Relationship between Epicardial and Coronary Adipose Tissue and the Expression of Adiponectin, Leptin, and Interleukin 6 in Patients with Coronary Artery Disease
Abstract
1. Introduction
2. Material and Methods
2.1. Study Inclusion Criteria
2.2. Study Population
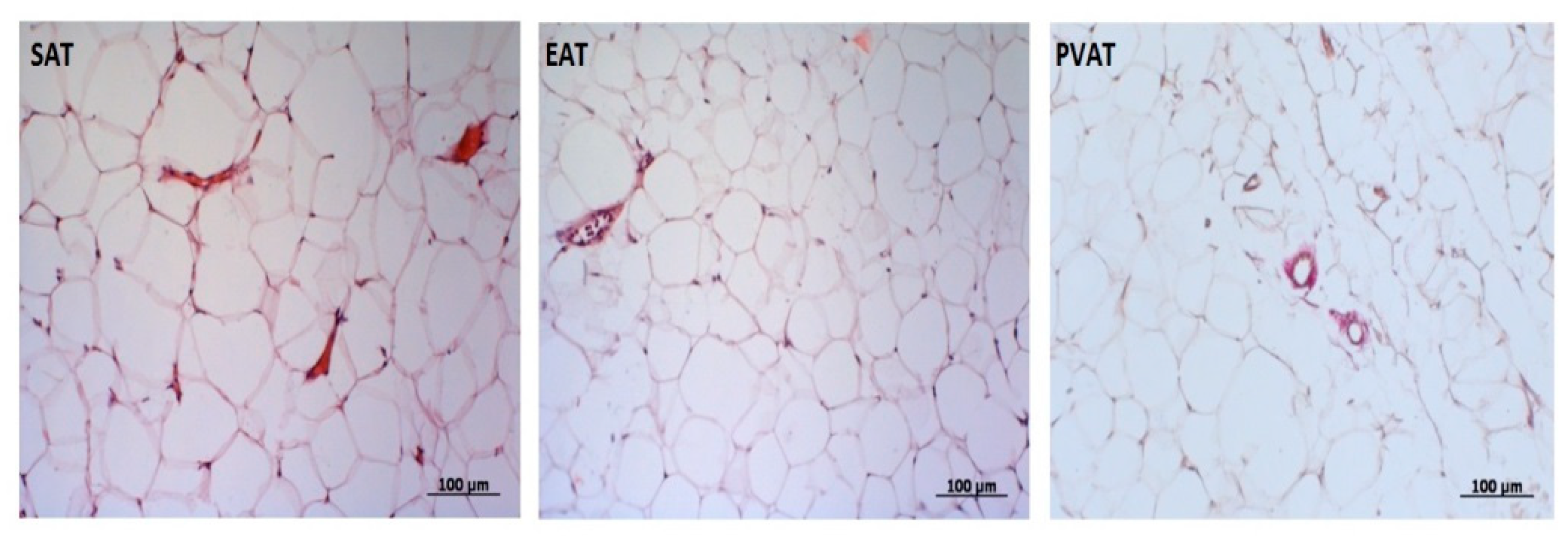
2.3. Measurement of the Area of SAT, EAT, and PVAT
2.4. Cell Collection
2.4.1. Obtaining Biopsies of AT from Various Sites
2.4.2. Adipocyte Extraction and Culture
2.5. Laboratory Assays
2.5.1. RNA Extraction
2.5.2. cDNA Synthesis
2.5.3. Real Time Quantitative Polymerase Chain Reaction (qRT-PCR)
2.5.4. ELISA
2.6. Statistical Analysis
3. Results
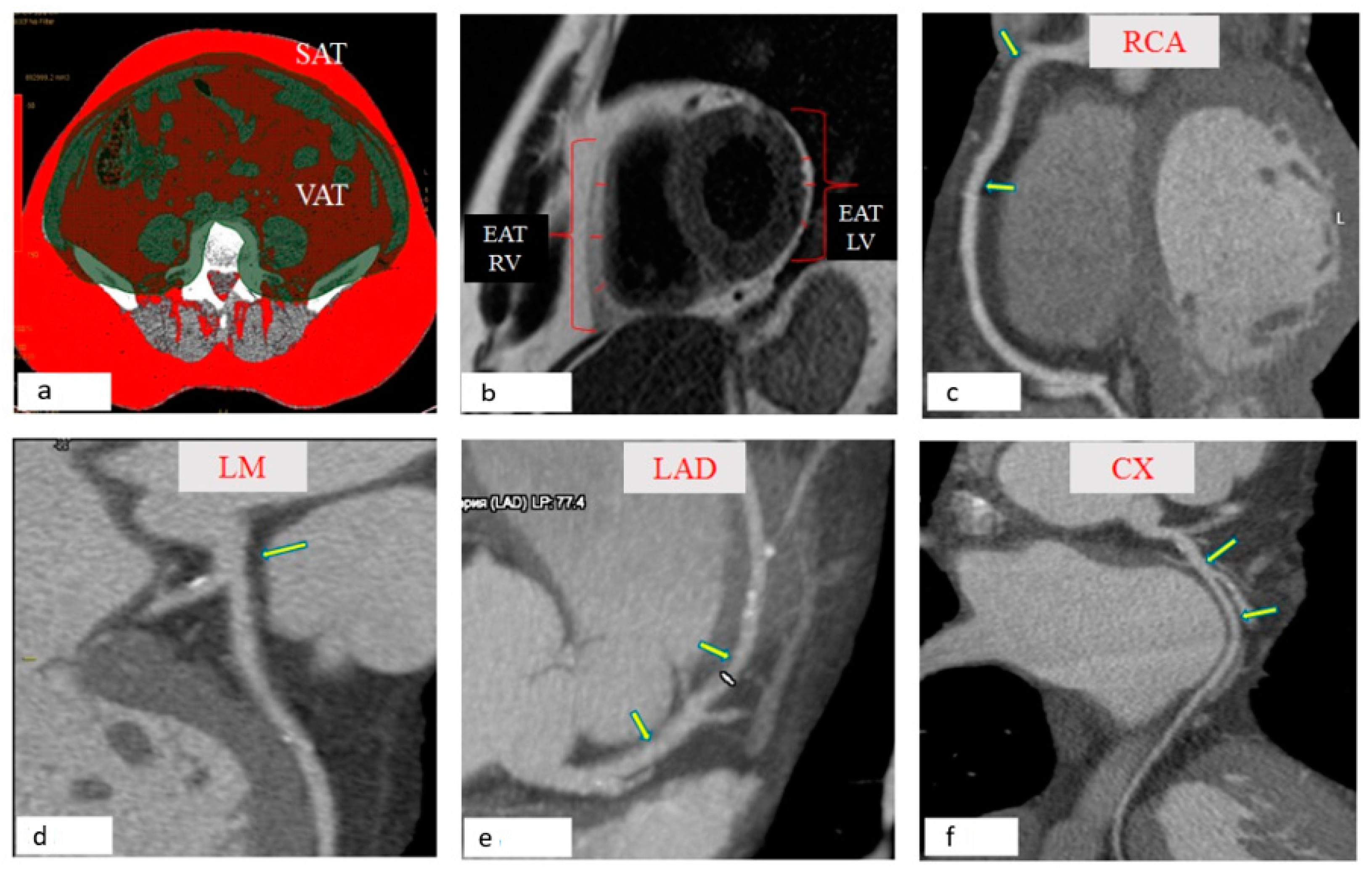
3.1. Visualization of Local Fat Depots (Epicardial, Perivascular, Abdominal) in Patients with Coronary Heart Disease
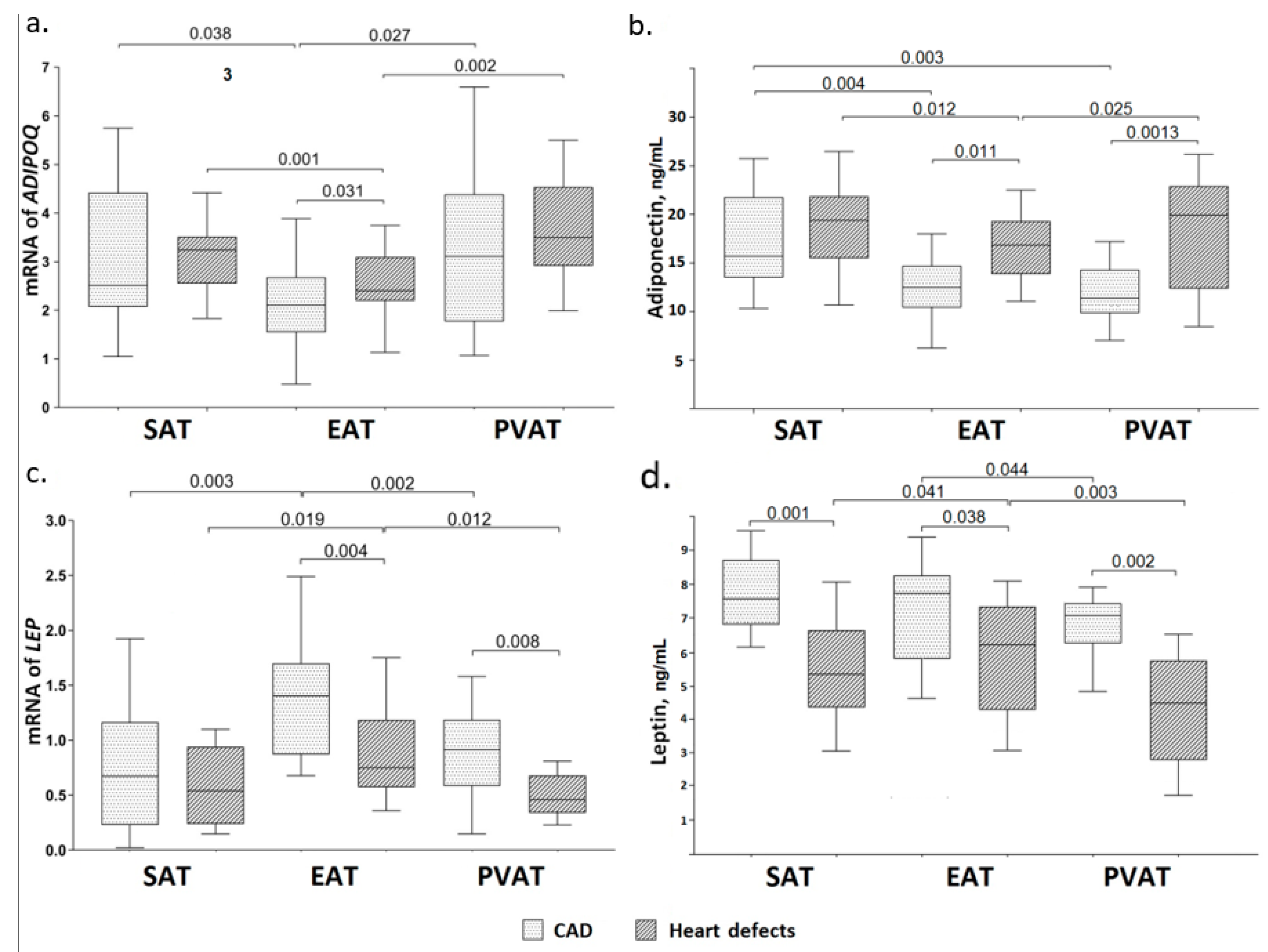
3.2. Adiponectin Gene Expression and Concentration of Adiponectin in the Daily Adipocyte Culture of Various Fat Depots
3.3. Leptin Gene Expression and Concentration of Leptin in the Daily Adipocyte Culture of Various Fat Depots
3.4. IL-6 Gene Expression and Concentration of IL-6 in the Daily Adipocyte Culture of Various Fat Depots
3.5. Relationship between Gene Expression and Secretion of Adipocytokines in AT with Indicators of Morphometric Characteristics of Local Fat Depots of the Heart and Blood Vessels in Patients with CAD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Nakamura, K.; Fuster, J.J.; Walsh, K. Adipokines: A link between obesity and cardiovascular disease. J. Cardiol. 2014, 63, 250–259. [Google Scholar] [CrossRef]
- Tanaka, K.; Fukuda, D.; Sata, M. Roles of epicardial adipose tissue in the pathogenesis of coronary atherosclerosis—An update on recent findings. Circ. J. 2020, 85, 2–8. [Google Scholar] [CrossRef]
- Bambace, C.; Sepe, A.; Zoico, E.; Telesca, M.; Olioso, D.; Venturi, S.; Rossi, A.; Corzato, F.; Faccioli, S.; Cominacini, L.; et al. Inflammatory profile in subcutaneous and epicardial adipose tissue in men with and without diabetes. Heart Vessels 2014, 29, 42–48. [Google Scholar] [CrossRef]
- Anthony, S.R.; Guarnieri, A.R.; Gozdiff, A.; Helsley, R.N.; Owens, A.P., III; Tranter, M. Mechanisms linking adipose tissue inflammation to cardiac hypertrophy and fibrosis. Clin. Sci. 2019, 133, 2329–2344. [Google Scholar] [CrossRef]
- Mahabadi, A.A.; Berg, M.H.; Lehmann, N.; Kalsch, H.; Bauer, M.; Kara, K.; Dragano, N.; Moebus, S.; Jockel, K.H.; Erbel, R.; et al. Association of epicardial fat with cardiovascular risk factors and incident myocardial infarction in the general population. J. Am. Coll. Cardiol. 2013, 61, 1388–1395. [Google Scholar] [CrossRef]
- Bambacea, C.; Telescab, M.; Zoicoa, E.; Sepe, A.; Olioso, D.; Rossi, A.; Corzato, F.; Di Francesco, V.; Mazzucco, A.; Santini, F.; et al. Adiponectin gene expression and adipocyte diameter: A comparison between epicardial and subcutaneous AT in men. Cardiovasc. Pathol. 2011, 20, e153–e156. [Google Scholar] [CrossRef]
