Molecular and Cellular Mechanism of Action of Chrysotile Asbestos in MRC5 Cell Line
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cultivation of Cell Culture
2.2. Treatment of MRC5 Cells with Asbestos
2.3. ROS Measurement
2.4. Comet Assay
2.5. Determination of Cell Viability
2.6. Isolation of cf mtDNA
2.7. cf mtDNA Isolation from Medium
2.8. microRNA Isolation from Cells
2.9. microRNA Analysis by qPCR
2.10. Statistical Data Analysis
3. Results
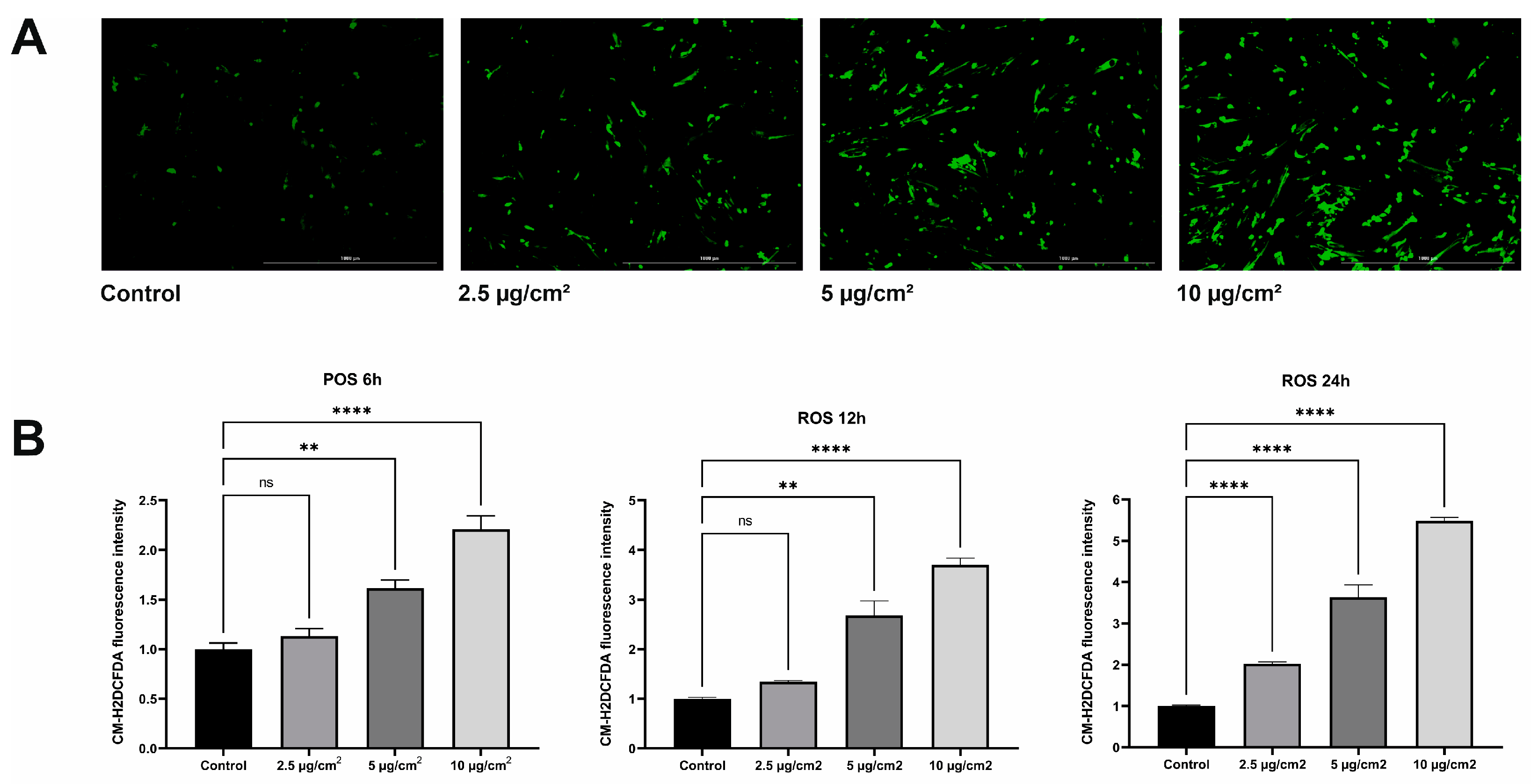
3.1. Asbestos Increases ROS Production in MRC5
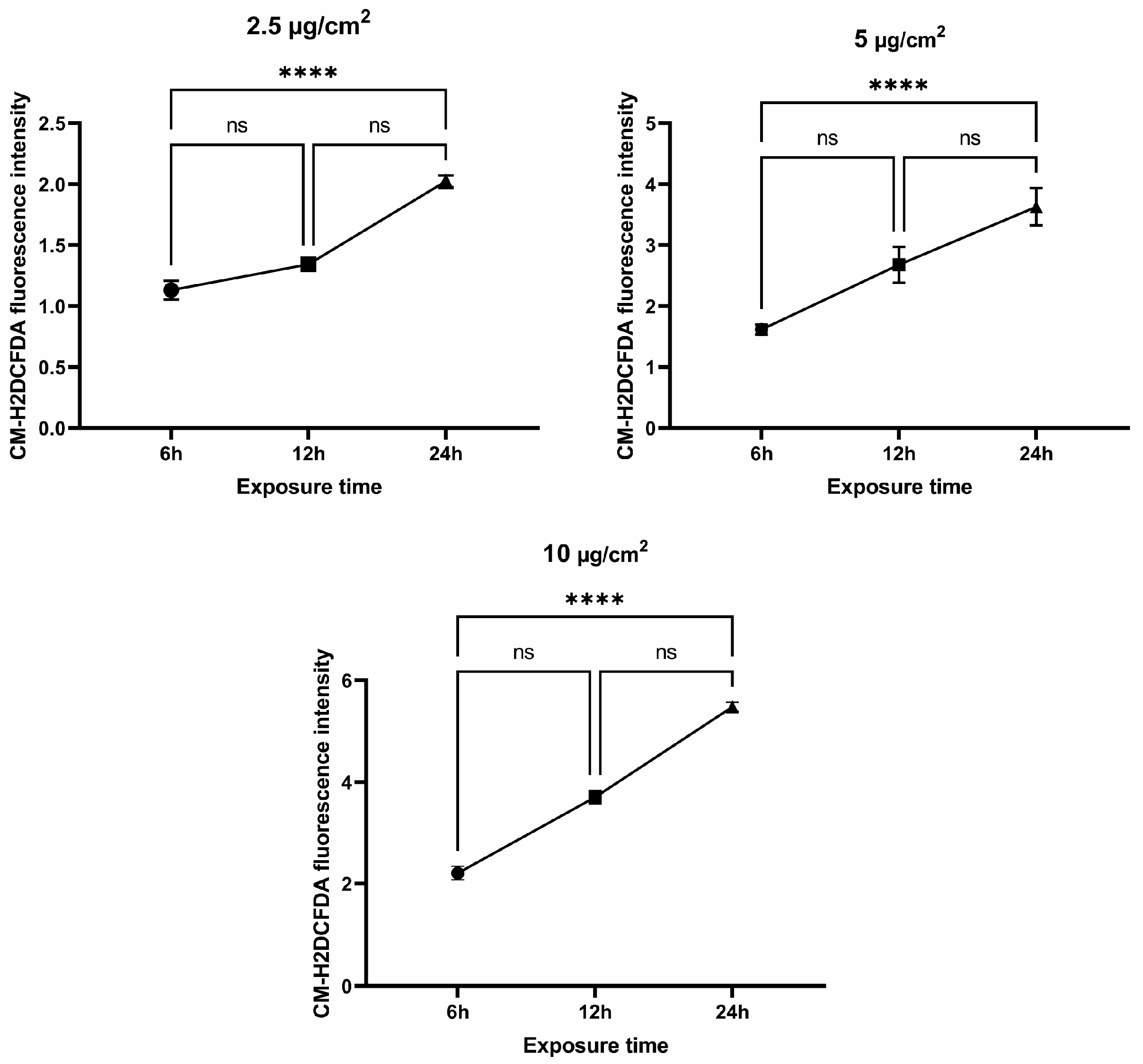
3.2. Genotoxic Effects of Chrysotile Asbestos
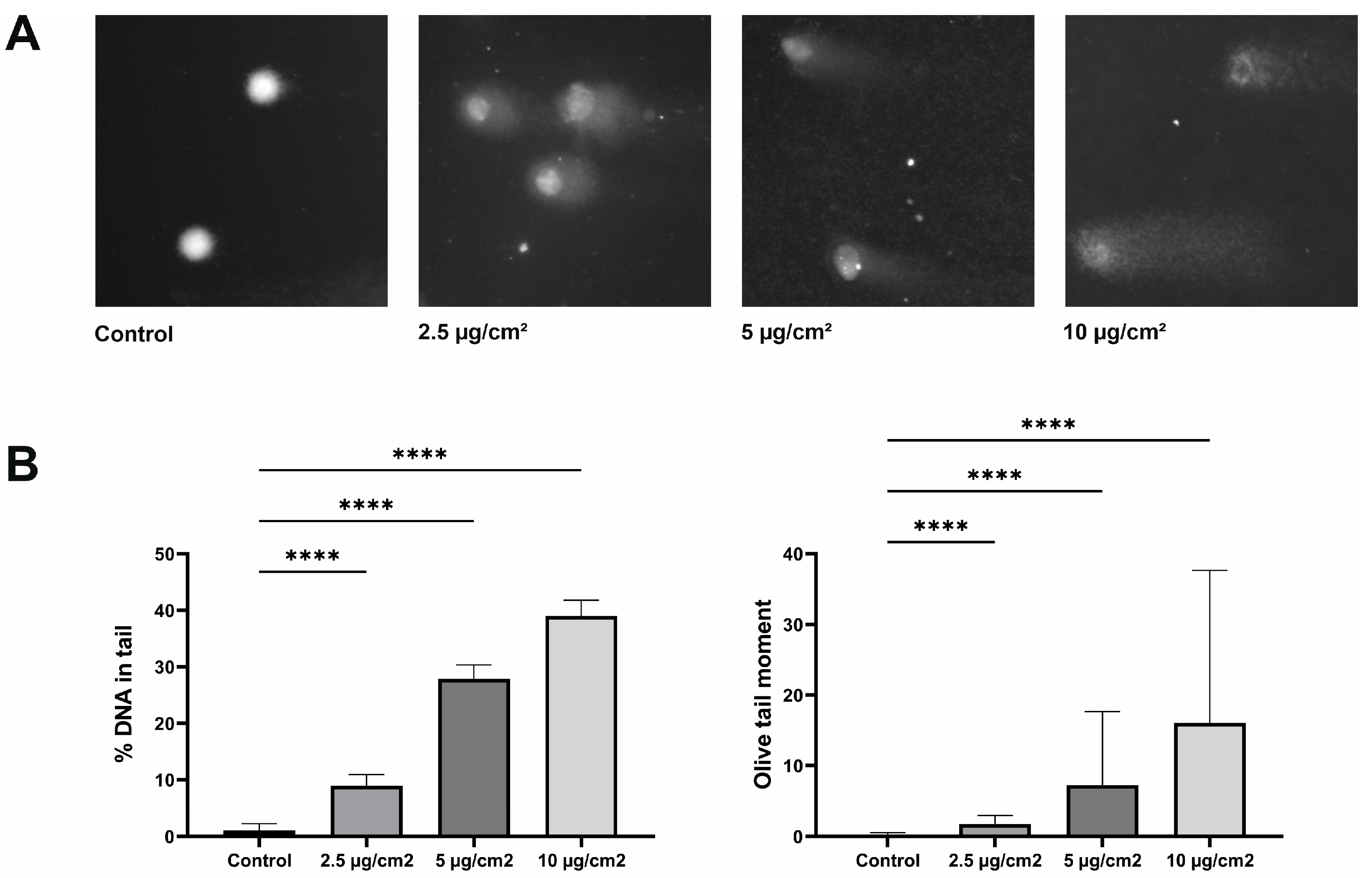
