Specific Therapy for T2 Asthma
Abstract
:1. Background
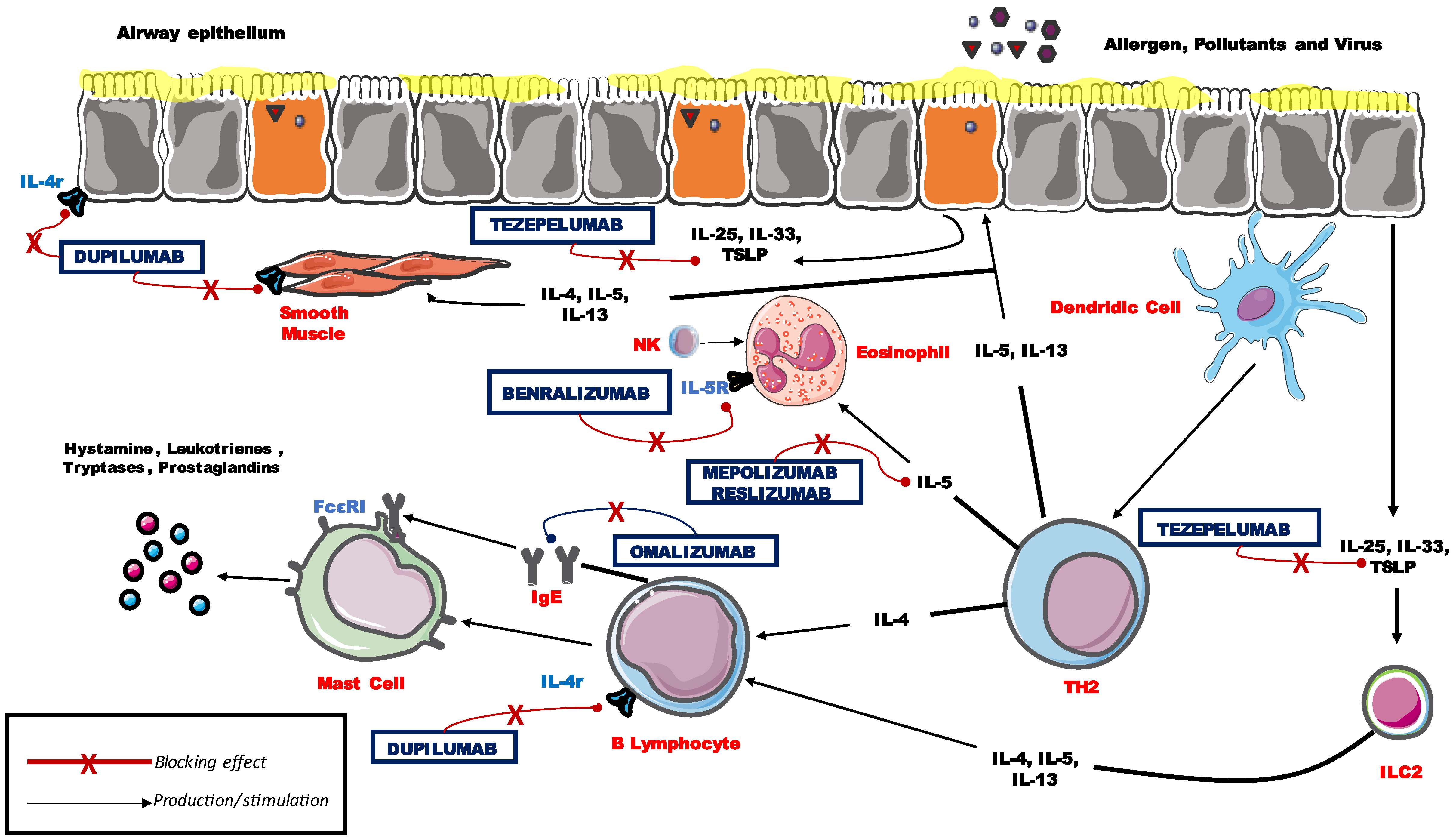
2. Identification of T2 Asthma
3. Current Therapies in Severe Asthma
4. Anti-IgE
Real-Life Experience with Omalizumab
5. Anti-IL-5 and IL-5Rα blockers
5.1. MEP in Real Life
5.2. RES in Real Life
5.3. BEN in Real Life
6. Anti-IL-4r
DUP in Real Life
7. Blocking Antibodies Targeting Epithelial Cell-Derived Cytokines
8. Future Perspective and Unmet Needs
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kyriakopoulos, C.; Gogali, A.; Bartziokas, K.; Kostikas, K. Identification and Treatment of T2-Low Asthma in the Era of Biologics. ERJ Open Res. 2021, 7, 00309-2020. [Google Scholar] [CrossRef] [PubMed]
- Kuruvilla, M.E.; Lee, F.E.H.; Lee, G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2018, 56, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, P.G.; Modrek, B.; Choy, D.F.; Jia, G.; Abbas, A.R.; Ellwanger, A.; Arron, J.R.; Koth, L.L.; Fahy, J.V. T-Helper Type 2-Driven Inflammation Defines Major Subphenotypes of Asthma. Am. J. Respir. Crit. Care Med. 2009, 180, 388–395. [Google Scholar] [CrossRef]
- Konradsen, J.R.; Skantz, E.; Nordlund, B.; Lidegran, M.; James, A.; Ono, J.; Ohta, S.; Izuhara, K.; Dahlén, S.E.; Alving, K.; et al. Predicting Asthma Morbidity in Children Using Proposed Markers of Th2-Type Inflammation. Pediatr. Allergy Immunol. 2015, 26, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Verstraete, K.; Peelman, F.; Braun, H.; Lopez, J.; van Rompaey, D.; Dansercoer, A.; Vandenberghe, I.; Pauwels, K.; Tavernier, J.; Lambrecht, B.N.; et al. Structure and Antagonism of the Receptor Complex Mediated by Human TSLP in Allergy and Asthma. Nat. Commun. 2017, 8, 14937. [Google Scholar] [CrossRef] [Green Version]
- Matera, M.G.; Rogliani, P.; Calzetta, L.; Cazzola, M. TSLP Inhibitors for Asthma: Current Status and Future Prospects. Drugs 2020, 80, 449–458. [Google Scholar] [CrossRef]
- Fildan, A.P.; Rajnoveanu, R.-M.; Cirjaliu, R.; Pohrib, I.; Tudorache, E.; Ilie, A.C.; Oancea, C.; Tofolean, D. Biological Therapies Targeting the Type 2 Inflammatory Pathway in Severe Asthma (Review). Exp. Ther. Med. 2021, 22, 1263. [Google Scholar] [CrossRef]
- Rogliani, P.; Calzetta, L.; Matera, M.G.; Laitano, R.; Ritondo, B.L.; Hanania, N.A.; Cazzola, M. Severe Asthma and Biological Therapy: When, Which, and for Whom. Pulm. Ther. 2020, 6, 47–66. [Google Scholar] [CrossRef] [Green Version]
