. [Google Scholar] [CrossRef]
- Shimron, M.; Williams, L.; Hazanov, Y.; Ghanim, D.; Kinany, W.; Amir, O.; Carasso, S. Clinical and echocardiographic characteristics of patients in sinus rhythm, normal left ventricular function, and indeterminate diastolic function. Echocardiography 2018, 35, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Fraser, A. A manifesto for cardiovascular imaging: Addressing the human factor. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 1311–1321. [Google Scholar] [CrossRef] [PubMed]
- Tamás, É.; Nylander, E. Decision support for assessment of left ventricular diastolic function. Physiol. Rep. 2018, 6, e13815. [Google Scholar] [CrossRef] [Green Version]
- Bamaiyi, A.; Woodiwiss, A.; Peterson, V.; Gomes, M.; Libhaber, C.; Sareli, P.; Norton, G. Insulin resistance influences the impact of hypertension on left ventricular diastolic dysfunction in a community sample. Clin Cardiol 2019, 42, 305–311. [Google Scholar] [CrossRef]
- Nagueh, S. Classification of Left Ventricular Diastolic Dysfunction and Heart Failure Diagnosis and Prognosis. J. Am. Soc. Echocardiogr. 2018, 31, 1209–1211. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.; Abraham, T.; Aurigemma, G.; Bax, J.; Beladan, C.; Browning, A.; Chamsi-Pasha, M.; Delgado, V.; Derumeaux, G.; Dolci, G.; et al. Interobserver Variability in Applying American Society of Echocardiography/European Association of Cardiovascular Imaging 2016 Guidelines for Estimation of Left Ventricular Filling Pressure. Circ. Cardiovasc. Imaging 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Steeds, R.; Garbi, M.; Cardim, N.; Kasprzak, J.; Sade, E.; Nihoyannopoulos, P.; Popescu, B.; Stefanidis, A.; Cosyns, B.; Monaghan, M.; et al. EACVI appropriateness criteria for the use of transthoracic echocardiography in adults: A report of literature and current practice review. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 1191–1204. [Google Scholar] [CrossRef]
- Gori, M.; Canova, P.; Calabrese, A.; Cioffi, G.; Trevisan, R.; De Maria, R.; Grosu, A.; Iacovoni, A.; Fontana, A.; Greene, S.J.; et al. Strategy to identify subjects with diabetes mellitus more suitable for selective echocardiographic screening: The DAVID-Berg study. Int. J. Cardiol. 2017, 248, 414–420. [Google Scholar] [CrossRef]
- Blomstrand, P.; Sjöblom, P.; Nilsson, M.; Wijkman, M.; Engvall, M.; Länne, T.; Nyström, F.; Östgren, C.; Engvall, J. Overweight and obesity impair left ventricular systolic function as measured by left ventricular ejection fraction and global longitudinal strain. Cardiovasc. Diabetol. 2018, 17. [Google Scholar] [CrossRef]
- Ng, A.; Prevedello, F.; Dolci, G.; Roos, C.; Djaberi, R.; Bertini, M.; Ewe, S.; Allman, C.; Leung, D.; Marsan, N.; et al. Impact of Diabetes and Increasing Body Mass Index Category on Left Ventricular Systolic and Diastolic Function. J. Am. Soc. Echocardiogr. 2018, 31, 916–925. [Google Scholar] [CrossRef]
- Loncarevic, B.; Trifunovic, D.; Soldatovic, I.; Vujisic-Tesic, B. Silent diabetic cardiomyopathy in everyday practice: A clinical and echocardiographic study. BMC Cardiovasc. Disord. 2016, 16. [Google Scholar] [CrossRef]