3.3. Cytotoxic Effect of Chrysotile Asbestos on Healthy Lung Fibroblasts
3.4. The Copy Number of cf mtDNA in Media
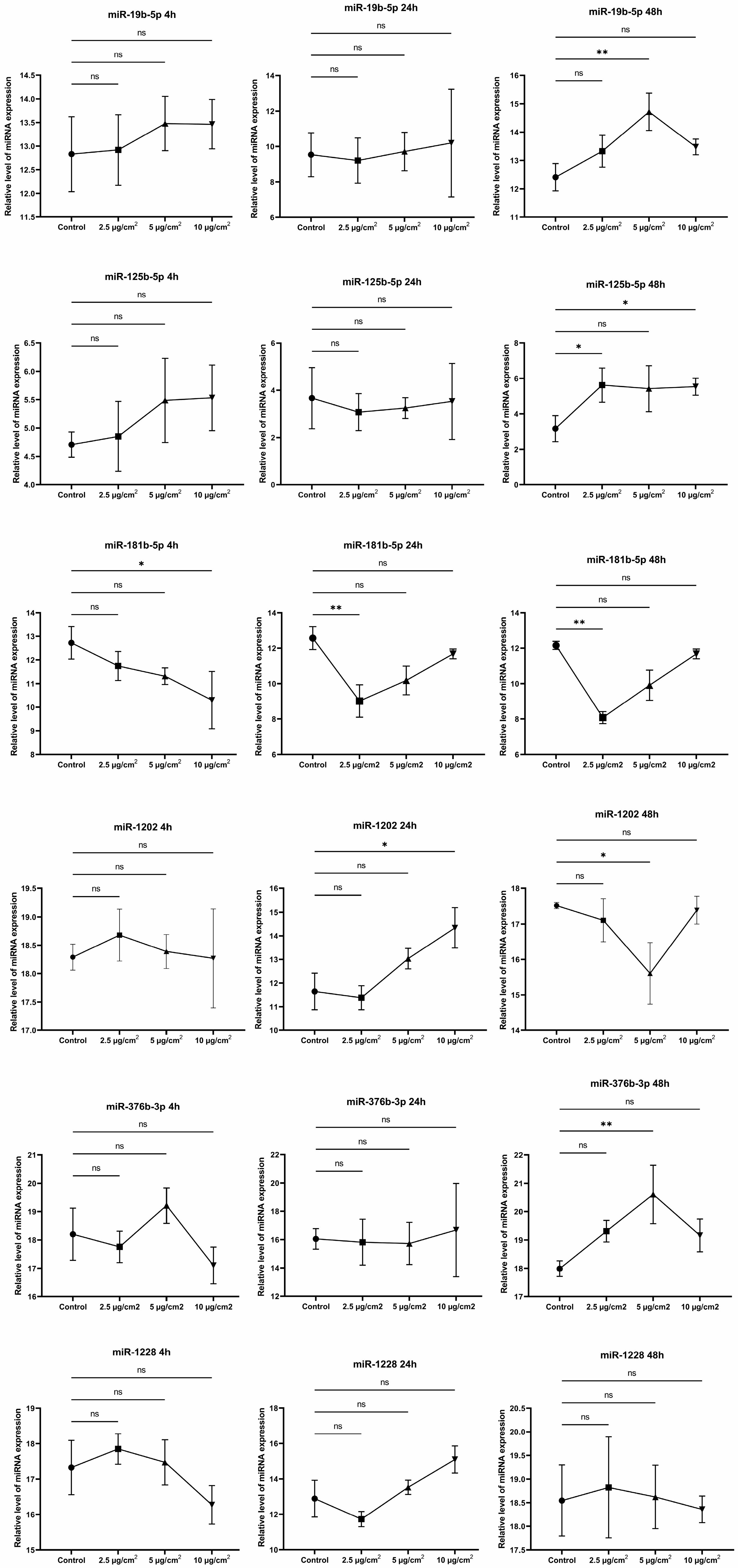
3.5. MicroRNA Expression Profile Analysis between Asbestos-Treated Cells and Controls
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jenkins, R.; Walker, J.; Roy, U.B. 2022 cancer statistics: Focus on lung cancer. Future Oncol. 2023; epub ahead of print. [Google Scholar] [CrossRef]
- The Kazakh Institute of Oncology and Radiology Scientific Council. Indicators of the Oncology Service of the Republic of Kazakhstan, 2021; Kaidarova, D.R., Ed.; KazIOR: Almaty, Kazakhstan, 2022; Volume 8. [Google Scholar]