- Kubo, M. Innate and Adaptive Type 2 Immunity in Lung Allergic Inflammation. Immunol. Rev. 2017, 278, 162–172. [Google Scholar] [CrossRef]
- Gandhi, N.A.; Bennett, B.L.; Graham, N.M.H.; Pirozzi, G.; Stahl, N.; Yancopoulos, G.D. Targeting Key Proximal Drivers of Type 2 Inflammation in Disease. Nat. Rev. Drug Discov. 2016, 15, 35–50. [Google Scholar] [CrossRef]
- Robinson, D.; Humbert, M.; Buhl, R.; Cruz, A.A.; Inoue, H.; Korom, S.; Hanania, N.A.; Nair, P. Revisiting Type 2-High and Type 2-Low Airway Inflammation in Asthma: Current Knowledge and Therapeutic Implications. Clin. Exp. Allergy 2017, 47, 161–175. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, J.A.; Panettieri, R. Treatment of Severe, Uncontrolled Eosinophilic Asthma: Where We Are Heading. J. Asthma 2018, 56, 459–472. [Google Scholar] [CrossRef] [PubMed]
- Parulekar, A.D.; Diamant, Z.; Hanania, N.A. Role of Biologics Targeting Type 2 Airway Inflammation in Asthma: What Have We Learned so Far? Curr. Opin. Pulm. Med. 2017, 23, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takatsu, K.; Nakajima, H. IL-5 and Eosinophilia. Curr. Opin. Immunol. 2008, 20, 288–294. [Google Scholar] [CrossRef]
- Licari, A.; Manti, S.; Castagnoli, R.; Marseglia, A.; Foiadelli, T.; Brambilla, I.; Marseglia, G.L. Immunomodulation in Pediatric Asthma. Front. Pediatr. 2019, 7, 289. [Google Scholar] [CrossRef]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS Guidelines on Definition, Evaluation and Treatment of Severe Asthma. Eur. Respir. J. 2014, 43, 343–373. [Google Scholar] [CrossRef] [Green Version]
- Bagnasco, D.; Caminati, M.; Passalacqua, G. Biologicals for Severe Asthma: What We Can Learn from Real-Life Experiences? Curr. Opin. Allergy Clin. Immunol. 2020, 20, 64–70. [Google Scholar] [CrossRef]
- Solidoro, P.; Nicola, S.; Ridolfi, I.; Canonica, G.W.; Blasi, F.; Paggiaro, P.; Heffler, E.; Bagnasco, D.; Patrucco, F.; Ribolla, F.; et al. Biologics in Severe Eosinophilic Asthma: Three-Year Follow-Up in a SANI Single Center. Biomedicines 2022, 10, 200. [Google Scholar] [CrossRef]
- Hanania, N.A.; Wenzel, S.; Roseń, K.; Hsieh, H.J.; Mosesova, S.; Choy, D.F.; Lal, P.; Arron, J.R.; Harris, J.M.; Busse, W. Exploring the Effects of Omalizumab in Allergic Asthma: An Analysis of Biomarkers in the EXTRA Study. Am. J. Respir. Crit. Care Med. 2013, 187, 804–811. [Google Scholar] [CrossRef]
- Omalizumab Approval. Available online: https://www.ema.europa.eu/en/documents/product-information/xolair-epar-product-information_en.pdf (accessed on 28 March 2022).