- Lehr, S.; Hartwig, S.; Lamers, D.; Famulla, S.; Muller, S.; Hanisch, F.G.; Cuvelier, C.; Ruige, J.; Eckardt, K.; Ouwens, D.M.; et al. Identification and validation of novel adipokines released from primary human adipocytes. Mol. Cell Proteom. 2012, 11, M111.010504. [Google Scholar] [CrossRef]
- Verhagen, S.N.; Visseren, F.L. Perivascular AT as a cause of atherosclerosis. Atherosclerosis 2011, 214, 3–10. [Google Scholar] [CrossRef]
- Gruzdeva, O.V.; Dyleva, Y.A.; Antonova, L.V.; Matveeva, V.G.; Uchasova, E.G.; Fanaskova, E.V.; Karetnikova, V.N.; Ivanov, S.V.; Barbarash, O.L. Adipokine and cytokine profiles of epicardial and subcutaneous at in patients with coronary heart disease. Bull. Exp. Biol. Med. 2017, 163, 608–611. [Google Scholar] [CrossRef]
- Suga, H.; Matsumoto, D.; Inoue, K.; Shigeura, T.; Eto, H.; Aoi, N.; Kato, H.; Abe, H.; Yoshimura, K. Numerical Measurement of Viable and Nonviable Adipocytes and Other Cellular Components in Aspirated Fat Tissue. Plast. Reconstr. Surg. 2008, 122, 103–114. [Google Scholar] [CrossRef]
- Sinitsky, M.Y.; Dyleva, Y.A.; Uchasova, E.G.; Belik, E.V.; Yuzhalin, A.E.; Gruzdeva, O.V.; Matveeva, V.G.; Ponasenko, A.V. Adipokine gene expression in adipocytes isolated from different fat depots of coronary artery disease patients. Arch. Physiol. Biochem. 2019, 1–9. [Google Scholar] [CrossRef]
- Pfaffl, M.W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001, 29, e45. [Google Scholar] [CrossRef]
- Mookadam, F.; Goel, R.; Alharthi, M.S.; Jiamsripong, P.; Cha, S. Epicardial fat and its association with cardiovascular risk: A cross-sectional observational study. Heart Views 2010, 11, 103. [Google Scholar]
- Chu, C.Y.; Lee, W.H.; Hsu, P.C.; Lee, M.K.; Lee, H.H.; Chiu, C.A.; Lin, T.H.; Lee, C.S.; Yen, H.W.; Voon, W.C.; et al. Association of Increased Epicardial Adipose Tissue Thickness With Adverse Cardiovascular Outcomes in Patients With Atrial Fibrillation. Medicine 2016, 95, e2874. [Google Scholar] [CrossRef]
- Guglielmi, V.; Sbraccia, P. Epicardial adipose tissue: At the heart of the obesity complications. Acta Diabetol. 2017, 54, 805–812. [Google Scholar] [CrossRef]
- Ben-Zvi, D.; Savion, N.; Kolodgie, F.; Simon, A.; Fisch, S.; Schafer, K.; Bachner-Hinenzon, N.; Cao, X.; Gertler, A.; Solomon, G.; et al. Local application of leptin antagonist attenuates angiotensin ii-induced ascending aortic aneurysm and cardiac remodeling. J. Am. Heart Assoc. 2016, 5, e003474. [Google Scholar] [CrossRef]
- Trayhurn, P.; Wood, I.S. Signalling role of AT: Adipokines and inflammation in obesity. Biochem. Soc. Trans. 2005, 33, 1078–1081. [Google Scholar] [CrossRef]