- National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Available online: https://seer.cancer.gov/ (accessed on 15 April 2022).
- International Agency for Research on Cancer (IARC). Available online: https://www.iarc.who.int/ (accessed on 10 December 2020).
- Markowitz, S. Asbestos-related lung cancer and malignant mesothelioma of the pleura: Selected current issues. Semin. Respir. Crit. Care Med. 2015, 36, 334–346. [Google Scholar] [CrossRef]
- Musk, A.W.; de Klerk, N.; Reid, A.; Hui, J.; Franklin, P.; Brims, F. Asbestos-related diseases. Int. J. Tuberc. Lung Dis. 2020, 24, 562–567. [Google Scholar] [CrossRef]
- Berman, D.W.; Crump, K.S. A meta-analysis of asbestos-related cancer risk that addresses fiber size and mineral type. Crit. Rev. Toxicol. 2008, 38 (Suppl. S1), 49–73. [Google Scholar] [CrossRef]
- Huang, X.Y.; Ye, Q. Asbestos exposure and asbestos-related malignant diseases:an epidemiological review. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2021, 39, 233–236. [Google Scholar]
- Chen, J.; Wang, C.; Zhang, J.; Zhang, T.; Liang, H.; Mao, S.; Li, H.; Wang, Z. A comparative study of the disease burden attributable to asbestos in Brazil, China, Kazakhstan, and Russia between 1990 and 2019. BMC Public Health 2022, 22, 2012. [Google Scholar] [CrossRef] [PubMed]
- Kostanai Minerals JSC. Available online: https://km.kz/ (accessed on 12 August 2010).