- Brusselle, G.G.; Koppelman, G.H. Biologic Therapies for Severe Asthma. N. Engl. J. Med. 2022, 386, 157–171. [Google Scholar] [CrossRef]
- Lombardi, C.; Asero, R.; Bagnasco, D.; Blasi, F.; Bonini, M.; Bussi, M.; Canevari, R.F.; Canonica, G.W.; Castelnuovo, P.; Cecchi, L.; et al. ARIA-ITALY Multidisciplinary Consensus on Nasal Polyposis and Biological Treatments. World Allergy Organ. J. 2021, 14, 100592. [Google Scholar] [CrossRef] [PubMed]
- Bidder, T.; Sahota, J.; Rennie, C.; Lund, V.J.; Robinson, D.S.; Kariyawasam, H.H. Omalizumab Treats Chronic Rhinosinusitis with Nasal Polyps and Asthma Together-a Real Life Study. Rhinology 2018, 56, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Busse, W.; Corren, J.; Lanier, B.Q.; McAlary, M.; Fowler-Taylor, A.; della Cioppa, G.; Gupta, N. Omalizumab, Anti-IgE Recombinant Humanized Monoclonal Antibody, for the Treatment of Severe Allergic Asthma. J. Allergy Clin. Immunol. 2001, 108, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Beasley, R.; Ayres, J.; Slavin, R.; Hébert, J.; Bousquet, J.; Beeh, K.M.; Ramos, S.; Canonica, G.W.; Hedgecock, S.; et al. Benefits of Omalizumab as Add-on Therapy in Patients with Severe Persistent Asthma Who Are Inadequately Controlled despite Best Available Therapy (GINA 2002 Step 4 Treatment): INNOVATE. Allergy Eur. J. Allergy Clin. Immunol. 2005, 60, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Agache, I.; Beltran, J.; Akdis, C.; Akdis, M.; Canelo-Aybar, C.; Canonica, G.W.; Casale, T.; Chivato, T.; Corren, J.; del Giacco, S.; et al. Efficacy and Safety of Treatment with Biologicals (Benralizumab, Dupilumab, Mepolizumab, Omalizumab and Reslizumab) for Severe Eosinophilic Asthma. A Systematic Review for the EAACI Guidelines—Recommendations on the Use of Biologicals in Severe Asthma. Allergy 2020, 75, 1023–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solèr, M.; Matz, J.; Townley, R.; Buhl, R.; O’Brien, J.; Fox, H.; Thirlwell, J.; Gupta, N.; della Cioppa, G. The Anti-IgE Antibody Omalizumab Reduces Exacerbations and Steroid Requirement in Allergic Asthmatics. Eur. Respir. J. 2001, 18, 254–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casale, T.B.; Luskin, A.T.; Busse, W.; Zeiger, R.S.; Trzaskoma, B.; Yang, M.; Griffin, N.M.; Chipps, B.E. Omalizumab Effectiveness by Biomarker Status in Patients with Asthma: Evidence From PROSPERO, A Prospective Real-World Study. J. Allergy Clin. Immunol. Pract. 2019, 7, 156–164.e1. [Google Scholar] [CrossRef]
- Heffler, E.; Saccheri, F.; Bartezaghi, M.; Canonica, G.W. Effectiveness of Omalizumab in Patients with Severe Allergic Asthma with and without Chronic Rhinosinusitis with Nasal Polyps: A PROXIMA Study Post Hoc Analysis. Clin. Transl. Allergy 2020, 10, 25. [Google Scholar] [CrossRef]
- Namazy, J.A.; Blais, L.; Andrews, E.B.; Scheuerle, A.E.; Cabana, M.D.; Thorp, J.M.; Umetsu, D.T.; Veith, J.H.; Sun, D.; Kaufman, D.G.; et al. Pregnancy Outcomes in the Omalizumab Pregnancy Registry and a Disease-Matched Comparator Cohort. J. Allergy Clin. Immunol. 2020, 145, 528–536.e1. [Google Scholar] [CrossRef] [Green Version]
- Beasley, R.; Harper, J.; Masoli, M. Anti-Interleukin-5 Therapy in Patients with Severe Asthma: From Clinical Trials to Clinical Practice. Lancet Respir. Med. 2020, 8, 425–427. [Google Scholar] [CrossRef]
- Bagnasco, D.; Ferrando, M.; Caminati, M.; Bragantini, A.; Puggioni, F.; Varricchi, G.; Passalacqua, G.; Canonica, G.W. Targeting Interleukin-5 or Interleukin-5Rα: Safety Considerations. Drug Saf. 2017, 40, 559–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mavissakalian, M.; Brady, S. The Current State of Biologic Therapies for Treatment of Refractory Asthma. Clin. Rev. Allergy Immunol. 2020, 59, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Leckie, M.J.; ten Brinke, A.; Khan, J.; Diamant, Z.; O’xonnor, B.J.; Walls, C.M.; Mathur, A.K.; Cowley, H.C.; Chung, K.F.; Djukanovic, R.; et al. Effects of an Interleukin-5 Blocking Monoclonal Antibody on Eosinophils, Airway Hyper-Responsiveness, and the Late Asthmatic Response. Lancet 2000, 356, 2144–2148. [Google Scholar] [CrossRef]
- Pavord, I.D.; Korn, S.; Howarth, P.; Bleecker, E.R.; Buhl, R.; Keene, O.N.; Ortega, H.; Chanez, P. Mepolizumab for Severe Eosinophilic Asthma (DREAM): A Multicentre, Double-Blind, Placebo-Controlled Trial. Lancet 2012, 380, 651–659. [Google Scholar] [CrossRef]
- Bel, E.H.; Wenzel, S.E.; Thompson, P.J.; Prazma, C.M.; Keene, O.N.; Yancey, S.W.; Ortega, H.G.; Pavord, I.D. Oral Glucocorticoid-Sparing Effect of Mepolizumab in Eosinophilic Asthma. N. Engl. J. Med. 2014, 371, 1189–1197. [Google Scholar] [CrossRef]