- Corradi, D.; Maestri, R.; Callegari, S.; Pastori, P.; Goldoni, M.; Luong, T.V.; Bordi, C. The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovasc. Pathol. 2004, 13, 313–316. [Google Scholar] [CrossRef]
- Iantorno, M.; Soleimanifard, S.; Schar, M.; Brown, T.T.; Bonanno, G.; Barditch-Crovo, P.; Mathews, L.; Lai, S.; Gerstenblith, G.; Weiss, R.G.; et al. Regional coronary endothelial dysfunction is related to the degree of local epicardial fat in people with HIV. Atherosclerosis 2018, 278, 7–14. [Google Scholar] [CrossRef]
- Picard, F.A.; Gueret, P.; Laissy, J.P.; Champagne, S.; Leclercq, F.; Carrie, D.; Juliard, J.M.; Henry, P.; Niarra, R.; Chatellier, G.; et al. Epicardial adipose tissue thickness correlates with the presence and severity of angiographic coronary artery disease in stable patients with chest pain. PLoS ONE 2014, 9, e110005. [Google Scholar] [CrossRef]
- Trayhurn, P. Hypoxia and adipose tissue function and dysfunction in obesity. Physiol. Rev. 2013, 93, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Labuzek, K.; Bułdak, L.; Duława-Bułdak, A.; Bielecka, A.; Krysiak, R.; Madej, A.; Okopien, B. Atorvastatin and fenofibric acid differentially affect the release of adipokines in the visceral and subcutaneous cultures of adipocytes that were obtained from patients with and without mixed dyslipidemia. Pharmacol. Rep. 2011, 63, 1124–1136. [Google Scholar] [CrossRef]
- Alexopoulos, N.; Melek, B.H.; Arepalli, C.D.; Hartlage, G.R.; Chen, Z.; Kim, S.; Raggi, E.S.P. Effect of intensive versus moderate lipid-lowering therapy on epicardial adipose tissue in hyperlipidemic post-menopausal women: A substudy of the BELLES Trial (Beyond endorsed lipid lowering with EBT scanning). JACC 2013, 61, 1956–1961. [Google Scholar] [CrossRef]
- Parisi, V.; Petraglia, L.; D’Esposito, V.; Cabaro, S.; Rengo, G.; Caruso, A.; Grimaldi, M.G.; Baldascino, F.; De Bellis, A.; Vitale, D.; et al. Statin therapy modulates thickness and inflammatory profile of human epicardial adipose tissue. Int. J. Cardiol. 2019, 274, 326–330. [Google Scholar] [CrossRef]
- Ishihara, Y.; Ohmori, K.; Mizukawa, M.; Hasan, A.U.; Noma, T.; Kohno, M. Beneficial direct adipotropic actions of pitavastatin in vitro and their manifestations in obese mice. Atherosclerosis 2010, 212, 131–138. [Google Scholar] [CrossRef]
- Lee, S.; Lee, Y.; Kim, J.; An, J.; Kim, K.; Lee, H.; Kong, H.; Song, Y.; Kim, K. Atorvastatin and rosuvastatin improve physiological parameters and alleviate immune dysfunction in metabolic disorders. Biochem. Biophys. Res. Commun. 2016, 478, 1242–1247. [Google Scholar] [CrossRef]
- Demircelik, M.B.; Yilmaz, O.C.; Gurel, O.M.; Selcoki, Y. Epicardial adipose tissue and pericoronary fat thickness measured with 64-multidetector computed tomography: Potential predictors of the severity of coronary artery disease. Clinics 2014, 69, 388–392. [Google Scholar] [CrossRef]