- Innes, E.; Yiu, H.H.P.; McLean, P.; Brown, W.; Boyles, M. Simulated biological fluids—A systematic review of their biological relevance and use in relation to inhalation toxicology of particles and fibers. Crit. Rev. Toxicol. 2021, 51, 217–248. [Google Scholar] [CrossRef]
- Turci, F.; Tomatis, M.; Lesci, I.G.; Roveri, N.; Fubini, B. The iron-related molecular toxicity mechanism of synthetic asbestos nanofibers: A model study for high-aspect-ratio nanoparticles. Chemistry 2011, 17, 350–358. [Google Scholar] [CrossRef]
- Gualtieri, A.F. Journey to the centre of the lung. The perspective of a mineralogist on the carcinogenic effects of mineral fibers in the lungs. J. Hazard. Mater. 2023, 442, 130077. [Google Scholar] [CrossRef] [PubMed]
- Picca, A.; Calvani, R.; Coelho-Junior, H.J.; Landi, F.; Bernabei, R.; Marzetti, E. Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation: Intertwined Roads to Neurodegeneration. Antioxidants 2020, 9, 647. [Google Scholar] [CrossRef]
- Bulgakova, O.; Kussainova, A.; Kakabayev, A.; Aripova, A.; Baikenova, G.; Izzotti, A.; Bersimbaev, R. The level of free-circulating mtDNA in patients with radon-induced lung cancer. Environ. Res. 2022, 207, 112215. [Google Scholar] [CrossRef] [PubMed]
- Hubaux, R.; Becker-Santos, D.D.; Enfield, K.S.; Lam, S.; Lam, W.L.; Martinez, V.D. Arsenic, asbestos and radon: Emerging players in lung tumorigenesis. Environ. Health 2012, 11, 89. [Google Scholar] [CrossRef]
- Bersimbaev, R.; Bulgakova, O.; Aripova, A.; Kussainova, A.; Ilderbayev, O. Role of microRNAs in Lung Carcinogenesis Induced by Asbestos. J. Pers. Med. 2021, 11, 97. [Google Scholar] [CrossRef]
- Liao, B.; Dong, S.; Xu, Z.; Gao, F.; Zhang, S.; Liang, R. MiR-19b-3p regulated by BC002059/ABHD10 axis promotes cell apoptosis in myocardial infarction. Biol. Direct 2022, 17, 20. [Google Scholar] [CrossRef] [PubMed]
- Vandghanooni, S.; Eskandani, M. Comet assay: A method to evaluate genotoxicity of nano-drug delivery system. Bioimpacts 2011, 1, 87–97. [Google Scholar] [CrossRef]
- Ellinger, J.; Müller, S.C.; Wernert, N.; von Ruecker, A.; Bastian, P.J. Mitochondrial DNA in serum of patients with prostate cancer: A predictor of biochemical recurrence after prostatectomy. BJU Int. 2008, 102, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Budnik, L.T.; Kloth, S.; Baur, X.; Preisser, A.M.; Schwarzenbach, H. Circulating mitochondrial DNA as biomarker linking environmental chemical exposure to early preclinical lesions elevation of mtDNA in human serum after exposure to carcinogenic halo-alkane-based pesticides. PLoS ONE 2013, 8, e64413. [Google Scholar] [CrossRef]
- Bozkurt, S.B.; Ozturk, B.; Kocak, N.; Unlu, A. Differences of time-dependent microRNA expressions in breast cancer cells. Noncoding RNA Res. 2020, 6, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Pira, E.; Donato, F.; Maida, L.; Discalzi, G. Exposure to asbestos: Past, present and future. J. Thorac. Dis. 2018, 10 (Suppl. S2), S237–S245. [Google Scholar] [CrossRef]
- Huh, D.A.; Chae, W.R.; Choi, Y.H.; Kang, M.S.; Lee, Y.J.; Moon, K.W. Disease Latency according to Asbestos Exposure Characteristics among Malignant Mesothelioma and Asbestos-Related Lung Cancer Cases in South Korea. Int. J. Environ. Res. Public Health 2022, 19, 15934. [Google Scholar] [CrossRef]
- LaDou, J.; Castleman, B.; Frank, A.; Gochfeld, M.; Greenberg, M.; Huff, J.; Joshi, T.K.; Landrigan, P.J.; Lemen, R.; Myers, J.; et al. The case for a global ban on asbestos. Environ. Health Perspect. 2010, 118, 897–901. [Google Scholar] [CrossRef]