- Ortega, H.G.; Liu, M.C.; Pavord, I.D.; Brusselle, G.G.; FitzGerald, J.M.; Chetta, A.; Humbert, M.; Katz, L.E.; Keene, O.N.; Yancey, S.W.; et al. Mepolizumab Treatment in Patients with Severe Eosinophilic Asthma. N. Engl. J. Med. 2014, 371, 1198–1207. [Google Scholar] [CrossRef] [Green Version]
- Chupp, G.L.; Bradford, E.S.; Albers, F.C.; Bratton, D.J.; Wang-Jairaj, J.; Nelsen, L.M.; Trevor, J.L.; Magnan, A.; ten Brinke, A. Efficacy of Mepolizumab Add-on Therapy on Health-Related Quality of Life and Markers of Asthma Control in Severe Eosinophilic Asthma (MUSCA): A Randomised, Double-Blind, Placebo-Controlled, Parallel-Group, Multicentre, Phase 3b Trial. Lancet Respir. Med. 2017, 5, 390–400. [Google Scholar] [CrossRef]
- Bagnasco, D.; Caminati, M.; Menzella, F.; Milanese, M.; Rolla, G.; Lombardi, C.; Bucca, C.; Heffler, E.; Paoletti, G.; Testino, E.; et al. One Year of Mepolizumab. Efficacy and Safety in Real-Life in Italy. Pulm. Pharmacol. Ther. 2019, 58, 101836. [Google Scholar] [CrossRef]
- Bagnasco, D.; Menzella, F.; Caminati, M.; Caruso, C.; Guida, G.; Bonavia, M.; Riccio, A.; Milanese, M.; Manfredi, A.; Senna, G.; et al. Efficacy of Mepolizumab in Patients with Previous Omalizumab Treatment Failure: Real-Life Observation. Allergy Eur. J. Allergy Clin. Immunol. 2019, 74, 2539–2541. [Google Scholar] [CrossRef]
- Lombardi, C.; Bagnasco, D.; Caruso, C.; D’Amato, M.; Menzella, F.; Milanese, M.; Senna, G.; Canonica, G.W.; Passalacqua, G. Analysis of the Drop-out Rate in Patients Receiving Mepolizumab for Severe Asthma in Real Life. Pulm. Pharmacol. Ther. 2019, 54, 87–89. [Google Scholar] [CrossRef]
- Pelaia, C.; Busceti, M.T.; Solinas, S.; Terracciano, R.; Pelaia, G. Real-Life Evaluation of the Clinical, Functional, and Hematological Effects of Mepolizumab in Patients with Severe Eosinophilic Asthma: Results of a Single-Centre Observational Study. Pulm. Pharmacol. Ther. 2018, 53, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bruno, S.; Gianna, C.; Elena, B.; Marco, S.; Elisiana, C.G.; Corrado, P.; Pierachille, S.; Mauro, M.; Simonetta, M.; Corsico, A.; et al. Mepolizumab Effectiveness on Small Airway Obstruction, Corticosteroid Sparing and Maintenance Therapy Step-down in Real Life. Pulm. Pharmacol. Ther. 2020, 61, 101899. [Google Scholar] [CrossRef]
- Harrison, T.; Canonica, G.W.; Chupp, G.; Lee, J.; Schleich, F.; Welte, T.; Valero, A.; Gemzoe, K.; Maxwell, A.; Joksaite, S.; et al. Real-World Mepolizumab in the Prospective Severe Asthma REALITI-A Study: Initial Analysis. Eur. Respir. J. 2020, 56, 2000151. [Google Scholar] [CrossRef] [PubMed]
- Lugogo, N.; Domingo, C.; Chanez, P.; Leigh, R.; Gilson, M.J.; Price, R.G.; Yancey, S.W.; Ortega, H.G. Long-Term Efficacy and Safety of Mepolizumab in Patients with Severe Eosinophilic Asthma: A Multi-Center, Open-Label, Phase IIIb Study. Clin. Ther. 2016, 38, 2058–2070.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khatri, S.; Moore, W.; Gibson, P.G.; Leigh, R.; Bourdin, A.; Maspero, J.; Barros, M.; Buhl, R.; Howarth, P.; Albers, F.C.; et al. Assessment of the Long-Term Safety of Mepolizumab and Durability of Clinical Response in Patients with Severe Eosinophilic Asthma. J. Allergy Clin. Immunol. 2019, 143, 1742–1751.e7. [Google Scholar] [CrossRef] [Green Version]
- Khurana, S.; Brusselle, G.G.; Bel, E.H.; FitzGerald, J.M.; Masoli, M.; Korn, S.; Kato, M.; Albers, F.C.; Bradford, E.S.; Gilson, M.J.; et al. Long-Term Safety and Clinical Benefit of Mepolizumab in Patients with the Most Severe Eosinophilic Asthma: The COSMEX Study. Clin. Ther. 2019, 41, 2041–2056.e5. [Google Scholar] [CrossRef] [Green Version]
- Corren, J.; Weinstein, S.; Janka, L.; Zangrilli, J.; Garin, M. Phase 3 Study of Reslizumab in Patients with Poorly Controlled Asthma: Effects Across a Broad Range of Eosinophil Counts. Chest 2016, 150, 799–810. [Google Scholar] [CrossRef] [Green Version]
- Castro, M.; Zangrilli, J.; Wechsler, M.E.; Bateman, E.D.; Brusselle, G.G.; Bardin, P.; Murphy, K.; Maspero, J.F.; O’Brien, C.; Korn, S. Reslizumab for Inadequately Controlled Asthma with Elevated Blood Eosinophil Counts: Results from Two Multicentre, Parallel, Double-Blind, Randomised, Placebo-Controlled, Phase 3 Trials. Lancet Respir. Med. 2015, 3, 355–366. [Google Scholar] [CrossRef]