- Kolodgie, F.D.; Virmani, R.; Cornhill, J.F.; Herderick, E.E.; Smialek, J. Increase in atherosclerosis and adventitial mast cells in cocaine abusers: An alternative mechanism of cocaine-associated coronary vasospasm and thrombosis. J. Am. Coll. Cardiol. 1991, 17, 1553–1560. [Google Scholar] [CrossRef]
- Omar, A.; Chatterjee, T.K.; Tang, Y.; Hui, D.Y.; Weintraub, N.L. Proinflammatory phenotype of perivascular adipocytes. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1631–1636. [Google Scholar] [CrossRef]
- Iacobellis, G.; Pistilli, D.; Gucciardo, M.; Leonetti, F.; Miraldi, F.; Brancaccio, G.; Gallo, P.; di Gioia, C.R.T. Adiponectin expression in human epicardial AT in vivo is lower in patients with coronary artery disease. Cytokine 2005, 29, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Eiras, S.; Teijeira-Fernández, E.; Shamagian, L.G.; Fernandez, A.L.; Vazquez-Boquete, A.; Gonzalez-Juanatey, J.R. Extension of coronary artery disease is associated with increased IL-6 and decreased adiponectin gene expression in epicardial AT. Cytokine 2008, 43, 174–180. [Google Scholar] [CrossRef]
- Iglesias, M.J.; Eiras, S.; Pineiro, R.; Lopez-Otero, D.; Gallego, R.; Fernandez, Á.L.; Lago, F.; González-Juanatey, J.R. Gender differences in adiponectin and leptin expression in epicardial and subcutaneous Adipose Tissue. findings in patients undergoing cardiac surgery. Rev. Esp. Cardiol. 2006, 59, 1252–1260. [Google Scholar] [CrossRef]
- Lee, H.Y.; Despres, J.P.; Koh, K.K. Perivascular AT in the pathogenesis of cardiovascular disease. Atherosclerosis 2013, 230, 177–184. [Google Scholar] [CrossRef]
- Withers, S.B.; Bussey, C.E.; Saxton, S.N.; Melrose, H.M.; Watkins, A.E.; Heagerty, A.M. Mechanisms of adiponectin-associated perivascular function in vascular disease. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1637–1642. [Google Scholar] [CrossRef]
- Cybularz, M.; Langbein, H.; Zatschler, B.; Brunssen, C.; Deussen, A.; Matschke, K.; Morawietz, H. Endothelial function and gene expression in perivascular adipose tissue from internal mammary arteries of obese patients with coronary arterydisease. Atheroscler. Suppl. 2017, 30, 149–158. [Google Scholar] [CrossRef]
- Payne, G.A.; Kohr, M.C.; Tune, J.D. Epicardial perivascular AT as a therapeutic target in obesity-related coronary artery disease. Br. J. Pharmacol. 2012, 165, 659–669. [Google Scholar] [CrossRef]
- Mazurek, T.; Zhang, L.F.; Zalewski, A.; Mannion, J.D.; Diehl, J.T.; Arafat, H.; Sarov-Blat, L.; O’Brien, S.; Keiper, E.A.; Johnson, A.G.; et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 2003, 108, 2460–2466. [Google Scholar] [CrossRef]