- Belackova, L.; Verbeek, J.H.; Hoving, J.L.; Molen, H.F.; Gagliardi, D.; Curti, S.; Hulshof, C.T.J.; Scheepers, P.T.J.; Marinaccio, A. Legal banning of asbestos for preventing asbestos exposure. Cochrane Database Syst. Rev. 2022, 2022, CD015106. [Google Scholar] [CrossRef]
- Lévêque, E.; Lacourt, A.; Luce, D.; Sylvestre, M.P.; Guénel, P.; Stücker, I.; Leffondré, K. Time-dependent effect of intensity of smoking and of occupational exposure to asbestos on the risk of lung cancer: Results from the ICARE case-control study. Occup. Environ. Med. 2018, 75, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Pietrofesa, R.A.; Velalopoulou, A.; Albelda, S.M.; Christofidou-Solomidou, M. Asbestos Induces Oxidative Stress and Activation of Nrf2 Signaling in Murine Macrophages: Chemopreventive Role of the Synthetic Lignan Secoisolariciresinol Diglucoside (LGM2605). Int. J. Mol. Sci. 2016, 17, 322. [Google Scholar] [CrossRef]
- Gulino, G.R.; Polimeni, M.; Prato, M.; Gazzano, E.; Kopecka, J.; Colombatto, S.; Ghigo, D.; Aldieri, E. Effects of Chrysotile Exposure in Human Bronchial Epithelial Cells: Insights into the Pathogenic Mechanisms of Asbestos-Related Diseases. Environ. Health Perspect. 2016, 124, 776–784. [Google Scholar] [CrossRef]
- Thompson, J.K.; MacPherson, M.B.; Beuschel, S.L.; Shukla, A. Asbestos-Induced Mesothelial to Fibroblastic Transition Is Modulated by the Inflammasome. Am. J. Pathol. 2017, 187, 665–678. [Google Scholar] [CrossRef] [PubMed]
- Sesko, A.M.; Mossman, B.T. Sensitivity of hamster tracheal epithelial cells to asbestiform minerals modulated by serum and by transforming growth factor beta 1. Cancer Res. 1989, 49, 2743–2749. [Google Scholar]
- Zhang, F.; Yuan, X.; Sun, H.; Yin, X.; Gao, Y.; Zhang, M.; Jia, Z.; Yu, M.; Ying, S.; Xia, H.; et al. A nontoxic dose of chrysotile can malignantly transform Met-5A cells, in which microRNA-28 has inhibitory effects. J. Appl. Toxicol. 2021, 41, 1879–1892. [Google Scholar] [CrossRef]
- Li, P.; Liu, T.; Kamp, D.W.; Lin, Z.; Wang, Y.; Li, D.; Yang, L.; He, H.; Liu, G. The c-Jun N-terminal kinase signaling pathway mediates chrysotile asbestos-induced alveolar epithelial cell apoptosis. Mol. Med. Rep. 2015, 11, 3626–3634. [Google Scholar] [CrossRef] [PubMed]
- Kido, T.; Morimoto, Y.; Asonuma, E.; Yatera, K.; Ogami, A.; Oyabu, T.; Tanaka, I.; Kido, M. Chrysotile asbestos causes AEC apoptosis via the caspase activation in vitro and in vivo. Inhal. Toxicol. 2008, 20, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Qi, F.; Okimoto, G.; Jube, S.; Napolitano, A.; Pass, H.I.; Laczko, R.; Demay, R.M.; Khan, G.; Tiirikainen, M.; Rinaudo, C.; et al. Continuous exposure to chrysotile asbestos can cause transformation of human mesothelial cells via HMGB1 and TNF-α signaling. Am. J. Pathol. 2013, 183, 1654–1666. [Google Scholar] [CrossRef]
- Vodicka, P.; Vodenkova, S.; Horak, J.; Opattova, A.; Tomasova, K.; Vymetalkova, V.; Stetina, R.; Hemminki, K.; Vodickova, L. An investigation of DNA damage and DNA repair in chemical carcinogenesis triggered by small-molecule xenobiotics and in cancer: Thirty years with the comet assay. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2023, 885, 503564. [Google Scholar] [CrossRef] [PubMed]
- Roos, W.P.; Kaina, B. DNA damage-induced cell death by apoptosis. Trends Mol. Med. 2006, 12, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Zanella, C.L.; Posada, J.; Tritton, T.R.; Mossman, B.T. Asbestos causes stimulation of the extracellular signal-regulated kinase 1 mitogen-activated protein kinase cascade after phosphorylation of the epidermal growth factor receptor. Cancer Res. 1996, 56, 5334–5338. [Google Scholar] [PubMed]