- FitzGerald, J.M.; Bleecker, E.R.; Nair, P.; Korn, S.; Ohta, K.; Lommatzsch, M.; Ferguson, G.T.; Busse, W.W.; Barker, P.; Sproule, S.; et al. Benralizumab, an Anti-Interleukin-5 Receptor α Monoclonal Antibody, as Add-on Treatment for Patients with Severe, Uncontrolled, Eosinophilic Asthma (CALIMA): A Randomised, Double-Blind, Placebo-Controlled Phase 3 Trial. Lancet 2016, 388, 2128–2141. [Google Scholar] [CrossRef]
- Bleecker, E.R.; FitzGerald, J.M.; Chanez, P.; Papi, A.; Weinstein, S.F.; Barker, P.; Sproule, S.; Gilmartin, G.; Aurivillius, M.; Werkström, V.; et al. Efficacy and Safety of Benralizumab for Patients with Severe Asthma Uncontrolled with High-Dosage Inhaled Corticosteroids and Long-Acting Β2-Agonists (SIROCCO): A Randomised, Multicentre, Placebo-Controlled Phase 3 Trial. Lancet 2016, 388, 2115–2127. [Google Scholar] [CrossRef]
- Laviolette, M.; Gossage, D.L.; Gauvreau, G.; Leigh, R.; Olivenstein, R.; Katial, R.; Busse, W.W.; Wenzel, S.; Wu, Y.; Datta, V.; et al. Effects of Benralizumab on Airway Eosinophils in Asthma with Sputum Eosinophilia. J. Allergy Clin. Immunol. 2013, 132, 1086–1096.e5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menzies-Gow, A.; Corren, J.; Bourdin, A.; Chupp, G.; Israel, E.; Wechsler, M.E.; Brightling, C.E.; Griffiths, J.M.; Hellqvist, Å.; Bowen, K.; et al. Tezepelumab in Adults and Adolescents with Severe, Uncontrolled Asthma. N. Engl. J. Med. 2021, 384, 1800–1809. [Google Scholar] [CrossRef] [PubMed]
- Diver, S.; Khalfaoui, L.; Emson, C.; Wenzel, S.E.; Menzies-Gow, A.; Wechsler, M.E.; Johnston, J.; Molfino, N.; Parnes, J.R.; Megally, A.; et al. Effect of Tezepelumab on Airway Inflammatory Cells, Remodelling, and Hyperresponsiveness in Patients with Moderate-to-Severe Uncontrolled Asthma (CASCADE): A Double-Blind, Randomised, Placebo-Controlled, Phase 2 Trial. Lancet Respir. Med. 2021, 9, 1299–1312. [Google Scholar] [CrossRef]
- Sverrild, A.; Hansen, S.; Hvidtfeldt, M.; Clausson, C.M.; Cozzolino, O.; Cerps, S.; Uller, L.; Backer, V.; Erjefält, J.; Porsbjerg, C. The Effect of Tezepelumab on Airway Hyperresponsiveness to Mannitol in Asthma (UPSTREAM). Eur. Respir. J. 2022, 59, 2101296. [Google Scholar] [CrossRef]
- Bagnasco, D.; Povero, M.; Pradelli, L.; Brussino, L.; Rolla, G.; Caminati, M.; Menzella, F.; Heffler, E.; Canonica, G.W.; Paggiaro, P.; et al. Economic Impact of Mepolizumab in Uncontrolled Severe Eosinophilic Asthma, in Real Life. World Allergy Organ. J. 2021, 14, 100509. [Google Scholar] [CrossRef]
- Kavanagh, J.E.; d’Ancona, G.; Elstad, M.; Green, L.; Fernandes, M.; Thomson, L.; Roxas, C.; Dhariwal, J.; Nanzer, A.M.; Kent, B.D.; et al. Real-World Effectiveness and the Characteristics of a “Super-Responder” to Mepolizumab in Severe Eosinophilic Asthma. Chest 2020, 158, 491–500. [Google Scholar] [CrossRef]
- Bodtger, U.; Pedersen, L.; Andersson, E.A.; Henriksen, D.P.; Norgaard, O.; Maltbaek, N.; Madsen, H.; Madsen, L.K.; Chawes, B.L.; Sidenius, K. Efficacy, Adverse Events, and Inter-Drug Comparison of Mepolizumab and Reslizumab Anti-IL-5 Treatments of Severe Asthma—A Systematic Review and Meta-Analysis. Eur. Clin. Respir. J. 2018, 5, 1536097. [Google Scholar] [CrossRef] [Green Version]
- Murphy, K.; Jacobs, J.; Bjermer, L.; Fahrenholz, J.M.; Shalit, Y.; Garin, M.; Zangrilli, J.; Castro, M. Long-Term Safety and Efficacy of Reslizumab in Patients with Eosinophilic Asthma. J. Allergy Clin. Immunol. Pract. 2017, 5, 1572–1581.e3. [Google Scholar] [CrossRef]
- de Llano, L.A.P.; Cosío, B.G.; Astiárraga, I.L.; Campos, G.S.; Alonso, M.Á.T.; Malanda, N.M.; Galo, A.P.; Landa, I.U.; de la Rosa, F.J.M.; García-Moguel, I. Asthma Control in Patients with Severe Eosinophilic Asthma Treated with Reslizumab: Spanish Real-Life Data. J. Asthma Allergy 2022, 15, 79–88. [Google Scholar] [CrossRef]
- Kavanagh, J.E.; Hearn, A.P.; Dhariwal, J.; D’Ancona, G.; Douiri, A.; Roxas, C.; Fernandes, M.; Green, L.; Thomson, L.; Nanzer, A.M.; et al. Real-World Effectiveness of Benralizumab in Severe Eosinophilic Asthma. Chest 2021, 159, 496–506. [Google Scholar] [CrossRef]
- Bagnasco, D.; Brussino, L.; Bonavia, M.; Calzolari, E.; Caminati, M.; Caruso, C.; D’Amato, M.; de Ferrari, L.; di Marco, F.; Imeri, G.; et al. Efficacy of Benralizumab in Severe Asthma in Real Life and Focus on Nasal Polyposis. Respir. Med. 2020, 171, 106080. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.J.; Harrison, T.; Menzella, F.; Shih, V.H.; Burden, A.; Gil, E.G. Identifying Super-Responders to Benralizumab in Severe Asthma. Eur. Respir. J. 2021, 58, PA3734. [Google Scholar] [CrossRef]