- Guo, R.; Han, M.; Song, J.; Liu, J.; Sun, Y. Adiponectin and its receptors are involved in hypertensive vascular injury. Mol. Med. Rep. 2018, 17, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Nacci, C.; Leo, V.; De Benedictis, L.; Potenza, M.A.; Sgarra, L.; De Salvia, M.A.; Quon, M.J.; Montagnani, M. Infliximab therapy restores adiponectin expression in perivascularAT and improves endothelial nitric oxide-mediatedvasodilation in mice with type 1 diabetes. Vasc. Pharmacol. 2016, 87, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Gao, E.; Jiao, X.; Yuan, Y.; Li, S.; Christopher, T.A.; Lopez, B.L.; Koch, W.; Chan, L.; Goldstein, B.J.; et al. Adiponectin cardioprotection after myocardial ischemia/reperfusion involves the reduction of oxidative/nitrative stress. Circulation 2007, 115, 1408–14016. [Google Scholar] [CrossRef] [PubMed]
- Bauche, I.B.; El Mkadem, S.A.; Rezsohazy, R.; Funahashi, T.; Maeda, N.; Miranda, L.M.; Brichard, S.M. Adiponectin downregulates its own production and the expression of its AdipoR2 receptor in transgenic mice. Biochem. Biophys. Res. Commun. 2006, 345, 1414–1424. [Google Scholar] [CrossRef] [PubMed]
- Kadowaki, T. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J. Clin. Investig. 2006, 116, 1784–1792. [Google Scholar] [CrossRef]
- Hasty, A.H.; Shimano, H.; Osuga, J.; Namatame, I.; Takahashi, A.; Yahagi, N.; Perrey, S.; Iizuka, Y.; Tamura, Y.; Amemiya-Kudo, M.; et al. Severe hypercholesterolemia, hypertriglyceridemia, and atherosclerosis in mice lacking both leptin and the low density lipoprotein receptor. J. Biol. Chem. 2001, 276, 37402–37408. [Google Scholar] [CrossRef] [PubMed]
- Gormez, S.; Demirkan, A.; Atalar, F.; Caynak, B.; Erdim, R.; Sozer, V.; Gunay, D.; Akpinar, B.; Ozbek, U.; Buyukdevrim, A.S. Adipose tissue gene expression of adiponectin, tumor necrosis factor alpha and leptin in metabolic syndrome patients with coronary artery disease. Intern. Med. 2011, 50, 805–910. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Polyakova, E.A.; Kolodina, D.A.; Miroshnikova, V.V.; Razgildina, N.D.; Bogdanova, E.O.; Lyapina, E.N.; Belyaeva, O.D.; Pchelina, S.N.; Berkovich, O.A.; Baranova, E.I. Subcutaneous and epicardial adipose tissue leptin gene expression in coronary artery disease patient. Transl. Med. 2019, 6, 25–35. (In Russian) [Google Scholar] [CrossRef]
- Bokeriya, L.A.; Aronov, D.M. Russian clinical guidelines. Coronary artery bypass grafting in patients with ischemic heart disease: Rehabilitation and secondary prevention. Cardiosomatics 2016, 7, 5–71. [Google Scholar] [CrossRef]
- Drosos, I.; Chalikias, G.; Pavlaki, M.; Kareli, D.; Epitropou, G.; Bougioukas, G.; Mikroulis, D.; Konstantinou, F.; Giatromanolaki, A.; Ritis, K.; et al. Differences between perivascular AT surrounding the heart and the internal mammary artery: Possible role for the leptin-inflammation-fibrosis-hypoxia axis. Clin. Res. Cardiol. 2016, 105, 887–900. [Google Scholar] [CrossRef]