- Ernande, L.; Bergerot, C.; Rietzschel, E.; De Buyzere, M.; Thibault, H.; PignonBlanc, P.; Croisille, P.; Ovize, M.; Groisne, L.; Moulin, P.; et al. Diastolic Dysfunction in Patients with Type 2 Diabetes Mellitus: Is It Really the First Marker of Diabetic Cardiomyopathy? J. Am. Soc. Echocardiogr. 2011, 24, 1268–1275. [Google Scholar] [CrossRef]
- Cameli, M.; Mandoli, G.; Loiacono, F.; Dini, F.; Henein, M.; Mondillo, S. Left atrial strain: A new parameter for assessment of left ventricular filling pressure. Heart Fail. Rev. 2015, 21, 65–76. [Google Scholar] [CrossRef]
- Henein, M.Y.; Lindqvist, P. Assessment of Left Ventricular Diastolic Function by Doppler Echocardiography. Card. Fail. Rev. 2015, 1, 87–89. [Google Scholar] [CrossRef]
- D’Andrea, A.; Vriz, O.; Ferrara, F.; Cocchia, R.; Conte, M.; Di Maio, M.; Driussi, C.; Scarafile, R.; Martone, F.; Sperlongano, S.; et al. Reference ranges and physiologic variations of left E/e’ ratio in healthy adults: Clinical and echocardiographic correlates. J. Cardiovasc. Echogr. 2018, 28, 101. [Google Scholar] [CrossRef]
- van Grootel, R.; Menting, M.; McGhie, J.; Roos-Hesselink, J.; van den Bosch, A. Echocardiographic chamber quantification in a healthy Dutch population. Neth. Heart J. 2017, 25, 682–690. [Google Scholar] [CrossRef] [Green Version]
- Omar, A.; Narula, S.; Abdel Rahman, M.; Pedrizzetti, G.; Raslan, H.; Rifaie, O.; Narula, J.; Sengupta, P. Precision Phenotyping in Heart Failure and Pattern Clustering of Ultrasound Data for the Assessment of Diastolic Dysfunction. JACC Cardiovasc. Imaging 2017, 10, 1291–1303. [Google Scholar] [CrossRef]
- Gong, F.; Campbell, D.; Prior, D. Noninvasive Cardiac Imaging and the Prediction of Heart Failure Progression in Preclinical Stage A/B Subjects. JACC Cardiovasc. Imaging 2017, 10, 1504–1519. [Google Scholar] [CrossRef]
- Flachskampf, F.; Biering-Sørensen, T.; Solomon, S.; Duvernoy, O.; Bjerner, T.; Smiseth, O. Cardiac Imaging to Evaluate Left Ventricular Diastolic Function. JACC Cardiovasc. Imaging 2015, 8, 1071–1093. [Google Scholar] [CrossRef] [Green Version]
- Plitt, G.; Spring, J.; Moulton, M.; Agrawal, D. Mechanisms, diagnosis, and treatment of heart failure with preserved ejection fraction and diastolic dysfunction. Expert Rev. Cardiovasc. 2018, 16, 579–589. [Google Scholar] [CrossRef]
- Davies, M.; D’Alessio, D.; Fradkin, J.; Kernan, W.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.; Buse, J. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2018, 61, 2461–2498. [Google Scholar] [CrossRef] [Green Version]
- Sakamoto, M.; Matsutani, D.; Kayama, Y. Possibility of a New Therapeutic Strategy for Left Ventricular Dysfunction in Type 2 Diabetes. J. Clin. Med. Res. 2018, 10, 799–805. [Google Scholar] [CrossRef] [Green Version]
- McHugh, K.; DeVore, A.; Wu, J.; Matsouaka, R.; Fonarow, G.; Heidenreich, P.; Yancy, C.; Green, J.; Altman, N.; Hernandez, A. Heart Failure with Preserved Ejection Fraction and Diabetes. JACC 2019, 73, 602–611. [Google Scholar] [CrossRef]
- de Lucia, C.; Sardu, C.; Metzinger, L.; Zuurbier, C. Editorial: Diabetes and Heart Failure: Pathogenesis and Novel Therapeutic Approaches. Front. Physiol. 2019, 10. [Google Scholar] [CrossRef]