- Zolondick, A.A.; Gaudino, G.; Xue, J.; Pass, H.I.; Carbone, M.; Yang, H. Asbestos-induced chronic inflammation in malignant pleural mesothelioma and related therapeutic approaches-a narrative review. Precis. Cancer Med. 2021, 4, 27. [Google Scholar] [CrossRef]
- Ray, P.D.; Huang, B.W.; Tsuji, Y. Reactive oxygen species (ROS) homeostasis and redox regulation in cellular signaling. Cell. Signal. 2012, 24, 981–990. [Google Scholar] [CrossRef]
- Pérez-Treviño, P.; Velásquez, M.; García, N. Mechanisms of mitochondrial DNA escape and its relationship with different metabolic diseases. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165761. [Google Scholar] [CrossRef]
- García, N.; Chávez, E. Mitochondrial DNA fragments released through the permeability transition pore correspond to specific gene size. Life Sci. 2007, 81, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Barbas, A.S.; Lin, L.; Scheuermann, U.; Bishawi, M.; Brennan, T.V. Mitochondria Released by Apoptotic Cell Death Initiate Innate Immune Responses. Immunohorizons 2018, 2, 384–397. [Google Scholar] [CrossRef]
- Zhang, Q.; Raoof, M.; Chen, Y.; Sumi, Y.; Sursal, T.; Junger, W.; Brohi, K.; Itagaki, K.; Hauser, C.J. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature 2010, 464, 104–107. [Google Scholar] [CrossRef]
- Hasleton, P.S. The internal surface area of the adult human lung. J. Anat. 1972, 112 Pt 3, 391–400. [Google Scholar]
- Ren, X.H.; Zhou, D.L.; Du, L.L.; Wang, M.Z.; Lan, Y.J. The dose-response relationship of chrysotile asbestos exposure and lung cancer in cohort study. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2013, 31, 189–194. [Google Scholar]
- Deng, Q.; Wang, X.; Wang, M.; Lan, Y. Exposure-response relationship between chrysotile exposure and mortality from lung cancer and asbestosis. Occup. Environ. Med. 2012, 69, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Lacourt, A.; Lévêque, E.; Guichard, E.; Gilg Soit Ilg, A.; Sylvestre, M.P.; Leffondré, K. Dose-time-response association between occupational asbestos exposure and pleural mesothelioma. Occup. Environ. Med. 2017, 74, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Panico, A.; Tumolo, M.R.; Leo, C.G.; Donno, A.D.; Grassi, T.; Bagordo, F.; Serio, F.; Idolo, A.; Masi, R.D.; Mincarone, P.; et al. The influence of lifestyle factors on miRNA expression and signal pathways: A review. Epigenomics 2021, 13, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Souma, K.; Shichino, S.; Hashimoto, S.; Ueha, S.; Tsukui, T.; Nakajima, T.; Suzuki, H.I.; Shand, F.H.W.; Inagaki, Y.; Nagase, T.; et al. Lung fibroblasts express a miR-19a-19b-20a sub-cluster to suppress TGF-β-associated fibroblast activation in murine pulmonary fibrosis. Sci. Rep. 2018, 8, 16642. [Google Scholar] [CrossRef]
- Biamonte, F.; Battaglia, A.M.; Zolea, F.; Oliveira, D.M.; Aversa, I.; Santamaria, G.; Giovannone, E.D.; Rocco, G.; Viglietto, G.; Costanzo, F. Ferritin heavy subunit enhances apoptosis of non-small cell lung cancer cells through modulation of miR-125b/p53 axis. Cell Death Dis. 2018, 9, 1174. [Google Scholar] [CrossRef]
- Liu, B.; Guo, Z.; Gao, W. miR-181b-5p promotes proliferation and inhibits apoptosis of hypertrophic scar fibroblasts through regulating the MEK/ERK/p21 pathway. Exp. Ther. Med. 2019, 17, 1537–1544. [Google Scholar] [CrossRef] [PubMed]