- Gotsman, I.; Stabholz, A.; Planer, D.; Pugatsch, T.; Lapidus, L.; Novikov, Y.; Masrawa, S.; Soskolne, A.; Lotan, C. Serum cytokine tumor necrosis factor-alpha and interleukin-6 associated with the severity of coronary artery disease: Indicators of an active inflammatory burden? Isr. Med. Assoc. J. 2008, 10, 494–498. [Google Scholar]
- Dandona, P.; Aljada, A.; Chaudhuri, A.; Mohanty, P.; Garg, R. Metabolic syndrome: A comprehensive perspective based on interaction between obesity, diabetes, and inflammation. Circulation 2005, 111, 1448–1454. [Google Scholar] [CrossRef]
- Shibasaki, I.; Nishikimi, T.; Mochizuki, Y.; Yamada, Y.; Yoshitatsu, M.; Inoue, Y.; Kuwata, T.; Ogawa, H.; Tsuchiya, G.; Ishimitsu, T.; et al. Greater expression of inflammatory cytokines, adrenomedullin, and natriuretic peptide receptor-C in epicardial AT in coronary artery disease. Regul. Pept. 2010, 165, 210–217. [Google Scholar] [CrossRef]
- Yang, R.; Barouch, L.A. Leptin signaling and obesity. Circ. Res. 2007, 101, 545–559. [Google Scholar] [CrossRef] [PubMed]
- Fujimaki, S.; Kanda, T.; Fujita, K.; Tamura, J.; Kobayashi, I. The significance of measuring plasma leptin in acute myocardial infarction. J. Int. Med. Res. 2001, 29, 13–108. [Google Scholar] [CrossRef] [PubMed]
- Hoene, M.; Weigert, C. The role of interleukin-6 in insulin resistence, body fat distribution and energy balance. Obes. Rev. 2008, 9, 20–29. [Google Scholar] [PubMed]
| Parameter | CAD (n = 125) | Heart Defects (n = 120) | p |
|---|---|---|---|
| Men, n (%) | 97 (77.6) | 60 (50) | 0.011 |
| Body mass index, kg/m2 | 28.89 (26.64; 32.12) | 26.78 (23.21; 29.01) | 0.069 |
| Arterial hypertension, n (%) | 118 (94.4) | 32 (26.7) | 0.001 |
| Hypercholesterolemia, n (%) | 31 (24.8) | 16 (13.3) | 0.025 |
| Smoking, n (%) | 90 (72) | 10 (8.3) | 0.0001 |
| Anamnesis | |||
| Family history of CAD, n (%) | 76 (60.8) | 42 (35) | 0.014 |
| History of myocardial infarction, n (%) | 86 (68.8) | 0 | - |
| History of stroke, n (%) | 11 (8.8) | 0 | - |
| Atherosclerosis of other pools, n (%) | 21 (16.8) | 0 | - |
| No angina, n (%) | 8 (6.4) | 120 (100) | 0.0001 |
| Functional class I angina, n (%) | 0 | 0 | - |
| Functional class II angina, n (%) | 51 (40.8) | 0 | - |
| Functional class III angina, n (%) | 66 (52.8) | 0 | - |
| Chronic heart failure NYHA I functional class, n (%) | 16 (12.8) | 26 (21.7) | 0.030 |
| Chronic heart failure NYHA II functional class, n (%) | 11 (8.8) | 54 (45) | 0.0002 |
| Chronic heart failure NYHA III functional class, n (%) | 7 (5.6) | 40 (33.3) | 0.003 |
| Chronic heart failure NYHA IV functional class, n (%) | 0 | 0 | - |
| Atherosclerosis of the 1st coronary artery, n (%) | 10 (8) | 0 | - |
| Atherosclerosis of the 2nd coronary artery, n (%) | 6 (4.8) | 0 | - |
| Atherosclerosis of three or more coronary artery, n (%) | 109 (87.2) | 0 | - |
| Ejection fraction, % | 51.0 (44.13; 56.377) | 53.2 (43.41; 58.03) | 0.125 |