- Wenzel, S.; Castro, M.; Corren, J.; Maspero, J.; Wang, L.; Zhang, B.; Pirozzi, G.; Sutherland, E.R.; Evans, R.R.; Joish, V.N.; et al. Dupilumab Efficacy and Safety in Adults with Uncontrolled Persistent Asthma despite Use of Medium-to-High-Dose Inhaled Corticosteroids plus a Long-Acting Β2 Agonist: A Randomised Double-Blind Placebo-Controlled Pivotal Phase 2b Dose-Ranging Trial. Lancet 2016, 388, 31–44. [Google Scholar] [CrossRef]
- Menzies-Gow, A.; Mansur, A.H.; Brightling, C.E. Clinical Utility of Fractional Exhaled Nitric Oxide in Severe Asthma Management. Eur. Respir. J. 2020, 55, 1901633. [Google Scholar] [CrossRef]
- Castro, M.; Corren, J.; Pavord, I.D.; Maspero, J.; Wenzel, S.; Rabe, K.F.; Busse, W.W.; Ford, L.; Sher, L.; FitzGerald, J.M.; et al. Dupilumab Efficacy and Safety in Moderate-to-Severe Uncontrolled Asthma. N. Engl. J. Med. 2018, 378, 2486–2496. [Google Scholar] [CrossRef]
- Dupin, C.; Belhadi, D.; Guilleminault, L.; Gamez, A.S.; Berger, P.; de Blay, F.; Bonniaud, P.; Leroyer, C.; Mahay, G.; Girodet, P.O.; et al. Effectiveness and Safety of Dupilumab for the Treatment of Severe Asthma in a Real-Life French Multi-Centre Adult Cohort. Clin. Exp. Allergy 2020, 50, 789–798. [Google Scholar] [CrossRef]
- Menzella, F.; Montanari, G.; Patricelli, G.; Cavazza, A.; Galeone, C.; Ruggiero, P.; Bagnasco, D.; Facciolongo, N. A Case of Chronic Eosinophilic Pneumonia in a Patient Treated with Dupilumab. Ther. Clin. Risk Manag. 2019, 15, 869–875. [Google Scholar] [CrossRef] [Green Version]
- Eger, K.; Pet, L.; Weersink, E.J.M.; Bel, E.H. Complications of Switching from Anti-IL-5 or Anti-IL-5R to Dupilumab in Corticosteroid-Dependent Severe Asthma. J. Allergy Clin. Immunol. Pract. 2021, 9, 2913–2915. [Google Scholar] [CrossRef]
- Hoy, S.M. Tezepelumab: First Approval. Drugs 2022, 82, 461–468. [Google Scholar] [CrossRef]
- Kelsen, S.G.; Agache, I.O.; Soong, W.; Israel, E.; Chupp, G.L.; Cheung, D.S.; Theess, W.; Yang, X.; Staton, T.L.; Choy, D.F.; et al. Astegolimab (Anti-ST2) Efficacy and Safety in Adults with Severe Asthma: A Randomized Clinical Trial. J. Allergy Clin. Immunol. 2021, 148, 790–798. [Google Scholar] [CrossRef]
- Pini, L.; Caruso, C.; Colantuono, S.; Bagnasco, D.; Maxwell, A.; Price, R.G.; Howarth, P.; Canonica, G.W. Prospective Italian Real-World Study of Mepolizumab in Severe Eosinophilic Asthma Validates Retrospective Outcome Reports. Clin. Transl. Allergy 2021, 11, e12067. [Google Scholar] [CrossRef] [PubMed]
- Langdon, C.; Mullol, J. Nasal Polyps in Patients with Asthma: Prevalence, Impact, and Management Challenges. J. Asthma Allergy 2016, 9, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fokkens, W.J.; Lund, V.J.; Mullol, J.; Bachert, C.; Alobid, I.; Baroody, F.; Cohen, N.; Cervin, A.; Douglas, R.; Gevaert, P.; et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol. Suppl. 2012, 50, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Brescia, G.; Sfriso, P.; Marioni, G. Role of Blood Inflammatory Cells in Chronic Rhinosinusitis with Nasal Polyps. Acta Oto-Laryngol. 2019, 139, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, P.; Lang-Loidolt, D.; Lackner, A.; Stammberger, H.; Staudinger, H.; van Zele, T.; Holtappels, G.; Tavernier, J.; van Cauwenberge, P.; Bachert, C. Nasal IL-5 Levels Determine the Response to Anti-IL-5 Treatment in Patients with Nasal Polyps. J. Allergy Clin. Immunol. 2006, 118, 1133–1141. [Google Scholar] [CrossRef]
- Lou, H.; Zhang, N.; Bachert, C.; Zhang, L. Highlights of Eosinophilic Chronic Rhinosinusitis with Nasal Polyps in Definition, Prognosis, and Advancement. Int. Forum Allergy Rhinol. 2018, 8, 1218–1225. [Google Scholar] [CrossRef]
- Wang, M.; Bu, X.; Luan, G.; Lin, L.; Wang, Y.; Jin, J.; Zhang, L.; Wang, C. Distinct Type 2-High Inflammation Associated Molecular Signatures of Chronic Rhinosinusitis with Nasal Polyps with Comorbid Asthma. Clin. Transl. Allergy 2020, 10, 26. [Google Scholar] [CrossRef]
- Tiotiu, A.; Oster, J.; Roux, P.; Nguyen Thi, P.; Peiffer, G.; Bonniaud, P.; Dalphin, J.; de Blay, F. Omalizumab’s Effectiveness in Severe Allergic Asthma and Nasal Polyps: A Real-Life Study. J. Investig. Allergol. Clin. Immunol. 2019, 30, 49–57. [Google Scholar] [CrossRef]
- Gevaert, P.; Calus, L.; van Zele, T.; Blomme, K.; de Ruyck, N.; Bauters, W.; Hellings, P.; Brusselle, G.; de Bacquer, D.; van Cauwenberge, P.; et al. Omalizumab Is Effective in Allergic and Nonallergic Patients with Nasal Polyps and Asthma. J. Allergy Clin. Immunol. 2013, 131, 110–116.e1. [Google Scholar] [CrossRef]
- Kariyawasam, H.H.; James, L.K.; Gane, S.B. Dupilumab: Clinical Efficacy of Blocking IL-4/IL-13 Signalling in Chronic Rhinosinusitis with Nasal Polyps. Drug Des. Dev. Ther. 2020, 14, 1757–1769. [Google Scholar] [CrossRef]