- Frankel, D.; Delecourt, V.; Novoa-del-Toro, E.M.; Robin, J.D.; Airault, C.; Bartoli, C.; Carabalona, A.; Perrin, S.; Mazaleyrat, K.; De Sandre-Giovannoli, A.; et al. miR-376a-3p and miR-376b-3p overexpression in Hutchinson-Gilford progeria fibroblasts inhibits cell proliferation and induces premature senescence. iScience 2022, 25, 103757. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Zhang, Y.; Tang, Y.; Dai, H.; OuYang, Y.; Li, C.; Yu, M. MiRNA-1202 promotes the TGF-β1-induced proliferation, differentiation and collagen production of cardiac fibroblasts by targeting nNOS. PLoS ONE 2021, 16, e0256066. [Google Scholar] [CrossRef]


| Dose of Exposure | Asbestos Fiber Type | Cell Culture | Exposure Time | Cellular Effect | Reference |
|---|---|---|---|---|---|
| 1 µg/cm2 | Chrysotile | BEAS-2B, NuLi-1, A549 | 30 min, 1, 3, 6, and 72 h | Significantly decreased levels of E-cadherin and β-catenin were noted, while TGF-β levels were increased. After 30 min, there was a decrease in cytoplasmic p-Smad2 and an increase in nuclear p-Smad2. TGF-β levels were increased after 1 h of asbestos exposure. The ratio of phosphorylated to nonphosphorylated Akt (p-Akt/Akt) was increased from 30 min to 3 h. | [29] |
| 1 µg/cm2 | Crocidolite | LP9 and HPM3 | 2 weeks | SNAI1 protein was shown to de-crease at 24 and 48 h in LP9 cells, and HPM3 cells showed a twofold increase after 1 week of asbestos exposure. TIMP1 protein was increased 36-fold in LP9 after just 24 h of exposure. | [30] |
| 1, 5, 10, and 20 µg/cm2 | Crocodilite | Murine peritoneal macrophages (MF) | 24 h | An asbestos dose of 20 µg/cm2 caused a twofold increase in ROS, as well as an increase in nuclear Nrf2 levels, with the highest concentrations observed 2 and 12 h after exposure. | [28] |
| 0.1–0.5 µg/cm2 | Crocidolite | Cloned diploid hamster tracheal epithelial cells | 3–24 h | Increases in [3H] thymidine incorporation and colony formation efficiency were observed. | [31] |
| 5 µg/cm2 | Chrysotile | MeT-5A cells | 24 h | Decreased expression of microRNA-28 has been shown. | [32] |
| 50, 100, 150, 200, and 300 µg/cm2 | Chrysotile | A549 | A dose of 150 µg/cm2 provoked the release of cytochrome c and an increase in the level of Bax/Bak and caspase-9 and, as a result, caused apoptosis after 48 h of exposure. | [33] | |
| 50 µg/cm2 | Chrysotile | A549 | 48 h | There was an increase in the expression of cleaved caspase-3 and -9. | [34] |
| 5 µg/cm2 | Crocidolite and chrysotile | HM cells | 24 h | Chrysotile has been observed to induce rapid cell death and increased release of HMGB1 and TNF-α. | [35] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kussainova, A.; Bulgakova, O.; Aripova, A.; Ibragimova, M.; Pulliero, A.; Begimbetova, D.; Bersimbaev, R.; Izzotti, A. Molecular and Cellular Mechanism of Action of Chrysotile Asbestos in MRC5 Cell Line. J. Pers. Med. 2023, 13, 1599. https://doi.org/10.3390/jpm13111599
Kussainova A, Bulgakova O, Aripova A, Ibragimova M, Pulliero A, Begimbetova D, Bersimbaev R, Izzotti A. Molecular and Cellular Mechanism of Action of Chrysotile Asbestos in MRC5 Cell Line. Journal of Personalized Medicine. 2023; 13(11):1599. https://doi.org/10.3390/jpm13111599
Chicago/Turabian StyleKussainova, Assiya, Olga Bulgakova, Akmaral Aripova, Milana Ibragimova, Alessandra Pulliero, Dinara Begimbetova, Rakhmetkazhi Bersimbaev, and Alberto Izzotti. 2023. "Molecular and Cellular Mechanism of Action of Chrysotile Asbestos in MRC5 Cell Line" Journal of Personalized Medicine 13, no. 11: 1599. https://doi.org/10.3390/jpm13111599
APA StyleKussainova, A., Bulgakova, O., Aripova, A., Ibragimova, M., Pulliero, A., Begimbetova, D., Bersimbaev, R., & Izzotti, A. (2023). Molecular and Cellular Mechanism of Action of Chrysotile Asbestos in MRC5 Cell Line. Journal of Personalized Medicine, 13(11), 1599. https://doi.org/10.3390/jpm13111599