| Treatment strategy/group of drugs (hospital period) | |||
| Aspirin, n (%) | 122 (97.6) | 0 | - |
| Clopidogrel, n (%) | 21 (16.8) | 0 | - |
| Warfarin, n (%) | 0 | 103 (85.8) | - |
| β-blockers, n (%) | 122 (97.6) | 111 (92.5) | 0.312 |
| Angiotensin-converting enzyme, n (%) | 96 (76.8) | 95 (79.2) | 0.247 |
| Statins, n (%) | 125 (100) | 98 (81.7) | 0.033 |
| Calcium channel Blocker, n (%) | 96 (76.8) | 90 (75) | 0.151 |
| Nitrates, n (%) | 11 (8.8) | 10 (8.3) | 0.417 |
| Diuretics, n (%) | 105 (84) | 110 (91.7) | 0.062 |
| Parameters | CAD 1, (n = 125) | Heart Defects, (n = 120) | p |
|---|---|---|---|
| Thickness EAT LV, mm | 3.53 (2.87; 4.36) | 2.76 (2.42; 3.21) | p = 0.022 |
| Thickness EAT RV, mm | 4.58 (4.09; 6.17) | 3.65 (3.12; 3.97) | p = 0.031 |
| Thickness PVAT p/3 RCA, mm | 4.55 (3.53; 5.76) | 2.70 (2.41; 3.29) | p = 0.002 |
| Thickness PVAT m/3 RCA, mm | 4.67 (3.49; 6.13) | 2.63 (2.24; 3.29) | p = 0.003 |
| Thickness PVAT LCA, mm | 3.64 (3.33; 4.46) | 2.77 (2.48; 3.12) | p = 0.027 |
| Thickness PVAT p/3 anterior descending artery, mm | 4.31 (3.51; 4.87) | 3.15 (2.56; 3.03) | p = 0.001 |
| Thickness PVAT m/3 anterior descending artery, mm | 3.71 (3.24; 4.92) | 2.62 (2.16; 2.88) | p = 0.012 |
| Thickness PVAT p/3 circumflex artery, mm | 3.35 (3.12; 4.47) | 2.74 (2.34; 2.93) | p = 0.037 |
| Thickness PVAT m/3 circumflex artery, mm | 3.67 (3.10; 4.99) | 2.55 (2.27; 2.83) | p = 0.002 |
| Area VAT, cm2 | 168.28 (149.21; 198.19) | 136.24 (96.28; 142.13) | p = 0.031 |
| Area SAT, cm2 | 264.51 (190.15; 311.46) | 277.36 (197.12; 344.31) | p = 0.418 |
| Parameters | AUC | p | 95% Confidence Interval (CI) | |
|---|---|---|---|---|
| Thickness EAT LV, mm | 0.871 | p < 0.012 | 0.693 | 0.983 |
| Thickness EAT RV, mm | 0.611 | p < 0.025 | 0.552 | 0.739 |
| Thickness PVAT p/3 RCA, mm | 0.706 | p < 0.031 | 0.708 | 0.979 |
| Thickness PVAT m/3 RCA, mm | 0.649 | p < 0.037 | 0.523 | 0.729 |
| Thickness PVAT LCA, mm | 0.793 | p < 0.022 | 0.642 | 0.937 |
| Thickness PVAT p/3 anterior descending artery, mm | 0.832 | p < 0.014 | 0.704 | 0.956 |
| Thickness PVAT m/3 anterior descending artery, mm | 0.626 | p < 0.033 | 0.686 | 0.769 |
| Thickness PVAT p/3 circumflex artery, mm | 0.771 | p < 0.019 | 0.631 | 0.847 |
| Thickness PVAT m/3 circumflex artery, mm | 0.611 | p < 0.041 | 0.556 | 0.718 |
| Area VAT, cm2 | 0.809 | p < 0.026 | 0.694 | 0.963 |
| Area SAT, cm2 | 0.598 | p < 0.035 | 0.386 | 0.627 |
| Parameter | Subcutaneous Adipocytes | Epicardial Adipocytes | Perivascular Adipocytes | p | ||||
|---|---|---|---|---|---|---|---|---|
| CAD | Heart Defects | CAD | Heart Defects | CAD | Heart Defects | |||
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| IL6 expression, Delta Ct | 0.037 (0.025; 0.051) | 0.053 (0.034; 0.061) | 0.077 (0.062; 0.081) | 0.056 (0.049; 0.075) | 0.048 (0.037; 0.057) | 0.029 (0.021; 0.032) | 0.012 | P1–3 = 0.003 P3–5 = 0.011 P2–6 = 0.0001 P4–6 = 0.0001 |