- Bachert, C.; Han, J.K.; Desrosiers, M.; Hellings, P.W.; Amin, N.; Lee, S.E.; Mullol, J.; Greos, L.S.; Bosso, J.v.; Laidlaw, T.M.; et al. Efficacy and Safety of Dupilumab in Patients with Severe Chronic Rhinosinusitis with Nasal Polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from Two Multicentre, Randomised, Double-Blind, Placebo-Controlled, Parallel-Group Phase 3 Trials. Lancet 2019, 394, 1638–1650. [Google Scholar] [CrossRef] [Green Version]
- Han, J.K.; Bachert, C.; Fokkens, W.; Desrosiers, M.; Wagenmann, M.; Lee, S.E.; Smith, S.G.; Martin, N.; Mayer, B.; Yancey, S.W.; et al. Mepolizumab for Chronic Rhinosinusitis with Nasal Polyps (SYNAPSE): A Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet Respir. Med. 2021, 9, 1141–1153. [Google Scholar] [CrossRef]
- Silver, J.; Bogart, M.; Molfino, N.A.; Siddall, J.; Small, M.; Hanson, M.; Hahn, B. Factors Leading to Discontinuation of Biologic Therapy in Patients with Severe Asthma. J. Asthma 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Eger, K.; Kroes, J.A.; ten Brinke, A.; Bel, E.H. Long-Term Therapy Response to Anti-IL-5 Biologics in Severe Asthma-A Real-Life Evaluation. J. Allergy Clin. Immunol. Pract. 2021, 9, 1194–1200. [Google Scholar] [CrossRef]
- Fong, W.C.G.; Azim, A.; Knight, D.; Mistry, H.; Freeman, A.; Felongco, M.; Kyyaly, A.; Harvey, M.; Dennison, P.; Zhang, H.; et al. Real-World Omalizumab and Mepolizumab Treated Difficult Asthma Phenotypes and Their Clinical Outcomes. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2021, 51, 1019–1032. [Google Scholar] [CrossRef]
- Ledford, D.; Busse, W.; Trzaskoma, B.; Omachi, T.A.; Rosén, K.; Chipps, B.E.; Luskin, A.T.; Solari, P.G. A randomized multicenter study evaluating Xolair persistence of response after long-term therapy. J. Allergy Clin. Immunol. 2017, 140, 162–169.e2. [Google Scholar] [CrossRef] [Green Version]
- Bel, E.H.D.; Moore, W.C.; Kornmann, O.; Poirier, C.; Kaneko, N.; Smith, S.G.; Martin, N.; Gilson, M.J.; Price, R.G.; Bradford, E.S.; et al. Continued Long-Term Mepolizumab in Severe Eosinophilic Asthma Protects from Asthma Worsening versus Stopping Mepolizumab: COMET Trial. Eur. Respir. J. 2020, 56, 5280. [Google Scholar] [CrossRef]
- Ortega, G.; Tongchinsub, P.; Carr, T. Combination Biologic Therapy for Severe Persistent Asthma. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2019, 123, 309–311. [Google Scholar] [CrossRef]
- Altman, M.C.; Lenington, J.; Bronson, S.; Ayars, A.G. Combination Omalizumab and Mepolizumab Therapy for Refractory Allergic Bronchopulmonary Aspergillosis. J. Allergy Clin. Immunol. Pract. 2017, 5, 1137–1139. [Google Scholar] [CrossRef]
- Dedaj, R.; Unsel, L. Case Study: A Combination of Mepolizumab and Omaluzimab Injections for Severe Asthma. J. Asthma Off. J. Assoc. Care Asthma 2019, 56, 473–474. [Google Scholar] [CrossRef]
- Mahar, P.D.; Zubrinich, C.M.; Manuelpillai, N.; Foley, P. Combination Treatment with Monoclonal Antibodies: Secukinumab, Benralizumab and Dupilumab for the Combined Management of Psoriasis and Severe Asthma. Australas. J. Dermatol. 2021, 62, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Domingo, C.; Pomares, X.; Morón, A.; Sogo, A. Dual Monoclonal Antibody Therapy for a Severe Asthma Patient. Front. Pharmacol. 2020, 11, 1587. [Google Scholar] [CrossRef] [PubMed]
| Drug | Administration Criteria |
|---|---|
| Omalizumab | 6–12 y
|
| Mepolizumab | >6 y
|
| Reslizumab | >18 y
|
| Benralizumab | >18 y
|
| Dupilumab | >12 y
|
| Drug | Dose and Route of Administration | Patient Characteristics | Efficacy | Main Side Effects | Other Diseases Approvation |
|---|---|---|---|---|---|
| Anti IgE | |||||
| Omalizumab [24,25] | Subcutaneous (SC) administration. Prefilled syringe 75 to 600 mg every 2 to 4 wk according to:
| Moderate to severe persistent asthma in adults and pediatric patients 6 years of age and older with a positive skin test or in vitro reactivity to a perennial aeroallergen and symptoms that are inadequately controlled with inhaled corticosteroids and second controller. | -Reduced exacerbations; -Reduced symptoms; -Small effect on FEV1; -Improved quality of life. | Injection side reaction, fever, arthralgia, fatigue, bone fracture, nausea, abdominal pain, pruritus, dermatitis, earache, hypereosinophilic conditions (e.g., EGPA), abrupt discontinuation of oral glucocorticoids; black-box warning for anaphylaxis. |
|
| Anti IL-5 | |||||
| Mepolizumab [35,36,37,38] | Subcutaneous (SC) administration.