- Dunlay, S.; Givertz, M.; Aguilar, D.; Allen, L.; Chan, M.; Desai, A.; Deswal, A.; Dickson, V.; Kosiborod, M.; Lekavich, C.; et al. Type 2 Diabetes Mellitus and Heart Failure: A Scientific Statement From the American Heart Association and the Heart Failure Society of America: This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation 2019, 140. [Google Scholar] [CrossRef]
- Arnett, D.; Blumenthal, R.; Albert, M.; Buroker, A.; Goldberger, Z.; Hahn, E.; Himmelfarb, C.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Circulation 2019. [Google Scholar] [CrossRef]
- Rossignol, P.; Hernandez, A.; Solomon, S.; Zannad, F. Heart failure drug treatment. Lancet 2019, 393, 1034–1044. [Google Scholar] [CrossRef]
- Selmeryd, J.; Henriksen, E.; Leppert, J.; Hedberg, P. Interstudy heterogeneity of definitions of diastolic dysfunction severely affects reported prevalence. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 892–899. [Google Scholar] [CrossRef]
- Bouthoorn, S.; Valstar, G.; Gohar, A.; den Ruijter, H.; Reitsma, H.; Hoes, A.; Rutten, F. The prevalence of left ventricular diastolic dysfunction and heart failure with preserved ejection fraction in men and women with type 2 diabetes: A systematic review and meta-analysis. Diab. Vasc. Dis. Res. 2018, 15, 477–493. [Google Scholar] [CrossRef] [Green Version]
- Reddy, Y.; Carter, R.; Obokata, M.; Redfield, M.; Borlaug, B. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure with Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef]
- Sardu, C.; Marfella, R.; Santamaria, M.; Papini, S.; Parisi, Q.; Sacra, C.; Colaprete, D.; Paolisso, G.; Rizzo, M.; Barbieri, M. Stretch. Injury and Inflammation Markers Evaluation to Predict Clinical Outcomes After Implantable Cardioverter Defibrillator Therapy in Heart Failure Patients with Metabolic Syndrome. Front. Physiol. 2018, 9. [Google Scholar] [CrossRef]
- Meagher, P.; Adam, M.; Civitarese, R.; Bugyei-Twum, A.; Connelly, K. Heart Failure with Preserved Ejection Fraction in Diabetes: Mechanisms and Management. Can. J. Cardiol. 2018, 34, 632–643. [Google Scholar] [CrossRef]







© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grigorescu, E.-D.; Lacatusu, C.-M.; Floria, M.; Mihai, B.-M.; Cretu, I.; Sorodoc, L. Left Ventricular Diastolic Dysfunction in Type 2 Diabetes—Progress and Perspectives. Diagnostics 2019, 9, 121. https://doi.org/10.3390/diagnostics9030121
Grigorescu E-D, Lacatusu C-M, Floria M, Mihai B-M, Cretu I, Sorodoc L. Left Ventricular Diastolic Dysfunction in Type 2 Diabetes—Progress and Perspectives. Diagnostics. 2019; 9(3):121. https://doi.org/10.3390/diagnostics9030121
Chicago/Turabian StyleGrigorescu, Elena-Daniela, Cristina-Mihaela Lacatusu, Mariana Floria, Bogdan-Mircea Mihai, Ioana Cretu, and Laurentiu Sorodoc. 2019. "Left Ventricular Diastolic Dysfunction in Type 2 Diabetes—Progress and Perspectives" Diagnostics 9, no. 3: 121. https://doi.org/10.3390/diagnostics9030121
APA StyleGrigorescu, E.-D., Lacatusu, C.-M., Floria, M., Mihai, B.-M., Cretu, I., & Sorodoc, L. (2019). Left Ventricular Diastolic Dysfunction in Type 2 Diabetes—Progress and Perspectives. Diagnostics, 9(3), 121. https://doi.org/10.3390/diagnostics9030121