| P1–2 = 0.124 | P3–4 = 0.002 | P5–6 = 0.0002 | ||||||
| IL-6, pg/mL | 12.37 (9.12; 16.27) | 13.92 (10.01; 16.26) | 29.35 (25.18; 37.16) | 21.55 (17.77; 23.34) | 18.12 (15.61; 21.06) | 11.64 (8.79; 14.17) | 0.011 | P1–3 = 0.0001 P3–5 = 0.0002 P2–4 = 0.022 P4–6 = 0.001 |
| P1–2 = 0.071 | P3–4 = 0.022 | P5–6 = 0.025 | ||||||
| Parameters | Odds Ratio (OR) | 95% Confidence Interval (CI) | p | |
|---|---|---|---|---|
| ADIPOQ expression in EAT | 0.47 | 0.39 | 0.53 | p = 0.013 |
| ADIPOQ expression in PVAT | 0.63 | 0.55 | 0.71 | p = 0.002 |
| LEP expression in EAT | 1.54 | 1.44 | 1.60 | p = 0.022 |
| IL6 expression in EAT | 1.51 | 1.43 | 1.59 | p = 0.002 |
| IL6 expression in PVAT | 1.41 | 1.35 | 1.50 | p = 0.002 |
| Adiponectin concentration in EAT | 0.55 | 0.46 | 0.61 | p = 0.001 |
| Leptin concentration in EAT | 2.52 | 2.46 | 2.60 | p = 0.014 |
| Leptin concentration in PVAT | 2.34 | 2.25 | 2.40 | p = 0.001 |
| IL-6 concentration in EAT | 1.49 | 1.40 | 1.58 | p = 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gruzdeva, O.V.; Dyleva, Y.A.; Belik, E.V.; Sinitsky, M.Y.; Stasev, A.N.; Kokov, A.N.; Brel, N.K.; Krivkina, E.O.; Bychkova, E.E.; Tarasov, R.S.; et al. Relationship between Epicardial and Coronary Adipose Tissue and the Expression of Adiponectin, Leptin, and Interleukin 6 in Patients with Coronary Artery Disease. J. Pers. Med. 2022, 12, 129. https://doi.org/10.3390/jpm12020129
Gruzdeva OV, Dyleva YA, Belik EV, Sinitsky MY, Stasev AN, Kokov AN, Brel NK, Krivkina EO, Bychkova EE, Tarasov RS, et al. Relationship between Epicardial and Coronary Adipose Tissue and the Expression of Adiponectin, Leptin, and Interleukin 6 in Patients with Coronary Artery Disease. Journal of Personalized Medicine. 2022; 12(2):129. https://doi.org/10.3390/jpm12020129
Chicago/Turabian StyleGruzdeva, Olga V., Yulia A. Dyleva, Ekaterina V. Belik, Maxim Y. Sinitsky, Aleksandr N. Stasev, Aleksandr N. Kokov, Natalia K. Brel, Evgenia O. Krivkina, Evgenia E. Bychkova, Roman S. Tarasov, and et al. 2022. "Relationship between Epicardial and Coronary Adipose Tissue and the Expression of Adiponectin, Leptin, and Interleukin 6 in Patients with Coronary Artery Disease" Journal of Personalized Medicine 12, no. 2: 129. https://doi.org/10.3390/jpm12020129
APA StyleGruzdeva, O. V., Dyleva, Y. A., Belik, E. V., Sinitsky, M. Y., Stasev, A. N., Kokov, A. N., Brel, N. K., Krivkina, E. O., Bychkova, E. E., Tarasov, R. S., & Barbarash, O. L. (2022). Relationship between Epicardial and Coronary Adipose Tissue and the Expression of Adiponectin, Leptin, and Interleukin 6 in Patients with Coronary Artery Disease. Journal of Personalized Medicine, 12(2), 129. https://doi.org/10.3390/jpm12020129