Children, ages 6–11 yr: 40 mg every 4 wk. | Add-on maintenance treatment of adult and pediatric patients aged 6 years and older with severe asthma and with an eosinophilic phenotype (>300 cell/µL previous 12 m and > 150 at the moment of first administration). | -Reduced exacerbations; -Reduced symptoms; -Small or moderate effect on FEV1; -Reduction or withdrawal of oral glucocorticoids if blood eosinophils > 150/µL; -Improved quality of life. | Headache, injection site reaction, back pain, arthralgia, fatigue, helminthic infections, hypersensitivity reactions, abrupt discontinuation of oral glucocorticoids, Herpes Zoster infections (rare). |
|
| Reslizumab [48,49] | Intravenous infusion only. Recommended dosage regimen is 3 mg/kg once every 4 weeks by intravenous infusion over 20–50 min. | Add-on maintenance treatment of patients with severe asthma aged 18 years and older and with an eosinophilic phenotype (>400 cell/µL). | -Reduced exacerbations; -Reduced symptoms; -Small or moderate effect on FEV1; -Improved quality of life. | Oropharyngeal pain, helminthic infections, abrupt discontinuation of oral glucocorticoids, black-box warning for anaphylaxis. | |
| Anti IL-5R | |||||
| Benralizumab [50,51] | Subcutaneous injection.
| Add-on maintenance treatment of patients with severe asthma aged 12 years and older and with an eosinophilic phenotype (>300 cell/µL). | -Exacerbations; -Reduced symptoms; -Small or moderate effect on FEV1; -Decrease or withdrawal of oral glucocorticoids if blood eosinophils > 150/µL; -Improved quality of life. | Helminthic infections, hypersensitivity reactions, abrupt discontinuation of oral glucocorticoids. | |
| Anti IL-4R | |||||
| Dupilumab [52] | Subcutaneous injection.
OR -Initial loading dose 600 mg (two 300 mg injections), subsequent dose 300 mg every 2 weeks. (For patients with OCS-dependent asthma or comorbidities *) OR -Dosage in Pediatric Patients 6 to 11 Years of Age (§). | Add-on maintenance treatment of adult and pediatric patients aged 12 years and older with moderate-to-severe asthma characterized by an eosinophilic phenotype or with oral corticosteroid dependent asthma (eosinophils ≥ 150 cell/µL; FeNO > 25 ppb). | -Reduced exacerbations; -Reduced symptoms; -Improved lung function; -Decrease or withdrawal of oral glucocorticoids; -Irrespective of blood eosinophil count at baseline; -Improved quality of life. | Injection site reactions, oropharyngeal pain, eosinophilia, helminthic infections, hypersensitivity reactions, abrupt discontinuation of oral glucocorticoids, hypereosinophilic conditions (e.g., EGPA), conjunctivitis. |
|
| Anti TSLP | |||||
| Tezepelumab µ [53,54,55] | Administer by subcutaneous injection. Recommended dosage is 210 mg administered once every 4 weeks. | Add-on maintenance treatment of adult and pediatric patients aged 12 years and older with severe asthma. | -Reduced exacerbations; -Reduced symptoms; -Improved lung function; -Improved quality of life. | Pharyngitis, arthralgia, back pain, hypersensitivity reactions, helminthic infections, abrupt discontinuation of oral glucocorticoids. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bagnasco, D.; Testino, E.; Nicola, S.; Melissari, L.; Russo, M.; Canevari, R.F.; Brussino, L.; Passalacqua, G. Specific Therapy for T2 Asthma. J. Pers. Med. 2022, 12, 593. https://doi.org/10.3390/jpm12040593
Bagnasco D, Testino E, Nicola S, Melissari L, Russo M, Canevari RF, Brussino L, Passalacqua G. Specific Therapy for T2 Asthma. Journal of Personalized Medicine. 2022; 12(4):593. https://doi.org/10.3390/jpm12040593
Chicago/Turabian StyleBagnasco, Diego, Elisa Testino, Stefania Nicola, Laura Melissari, Maria Russo, Rikki Frank Canevari, Luisa Brussino, and Giovanni Passalacqua. 2022. "Specific Therapy for T2 Asthma" Journal of Personalized Medicine 12, no. 4: 593. https://doi.org/10.3390/jpm12040593
APA StyleBagnasco, D., Testino, E., Nicola, S., Melissari, L., Russo, M., Canevari, R. F., Brussino, L., & Passalacqua, G. (2022). Specific Therapy for T2 Asthma. Journal of Personalized Medicine, 12(4), 593. https://doi.org/10.3390/jpm12040593






